Label: FINASTERIDE tablet, film coated
-
NDC Code(s):
31722-525-01,
31722-525-05,
31722-525-10,
31722-525-30, view more31722-525-90
- Packager: Camber Pharmaceuticals Inc.
- Category: HUMAN PRESCRIPTION DRUG LABEL
- DEA Schedule: None
- Marketing Status: Abbreviated New Drug Application
Drug Label Information
Updated July 15, 2010
If you are a consumer or patient please visit this version.
- Download DRUG LABEL INFO: PDF XML
- Official Label (Printer Friendly)
-
DESCRIPTION
Finasteride USP, a synthetic 4-azasteroid compound, is a specific inhibitor of steroid Type II 5α-reductase, an intracellular enzyme that converts the androgen testosterone into 5α-dihydrotestosterone (DHT).
Finasteride is 4-azaandrost-1-ene-17-carboxamide, N-(1,1-dimethylethyl)-3-oxo-, (5α,17β)-. The empirical formula of finasteride is C23H36N2O2 and its molecular weight is 372.55. Its structural formula is:
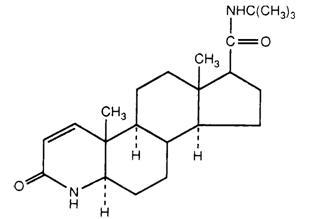
Finasteride is a white crystalline powder with a melting point near 250°C. It is freely soluble in chloroform and in lower alcohol solvents, but is practically insoluble in water.
Finasteride tablets USP for oral administration are film-coated tablets that contain 5 mg of finasteride and the following inactive ingredients: lactose monohydrate, microcrystalline cellulose, pregelatinized starch, sodium starch glycolate, docusate sodium, magnesium stearate, opadry blue (FD&C blue #2 aluminum lake, hypromellose, talc, titanium dioxide, yellow iron oxide).
-
CLINICAL PHARMACOLOGY
The development and enlargement of the prostate gland is dependent on the potent androgen, 5α-dihydrotestosterone (DHT). Type II 5α-reductase metabolizes testosterone to DHT in the prostate gland, liver and skin. DHT induces androgenic effects by binding to androgen receptors in the cell nuclei of these organs.
Finasteride is a competitive and specific inhibitor of Type II 5α-reductase with which it slowly forms a stable enzyme complex. Turnover from this complex is extremely slow (t½ ~ 30 days). This has been demonstrated both in vivo and in vitro. Finasteride has no affinity for the androgen receptor. In man, the 5α-reduced steroid metabolites in blood and urine are decreased after administration of finasteride.
In man, a single 5 mg oral dose of finasteride tablets USP produces a rapid reduction in serum DHT concentration, with the maximum effect observed 8 hours after the first dose. The suppression of DHT is maintained throughout the 24-hour dosing interval and with continued treatment. Daily dosing of finasteride tablets USP at 5 mg/day for up to 4 years has been shown to reduce the serum DHT concentration by approximately 70%. The median circulating level of testosterone increased by approximately 10 to 20% but remained within the physiologic range.
Adult males with genetically inherited Type II 5α-reductase deficiency also have decreased levels of DHT. Except for the associated urogenital defects present at birth, no other clinical abnormalities related to Type II 5α-reductase deficiency have been observed in these individuals. These individuals have a small prostate gland throughout life and do not develop BPH.
In patients with BPH treated with finasteride (1 to 100 mg/day) for 7 to 10 days prior to prostatectomy, an approximate 80% lower DHT content was measured in prostatic tissue removed at surgery, compared to placebo; testosterone tissue concentration was increased up to 10 times over pretreatment levels, relative to placebo. Intraprostatic content of prostate-specific antigen (PSA) was also decreased.
In healthy male volunteers treated with finasteride tablets USP for 14 days, discontinuation of therapy resulted in a return of DHT levels to pretreatment levels in approximately 2 weeks. In patients treated for three months, prostate volume, which declined by approximately 20%, returned to close to baseline value after approximately three months of discontinuation of therapy.
Pharmacokinetics
Absorption
In a study of 15 healthy young subjects, the mean bioavailability of finasteride 5 mg tablets was 63% (range 34 to 108 %), based on the ratio of area under the curve (AUC) relative to an intravenous (IV) reference dose. Maximum finasteride plasma concentration averaged 37 ng/mL (range, 27 to 49 ng/mL) and was reached 1 to 2 hours postdose. Bioavailability of finasteride was not affected by food.
Distribution
Mean steady-state volume of distribution was 76 liters (range, 44 to 96 liters). Approximately 90% of circulating finasteride is bound to plasma proteins. There is a slow accumulation phase for finasteride after multiple dosing. After dosing with 5 mg/day of finasteride for 17 days, plasma concentrations of finasteride were 47 and 54% higher than after the first dose in men 45 to 60 years old (n=12) and ≥70 years old (n=12), respectively. Mean trough concentrations after 17 days of dosing were 6.2 ng/mL (range, 2.4 to 9.8 ng/mL) and 8.1 ng/mL (range, 1.8 to 19.7 ng/mL), respectively, in the two age groups. Although steady state was not reached in this study, mean trough plasma concentration in another study in patients with BPH (mean age, 65 years) receiving 5 mg/day was 9.4 ng/mL (range, 7.1 to 13.3 ng/mL; n=22) after over a year of dosing.
Finasteride has been shown to cross the blood brain barrier but does not appear to distribute preferentially to the CSF.
