Label: PROQUAD- measles, mumps, rubella and varicella virus vaccine live injection, powder, lyophilized, for suspension
- NDC Code(s): 0006-4171-00, 0006-4171-01
- Packager: Merck Sharp & Dohme LLC
- Category: VACCINE LABEL
- DEA Schedule: None
- Marketing Status: Biologic Licensing Application
Drug Label Information
Updated August 21, 2023
If you are a consumer or patient please visit this version.
- Download DRUG LABEL INFO: PDF XML
- Official Label (Printer Friendly)
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use ProQuad safely and effectively. See full prescribing information for ProQuad.
ProQuad®
Measles, Mumps, Rubella and Varicella Virus Vaccine Live
Suspension for intramuscular or subcutaneous injection
Initial U.S. Approval: 2005RECENT MAJOR CHANGES
INDICATIONS AND USAGE
ProQuad is a vaccine indicated for active immunization for the prevention of measles, mumps, rubella, and varicella in children 12 months through 12 years of age. (1)
DOSAGE AND ADMINISTRATION
DOSAGE FORMS AND STRENGTHS
CONTRAINDICATIONS
WARNINGS AND PRECAUTIONS
- Administration of ProQuad (dose 1) to children 12 to 23 months old who have not been previously vaccinated against measles, mumps, rubella, or varicella, nor had a history of the wild-type infections, is associated with higher rates of fever and febrile seizures at 5 to 12 days after vaccination when compared to children vaccinated with M-M-R® II and VARIVAX® administered separately. Exercise caution when administering ProQuad to persons with an individual or family history of febrile seizures. (5.1, 6.1, 6.3)
- Use caution when administering ProQuad to children with anaphylaxis or immediate hypersensitivity following egg ingestion. (5.2)
- Use caution when administering ProQuad to children with thrombocytopenia. (5.3)
- Evaluate individuals for immune competence prior to administration of ProQuad if there is a family history of congenital or hereditary immunodeficiency. (5.4)
- Avoid close contact with high-risk individuals susceptible to varicella because of possible transmission of varicella vaccine virus. (5.6)
- Immune Globulins (IG) and other blood products should not be given concurrently with ProQuad. (5.7, 7.1)
- Avoid using salicylates for 6 weeks after vaccination with ProQuad. (5.8, 7.2, 17)
ADVERSE REACTIONS
- The most frequent vaccine-related adverse events reported in ≥5% of subjects vaccinated with ProQuad were:
- injection-site reactions (pain/tenderness/soreness, erythema, and swelling)
- fever
- irritability. (6.1)
- Systemic vaccine-related adverse events that were reported at a significantly greater rate in recipients of ProQuad than in recipients of the component vaccines administered concomitantly were:
- fever
- measles-like rash. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Merck Sharp & Dohme LLC at 1-877-888-4231 or VAERS at 1-800-822-7967 or www.vaers.hhs.gov .
DRUG INTERACTIONS
- Administration of immune globulins and other blood products concurrently with ProQuad vaccine may interfere with the expected immune response. (7.1)
- ProQuad vaccination may result in a temporary depression of purified protein derivative (PPD) tuberculin skin sensitivity. (7.4)
- ProQuad may be administered concomitantly with Haemophilus influenzae type b conjugate vaccine and/or hepatitis B vaccine at separate injection sites. (7.5)
- ProQuad may be administered concomitantly with pneumococcal 7-valent conjugate vaccine and/or hepatitis A vaccine (inactivated) at separate injection sites. (7.5)
USE IN SPECIFIC POPULATIONS
Pregnancy: Do not administer ProQuad to females who are pregnant. Pregnancy should be avoided for 3 months following vaccination with ProQuad. (4.5, 8.1, 17)
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 8/2023
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Dose and Schedule
2.2 Preparation for Administration
2.3 Administration
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
4.1 Hypersensitivity
4.2 Immunosuppression
4.3 Moderate or Severe Febrile Illness
4.4 Active Untreated Tuberculosis
4.5 Pregnancy
5 WARNINGS AND PRECAUTIONS
5.1 Fever and Febrile Seizures
5.2 Hypersensitivity to Eggs
5.3 Thrombocytopenia
5.4 Family History of Immunodeficiency
5.5 Use in HIV-Infected Individuals
5.6 Risk of Vaccine Virus Transmission
5.7 Immune Globulins and Transfusions
5.8 Salicylate Therapy
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Post-Marketing Experience
6.3 Post-Marketing Observational Safety Surveillance Study
7 DRUG INTERACTIONS
7.1 Immune Globulins and Transfusions
7.2 Salicylates
7.3 Corticosteroids and Immunosuppressive Drugs
7.4 Drug/Laboratory Test Interactions
7.5 Use with Other Vaccines
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.6 Persistence of Antibody Responses after Vaccination
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
15 REFERENCES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- *
- Sections or subsections omitted from the full prescribing information are not listed.
- 1 INDICATIONS AND USAGE
-
2 DOSAGE AND ADMINISTRATION
For Intramuscular or Subcutaneous administration only
2.1 Dose and Schedule
A single dose of ProQuad is approximately 0.5 mL.
The first dose is administered at 12 to 15 months of age but may be given anytime through 12 years of age.
The second dose is administered at 4 to 6 years of age.
At least 1 month should elapse between a dose of a measles-containing vaccine and a dose of ProQuad. At least 3 months should elapse between a dose of varicella-containing vaccine and ProQuad.
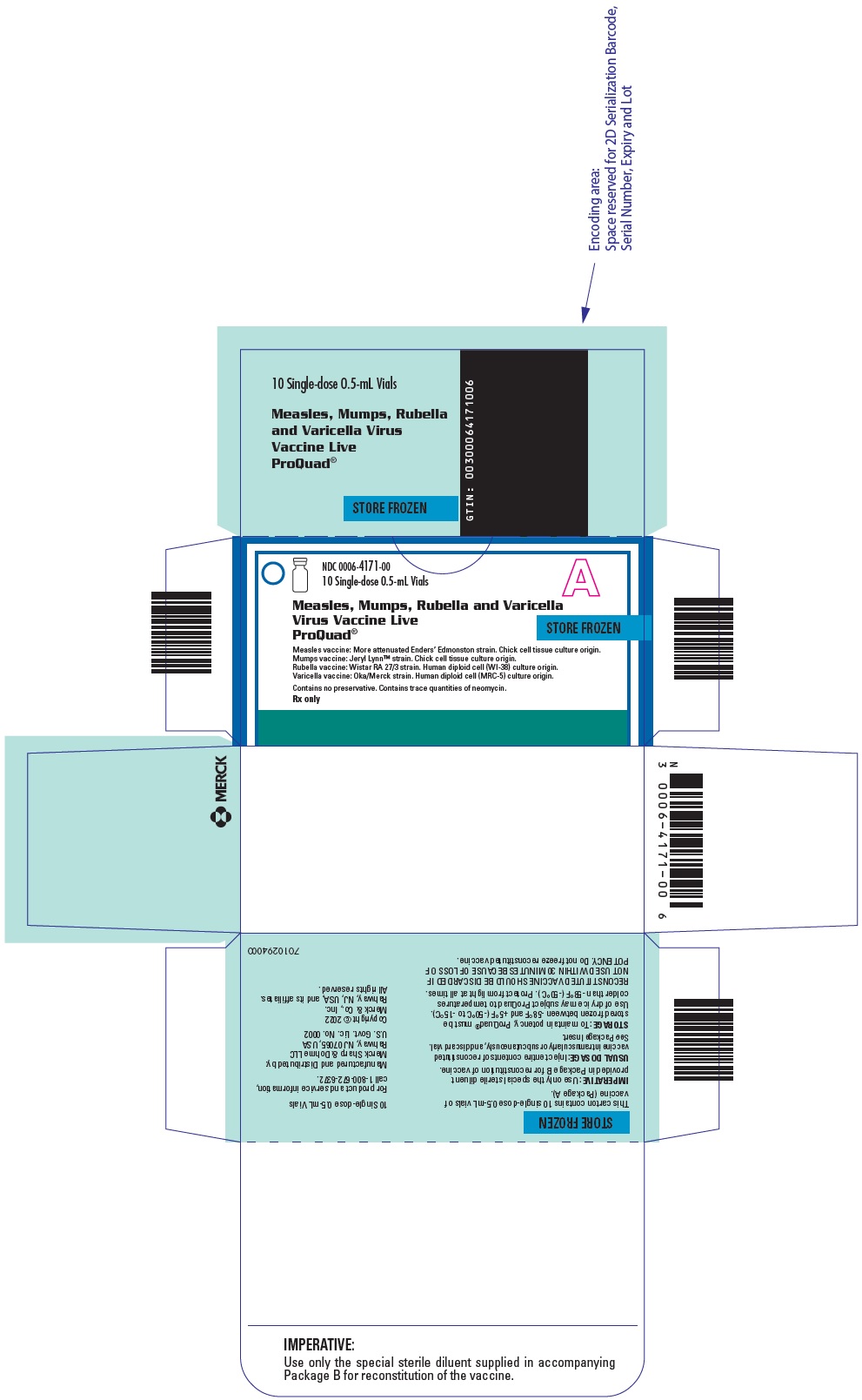
2.2 Preparation for Administration
The sterile diluent for ProQuad is provided in either a vial or prefilled syringe.
Sterile Diluent Vial
Use a sterile syringe free of preservatives, antiseptics, and detergents for each injection and/or reconstitution of the vaccine because these substances may inactivate the live virus vaccine. To reconstitute, use the sterile diluent vial supplied with ProQuad. The sterile diluent does not contain preservatives or other antiviral substances which might inactivate the vaccine viruses.
To reconstitute the vaccine, withdraw the entire volume of the supplied sterile diluent from the vial and slowly inject into the lyophilized vaccine vial. Gently agitate to dissolve completely. Discard if the lyophilized vaccine cannot be dissolved.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit. Visually inspect the vaccine before and after reconstitution prior to administration. Before reconstitution, the lyophilized vaccine is a white to pale yellow compact crystalline plug. ProQuad, when reconstituted, is a clear pale yellow to light pink liquid. Do not use the reconstituted vaccine if particulates are present or if it appears discolored.
Withdraw and administer the entire volume of the reconstituted vaccine.
Administer ProQuad immediately after reconstitution. If not used immediately, the reconstituted vaccine may be stored at room temperature, protected from light, for up to 30 minutes. Discard reconstituted vaccine if it is not used within 30 minutes.
Sterile Diluent Prefilled Syringe
To reconstitute, use the sterile diluent prefilled syringe supplied with the vaccine since it does not contain preservatives or other antiviral substances which might inactivate the vaccine viruses.