In 2 studies of healthy subjects (n=69) receiving finasteride tablets USP, 5 mg/day for 6 to 24 weeks, finasteride concentrations in semen ranged from undetectable (<0.1 ng/mL) to 10.54 ng/mL. In an earlier study using a less sensitive assay, finasteride concentrations in the semen of 16 subjects receiving finasteride tablets USP, 5 mg/day ranged from undetectable (<1.0 ng/mL) to 21 ng/mL. Thus, based on a 5-mL ejaculate volume, the amount of finasteride in semen was estimated to be 50- to 100-fold less than the dose of finasteride (5 mcg) that had no effect on circulating DHT levels in men (see also PRECAUTIONS, Pregnancy).
Metabolism
Finasteride is extensively metabolized in the liver, primarily via the cytochrome P450 3A4 enzyme subfamily. Two metabolites, the t-butyl side chain monohydroxylated and monocarboxylic acid metabolites, have been identified that possess no more than 20% of the 5α-reductase inhibitory activity of finasteride.
In healthy young subjects (n=15), mean plasma clearance of finasteride was 165 mL/min (range, 70 to 279 mL/min) and mean elimination half-life in plasma was 6 hours (range, 3 to 16 hours). Following an oral dose of 14C-finasteride in man (n=6), a mean of 39% (range, 32 to 46 %) of the dose was excreted in the urine in the form of metabolites; 57% (range, 51 to 64 %) was excreted in the feces.
The mean terminal half-life of finasteride in subjects ≥70 years of age was approximately 8 hours (range, 6 to 15 hours; n=12), compared with 6 hours (range, 4 to 12 hours; n=12) in subjects 45 to 60 years of age. As a result, mean AUC(0 to 24 hr) after 17 days of dosing was 15% higher in subjects ≥70 years of age than in subjects 45 to 60 years of age (p=0.02).
Special Populations
Pediatric: Finasteride pharmacokinetics have not been investigated in patients <18 years of age.
Gender: Finasteride pharmacokinetics in women are not available.
Geriatric: No dosage adjustment is necessary in the elderly. Although the elimination rate of finasteride is decreased in the elderly, these findings are of no clinical significance. See also Pharmacokinetics, Excretion, PRECAUTIONS, Geriatric Use and DOSAGE AND ADMINISTRATION.
Race: The effect of race on finasteride pharmacokinetics has not been studied.
Renal Insufficiency: No dosage adjustment is necessary in patients with renal insufficiency. In patients with chronic renal impairment, with creatinine clearances ranging from 9.0 to 55 mL/min, AUC, maximum plasma concentration, half-life, and protein binding after a single dose of 14C-finasteride were similar to values obtained in healthy volunteers. Urinary excretion of metabolites was decreased in patients with renal impairment. This decrease was associated with an increase in fecal excretion of metabolites. Plasma concentrations of metabolites were significantly higher in patients with renal impairment (based on a 60% increase in total radioactivity AUC). However, finasteride has been well tolerated in BPH patients with normal renal function receiving up to 80 mg/day for 12 weeks, where exposure of these patients to metabolites would presumably be much greater.
Hepatic Insufficiency: The effect of hepatic insufficiency on finasteride pharmacokinetics has not been studied. Caution should be used in the administration of finasteride tablets USP in those patients with liver function abnormalities, as finasteride is metabolized extensively in the liver.
Drug Interactions (also see PRECAUTIONS, Drug Interactions)
No drug interactions of clinical importance have been identified. Finasteride does not appear to affect the cytochrome P450-linked drug metabolism enzyme system. Compounds that have been tested in man have included antipyrine, digoxin, propranolol, theophylline, and warfarin, and no clinically meaningful interactions were found.
Mean (SD) Pharmacokinetic Parameters in Healthy Young Subjects (n=15) Mean (± SD) *Range Bioavailability 63%
(34 to 108 %)*Clearance (mL/min) 165 (55) Volume of Distribution (L) 76 (14) Half-Life (hours) 6.2 (2.1) Mean (SD) Noncompartmental Pharmacokinetic Parameters After Multiple Doses of 5 mg/day in Older Men Mean (± SD) 45 to 60 years
old (n=12)≥70 years
old (n=12)*First-dose values; all other parameters are last-dose values AUC (ng•hr/mL) 389 (98) 463 (186) Peak Concentration (ng/mL) 46.2 (8.7) 48.4 (14.7) Time to Peak (hours) 1.8 (0.7) 1.8 (0.6) Half-Life (hours)* 6.0 (1.5) 8.2 (2.5) Finasteride tablets USP, 5 mg/day was initially evaluated in patients with symptoms of BPH and enlarged prostates by digital rectal examination in two 1-year, placebo-controlled, randomized, double-blind studies and their 5-year open extensions.
Finasteride tablets USP was further evaluated in a long-term efficacy and safety study, a double-blind, randomized, placebo-controlled, 4-year, multicenter study. 3040 patients between the ages of 45 and 78, with moderate to severe symptoms of BPH and an enlarged prostate upon digital rectal examination, were randomized into the study (1524 to finasteride, 1516 to placebo) and 3016 patients were evaluable for efficacy. 1883 patients completed the 4-year study (1000 in the finasteride group, 883 in the placebo group).
Effect on Symptom Score
Symptoms were quantified using a score similar to the American Urological Association Symptom Score, which evaluated both obstructive symptoms (impairment of size and force of stream, sensation of incomplete bladder emptying, delayed or interrupted urination) and irritative symptoms (nocturia, daytime frequency, need to strain or push the flow of urine) by rating on a 0 to 5 scale for six symptoms and a 0 to 4 scale for one symptom, for a total possible score of 34.
Patients in a long-term efficacy and safety study had moderate to severe symptoms at baseline (mean of approximately 15 points on a 0 to 34 point scale). Patients randomized to finasteride tablets USP who remained on therapy for 4 years had a mean (±1 SD) decrease in symptom score of 3.3 (± 5.8) points compared with 1.3 (± 5.6) points in the placebo group. (See Figure 1.) A statistically significant improvement in symptom score was evident at 1 year in patients treated with finasteride tablets USP vs. placebo (–2.3 vs –1.6), and this improvement continued through Year 4.
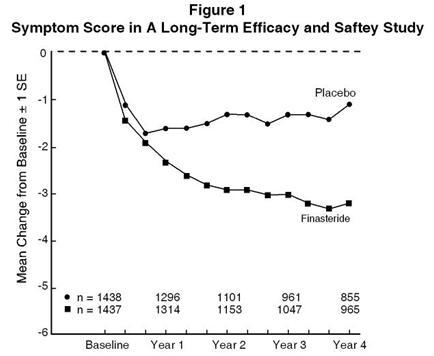
Results seen in earlier studies were comparable to those seen in a long-term efficacy and safety study. Although an early improvement in urinary symptoms was seen in some patients, a therapeutic trial of at least 6 months was generally necessary to assess whether a beneficial response in symptom relief had been achieved. The improvement in BPH symptoms was seen during the first year and maintained throughout an additional 5 years of open extension studies.
Effect on the Need for Surgery
In a long-term efficacy and safety study, efficacy was also assessed by evaluating treatment failures. Treatment failure was prospectively defined as BPH-related urological events or clinical deterioration, lack of improvement and/or the need for alternative therapy. BPH-related urological events were defined as urological surgical intervention. Complete event information was available for 92% of the patients. The following table summarizes the results.
Table 1 All Treatment Failures in A Long-Term Efficacy and Safety Study Patients (%) * Event Placebo
N=1503Finasteride
N=1513Relative
Risk**95% CI P
Value*** Patients with multiple events may be counted more than once for each type of event ** Hazard ratio based on log rank test All Treatment Failures 37.1 26.2 0.68 (0.57 to 0.79) <0.001 Surgical Interventions
for BPH10.1 4.6 0.45 (0.32 to 0.63) <0.001 Two consecutive
symptom scores
≥209.2 6.7 Bladder Stone 0.4 0.5 Incontinence 2.1 1.7 Renal Failure 0.5 0.6 UTI 5.7 4.9 Discontinuation due
to worsening of BPH,
lack of improvement,
or to receive other
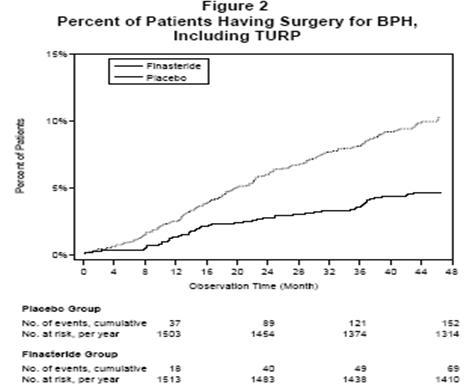
medical treatment21.8 13.3 Compared with placebo, finasteride tablets USP was associated with a significantly lower need for BPH-related surgery. Compared with placebo, finasteride tablets USP was associated with a significantly lower risk for surgery [10.1% for placebo vs 4.6% for finasteride tablets USP; 55% reduction in risk, 95% CI: (37 to 68%)]; see Figure 2.
Effect on Maximum Urinary Flow Rate
In the patients in a long-term efficacy and safety study who remained on therapy for the duration of the study and had evaluable urinary flow data, finasteride tablets USP increased maximum urinary flow rate by 1.9 mL/sec compared with 0.2 mL/sec in the placebo group.
There was a clear difference between treatment groups in maximum urinary flow rate in favor of finasteride tablets USP by month 4 (1.0 vs 0.3 mL/sec) which was maintained throughout the study. In the earlier 1-year studies, increase in maximum urinary flow rate was comparable to a long-term efficacy and safety study and was maintained through the first year and throughout an additional 5 years of open extension studies.
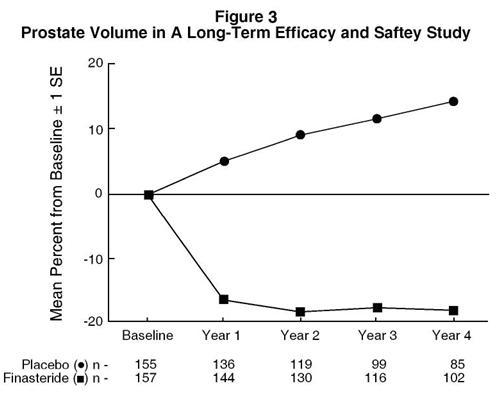
Effect on Prostate Volume
In a long-term efficacy and safety study, prostate volume was assessed yearly by magnetic resonance imaging (MRI) in a subset of patients. In patients treated with finasteride tablets USP who remained on therapy, prostate volume was reduced compared with both baseline and placebo throughout the 4-year study. Finasteride tablets USP decreased prostate volume by 17.9% (from 55.9 mL at baseline to 45.8 mL at 4 years) compared with an increase of 14.1% (from 51.3 mL to 58.5 mL) in the placebo group (p<0.001). (See Figure 3.)