Attach a needle to the prefilled syringe.
Reconstitute the vaccine by slowly injecting the entire volume of sterile diluent contained in the prefilled syringe into the lyophilized vaccine vial. Gently agitate to dissolve completely. Discard if the lyophilized vaccine cannot be dissolved.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit. Visually inspect the vaccine before and after reconstitution prior to administration. Before reconstitution, the lyophilized vaccine is a white to pale yellow compact crystalline plug. ProQuad, when reconstituted, is a clear pale yellow to light pink liquid. Do not use the reconstituted vaccine if particulates are present or if it appears discolored.
Withdraw and administer the entire volume of the reconstituted vaccine.
Administer ProQuad immediately after reconstitution. If not used immediately, the reconstituted vaccine may be stored at room temperature, protected from light, for up to 30 minutes. Discard reconstituted vaccine if it is not used within 30 minutes.
-
3 DOSAGE FORMS AND STRENGTHS
ProQuad is a suspension for injection supplied as a single dose vial of lyophilized vaccine to be reconstituted using the accompanying sterile diluent [see Dosage and Administration (2.2) and How Supplied/Storage and Handling (16)]. A single dose after reconstitution is approximately 0.5 mL.
-
4 CONTRAINDICATIONS
4.1 Hypersensitivity
Do not administer ProQuad to individuals with a history of hypersensitivity to any component of the vaccine (including gelatin) {1} or to a previous dose of M-M-R II (Measles, Mumps, Rubella, Live), ProQuad or VARIVAX (Varicella Virus Vaccine Live) vaccine, or any other measles, mumps, and rubella or varicella-containing vaccine. Do not administer ProQuad to individuals with a history of anaphylaxis to neomycin [see Description (11)].
4.2 Immunosuppression
Do not administer ProQuad vaccine to individuals who are immunodeficient or immunosuppressed due to disease or medical therapy. Measles inclusion body encephalitis {2} (MIBE), pneumonitis {3} and death as a direct consequence of disseminated measles vaccine virus infection have been reported in immunocompromised individuals inadvertently vaccinated with measles-containing vaccine. In this population, disseminated mumps and rubella vaccine virus infection have also been reported. Disseminated varicella disease and extensive vaccine-associated rash have been reported in individuals who are immunosuppressed or immunodeficient who were inadvertently vaccinated with a varicella-containing vaccine {4}.
4.3 Moderate or Severe Febrile Illness
Do not administer ProQuad to individuals with an active febrile illness with fever >101.3°F (>38.5°C).
4.4 Active Untreated Tuberculosis
Do not administer ProQuad vaccine to individuals with active untreated tuberculosis (TB).
4.5 Pregnancy
Do not administer ProQuad to individuals who are pregnant or planning on becoming pregnant in the next 3 months [see Use in Specific Populations (8.1) and Patient Counseling Information (17)].
-
5 WARNINGS AND PRECAUTIONS
5.1 Fever and Febrile Seizures
Administration of ProQuad (dose 1) to children 12 to 23 months old who have not been previously vaccinated against measles, mumps, rubella, or varicella, nor had a history of the wild-type infections, is associated with higher rates of fever and febrile seizures at 5 to 12 days after vaccination when compared to children vaccinated with a first dose of M-M-R II and VARIVAX administered concomitantly [see Adverse Reactions (6.3)]. Exercise caution when administering ProQuad to persons with an individual or family history of febrile seizures.
5.2 Hypersensitivity to Eggs
Individuals with a history of anaphylactic, anaphylactoid, or other immediate reactions (e.g., hives, swelling of the mouth and throat, difficulty breathing, hypotension, or shock) subsequent to egg ingestion may be at an enhanced risk of immediate-type hypersensitivity reactions after receiving ProQuad vaccine. The potential risks and known benefits should be evaluated before considering vaccination in these individuals [see Contraindications (4.1)] {5}.
5.3 Thrombocytopenia
Transient thrombocytopenia has been reported within 4-6 weeks following vaccination with measles, mumps and rubella vaccine. Carefully evaluate the potential risk and benefit of vaccination in children with thrombocytopenia or in those who experienced thrombocytopenia after vaccination with a previous dose of a measles, mumps, and rubella-containing vaccine [see Adverse Reactions (6.2)] {6-8}.
5.4 Family History of Immunodeficiency
Vaccination should be deferred in individuals with a family history of congenital or hereditary immunodeficiency until the individual's immune status has been evaluated and the individual has been found to be immunocompetent.
5.5 Use in HIV-Infected Individuals
The Advisory Committee on Immunization Practices (ACIP) has recommendations on the use of varicella vaccine in HIV-infected individuals.
5.6 Risk of Vaccine Virus Transmission
Post-licensing experience suggests that transmission of varicella vaccine virus (Oka/Merck) resulting in varicella infection including disseminated disease may occur between vaccine recipients (who develop or do not develop a varicella-like rash) and contacts susceptible to varicella including healthy as well as high-risk individuals.
High-risk individuals susceptible to varicella include:
- Immunocompromised individuals;
- Pregnant women without documented positive history of varicella (chickenpox) or laboratory evidence of prior infection;
- Newborn infants of mothers without documented positive history of varicella or laboratory evidence of prior infection and all newborn infants born at <28 weeks gestation regardless of maternal varicella immunity.
Vaccine recipients should attempt to avoid, to the extent possible, close association with high-risk individuals susceptible to varicella for up to 6 weeks following vaccination. In circumstances where contact with high-risk individuals susceptible to varicella is unavoidable, the potential risk of transmission of the varicella vaccine virus should be weighed against the risk of acquiring and transmitting wild-type varicella virus.
Excretion of small amounts of the live, attenuated rubella virus from the nose or throat has occurred in the majority of susceptible individuals 7 to 28 days after vaccination. There is no confirmed evidence to indicate that such virus is transmitted to susceptible persons who are in contact with the vaccinated individuals. Consequently, transmission through close personal contact, while accepted as a theoretical possibility, is not regarded as a significant risk. However, transmission of the rubella vaccine virus to infants via breast milk has been documented [see Use in Specific Populations (8.2)].
There are no reports of transmission of the more attenuated Enders' Edmonston strain of measles virus or the Jeryl Lynn™ strain of mumps virus from vaccine recipients to susceptible contacts.
5.7 Immune Globulins and Transfusions
Immune Globulins (IG) and other blood products should not be given concurrently with ProQuad [see Drug Interactions (7.1)]. These products may contain antibodies that interfere with vaccine virus replication and decrease the expected immune response.
The ACIP has specific recommendations for intervals between administration of antibody containing products and live virus vaccines.
5.8 Salicylate Therapy
Avoid the use of salicylates (aspirin) or salicylate-containing products in children and adolescents 12 months through 12 years of age, for six weeks following vaccination with ProQuad due to the association of Reye syndrome with salicylate therapy and wild-type varicella infection [see Drug Interactions (7.2) and Patient Counseling Information (17)].
-
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a vaccine cannot be directly compared to rates in the clinical trials of another vaccine and may not reflect the rates observed in practice. Vaccine-related adverse reactions reported during clinical trials were assessed by the study investigators to be possibly, probably, or definitely vaccine-related and are summarized below.
Children 12 Through 23 Months of Age Who Received a Single Dose of ProQuad
ProQuad was administered subcutaneously to 4497 children 12 through 23 months of age involved in 4 randomized clinical trials without concomitant administration with other vaccines. The safety of ProQuad was compared with the safety of M-M-R II and VARIVAX given concomitantly (N=2038) at separate injection sites. The safety profile for ProQuad was similar to the component vaccines. Children in these studies were monitored for up to 42 days postvaccination using vaccination report card-aided surveillance. Safety follow-up was obtained for 98% of children in each group. Few subjects (<0.1%) who received ProQuad discontinued the study due to an adverse reaction. The race distribution of the study subjects across these studies following a first dose of ProQuad was as follows: 65.2% White; 13.1% African-American; 11.1% Hispanic; 5.8% Asian/Pacific; 4.5% other; and 0.2% American Indian. The racial distribution of the control group was similar to that of the group who received ProQuad. The gender distribution across the studies following a first dose of ProQuad was 52.5% male and 47.5% female. The gender distribution of the control group was similar to that of the group who received ProQuad. Vaccine-related injection-site and systemic adverse reactions observed among recipients of ProQuad or M-M-R II and VARIVAX at a rate of at least 1% are shown in Table 1. Systemic vaccine-related adverse reactions that were reported at a significantly greater rate in individuals who received a first dose of ProQuad than in individuals who received first doses of M-M-R II and VARIVAX concomitantly at separate injection sites were fever (≥102°F [≥38.9°C] oral equivalent or abnormal) (21.5% versus 14.9%, respectively, risk difference 6.6%, 95% CI: 4.6, 8.5), and measles-like rash (3.0% versus 2.1%, respectively, risk difference 1.0%, 95% CI: 0.1, 1.8). Both fever and measles-like rash usually occurred within 5 to 12 days following the vaccination, were of short duration, and resolved with no long-term sequelae. Pain/tenderness/soreness at the injection site was reported at a statistically lower rate in individuals who received ProQuad than in individuals who received M-M-R II and VARIVAX concomitantly at separate injection sites (22.0% versus 26.8%, respectively, risk difference -4.8%, 95% CI: -7.1, -2.5). The only vaccine-related injection-site adverse reaction that was more frequent among recipients of ProQuad than recipients of M-M-R II and VARIVAX was rash at the injection site (2.4% versus 1.6%, respectively, risk difference 0.9%, 95% CI: 0.1, 1.5).
Table 1: Vaccine-Related Injection-Site and Systemic Adverse Reactions Reported in ≥1% of Children Who Received ProQuad Dose 1 or M-M-R II and VARIVAX at 12 to 23 Months of Age (0 to 42 Days Postvaccination) ProQuad
(N=4497)M-M-R II and VARIVAX
(N=2038)Adverse Reactions (n=4424)
%(n=1997)
%N = number of subjects vaccinated.
n = number of subjects with safety follow-up.- *
- Injection-site adverse reactions for M-M-R II and VARIVAX are based on occurrence with either of the vaccines administered.
- †
- Designates a solicited adverse reaction. Injection-site adverse reactions were solicited only from Days 0 to 4 postvaccination.
- ‡
- Temperature reported as elevated (≥102°F, oral equivalent) or abnormal.
Injection Site* Pain/tenderness/soreness† 22.0 26.7 Erythema† 14.4 15.8 Swelling† 8.4 9.8 Ecchymosis 1.5 2.3 Rash 2.3 1.5 Systemic Fever†,‡ 21.5 14.9 Irritability 6.7 6.7 Measles-like rash† 3.0 2.1 Varicella-like rash† 2.1 2.2 Rash (not otherwise specified) 1.6 1.4 Upper respiratory infection 1.3 1.1 Viral exanthema 1.2 1.1 Diarrhea 1.2 1.3 Rubella-like rashes were observed in <1% of subjects following a first dose of ProQuad.
In these clinical trials, two cases of herpes zoster were reported among 2108 healthy subjects 12 through 23 months of age who were vaccinated with their first dose of ProQuad and followed for 1 year. Both cases were unremarkable and no sequelae were reported.
Children 15 to 31 Months of Age Who Received a Second Dose of ProQuad
In 5 clinical trials, 2780 healthy children were vaccinated subcutaneously with ProQuad (dose 1) at 12 to 23 months of age and then administered a second dose approximately 3 to 9 months later. The race distribution of the study subjects across these studies following a second dose of ProQuad was as follows: 64.4% White; 14.1% African-American; 12.0% Hispanic; 5.9% other; 3.5% Asian/Pacific; and 0.1% American Indian. The gender distribution across the studies following a second dose of ProQuad was 51.5% male and 48.5% female. Children in these open-label studies were monitored for at least 28 days postvaccination using vaccination report card-aided surveillance. Safety follow-up was obtained for approximately 97% of children overall. Vaccine-related injection-site and systemic adverse reactions observed after Dose 1 and 2 of ProQuad at a rate of at least 1% are shown in Table 2. In these trials, the overall rates of systemic adverse reactions after ProQuad (dose 2) were comparable to, or lower than, those seen with the first dose. In the subset of children who received both ProQuad dose 1 and dose 2 in these trials (N=2408) with follow-up for fever, fever ≥102.2°F (≥38.9°C) was observed significantly less frequently days 1 to 28 after the second dose (10.8%) than after the first dose (19.1%) (risk difference 8.3%, 95% CI: 6.4, 10.3). Fevers ≥102.2°F (≥38.9°C) days 5 to 12 after vaccinations were also reported significantly less frequently after dose 2 (3.9%) than after dose 1 (13.6%) (risk difference 9.7%, 95% CI: 8.1, 11.3). In the subset of children who received both doses and for whom injection-site reactions were reported (N=2679), injection-site erythema was noted significantly more frequently after ProQuad (dose 2) as compared to ProQuad (dose 1) (12.6% and 10.8%, respectively, risk difference -1.8, 95% CI: -3.3, -0.3); however, pain and tenderness at the injection site was significantly lower after dose 2 (16.1%) as compared with after dose 1 (21.9%) (risk difference, 5.8%, 95% CI: 4.1, 7.6). Two children had febrile seizures after ProQuad (dose 2); both febrile seizures were thought to be related to a concurrent viral illness [see Adverse Reactions (6.3) and Clinical Studies (14)]. These studies were not designed or statistically powered to detect a difference in rates of febrile seizure between recipients of ProQuad as compared to M-M-R II and VARIVAX. The risk of febrile seizure has not been evaluated in a clinical study comparing the incidence rate after ProQuad (dose 2) with the incidence rate after concomitant M-M-R II (dose 2) and VARIVAX (dose 2) [see Adverse Reactions (6.1), Children 4 to 6 Years of Age Who Received ProQuad After Primary Vaccination with M-M-R II and VARIVAX].
Table 2: Vaccine-Related Injection-Site and Systemic Adverse Reactions Reported in ≥1% of Children Who Received ProQuad Dose 1 at 12 to 23 Months of Age and Dose 2 at 15 to 31 Months of Age (1 to 28 Days Postvaccination) ProQuad
Dose 1ProQuad
Dose 2Adverse Reactions (N=3112)
(n=3019)
%(N=2780)
(n=2695)
%N = number of subjects vaccinated.
n = number of subjects with safety follow-up.Injection-Site Pain/tenderness/soreness* 21.4 15.9 Erythema* 10.7 12.4 Swelling* 8.0 8.5 Injection-site bruising 1.1 0.0 Systemic Fever*,† 20.4 8.3 Irritability 6.0 2.4 Measles-like/Rubella-like rash 4.3 0.9 Varicella-like/Vesicular rash 1.5 0.1 Diarrhea 1.3 0.6 Upper respiratory infection 1.3 1.4 Rash (not otherwise specified) 1.2 0.6 Rhinorrhea 1.1 1.0 Children 4 to 6 Years of Age Who Received ProQuad After Primary Vaccination with M-M-R II and VARIVAX
In a double-blind clinical trial, 799 healthy 4- to 6-year-old children who received M-M-R II and VARIVAX at least 1 month prior to study entry were randomized to receive ProQuad administered subcutaneously and placebo (N=399), M-M-R II and placebo concomitantly (N=205) at separate injection sites, or M-M-R II and VARIVAX (N=195) concomitantly at separate injection sites [see Clinical Studies (14)]. Children in these studies were monitored for up to 42 days postvaccination using vaccination report card-aided surveillance. Safety follow-up was obtained for >98% of children in each group. The race distribution of the study subjects following a dose of ProQuad was as follows: 78.4% White; 12.3% African-American; 3.8% Hispanic; 3.5% other; and 2.0% Asian/Pacific. The gender distribution following a dose of ProQuad was 52.1% male and 47.9% female. Injection-site and systemic adverse reactions observed after Dose 1 and 2 of ProQuad at a rate of at least 1% are shown in Table 3 [see Clinical Studies (14)].
Table 3: Vaccine-Related Injection-Site and Systemic Adverse Reactions Reported in ≥1% of Children Previously Vaccinated with M-M-R II and VARIVAX Who Received ProQuad + Placebo, M-M-R II + Placebo, or M-M-R II + VARIVAX at 4 to 6 Years of Age (1 to 43 Days Postvaccination)
Adverse ReactionsProQuad + Placebo
(N=399)
(n=397)
%M-M-R II + Placebo
(N=205)
(n=205)
%M-M-R II + VARIVAX
(N=195)
(n=193)
%N = number of subjects vaccinated.
n = number of subjects with safety follow-up.Systemic Fever*,† 2.5 2.0 4.1 Cough 1.3 0.5 0.5 Irritability 1.0 0.5 1.0 Headache 0.8 1.5 1.6 Rhinorrhea 0.5 1.0 0.5 Nasopharyngitis 0.3 1.0 1.0 Vomiting 0.3 1.0 0.5 Upper respiratory infection 0.0 0.0 1.0 ProQuad
%Placebo
%M-M-R II
%Placebo
%M-M-R II
%VARIVAX
%Injection-Site Pain* 41.1 34.5 36.6 34.1 35.2 36.8 Erythema* 24.4 13.4 15.6 14.1 14.5 15.5 Swelling* 15.6 8.1 10.2 8.8 7.8 10.9 Bruising 3.5 3.8 2.4 3.4 1.6 2.1 Rash 1.5 1.3 0.0 0.0 0.5 0.0 Pruritus 1.0 0.3 0.0 0.0 0.0 1.0 Nodule 0.0 0.0 0.0 0.0 0.0 1.0 Safety in Trials That Evaluated Concomitant Use with Other Vaccines
ProQuad Administered with Diphtheria and Tetanus Toxoids and Acellular Pertussis Vaccine Adsorbed (DTaP) and Haemophilus influenzae type b Conjugate (Meningococcal Protein Conjugate) and Hepatitis B (Recombinant) Vaccine
In an open-label clinical trial, 1434 children were randomized to receive ProQuad administered subcutaneously given with diphtheria and tetanus toxoids and acellular pertussis vaccine adsorbed (DTaP) and Haemophilus influenzae type b conjugate (meningococcal protein conjugate) and hepatitis B (recombinant) vaccine concomitantly (N=949) or non-concomitantly with ProQuad given first and the other vaccines 6 weeks later (N=485). No clinically significant differences in adverse events were reported between treatment groups [see Clinical Studies (14)]. The race distribution of the study subjects who received ProQuad was as follows: 70.7% White; 10.9% Asian/Pacific; 10.7% African-American; 4.5% Hispanic; 3.0% other; and 0.2% American Indian. The gender distribution of the study subjects who received ProQuad was 53.6% male and 46.4% female.
ProQuad Administered with Pneumococcal 7-valent Conjugate Vaccine and/or Hepatitis A Vaccine, Inactivated
In an open-label clinical trial, 1027 healthy children 12 to 23 months of age were randomized to receive ProQuad administered subcutaneously (dose 1) and pneumococcal 7-valent conjugate vaccine (dose 4) concomitantly (N=510) or non-concomitantly at different clinic visits (N=517). The race distribution of the study subjects was as follows: 65.2% White; 15.1% African-American; 10.0% Hispanic; 6.6% other; and 3.0% Asian/Pacific. The gender distribution of the study subjects was 54.5% male and 45.5% female. Injection-site and systemic adverse reactions observed among recipients of ProQuad administered concomitantly or non-concomitantly with pneumococcal 7-valent conjugate vaccine at a rate of at least 1% are shown in Table 4. No clinically significant differences in adverse reactions were reported between the concomitant and non-concomitant treatment groups [see Clinical Studies (14)].
Table 4: Vaccine-Related Injection-Site and Systemic Adverse Reactions Reported in ≥1% of Children Who Received ProQuad (dose 1) Concomitantly or Non-Concomitantly with PCV7* (dose 4) at the First Visit (1 to 28 Days Postvaccination)
Adverse ReactionsProQuad + PCV7
(N=510)
(n=498)
%PCV7
(N=258)
(n=250)
%ProQuad
(N=259)
(n=255)
%N/A = Not applicable.