Results seen in earlier studies were comparable to those seen in a long-term efficacy and safety study. Mean prostate volume at baseline ranged between 40 to 50 mL. The reduction in prostate volume was seen during the first year and maintained throughout an additional five years of open extension studies.
Prostate Volume as a Predictor of Therapeutic Response
A meta-analysis combining 1-year data from seven double-blind, placebo-controlled studies of similar design, including 4491 patients with symptomatic BPH, demonstrated that, in patients treated with finasteride tablets USP, the magnitude of symptom response and degree of improvement in maximum urinary flow rate were greater in patients with an enlarged prostate at baseline.
Summary of Clinical Studies
The data from these studies, showing improvement in BPH-related symptoms, reduction in treatment failure (BPH-related urological events), increased maximum urinary flow rates, and decreasing prostate volume, suggest that finasteride tablets USP arrests the disease process of BPH in men with an enlarged prostate.
- INDICATIONS AND USAGE
-
CONTRAINDICATIONS
Finasteride tablets USP are contraindicated in the following:
Hypersensitivity to any component of this medication.
Pregnancy. Finasteride use is contraindicated in women when they are or may potentially be pregnant. Because of the ability of Type II 5α-reductase inhibitors to inhibit the conversion of testosterone to DHT, finasteride may cause abnormalities of the external genitalia of a male fetus of a pregnant woman who receives finasteride. If this drug is used during pregnancy, or if pregnancy occurs while taking this drug, the pregnant woman should be apprised of the potential hazard to the male fetus. (See also WARNINGS, EXPOSURE OF WOMEN — RISK TO MALE FETUS and PRECAUTIONS, Information for Patients and Pregnancy.) In female rats, low doses of finasteride administered during pregnancy have produced abnormalities of the external genitalia in male offspring.
-
WARNINGS
Finasteride tablets USP are not indicated for use in pediatric patients (see PRECAUTIONS, Pediatric Use) or women (see also WARNINGS, EXPOSURE OF WOMEN — RISK TO MALE FETUS; PRECAUTIONS, Information for Patients and Pregnancy; and HOW SUPPLIED).
EXPOSURE OF WOMEN — RISK TO MALE FETUS
Women should not handle crushed or broken finasteride tablets USP when they are pregnant or may potentially be pregnant because of the possibility of absorption of finasteride and the subsequent potential risk to a male fetus. Finasteride tablets USP are coated and will prevent contact with the active ingredient during normal handling, provided that the tablets have not been broken or crushed. (See CONTRAINDICATIONS; PRECAUTIONS, Information for Patients and Pregnancy; and HOW SUPPLIED.)
-
PRECAUTIONS
General
Prior to initiating therapy with finasteride tablets USP, appropriate evaluation should be performed to identify other conditions such as infection, prostate cancer, stricture disease, hypotonic bladder or other neurogenic disorders that might mimic BPH.
Patients with large residual urinary volume and/or severely diminished urinary flow should be carefully monitored for obstructive uropathy. These patients may not be candidates for finasteride therapy.
Caution should be used in the administration of finasteride tablets USP in those patients with liver function abnormalities, as finasteride is metabolized extensively in the liver.
Effects on PSA and Prostate Cancer Detection
No clinical benefit has been demonstrated in patients with prostate cancer treated with finasteride tablets USP. Patients with BPH and elevated PSA were monitored in controlled clinical studies with serial PSAs and prostate biopsies. In these BPH studies, finasteride tablets USP did not appear to alter the rate of prostate cancer detection, and the overall incidence of prostate cancer was not significantly different in patients treated with finasteride tablets USP or placebo.
Finasteride tablets USP causes a decrease in serum PSA levels by approximately 50% in patients with BPH. This decrease is predictable over the entire range of PSA values, although it may vary in individual patients. Analysis of PSA data from over 3000 patients in a long-term efficacy and safety study confirmed that in typical patients treated with finasteride tablets USP for six months or more, PSA values should be doubled for comparison with normal ranges in untreated men. This adjustment preserves the sensitivity and specificity of the PSA assay and maintains its ability to detect prostate cancer. Finasteride tablets USP may also cause decreases in serum PSA in the presence of prostate cancer.
Any confirmed increases in PSA levels from nadir while on finasteride tablets USP may signal the presence of prostate cancer and should be carefully evaluated, even if these values are still within the normal range for men not taking a 5α-reductase inhibitor. Non compliance with finasteride tablets USP therapy may also affect PSA test results.
Percent free PSA (free to total PSA ratio) is not significantly decreased by finasteride tablets USP. The ratio of free to total PSA remains constant even under the influence of finasteride tablets USP. If clinicians elect to use percent free PSA as an aid in the detection of prostate cancer in men undergoing finasteride therapy, no adjustment to its value appears necessary.
Information for Patients
Women should not handle crushed or broken finasteride tablets USP when they are pregnant or may potentially be pregnant because of the possibility of absorption of finasteride and the subsequent potential risk to the male fetus (see CONTRAINDICATIONS; WARNINGS, EXPOSURE OF WOMEN — RISK TO MALE FETUS; PRECAUTIONS, Pregnancy and HOW SUPPLIED).
Physicians should inform patients that the volume of ejaculate may be decreased in some patients during treatment with finasteride tablets USP. This decrease does not appear to interfere with normal sexual function. However, impotence and decreased libido may occur in patients treated with finasteride tablets USP (see ADVERSE REACTIONS).