N = number of subjects vaccinated.
n = number of subjects with safety follow-up.Injection-Site - ProQuad Pain† 24.9 N/A 24.7 Erythema† 12.4 N/A 11.0 Swelling† 10.8 N/A 7.5 Bruising 2.0 N/A 1.6 Injection-Site - PCV7 Pain† 30.5 29.6 N/A Erythema† 21.1 24.4 N/A Swelling† 17.9 20.0 N/A Bruising 1.6 1.2 N/A Systemic Fever†,‡ 15.5 10.0 15.3 Measles-like rash 4.4 0.8 5.1 Irritability 3.8 3.6 3.5 Upper respiratory infection 1.6 0.8 1.2 Varicella-like/vesicular rash 1.6 0.0 1.2 Diarrhea 0.8 1.2 1.2 Vomiting 0.6 0.8 1.2 Rash 0.4 0.0 1.2 Somnolence 0.0 0.0 1.2 In an open-label clinical trial, 699 healthy children 12 to 23 months of age were randomized to receive 2 doses of VAQTA (hepatitis A vaccine, inactivated) (N=352) or 2 doses of VAQTA concomitantly with 2 doses of ProQuad administered subcutaneously (N=347) at least 6 months apart. An additional 1101 subjects received 2 doses of VAQTA alone at least 6 months apart (non-randomized), resulting in 1453 subjects receiving 2 doses of VAQTA alone (1101 non-randomized and 352 randomized) and 347 subjects receiving 2 doses of VAQTA concomitantly with ProQuad (all randomized). The race distribution of the study subjects following a dose of ProQuad was as follows: 47.3% White; 42.7% Hispanic; 5.5% other; 2.9% African-American; and 1.7% Asian/Pacific. The gender distribution of the study subjects following a dose of ProQuad was 49.3% male and 50.7% female. Vaccine-related injection-site adverse reactions (days 1 to 5 postvaccination) and systemic adverse events (days 1 to 14 post VAQTA and days 1 to 28 post ProQuad vaccination) observed among recipients of VAQTA and ProQuad administered concomitantly with VAQTA at a rate of at least 1% are shown in Tables 5 and 6, respectively. In addition, among the randomized cohort, in the 14 days after each vaccination, the rates of fever (including all vaccine- and non-vaccine-related reports) were significantly higher in subjects who received ProQuad with VAQTA concomitantly after dose 1 (22.0%) as compared to subjects given dose 1 of VAQTA without ProQuad (10.8%). However, rates of fever were not significantly higher in subjects who received ProQuad with VAQTA concomitantly after dose 2 (12.5%) as compared to subjects given dose 2 of VAQTA without ProQuad (9.4%). In post-hoc analyses, these rates were significantly different for dose 1 (relative risk (RR) 2.03 [95% CI: 1.42, 2.94]), but not dose 2 (RR 1.32 [95% CI: 0.82, 2.13]). Rates of injection-site adverse reactions and other systemic adverse events were lower following a second dose than following the first dose of both vaccines given concomitantly.
Table 5: Vaccine-Related Injection-Site Adverse Reactions Reported in ≥1% of Children Who Received VAQTA or ProQuad Concomitantly with VAQTA 1 to 5 Days After Vaccination with VAQTA or VAQTA and ProQuad Dose 1 Dose 2
Adverse ReactionsVAQTA
(N=1453)
(n=1412)
%ProQuad + VAQTA
(N=347)
(n=328)
%VAQTA
(N=1301)
(n=1254)
%ProQuad + VAQTA
(N=292)
(n=264)
%N/A = Not applicable.
N = number of subjects vaccinated.
n = number of subjects with safety follow-up.- *
- Designates a solicited adverse reaction. Injection-site adverse reactions were solicited only from Days 1 to 5 postvaccination.
Injection-Site - VAQTA Pain/tenderness* 29.2 27.1 30.1 25.0 Erythema* 13.5 12.5 14.3 11.7 Swelling* 7.1 9.1 9.0 8.0 Injection-site bruising 1.9 2.4 1.0 0.8 Injection-Site - ProQuad Pain/tenderness* N/A 30.5 N/A 26.2 Erythema* N/A 13.4 N/A 12.9 Swelling* N/A 6.7 N/A 6.5 Injection-site bruising N/A 1.5 N/A 0.4 Table 6: Vaccine-Related Systemic Adverse Reactions Reported in ≥1% of Children Who Received VAQTA* or ProQuad Concomitantly with VAQTA 1 to 14 Days After VAQTA or Vaccination with ProQuad and VAQTA and 1 to 28 Days After Vaccination with ProQuad and VAQTA Adverse Reactions Dose 1 Dose 2 Days 1 to 14 Days 1 to 28 Days 1 to 14 Days 1 to 28 VAQTA†
(N=1453)
(n=1412)
%ProQuad + VAQTA†
(N=347)
(n=328)
%ProQuad + VAQTA
(N=347)
(n=328)
%VAQTA
(N=1301)
(n=1254)
%ProQuad + VAQTA†
(N=292)
(n=264)
%ProQuad + VAQTA†
(N=291)
(n=263)
%N = number of subjects vaccinated.
n = number of subjects with safety follow-up.Fever‡,§ 5.7 14.9 15.2 4.1 8.0 8.4 Irritability 5.8 7.0 7.3 3.5 5.3 5.3 Measles-like rash 0.0 3.4 3.4 0.0 1.1 1.1 Rhinorrhea 0.6 2.7 3.0 0.6 1.1 2.7 Diarrhea 1.5 1.8 2.4 1.7 0.4 0.8 Cough 0.6 2.1 2.1 0.2 0.8 1.5 Vomiting 1.1 0.3 0.9 0.6 0.8 1.1 In an open-label clinical trial, 653 children 12 to 23 months of age were randomized to receive a first dose of ProQuad administered subcutaneously with VAQTA and pneumococcal 7-valent conjugate vaccine concomitantly (N=330) or a first dose of ProQuad administered subcutaneously and pneumococcal 7-valent conjugate vaccine concomitantly and then vaccinated with VAQTA 6 weeks later (N=323). Approximately 6 months later, subjects received either the second doses of ProQuad and VAQTA concomitantly or the second doses of ProQuad and VAQTA separately. The race distribution of the study subjects was as follows: 60.3% White; 21.6% African-American; 9.5% Hispanic; 7.2% other; 1.1% Asian/Pacific; and 0.3% American Indian. The gender distribution of the study subjects was 50.7% male and 49.3% female. Vaccine-related injection-site and systemic adverse reactions observed among recipients of concomitant ProQuad, VAQTA, and pneumococcal 7-valent conjugate vaccine and ProQuad and pneumococcal 7-valent conjugate vaccine at a rate of at least 1% are shown in Tables 7 and 8. In the 28 days after vaccination with the first dose of ProQuad, the rates of fever (including all vaccine- and non-vaccine-related reports) were comparable in subjects who received the 3 vaccines together (38.6%) as compared with subjects given ProQuad and pneumococcal 7-valent conjugate vaccine (42.7%). The rates of fever in the 28 days following the second dose of ProQuad were also comparable in subjects who received ProQuad and VAQTA together (17.4%) as compared with subjects given ProQuad separately from VAQTA (17.0%). In a post-hoc analysis, these differences were not statistically significant after ProQuad (dose 1) (RR 0.90 [95% CI: 0.75, 1.09]) nor after dose 2 (RR 1.02 [95% CI: 0.70, 1.51]). No clinically significant differences in adverse reactions were reported among treatment groups [see Clinical Studies (14)].
Table 7: Vaccine-Related Injection-Site Adverse Reactions Reported in ≥1% of Children Who Received ProQuad + VAQTA + PCV7* Concomitantly or VAQTA Alone Followed by ProQuad + PCV7 Concomitantly (1 to 5 Days After a Dose of ProQuad) Adverse Reactions Dose 1 Dose 2 VAQTA + ProQuad + PCV7
(N=330)
(n=311)
%VAQTA Alone Followed by ProQuad + PCV7
(N=323)
(n=302)
%VAQTA + ProQuad
(N=273)
(n=265)
%VAQTA Alone Followed by ProQuad
(N=240)
(n=230)
%N/A = Not applicable.
N = number of subjects vaccinated.
n = number of subjects with safety follow-up.Injection-Site - ProQuad Pain/tenderness† 21.2 24.2 18.1 17.0 Erythema† 13.5 11.9 10.6 13.0 Swelling† 7.4 10.9 8.3 11.7 Bruising 1.9 1.3 0.8 0.4 Injection-Site - VAQTA Pain/tenderness† 20.6 15.3 17.5 20.3 Erythema† 9.6 11.7 9.1 12.7 Swelling† 6.8 9.5 6.1 7.6 Bruising 1.3 1.1 1.1 1.6 Rash 1.0 0.0 0.4 0.4 Injection-Site - PCV7 Pain/tenderness† 25.4 27.6 N/A N/A Erythema† 16.4 16.6 N/A N/A Swelling† 13.2 14.3 N/A N/A Bruising 0.6 1.7 N/A N/A Table 8: Vaccine-Related Systemic Adverse Reactions Reported in ≥1% of Children Who Received ProQuad + VAQTA + PCV7* Concomitantly, or VAQTA Alone Followed by ProQuad + PCV7 Concomitantly (1 to 28 Days After a Dose of ProQuad) Adverse Reactions Dose 1 Dose 2 VAQTA + ProQuad + PCV7
(N=330)
(n=311)
%VAQTA Alone Followed by ProQuad + PCV7
(N=323)
(n=302)
%VAQTA + ProQuad
(N=273)
(n=265)
%VAQTA Alone Followed by ProQuad
(N=240)
(n=230)
%N = number of subjects vaccinated.
n = number of subjects with safety follow-up.Fever†,‡ 26.4 27.2 9.1 9.6 Irritability 4.8 6.3 1.9 1.3 Measles-like rash† 2.3 4.0 0.0 0.0 Varicella-like rash† 1.0 1.7 0.0 0.0 Rash (not otherwise specified) 1.3 1.3 0.0 0.9 Diarrhea 1.3 1.3 0.4 1.3 Upper respiratory infection 1.0 1.3 1.1 0.9 Viral infection 1.0 0.7 0.0 0.0 Rhinorrhea 0.0 0.7 1.1 0.0 In a randomized open-label clinical trial (NCT00402831), conducted in France, 405 children 12 months through 18 months of age received 2 doses of ProQuad, administered 30 days apart (a non-US licensed interval), by either the intramuscular (n=202) or subcutaneous (n=203) route. In the overall population, 50.9% were male and the median age was 13.3 months. Local and systemic solicited adverse reactions were recorded by parents or guardians using standardized diary cards. Local solicited reactions were recorded for 4 days after vaccination, and systemic solicited adverse reactions were recorded for 28 days after vaccination. In the event that a participant experienced a rash or a mumps-like illness, parents and/or guardians were instructed to contact the investigator for an examination as soon as possible and no later than 72 hours following onset of symptoms. The nature of any rash was characterized by principal investigator either as measles-like, rubella-like, varicella-like or “other”. Study investigators reviewed the diary card with the participant or participant’s legal guardian 30 days and 42 days after dose 1 and dose 2, respectively to ensure consistency with protocol definitions. Tables 9 and 10 below present the frequency of solicited adverse reactions based on the final assessment by the study investigators.
Table 9. Proportion of Participants Reporting Solicited Adverse Reactions Following First Vaccination with ProQuad, by the Intramuscular or Subcutaneous Route INTRAMUSCULAR
N=202
%SUBCUTANEOUS
N=203
%N=total number of participants in the group - *
- Post-dose 1 (0-28 days), there was one episode of an injection-site rubella-like rash and one injection-site varicella-like rash. They were both reported in the subcutaneous group.
- †
- Intensity of injection site reaction: mild or ≤2.5 cm; moderate or >2.5 to ≤5.0 cm; severe or >5.0 cm.
- ‡
- Intensity of pain: mild: awareness of symptom but easily tolerated; moderate: definitely acting like something is wrong; severe: extremely distressed or unable to do usual activities.
- §
- The percentage of fever is defined within the population who had valid temperature measurements. Three participants in IM group and four participants in SC group do not have temperature measurements and were excluded from the denominator; resulting in N=199 and N=199, respectively.
- ¶
- In the IM Group 96.0% of fevers were documented using the rectal route of measurement and 4.0% of fevers were documented only by the axillary route of measurement. In the SC Group 99.3% of fevers were documented using the rectal route of measurement and 0.7% of fevers were documented only by the axillary route of measurement.
Solicited local injection-site adverse reactions (Days 0 to 4)* Erythema† 5.0 14.3 Mild 4.5 12.8 Moderate 0 1.5 Severe 0 0 Missing 0.5 0 Pain‡ 10.9 5.9 Mild 8.9 3.9 Moderate 2.0 2.0 Severe 0 0 Swelling† 1.0 3.9 Mild 1.0 3.9 Moderate 0 0 Severe 0 0 Solicited systemic adverse reactions (Days 0 to 28) Measles/Measles-like rash 0.5 2.0 Rubella/Rubella-like rash 3.0 3.0 Varicella/Varicella-like rash 1.0 0.5 Zoster/Zoster-like rash 0 0 Mumps-like illness 0.5 0 Fever (temperature ≥38.0°C)§,¶ 62.8 68.3 38.0-38.5°C 21.1 17.6 >38.5-39.0°C 18.1 21.6 >39.0-39.5°C 14.1 18.1 >39.5-40.0°C 7.0 9.0 >40.0°C 2.5 2.0 Table 10. Proportion of Participants Reporting Solicited Adverse Reactions Following Second Vaccination with ProQuad, by the Intramuscular or Subcutaneous Route INTRAMUSCULAR
N=201
%SUBCUTANEOUS
N=200
%N=total number of participants in the group - *
- Post-dose 2 (0-28 days), there was only 1 episode of an injection-site measle-like rash and this was reported in the subcutaneous group.
- †
- Intensity of injection site reaction: mild or ≤2.5 cm; moderate or >2.5 to ≤5.0 cm; severe or >5.0 cm.
- ‡
- Intensity of pain: mild: awareness of symptom but easily tolerated; moderate: definitely acting like something is wrong; severe: extremely distressed or unable to do usual activities.
- §
- The percentage of fever is defined within the population who had valid temperature measurements. Five participants in IM group and five participants in SC group did not have temperature measurements and were excluded from the denominator; resulting in N=196 and N=195, respectively.
- ¶
- In the IM Group 95.9% of fevers were documented using the rectal route of measurement and 4.1% of fevers were documented only by the axillary route of measurement. In the SC Group 98.9% of fevers were documented using the rectal route of measurement and 1.1% of fevers were documented only by the axillary route of measurement.
Solicited local injection-site adverse reactions (Days 0 to 4)* Erythema† 15.4 27.0 Mild 13.9 22.5 Moderate 1.0 4.5 Severe 0 0 Missing 0.5 0 Pain‡ 10.0 10.0 Mild 9.0 7.0 Moderate 0.5 3.0 Severe 0.5 0 Swelling† 6.0 12.5 Mild 5.0 11.0 Moderate 1.0 1.0 Severe 0 0 Missing 0 0.5% (1/200) Solicited systemic adverse reactions (Days 0 to 28) Measles-like rash 0 1.0 Rubella-like rash 2.0 1.0 Varicella-like rash 0 2.0 Zoster-like rash 0 0 Mumps-like illness 0.5 0 Fever (temperature ≥38.0°C)§,¶ 50.0 47.2 38.0-38.5°C 13.8 16.4 >38.5-39.0°C 18.4 10.8 >39.0-39.5°C 11.2 11.3 >39.5-40.0°C 5.6 7.2 >40.0°C 1.0 1.5 Unsolicited adverse events (0-28 days post-vaccination 1 and 2) and serious adverse events (day 0 to last visit) were recorded using diary cards supplemented by medical review. Data on unsolicited adverse events were transcribed into the study database during an on-site visit at day 30 and day 42. Serious adverse events occurred at a rate of 1% and 0.5% in each group post-dose 1 and 2, respectively. None of the serious adverse events that occurred were considered related to the study vaccination.
Herpes Zoster
ProQuad and VARIVAX each contain the Oka/Merck varicella virus vaccine strain. Clinical trial data with VARIVAX are therefore, relevant to ProQuad. Overall, 9454 healthy children (12 months to 12 years of age) and 1648 adolescents and adults (13 years of age and older) have been vaccinated with VARIVAX in clinical trials. Eight cases of herpes zoster have been reported in children during 42,556 person-years of follow-up in clinical trials, resulting in a calculated incidence of at least 18.8 cases per 100,000 person-years. The completeness of this reporting has not been determined. One case of herpes zoster has been reported in the adolescent and adult age group during 5410 person-years of follow-up in clinical trials, resulting in a calculated incidence of 18.5 cases per 100,000 person-years. All 9 cases were mild and without sequelae. Two cultures (one child and one adult) obtained from vesicles were positive for wild-type VZV as confirmed by restriction endonuclease analysis {11}. The long-term effect of VARIVAX on the incidence of herpes zoster, particularly in those vaccinees exposed to wild-type varicella, is unknown at present.
In children, the reported rate of herpes zoster in VARIVAX recipients appears not to exceed that previously determined in a population-based study of healthy children who had experienced wild-type varicella {12}. The incidence of herpes zoster in adults who have had wild-type varicella infection is higher than that in children.
6.2 Post-Marketing Experience
The following adverse events have been identified during post-approval use of either the components of ProQuad or ProQuad. Because the events are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to vaccine exposure.
Subacute sclerosing panencephalitis, encephalitis, aseptic meningitis, meningitis, measles, atypical measles, pneumonia, respiratory infection, infection, varicella (vaccine strain), influenza, wild-type or vaccine strain herpes zoster, orchitis, epididymitis, cellulitis, skin infection, retinitis, bronchitis, parotitis, sinusitis, impetigo, herpes simplex, candidiasis, rhinitis.
The vaccine virus (Oka/Merck strain) contained in ProQuad may establish latency of varicella zoster virus in immunocompetent individuals, with the potential for later development of herpes zoster.
Cases of encephalitis or meningitis caused by vaccine strain varicella virus have been reported in immunocompromised and immunocompetent individuals previously vaccinated with VARIVAX (same varicella vaccine strain as in ProQuad) months to years after vaccination. Reported cases were commonly associated with preceding or concurrent herpes zoster rash.
Blood and the lymphatic system disorders
Aplastic anemia, thrombocytopenia, regional lymphadenopathy, lymphadenitis.
Immune system disorders
Anaphylaxis and related phenomena such as angioneurotic edema, facial edema, and peripheral edema, anaphylactoid reaction.
Psychiatric disorders
Agitation, apathy, nervousness.
Nervous system disorders
Measles inclusion body encephalitis, acute disseminated encephalomyelitis, transverse myelitis, cerebrovascular accident, encephalopathy, Guillain-Barré syndrome, optic neuritis, Bell’s palsy, polyneuropathy, ataxia, hypersomnia, afebrile convulsions or seizures, febrile seizure, headache, syncope, dizziness, tremor, paresthesia.
Eye disorders
Necrotizing retinitis (in immunocompromised individuals), retrobulbar neuritis, ocular palsies, edema of the eyelid, irritation eye.
Ear and labyrinth disorders
Nerve deafness, ear pain.
Vascular disorders
Extravasation blood.
Respiratory, thoracic and mediastinal disorders
Pneumonitis, pulmonary congestion, wheezing, bronchial spasm, epistaxis, sore throat.
Gastrointestinal disorders
Hematochezia, abdominal pain, mouth ulcer.
Skin and subcutaneous tissue disorders
Stevens-Johnson syndrome, Henoch-Schönlein purpura, erythema multiforme, acute hemorrhagic edema of infancy, purpura, skin induration, panniculitis, pruritus.
Musculoskeletal, connective tissue and bone disorders
Arthritis, arthralgia, pain of the hip, leg, or neck; myalgia; musculoskeletal pain.
General disorders and administration site conditions
Injection-site complaints including wheal and flare, warm to touch, stiffness, warm sensation, inflammation, injection-site hemorrhage, injection-site injury.
Herpes Zoster
The vaccine virus (Oka/Merck strain) contained in ProQuad may establish latency of varicella zoster virus in immunocompetent individuals, with the potential for later development of herpes zoster.
6.3 Post-Marketing Observational Safety Surveillance Study
Safety was evaluated in an observational study that included 69,237 children vaccinated with ProQuad 12 months to 12 years old. A historical comparison group included 69,237 age-, gender-, and date-of-vaccination- (day and month) matched subjects who were given M-M-R II and VARIVAX concomitantly. The primary objective was to assess the incidence of febrile seizures occurring within various time intervals after vaccination in 12- to 60-month-old children who had neither been vaccinated against measles, mumps, rubella, or varicella, nor had a history of the wild-type infections (N=31,298 vaccinated with ProQuad, including 31,043 who were 12 to 23 months old). The incidence of febrile seizures was also assessed in a historical control group of children who had received their first vaccination with M-M-R II and VARIVAX concomitantly (N=31,298, including 31,019 who were 12 to 23 months old). The secondary objective was to assess the general safety of ProQuad in the 30-day period after vaccination in children 12 months to 12 years old.