Physicians should instruct their patients to promptly report any changes in their breasts such as lumps, pain or nipple discharge. Breast changes including breast enlargement, tenderness and neoplasm have been reported (see ADVERSE REACTIONS).
Physicians should instruct their patients to read the patient package insert before starting therapy with finasteride tablets USP and to reread it each time the prescription is renewed so that they are aware of current information for patients regarding finasteride tablets USP.
Drug/Laboratory Test Interactions
In patients with BPH, finasteride tablets USP has no effect on circulating levels of cortisol, estradiol, prolactin, thyroid-stimulating hormone, or thyroxine. No clinically meaningful effect was observed on the plasma lipid profile (i.e., total cholesterol, low density lipoproteins, high density lipoproteins and triglycerides) or bone mineral density. Increases of about 10% were observed in luteinizing hormone (LH) and follicle-stimulating hormone (FSH) in patients receiving finasteride tablets USP, but levels remained within the normal range. In healthy volunteers, treatment with finasteride tablets USP did not alter the response of LH and FSH to gonadotropin-releasing hormone indicating that the hypothalamic-pituitary-testicular axis was not affected.
Treatment with finasteride tablets USP for 24 weeks to evaluate semen parameters in healthy male volunteers revealed no clinically meaningful effects on sperm concentration, mobility, morphology, or pH. A 0.6 mL (22.1%) median decrease in ejaculate volume with a concomitant reduction in total sperm per ejaculate was observed. These parameters remained within the normal range and were reversible upon discontinuation of therapy with an average time to return to baseline of 84 weeks.
Drug Interactions
No drug interactions of clinical importance have been identified. Finasteride does not appear to affect the cytochrome P450-linked drug metabolizing enzyme system. Compounds that have been tested in man have included antipyrine, digoxin, propranolol, theophylline, and warfarin and no clinically meaningful interactions were found.
Other Concomitant Therapy: Although specific interaction studies were not performed, finasteride tablets USP was concomitantly used in clinical studies with acetaminophen, acetylsalicylic acid, α-blockers, angiotensin-converting enzyme (ACE) inhibitors, analgesics, anti-convulsants, beta-adrenergic blocking agents, diuretics, calcium channel blockers, cardiac nitrates, HMG-CoA reductase inhibitors, nonsteroidal anti-inflammatory drugs (NSAIDs), benzodiazepines, H2 antagonists and quinolone anti-infectives without evidence of clinically significant adverse interactions.
Carcinogenesis, Mutagenesis, Impairment of Fertility
No evidence of a tumorigenic effect was observed in a 24-month study in Sprague-Dawley rats receiving doses of finasteride up to 160 mg/kg/day in males and 320 mg/kg/day in females. These doses produced respective systemic exposure in rats of 111 and 274 times those observed in man receiving the recommended human dose of 5 mg/day. All exposure calculations were based on calculated AUC (0 to 24 hr) for animals and mean AUC (0 to 24 hr) for man (0.4 mcg•hr/mL).
In a 19-month carcinogenicity study in CD-1 mice, a statistically significant (p≤0.05) increase in the incidence of testicular Leydig cell adenomas was observed at a dose of 250 mg/kg/day (228 times the human exposure). In mice at a dose of 25 mg/kg/day (23 times the human exposure, estimated) and in rats at a dose of ≥40 mg/kg/day (39 times the human exposure) an increase in the incidence of Leydig cell hyperplasia was observed. A positive correlation between the proliferative changes in the Leydig cells and an increase in serum LH levels (2- to 3-fold above control) has been demonstrated in both rodent species treated with high doses of finasteride. No drug-related Leydig cell changes were seen in either rats or dogs treated with finasteride for 1 year at doses of 20 mg/kg/day and 45 mg/kg/day (30 and 350 times, respectively, the human exposure) or in mice treated for 19 months at a dose of 2.5 mg/kg/day (2.3 times the human exposure, estimated).
No evidence of mutagenicity was observed in an in vitro bacterial mutagenesis assay, a mammalian cell mutagenesis assay, or in an in vitro alkaline elution assay. In an in vitro chromosome aberration assay, using Chinese hamster ovary cells, there was a slight increase in chromosome aberrations. These concentrations correspond to 4000 to 5000 times the peak plasma levels in man given a total dose of 5 mg. In an in vivo chromosome aberration assay in mice, no treatment-related increase in chromosome aberration was observed with finasteride at the maximum tolerated dose of 250 mg/kg/day (228 times the human exposure) as determined in the carcinogenicity studies.
In sexually mature male rabbits treated with finasteride at 80 mg/kg/day (543 times the human exposure) for up to 12 weeks, no effect on fertility, sperm count, or ejaculate volume was seen. In sexually mature male rats treated with 80 mg/kg/day of finasteride (61 times the human exposure), there were no significant effects on fertility after 6 or 12 weeks of treatment; however, when treatment was continued for up to 24 or 30 weeks, there was an apparent decrease in fertility, fecundity and an associated significant decrease in the weights of the seminal vesicles and prostate. All these effects were reversible within 6 weeks of discontinuation of treatment. No drug-related effect on testes or on mating performance has been seen in rats or rabbits. This decrease in fertility in finasteride-treated rats is secondary to its effect on accessory sex organs (prostate and seminal vesicles) resulting in failure to form a seminal plug. The seminal plug is essential for normal fertility in rats and is not relevant in man.
Pregnancy
Teratogenic Effects:Pregnancy Category X
See CONTRAINDICATIONS.