In pre-licensure clinical studies, an increase in fever was observed 5 to 12 days after vaccination with ProQuad (dose 1) compared to M-M-R II and VARIVAX (dose 1) given concomitantly. In the post-marketing observational surveillance study, results from the primary safety analysis revealed an approximate two-fold increase in the risk of febrile seizures in the same 5 to 12 day timeframe after vaccination with ProQuad (dose 1). The incidence of febrile seizures 5 to 12 days after ProQuad (dose 1) (0.70 per 1000 children) was higher than that in children receiving M-M-R II and VARIVAX concomitantly (0.32 per 1000 children) [RR 2.20, 95% confidence interval (CI): 1.04, 4.65]. The incidence of febrile seizures 0 to 30 days after ProQuad (dose 1) (1.41 per 1000 children) was similar to that observed in children receiving M-M-R II and VARIVAX concomitantly [RR 1.10 (95% CI: 0.72, 1.69)]. See Table 11. General safety analyses revealed that the risks of fever (RR=1.89; 95% CI: 1.67, 2.15) and skin eruption (RR=1.68; 95% CI: 1.07, 2.64) were significantly higher after ProQuad (dose 1) compared with those who received concomitant first doses of M-M-R II and VARIVAX, respectively. All medical events that resulted in hospitalization or emergency room visits were compared between the group given ProQuad and the historical comparison group, and no other safety concerns were identified in this study.
Table 11: Confirmed Febrile Seizures Days 5 to 12 and 0 to 30 After Vaccination with ProQuad (dose 1) Compared to Concomitant Vaccination with M-M-R II and VARIVAX (dose 1) in Children 12 to 60 Months of Age Time Period ProQuad cohort (N=31,298) MMR+V cohort (N=31,298) Relative risk (95% CI) n Incidence per 1000 n Incidence per 1000 5 to 12 Days 22 0.70 10 0.32 2.20 (1.04, 4.65) 0 to 30 Days 44 1.41 40 1.28 1.10 (0.72, 1.69) In this observational post-marketing study, no case of febrile seizure was observed during the 5 to 12 day postvaccination time period among 26,455 children who received ProQuad as a second dose of M-M-R II and VARIVAX. In addition, detailed general safety data were available from more than 25,000 children who received ProQuad as a second dose of M-M-R II and VARIVAX, most of them (95%) between 4 and 6 years of age, and an analysis of these data by an independent, external safety monitoring committee did not identify any specific safety concern.
-
7 DRUG INTERACTIONS
7.1 Immune Globulins and Transfusions
Administration of immune globulins and other blood products concurrently with ProQuad vaccine may interfere with the expected immune response [see Warnings and Precautions (5.7)] {9-11}. The ACIP has specific recommendations for intervals between administration of antibody containing products and live virus vaccines.
7.2 Salicylates
Reye syndrome has been reported following the use of salicylates during wild-type varicella infection. Vaccine recipients should avoid use of salicylates for 6 weeks after vaccination with ProQuad [see Warnings and Precautions (5.8) and Patient Counseling Information (17)].
7.3 Corticosteroids and Immunosuppressive Drugs
ProQuad vaccine should not be administered to individuals receiving immunosuppressive therapy, including high dose corticosteroids. Vaccination with ProQuad vaccine can result in disseminated disease and extensive vaccine-associated rash in individuals on immunosuppressive drugs [see Contraindications (4.2)].
7.4 Drug/Laboratory Test Interactions
Live, attenuated measles, mumps, and rubella virus vaccines given individually may result in a temporary depression of tuberculin skin sensitivity. Therefore, if a tuberculin test is to be done, it should be administered either any time before, simultaneously with, or at least 4 to 6 weeks after ProQuad.
7.5 Use with Other Vaccines
At least 1 month should elapse between a dose of a measles-containing vaccine and a dose of ProQuad, and at least 3 months should elapse between administration of 2 doses of ProQuad or varicella-containing vaccines.
ProQuad may be administered concomitantly with Haemophilus influenzae type b conjugate (meningococcal protein conjugate) and hepatitis B (recombinant). Additionally, ProQuad may be administered concomitantly with pneumococcal 7-valent conjugate vaccine, and/or hepatitis A (inactivated) vaccines [see Clinical Studies (14)].
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
ProQuad vaccine contains live attenuated measles, mumps, rubella and varicella viruses. The vaccine is contraindicated for use in pregnant women because infection during pregnancy with the wild-type viruses is associated with maternal and fetal adverse outcomes.
For women who are inadvertently vaccinated when pregnant or who become pregnant within 3 months of administration of ProQuad, the healthcare provider should be aware of the following: (1) Reports have indicated that contracting wild-type measles during pregnancy enhances fetal risk. Increased rates of spontaneous abortion, stillbirth, congenital defects, and prematurity have been observed subsequent to infection with wild-type measles during pregnancy. There are no adequate studies of the attenuated (vaccine) strain of measles virus in pregnancy; (2) Mumps infection during the first trimester of pregnancy may increase the rate of spontaneous abortion. Although mumps vaccine virus has been shown to infect the placenta and fetus, there is no evidence that it causes congenital malformations in humans {12}; (3) In a 10-year survey involving over 700 pregnant women who received rubella vaccine within 3 months before or after conception (of whom 189 received the Wistar RA 27/3 strain), none of the newborns had abnormalities compatible with congenital rubella syndrome {13}; and (4) Wild-type varicella, if acquired during pregnancy, can sometimes cause congenital varicella syndrome.
Available data on inadvertent administration of ProQuad to pregnant women are insufficient to inform vaccine-associated risks in pregnancy.
There are no relevant animal data.
All pregnancies have a risk of birth defect, loss, or other adverse outcomes. In the US general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4%, and 15% to 20%, respectively {14,15}.
Data
Human Data
In a 10-year CDC survey involving over 700 pregnant women who received rubella vaccine within 3 months before or after conception (of whom 189 received the Wistar RA 27/3 strain), none of the newborns had abnormalities compatible with congenital rubella syndrome {13}.
8.2 Lactation
Risk Summary
It is not known whether varicella, measles, or mumps vaccine virus is excreted in human milk. Studies have shown that lactating postpartum women vaccinated with live rubella vaccine may secrete the virus in breast milk and transmit it to breastfed infants [see Warnings and Precautions (5.6)] {16,17}.
The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for ProQuad, and any potential adverse effects on the breastfed child from ProQuad or from the underlying maternal condition. For preventive vaccines, the underlying maternal condition is susceptibility to disease prevented by the vaccine.
8.4 Pediatric Use
Do not administer ProQuad to infants younger than 12 months of age or to children 13 years and older. Safety and effectiveness of ProQuad in infants younger than 12 months of age and in children 13 years and older have not been established [see Clinical Studies (14)].
-
11 DESCRIPTION
ProQuad (Measles, Mumps, Rubella and Varicella Virus Vaccine Live) is a combined, attenuated, live virus vaccine containing measles, mumps, rubella, and varicella viruses. ProQuad is a sterile lyophilized preparation of (1) the components of M-M-R II (Measles, Mumps, and Rubella Virus Vaccine Live): Measles Virus Vaccine Live, a more attenuated line of measles virus, derived from Enders' attenuated Edmonston strain and propagated in chick embryo cell culture; Mumps Virus Vaccine Live, the Jeryl Lynn™ (B level) strain of mumps virus propagated in chick embryo cell culture; Rubella Virus Vaccine Live, the Wistar RA 27/3 strain of live attenuated rubella virus propagated in WI-38 human diploid lung fibroblasts; and (2) Varicella Virus Vaccine Live (Oka/Merck), the Oka/Merck strain of varicella-zoster virus propagated in MRC-5 cells. The cells, virus pools, bovine serum, and recombinant human albumin used in manufacturing are all tested to provide assurance that the final product is free of potential adventitious agents.
ProQuad, when reconstituted as directed, is a sterile suspension for intramuscular or subcutaneous administration. Each approximately 0.5 mL dose contains not less than 3.00 log10 TCID50 of measles virus; 4.30 log10 TCID50 of mumps virus; 3.00 log10 TCID50 of rubella virus; and not less than 3.99 log10 PFU of Oka/Merck varicella virus.
After reconstitution, each 0.5 mL dose of the vaccine also contains 21 mg of sucrose, 11 mg of hydrolyzed gelatin, 2.4 mg of sodium chloride, 1.8 mg of sorbitol, 0.40 mg of monosodium L-glutamate, 0.34 mg of sodium phosphate dibasic, 0.31 mg of recombinant human albumin, 0.17 mg of sodium bicarbonate, 72 mcg of potassium phosphate monobasic, 60 mcg of potassium chloride; 36 mcg of potassium phosphate dibasic; and residual components from the manufacturing process: MRC-5 cells including DNA and protein; <16 mcg of neomycin, ≤0.5 mcg of bovine calf serum, and other buffer and media ingredients. The product contains no preservative.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
ProQuad has been shown to induce measles-, mumps-, rubella-, and varicella-specific immunity, which is thought to be the mechanism by which it protects against these four childhood diseases.
The efficacy of ProQuad was established through the use of immunological correlates for protection against measles, mumps, rubella, and varicella. Results from efficacy studies or field effectiveness studies that were previously conducted for the component vaccines were used to define levels of serum antibodies that correlated with protection against measles, mumps, and rubella. Also, in previous studies with varicella vaccine, antibody responses against varicella virus ≥5 gpELISA units/mL in a glycoprotein enzyme-linked immunosorbent assay (gpELISA) (not commercially available) similarly correlated with long-term protection. In these efficacy studies, the clinical endpoint for measles and mumps was a clinical diagnosis of either disease confirmed by a 4-fold or greater rise in serum antibody titers between either postvaccination or acute and convalescent titers; for rubella, a 4-fold or greater rise in antibody titers with or without clinical symptoms of rubella; and for varicella, varicella-like rash that occurred >42 days postvaccination and for which varicella was not excluded by either viral cultures of the lesion or serological tests. Specific laboratory evidence of varicella either by serology or culture was not required to confirm the diagnosis of varicella. Clinical studies with a single dose of ProQuad have shown that vaccination elicited rates of antibody responses against measles, mumps, and rubella that were similar to those observed after vaccination with a single dose of M-M-R II [see Clinical Studies (14)] and seroresponse rates for varicella virus were similar to those observed after vaccination with a single dose of VARIVAX [see Clinical Studies (14)]. The duration of protection from measles, mumps, rubella, and varicella infections after vaccination with ProQuad is unknown.
12.6 Persistence of Antibody Responses after Vaccination
The persistence of antibody at 1 year after vaccination was evaluated in a subset of 2107 children enrolled in the clinical trials. Antibody was detected in 98.9% (1722/1741) for measles, 96.7% (1676/1733) for mumps, 99.6% (1796/1804) for rubella, and 97.5% (1512/1550) for varicella (≥5 gpELISA units/mL) of vaccinees following a single dose of ProQuad.
Experience with M-M-R II demonstrates that neutralizing and ELISA antibodies to measles, mumps, and rubella viruses are still detectable in 95-100%, 74-91%, and 90-100% of individuals respectively, 11 to 13 years after primary vaccination series {18-24}. Varicella antibodies were present for up to ten years postvaccination in most of the individuals tested who received 1 dose of VARIVAX.