Finasteride tablets USP are not indicated for use in women.
Administration of finasteride to pregnant rats at doses ranging from 100 mcg/kg/day to 100 mg/kg/day (1 to 1000 times the recommended human dose of 5 mg/day) resulted in dose-dependent development of hypospadias in 3.6 to 100% of male offspring. Pregnant rats produced male offspring with decreased prostatic and seminal vesicular weights, delayed preputial separation and transient nipple development when given finasteride at ≥30 mcg/kg/day (≥3/10 of the recommended human dose of 5 mg/day) and decreased anogenital distance when given finasteride at ≥3 mcg/kg/day (≥3/100 of the recommended human dose of 5 mg/day). The critical period during which these effects can be induced in male rats has been defined to be days 16 to 17 of gestation. The changes described above are expected pharmacological effects of drugs belonging to the class of Type II 5α-reductase inhibitors and are similar to those reported in male infants with a genetic deficiency of Type II 5α-reductase. No abnormalities were observed in female offspring exposed to any dose of finasteride in utero.
No developmental abnormalities have been observed in first filial generation (F1) male or female offspring resulting from mating finasteride-treated male rats (80 mg/kg/day; 61 times the human exposure) with untreated females. Administration of finasteride at 3 mg/kg/day (30 times the recommended human dose of 5 mg/day) during the late gestation and lactation period resulted in slightly decreased fertility in F1 male offspring. No effects were seen in female offspring. No evidence of malformations has been observed in rabbit fetuses exposed to finasteride in utero from days 6 to 18 of gestation at doses up to 100 mg/kg/day (1000 times the recommended human dose of 5 mg/day). However, effects on male genitalia would not be expected since the rabbits were not exposed during the critical period of genital system development.
The in utero effects of finasteride exposure during the period of embryonic and fetal development were evaluated in the rhesus monkey (gestation days 20 to 100), a species more predictive of human development than rats or rabbits. Intravenous administration of finasteride to pregnant monkeys at doses as high as 800 ng/day (at least 60 to 120 times the highest estimated exposure of pregnant women to finasteride from semen of men taking 5 mg/day) resulted in no abnormalities in male fetuses. In confirmation of the relevance of the rhesus model for human fetal development, oral administration of a dose of finasteride (2 mg/kg/day; 20 times the recommended human dose of 5 mg/day or approximately 1 to 2 million times the highest estimated exposure to finasteride from semen of men taking 5 mg/day) to pregnant monkeys resulted in external genital abnormalities in male fetuses. No other abnormalities were observed in male fetuses and no finasteride-related abnormalities were observed in female fetuses at any dose.
Nursing Mothers
Finasteride tablets USP are not indicated for use in women.
It is not known whether finasteride is excreted in human milk.
Pediatric Use
Finasteride tablets USP are not indicated for use in pediatric patients.
Safety and effectiveness in pediatric patients have not been established.
Geriatric Use
Of the total number of subjects included in a long-term efficacy and safety study, 1480 and 105 subjects were 65 and over and 75 and over, respectively. No overall differences in safety or effectiveness were observed between these subjects and younger subjects, and other reported clinical experience has not identified differences in responses between the elderly and younger patients. No dosage adjustment is necessary in the elderly (see CLINICAL PHARMACOLOGY, Pharmacokinetics and Clinical Studies).
-
ADVERSE REACTIONS
Finasteride tablets USP are generally well tolerated; adverse reactions usually have been mild and transient.
4-Year Placebo-Controlled Study
In a long-term efficacy and safety study, 1524 patients treated with finasteride tablets USP and 1516 patients treated with placebo were evaluated for safety over a period of 4 years. The most frequently reported adverse reactions were related to sexual function. 3.7% (57 patients) treated with finasteride tablets USP and 2.1% (32 patients) treated with placebo discontinued therapy as a result of adverse reactions related to sexual function, which are the most frequently reported adverse reactions.
Table 2 presents the only clinical adverse reactions considered possibly, probably or definitely drug related by the investigator, for which the incidence on finasteride tablets USP was ≥1% and greater than placebo over the 4 years of the study. In years 2 to 4 of the study, there was no significant difference between treatment groups in the incidences of impotence, decreased libido and ejaculation disorder.
TABLE 2 Drug-Related Adverse Experiences
Year 1(%)
Years 2, 3 and 4* (%)Finasteride Placebo Finasteride Placebo *Combined Years 2 to 4 N = 1524 and 1516, finasteride vs placebo, respectively Impotence 8.1 3.7 5.1 5.1 Decreased Libido 6.4 3.4 2.6 2.6 Decreased Volume of Ejaculate 3.7 0.8 1.5 0.5 Ejaculation Disorder 0.8 0.1 0.2 0.1 Breast Enlargement 0.5 0.1 1.8 1.1 Breast Tenderness 0.4 0.1 0.7 0.3 Rash 0.5 0.2 0.5 0.1 Phase III Studies and 5-Year Open Extensions
The adverse experience profile in the 1-year, placebo-controlled, Phase III studies, the 5-year open extensions, and a long-term efficacy and safety study were similar.
Long-Term Data
There is no evidence of increased adverse experiences with increased duration of treatment with finasteride tablets USP. New reports of drug-related sexual adverse experiences decreased with duration of therapy.
During the 4- to 6-year placebo- and comparator-controlled study that enrolled 3047 men, there were 4 cases of breast cancer in men treated with finasteride but no cases in men not treated with finasteride. During the 4-year, placebo-controlled long-term efficacy and safety study that enrolled 3040 men, there were 2 cases of breast cancer in placebo-treated men, but no cases were reported in men treated with finasteride. The relationship between long-term use of finasteride and male breast neoplasia is currently unknown.
In a 7-year placebo-controlled trial that enrolled 18,882 healthy men, 9060 had prostate needle biopsy data available for analysis. In the finasteride tablets USP group, 280 (6.4%) men had prostate cancer with Gleason scores of 7 to 10 detected on needle biopsy vs. 237 (5.1%) men in the placebo group. Of the total cases of prostate cancer diagnosed in this study, approximately 98% were classified as intracapsular (stage T1 or T2). The clinical significance of these findings is unknown. This information from the literature (Thompson IM, Goodman PJ, Tangen CM, et al. The influence of finasteride on the development of prostate cancer. N Engl J Med 2003;349:213-22) is provided for consideration by physicians when finasteride tablets USP are used as indicated (see INDICATIONS AND USAGE). Finasteride tablets USP are not approved to reduce the risk of developing prostate cancer.
Post-Marketing Experience
The following additional adverse effects have been reported in post-marketing experience:
– hypersensitivity reactions, including pruritus, urticaria, and swelling of the lips and face
– testicular pain.
-
OVERDOSAGE
Patients have received single doses of finasteride tablets USP up to 400 mg and multiple doses of finasteride tablets USP up to 80 mg/day for three months without adverse effects. Until further experience is obtained, no specific treatment for an overdose with finasteride tablets USP can be recommended.
Significant lethality was observed in male and female mice at single oral doses of 1500 mg/m2 (500 mg/kg) and in female and male rats at single oral doses of 2360 mg/m2 (400 mg/kg) and 5900 mg/m2 (1000 mg/kg), respectively.
-
DOSAGE AND ADMINISTRATION
The recommended dose is 5 mg orally once a day.
Finasteride tablets USP may be administered with or without meals.
No dosage adjustment is necessary for patients with renal impairment or for the elderly (see CLINICAL PHARMACOLOGY, Pharmacokinetics).
-
HOW SUPPLIED
Finasteride tablets USP, 5 mg are blue color, round film coated tablets, debossed with ‘H’ on one side ‘37’ on other side, They are supplied as follows:
NDC 31722-525-30 bottles of 30
NDC 31722-525-01 bottles of 100
NDC 31722-525-10 bottles of 1000
NDC 31722-525-90 bottles of 90
NDC 31722-525-05 bottles of 500Storage and Handling
Store at 20° to 25°C (68° to 77°F) [see USP Controlled Room Temperature]. Protect from light and keep container tightly closed.
Women should not handle crushed or broken finasteride tablets USP when they are pregnant or may potentially be pregnant because of the possibility of absorption of finasteride and the subsequent potential risk to a male fetus (see WARNINGS, EXPOSURE OF WOMEN - RISK TO MALE FETUS, and PRECAUTIONS, Information for Patients and Pregnancy).
Manufactured for:
Camber Pharmaceuticals, Inc.
Piscataway, NJ 08854By: Hetero Drugs Limited 2007536-01
Jeedimetla, Hyderabad- 500 055, IndiaFinasteride Tablets USP
Patient Information about
Finasteride Tablets USP
(fin-AS-tur-eyed)Finasteride tablets USP are for use by men only.
Please read this leaflet before you start taking finasteride tablets USP. Also, read it each time you renew your prescription, just in case anything has changed. Remember, this leaflet does not take the place of careful discussions with your doctor. You and your doctor should discuss finasteride tablets USP when you start taking your medication and at regular checkups.
What are finasteride tablets USP?
Finasteride tablets USP is a medication used to treat symptoms of benign prostatic hyperplasia (BPH) in men with an enlarged prostate. Finasteride tablets USP may also be used to reduce the need for surgery related to BPH in men with an enlarged prostate.
Who should NOT take finasteride tablets USP?
Finasteride tablets USP are for use by MEN only.
Do Not Take finasteride tablets USP if you are:
- a woman who is pregnant or may potentially be pregnant. Finasteride tablets USP may harm your unborn baby. Do not touch or handle crushed or broken finasteride tablets USP (see “A warning about finasteride tablets USP and pregnancy”).
- allergic to finasteride or any of the ingredients in finasteride tablets USP. See the end of this leaflet for a complete list of ingredients in finasteride tablets USP.
A warning about finasteride tablets USP and pregnancy.
Women who are or may potentially be pregnant must not use finasteride tablets USP. They should also not handle crushed or broken tablets of finasteride tablets USP. finasteride tablets USP are coated and will prevent contact with the active ingredient during normal handling, provided that the tablets are not broken or crushed.
If a woman who is pregnant with a male baby absorbs the active ingredient in finasteride tablets USP after oral use or through the skin, it may cause the male baby to be born with abnormalities of the sex organs. If a woman who is pregnant comes into contact with the active ingredient in finasteride tablets USP, a doctor should be consulted.
How should I take finasteride tablets USP?
Follow your doctor's instruction.
- Take one tablet by mouth each day. To avoid forgetting to take finasteride tablets USP, you can take it at the same time every day.
- If you forget to take finasteride tablets USP, do not take an extra tablet. Just take the next tablet as usual.
- You may take finasteride tablets USP with or without food.
- Do not share finasteride tablets USP with anyone else; it was prescribed only for you.
What are the possible side effects of finasteride tablets USP?