- 13 NONCLINICAL TOXICOLOGY
-
14 CLINICAL STUDIES
Formal studies to evaluate the clinical efficacy of ProQuad have not been performed.
Efficacy of the measles, mumps, rubella, and varicella components of ProQuad was previously established in a series of clinical studies with the monovalent vaccines. A high degree of protection from infection was demonstrated in these studies {25-32}.
Immunogenicity in Children 12 Months to 6 Years of Age
Prior to licensure, immunogenicity was studied in 5845 healthy children 12 months to 6 years of age with a negative clinical history of measles, mumps, rubella, and varicella who participated in 5 randomized clinical trials. The immunogenicity of ProQuad administered subcutaneously was similar to that of its individual component vaccines (M-M-R II and VARIVAX), which are currently used in routine vaccination.
The presence of detectable antibody was assessed by an appropriately sensitive enzyme-linked immunosorbent assay (ELISA) for measles, mumps (wild-type and vaccine-type strains), and rubella, and by gpELISA for varicella. For evaluation of vaccine response rates, a positive result in the measles ELISA corresponded to measles antibody concentrations of ≥255 mIU/mL when compared to the WHO II (66/202) Reference Immunoglobulin for Measles.
Children were positive for mumps antibody if the antibody level was ≥10 ELISA units/mL. A positive result in the rubella ELISA corresponded to concentrations of ≥10 IU rubella antibody/mL when compared to the WHO International Reference Serum for Rubella; children with varicella antibody levels ≥5 gpELISA units/mL were considered to be seropositive since a response rate based on ≥5 gpELISA units/mL has been shown to be highly correlated with long-term protection.
Immunogenicity in Children 12 to 23 Months of Age After a Single Dose
In 4 randomized clinical trials, 5446 healthy children 12 to 23 months of age were administered ProQuad subcutaneously, and 2038 children were vaccinated with M-M-R II and VARIVAX given concomitantly at separate injection sites. Subjects enrolled in each of these trials had a negative clinical history, no known recent exposure, and no vaccination history for varicella, measles, mumps, and rubella. Children were excluded from study participation if they had an immune impairment or had a history of allergy to components of the vaccine(s). Except for in 1 trial [see ProQuad Administered with Diphtheria and Tetanus Toxoids and Acellular Pertussis Vaccine Adsorbed (DTaP) and Haemophilus influenzae type b Conjugate (Meningococcal Protein Conjugate) and Hepatitis B (Recombinant) Vaccine below], no concomitant vaccines were permitted during study participation. The race distribution of the study subjects across these studies following a first dose of ProQuad was as follows: 66.3% White; 12.7% African-American; 9.9% Hispanic; 6.7% Asian/Pacific; 4.2% other; and 0.2% American Indian. The gender distribution of the study subjects across these studies following a first dose of ProQuad was 52.6% male and 47.4% female. A summary of combined immunogenicity results 6 weeks following administration of a single dose of ProQuad or M-M-R II and VARIVAX is shown in Table 12. These results were similar to the immune response rates induced by concomitant administration of single doses of M-M-R II and VARIVAX at separate injection sites (lower bound of the 95% CI for the risk difference in measles, mumps, and rubella seroconversion rates were >-5.0 percentage points and the lower bound of the 95% CI for the risk difference in varicella seroprotection rates was either >-15 percentage points [one study] or >-10.0 percentage points [three studies]).
Table 12: Summary of Combined Immunogenicity Results 6 Weeks Following the Administration of a Single Dose of ProQuad (Varicella Virus Potency ≥3.97 log10 PFU) or M-M-R II and VARIVAX (Per-Protocol Population) Group Antigen n Observed Response Rate
(95% CI)Observed GMT
(95% CI)n = Number of per-protocol subjects with evaluable serology.
CI = Confidence interval.
GMT = Geometric mean titer.
ELISA = Enzyme-linked immunosorbent assay.
PFU = Plaque-forming units.
OD = Optical density.- *
- Includes ProQuad + Placebo followed by ProQuad (Visit 1) (Protocol 009), ProQuad Middle and High Doses (Visit 1) (Protocol 011), ProQuad (Lot 1, Lot 2, Lot 3) (Protocol 012), both the Concomitant and Non-concomitant groups (Protocol 013).
- †
- The mumps antibody response was assessed by a vaccine-strain ELISA in Protocols 009 and 011 and by a wild-type ELISA in Protocols 012 and 013. In the former assay, the serostatus was based on the OD cutoff of the assay. In the latter assay, 10 mumps ELISA units was used as the serostatus cutoff.
ProQuad
(N=5446*)Varicella 4381 91.2%
(90.3%, 92.0%)15.5
(15.0, 15.9)Measles 4733 97.4%
(96.9%, 97.9%)3124.9
(3038.9, 3213.3)Mumps
(OD cutoff)†973 98.8%
(97.9%, 99.4%)105.3
(98.0, 113.1)Mumps (wild-type ELISA)† 3735 95.8%
(95.1%, 96.4%)93.1
(90.2, 96.0)Rubella 4773 98.5%
(98.1%, 98.8%)91.8
(89.6, 94.1)M-M-R II + VARIVAX
(N=2038*)Varicella 1417 94.1%
(92.8%, 95.3%)16.6
(15.9, 17.4)Measles 1516 98.2%
(97.4%, 98.8%)2239.6
(2138.3, 2345.6)Mumps
(OD cutoff)†501 99.4%
(98.3%, 99.9%)87.5
(79.7, 96.0)Mumps (wild-type ELISA)† 1017 98.0%
(97.0%, 98.8%)90.8
(86.2, 95.7)Rubella 1528 98.5%
(97.7%, 99.0%)102.2
(97.8, 106.7)Immunogenicity in Children 15 to 31 Months of Age After a Second Dose of ProQuad
In 2 of the 4 randomized clinical trials described above, a subgroup (N=1035) of the 5446 children administered a single dose of ProQuad subcutaneously were administered a second dose of ProQuad subcutaneously, approximately 3 to 9 months after the first dose. Children were excluded from receiving a second dose of ProQuad if they were recently exposed to or developed varicella, measles, mumps, and/or rubella prior to receipt of the second dose. No concomitant vaccines were administered to these children. The race distribution across these studies following a second dose of ProQuad was as follows: 67.3% White; 14.3% African-American; 8.3% Hispanic; 5.4% Asian/Pacific; 4.4% other; 0.2% American Indian; and 0.10% mixed. The gender distribution of the study subjects across these studies following a second dose of ProQuad was 50.4% male and 49.6% female. A summary of immune responses following a second dose of ProQuad is presented in Table 13. Results from this study showed that 2 doses of ProQuad administered at least 3 months apart elicited a positive antibody response to all four antigens in greater than 98% of subjects. The geometric mean titers (GMTs) following the second dose of ProQuad increased approximately 2-fold each for measles, mumps, and rubella, and approximately 41-fold for varicella.
Table 13: Summary of Immune Response to a First and Second Dose of ProQuad in Subjects <3 Years of Age Who Received ProQuad with a Varicella Virus Dose ≥3.97 Log10 PFU* Dose 1
N=1097Dose 2
N=1097Serostatus Cutoff/ Observed Response Rate Observed GMT Observed Response Rate Observed GMT Antigen Response Criteria n (95% CI) (95% CI) n (95% CI) (95% CI) ProQuad (Middle Dose) = ProQuad containing a varicella virus dose of 3.97 log10 PFU.
ProQuad (High Dose) = ProQuad containing a varicella virus dose of 4.25 log10 PFU.
ELISA = Enzyme-linked immunosorbent assay.
gpELISA = Glycoprotein enzyme-linked immunosorbent assay.
N = Number vaccinated at baseline.
n = Number of subjects who were per-protocol Postdose 1 and Postdose 2 and satisfied the given prevaccination serostatus cutoff.
CI = Confidence interval.
GMT = Geometric mean titer.
PFU = Plaque-forming units.- *
- Includes the following treatment groups: ProQuad + Placebo followed by ProQuad (Visit 1) (Protocol 009) and ProQuad (Middle and High Dose) (Protocol 011).
- †
- Samples from Protocols 009 and 011 were assayed in the legacy format Measles ELISA, which reported antibody titers in Measles ELISA units. To convert titers from ELISA units to mIU/mL, titers for these 2 protocols were divided by 0.1025. The lowest measurable titer postvaccination is 207.5 mIU/mL. The response rate for measles in the legacy format is the percent of subjects with a negative baseline measles antibody titer, as defined by the optical density (OD) cutoff, with a postvaccination measles antibody titer ≥207.5 mIU/mL.
Samples from Protocols 009 and 011 were assayed in the legacy format Rubella ELISA, which reported antibody titers in Rubella ELISA units. To convert titers from ELISA units to IU/mL, titers for these 2 protocols were divided by 1.28.
Measles ≥120 mIU/mL† 915 98.1% (97.0%, 98.9%) 2956.8 (2786.3, 3137.7) 915 99.5% (98.7%, 99.8%) 5958.0 (5518.9, 6432.1) ≥255 mIU/mL 943 97.8% (96.6%, 98.6%) 2966.0 (2793.4, 3149.2) 943 99.4% (98.6%, 99.8%) 5919.3 (5486.2, 6386.6) Mumps ≥OD Cutoff (ELISA antibody units) 920 98.7% (97.7%, 99.3%) 106.7 (99.1, 114.8) 920 99.9% (99.4%, 100%) 253.1 (237.9, 269.2) Rubella ≥10 IU/mL 937 97.7% (96.5%, 98.5%) 91.1 (85.9, 96.6) 937 98.3% (97.2%, 99.0%) 158.8 (149.1, 169.2) Varicella <1.25 to ≥5 gpELISA units 864 86.6% (84.1%, 88.8%) 11.6 (10.9, 12.3) 864 99.4% (98.7%, 99.8%) 477.5 (437.8, 520.7) ≥OD Cutoff (gpELISA units) 695 87.2% (84.5%, 89.6%) 11.6 (10.9, 12.4) 695 99.4% (98.5%, 99.8%) 478.7 (434.8, 527.1) Immunogenicity in Children 4 to 6 Years of Age Who Received a First Dose of ProQuad After Primary Vaccination With M-M-R II and VARIVAX
In a clinical trial, 799 healthy 4- to 6-year-old children who had received M-M-R II and VARIVAX at least 1 month prior to study entry were randomized to receive ProQuad subcutaneously and placebo (N=399), M-M-R II and placebo concomitantly at separate injection sites (N=205), or M-M-R II and VARIVAX concomitantly at separate injection sites (N=195). Children were eligible if they were previously administered primary doses of M-M-R II and VARIVAX, either concomitantly or non-concomitantly, at 12 months of age or older. Children were excluded if they were recently exposed to measles, mumps, rubella, and/or varicella, had an immune impairment, or had a history of allergy to components of the vaccine(s). No concomitant vaccines were permitted during study participation [see Adverse Reactions (6.1) for ethnicity and gender information].