The most common side effects of finasteride tablets USP include:
- trouble getting or keeping an erection (impotence)
- decrease in sex drive
- decreased volume of ejaculate
- ejaculation disorders
- enlarged or painful breast. You should promptly report to your doctor any changes in your breasts such as lumps, pain or nipple discharge.
Allergic reactions: Call your doctor if you get any signs of an allergic reaction while taking finasteride tablets USP, including rash, itching, hives, and swelling of the lips and face.
Testicular pain: Rarely, some men may have testicular pain while taking finasteride tablets USP.
You should discuss side effects with your doctor before taking finasteride tablets USP and anytime you think you are having a side effect. These are not all the possible side effects with finasteride tablets USP. For more information, ask your doctor or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at: 1-800-FDA-1088.
What you need to know while taking finasteride tablets USP
- You should see your doctor regularly while taking finasteride tablets USP. Follow your doctor's advice about when to have these checkups.
- Checking for prostate cancer. Your doctor has prescribed finasteride tablets USP for BPH and not for treatment of prostate cancer — but a man can have BPH and prostate cancer at the same time. Checking for prostate cancer should continue while you take finasteride tablets USP.
- About Prostate-Specific Antigen (PSA). Your doctor may have done a blood test called PSA for the screening of prostate cancer. Because finasteride tablets USP decreases PSA levels, you should tell your doctor(s) that you are taking finasteride tablets USP. Changes in PSA levels will need to be carefully evaluated by your doctor(s). Any increase in follow-up PSA levels from their lowest point should be carefully evaluated, even if the test results are still within the normal range. You should also tell your doctor if you have not been taking finasteride tablets USP as prescribed because this may affect the PSA test results. For more information, talk to your doctor.
How should I store finasteride tablets USP?
- Store finasteride tablets USP in a dry place at room temperature.
- Keep finasteride tablets USP in the original container and keep the container closed.
Finasteride tablets USP tablets are coated and will prevent contact with the active ingredient during normal handling, provided that the tablets are not broken or crushed.
Keep finasteride tablets USP and all medications out of the reach of children.
Do not give your finasteride tablets USP to anyone else. It has been prescribed only for you.
What are the ingredients in finasteride tablets USP?
Active ingredients: finasteride
Inactive ingredients: lactose monohydrate, microcrystalline cellulose, pregelatinized starch, sodium starch glycolate, docusate sodium, magnesium stearate, opadry blue (FD&C blue # 2 aluminum lake, hypromellose, talc, titanium dioxide, yellow iron oxide).
What is BPH?
BPH is an enlargement of the prostate gland. The prostate is located below the bladder. As the prostate enlarges, it may slowly restrict the flow of urine. This can lead to symptoms such as:
- a weak or interrupted urinary stream
- a feeling that you cannot empty your bladder completely
- a feeling of delay or hesitation when you start to urinate
- a need to urinate often, especially at night
- a feeling that you must urinate right away.
In some men, BPH can lead to serious problems, including urinary tract infections, as well as the need for surgery.
What finasteride tablets USP does
Finasteride tablets USP lowers levels of a hormone called DHT (dihydrotestosterone), which is a cause of prostate growth. Lowering DHT leads to shrinkage of the enlarged prostate gland in most men. This can lead to gradual improvement in urine flow and symptoms over the next several months. Finasteride tablets USP will help reduce the need for surgery related to an enlarged prostate. However, since each case of BPH is different, you should know that:
- Even though the prostate shrinks, you may NOT notice an improvement in urine flow or symptoms.
- You may need to take finasteride tablets USP for six (6) months or more to see whether it improves your symptoms.
- Therapy with finasteride tablets USP may reduce the need for surgery for an enlarged prostate.
Manufactured for:
Camber Pharmaceuticals, Inc.
Piscataway, NJ 08854By: Hetero Drugs Limited
Jeedimetla, Hyderabad- 500 055, India - PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
FINASTERIDE
finasteride tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:31722-525 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength FINASTERIDE (UNII: 57GNO57U7G) (FINASTERIDE - UNII:57GNO57U7G) FINASTERIDE 5 mg Inactive Ingredients Ingredient Name Strength LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) CELLULOSE, MICROCRYSTALLINE (UNII: OP1R32D61U) STARCH, CORN (UNII: O8232NY3SJ) SODIUM STARCH GLYCOLATE TYPE A POTATO (UNII: 5856J3G2A2) DOCUSATE SODIUM (UNII: F05Q2T2JA0) MAGNESIUM STEARATE (UNII: 70097M6I30) FD&C BLUE NO. 2 (UNII: L06K8R7DQK) ALUMINUM OXIDE (UNII: LMI26O6933) HYPROMELLOSES (UNII: 3NXW29V3WO) TALC (UNII: 7SEV7J4R1U) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) FERRIC OXIDE YELLOW (UNII: EX438O2MRT) Product Characteristics Color BLUE Score no score Shape ROUND Size 3mm Flavor Imprint Code H;37 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:31722-525-30 12 in 1 CASE 1 30 in 1 BOTTLE 2 NDC:31722-525-01 100 in 1 BOTTLE 3 NDC:31722-525-10 1000 in 1 BOTTLE 4 NDC:31722-525-90 12 in 1 CASE 4 90 in 1 BOTTLE 5 NDC:31722-525-05 500 in 1 BOTTLE Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA090061 08/01/2010 Labeler - Camber Pharmaceuticals Inc. (826774775) Establishment Name Address ID/FEI Business Operations Hetero Drug LTD 676162024 MANUFACTURE, ANALYSIS