A summary of antibody responses to measles, mumps, rubella, and varicella at 6 weeks postvaccination in subjects who had previously received M-M-R II and VARIVAX is shown in Table 14. Results from this study showed that a first dose of ProQuad after primary vaccination with M-M-R II and VARIVAX elicited a positive antibody response to all four antigens in greater than 98% of subjects. Postvaccination GMTs for recipients of ProQuad were similar to those following a second dose of M-M-R II and VARIVAX administered concomitantly at separate injection sites (the lower bound of the 95% CI around the fold difference in measles, mumps, rubella, and varicella GMTs excluded 0.5). Additionally, GMTs for measles, mumps, and rubella were similar to those following a second dose of M-M-R II given concomitantly with placebo (the lower bound of the 95% CI around the fold difference for the comparison of measles, mumps, and rubella GMTs excluded 0.5).
Table 14: Summary of Antibody Responses to Measles, Mumps, Rubella, and Varicella at 6 Weeks Postvaccination in Subjects 4 to 6 Years of Age Who Had Previously Received M-M-R II and VARIVAX (Per-Protocol Population) Group Number GMT
(95% CI)Seropositivity Rate
(95% CI)% ≥4-Fold Rise in Titer
(95% CI)Geometric Mean Fold Rise
(95% CI)(Description) n Measles* gpELISA = Glycoprotein enzyme-linked immunosorbent assay; ELISA = Enzyme-linked immunosorbent assay; CI = Confidence interval; GMT = Geometric mean titer; N/A = Not applicable; N = Number of subjects vaccinated; n = number of subjects in the per-protocol analysis. - *
- Measles GMTs are reported in mIU/mL; seropositivity corresponds to ≥120 mIU/mL.
- †
- Mumps GMTs are reported in mumps Ab units/mL; seropositivity corresponds to ≥10 Ab units/mL.
- ‡
- Rubella titers obtained by the legacy format were converted to their corresponding titers in the modified format. Rubella serostatus was determined after the conversion to IU/mL: seropositivity corresponds to ≥10 IU/mL.
- §
- Varicella GMTs are reported in gpELISA units/mL; seropositivity rate is reported by % of subjects with postvaccination antibody titers ≥5 gpELISA units/mL. Percentages are calculated as the number of subjects who met the criterion divided by the number of subjects contributing to the per-protocol analysis.
Group 1 (N=399) 367 1985.9 100% 4.9% 1.21 (ProQuad + placebo) (1817.6, 2169.9) (99.0%, 100%) (2.9%, 7.6%) (1.13, 1.30) Group 2 (N=205) 185 2046.9 100% 4.3% 1.28 (M-M-R II + placebo) (1815.2, 2308.2) (98.0%, 100%) (1.9%, 8.3%) (1.17, 1.40) Group 3 (N=195) 171 2084.3 99.4% 4.7% 1.31 (M-M-R II + VARIVAX) (1852.3, 2345.5) (96.8%, 100%) (2.0%, 9.0%) (1.17, 1.46) Mumps† Group 1 (N=399) 367 206.0 99.5% 27.2% 2.43 (ProQuad + placebo) (188.2, 225.4) (98.0%, 99.9%) (22.8%, 32.1%) (2.19, 2.69) Group 2 (N=205) 185 308.5 100% 41.1% 3.69 (M-M-R II + placebo) (269.6, 352.9) (98.0%, 100%) (33.9%, 48.5%) (3.14, 4.32) Group 3 (N=195) 171 295.9 100% 41.5% 3.36 (M-M-R II + VARIVAX) (262.5, 333.5) (97.9%, 100%) (34.0%, 49.3%) (2.84, 3.97) Rubella‡ Group 1 (N=399) 367 217.3 100% 32.7% 3.00 (ProQuad + placebo) (200.1, 236.0) (99.0%, 100%) (27.9%, 37.8%) (2.72, 3.31) Group 2 (N=205) 185 174.0 100% 31.9% 2.81 (M-M-R II + placebo) (157.3, 192.6) (98.0%, 100%) (25.2%, 39.1%) (2.41, 3.27) Group 3 (N=195) 171 154.1 99.4% 26.9% 2.47 (M-M-R II + VARIVAX) (138.9, 170.9) (96.8%, 100%) (20.4%, 34.2%) (2.17, 2.81) Varicella§ Group 1 (N=399) 367 322.2 98.9% 80.7% 12.43 (ProQuad + placebo) (278.9, 372.2) (97.2%, 99.7%) (76.2%, 84.6%) (10.63, 14.53) Group 2 (N=205)
(M-M-R II + placebo)185 N/A N/A N/A N/A Group 3 (N=195) 171 209.3 99.4% 71.9% 8.50 (M-M-R II + VARIVAX) (171.2, 255.9) (96.8%, 100%) (64.6%, 78.5%) (6.69, 10.81) Immunogenicity Following 2 Doses of ProQuad Administered Intramuscularly or Subcutaneously
In an open label clinical trial (NCT00402831) 405 children 12 through 18 months of age received two doses of ProQuad, administered 30 days apart (a non-US licensed interval), either intramuscularly (n=202) or subcutaneously (n=203). Antibody responses to measles, mumps, rubella and varicella viruses were measured by ELISAs using sera obtained 30 days post-dose 1, and 6-weeks post-dose 2. For anti-measles virus, anti-mumps virus, anti-rubella virus and anti-varicella virus, seroresponse rates were defined as the percentage of children seronegative at baseline who achieved antibody titers above the respective seroresponse threshold for each assay 30 days post-dose 1 and 6 weeks post-dose 2. Seroresponse thresholds were defined as 255 mIU/mL, 10 EU/mL, 10 IU/mL and 5 gpELISA units for anti-measles virus, anti-mumps virus, anti-rubella virus and anti-varicella virus antibodies, respectively after each dose. For each vaccine antigen at least 87% of enrolled children were seronegative at baseline.
The seroresponse rates to measles, mumps, and varicella viruses after dose 1 were noninferior in the intramuscular group compared to the subcutaneous group in a post hoc analysis (lower bound of the 95% confidence interval for the difference in seroresponse rates [intramuscular group minus subcutaneous group] ≥-5%). The seroresponse rate to rubella virus narrowly missed meeting the criterion for noninferiority (lower bounds of the 95% CI for the difference in seroresponse rate -5.5%). For measles, mumps, rubella, and varicella antigens, the lower bound of the 95% CI of the seroresponse rate was ˃90% after intramuscular administration. The proportions of children achieving antibody titers above the seroresponse thresholds for measles, mumps, rubella and varicella viruses after dose 1 were as follows: 100%, 97.4%, 98.4%, and 98.6%, respectively, in the intramuscular group and 97.3%, 91.3%, 100%, and 98.5%, respectively, in the subcutaneous group.
Immunogenicity Following Concomitant Use with Other Vaccines
ProQuad with Pneumococcal 7-valent Conjugate Vaccine and/or VAQTA
In a clinical trial, 1027 healthy children 12 to 15 months of age were randomized to receive ProQuad subcutaneously and pneumococcal 7-valent conjugate vaccine concomitantly (N=510) at separate injection sites or ProQuad administered subcutaneously and pneumococcal 7-valent conjugate vaccine non-concomitantly (N=517) at separate clinic visits [see Adverse Reactions (6.1) for ethnicity and gender information]. The statistical analysis of non-inferiority in antibody response rates to measles, mumps, rubella, and varicella at 6 weeks postvaccination for subjects are shown in Table 15. In the per-protocol population, seroconversion rates were not inferior in children given ProQuad and pneumococcal 7-valent conjugate vaccine concomitantly when compared to seroconversion rates seen in children given these vaccines non-concomitantly for measles, mumps, and rubella. In children with baseline varicella antibody titers <1.25 gpELISA units/mL, the varicella seroprotection rates were not inferior when rates after concomitant and non-concomitant vaccination were compared 6 weeks postvaccination. Statistical analysis of non-inferiority in GMTs to S. pneumoniae serotypes at 6 weeks postvaccination are shown in Table 16. Geometric mean antibody titers (GMTs) for S. pneumoniae types 4, 6B, 9V, 14, 18C, 19F, and 23F were not inferior when antibody titers in the concomitant and non-concomitant groups were compared 6 weeks postvaccination.
Table 15: Statistical Analysis of Non-Inferiority in Antibody Response Rates to Measles, Mumps, Rubella, and Varicella at 6 Weeks Postvaccination for Subjects Initially Seronegative to Measles, Mumps, or Rubella, or With Varicella Antibody Titer <1.25 gpELISA units at Baseline in the ProQuad + PCV7* Treatment Group and the ProQuad Followed by PCV7 Control Group (Per-Protocol Analysis) ProQuad + PCV7
(N=510)ProQuad followed by PCV7
(N=259)Difference Assay
Parametern Estimated Response† n Estimated Response† (percentage points)†,‡ (95% CI) N = Number of subjects vaccinated in each treatment group.
n = Number of subjects with measles antibody titer <255 mIU/mL, mumps antibody titer <10 ELISA Ab units/mL, rubella antibody titer <10 IU/mL, or varicella antibody titer <1.25 gpELISA units/mL at baseline and with postvaccination serology contributing to the per-protocol analysis.
Ab = antibody; ELISA = Enzyme-linked immunosorbent assay; gpELISA = Glycoprotein enzyme-linked immunosorbent assay; CI = Confidence interval.- *
- PCV7 = Pneumococcal 7-valent conjugate vaccine.
Seronegative defined as baseline measles antibody titer <255 mIU/mL for measles, baseline mumps antibody titer <10 ELISA Ab units/mL for mumps, and baseline rubella antibody titer <10 IU/mL for rubella. - †
- Estimated responses and their differences were based on statistical analysis models adjusting for study center.
- ‡
- ProQuad + PCV7 - ProQuad followed by PCV7.
The conclusion of non-inferiority is based on the lower bound of the 2-sided 95% CI on the risk difference being greater than -10 percentage points (i.e., excluding a decrease equal to or more than the prespecified criterion of 10.0 percentage points). This indicates that the difference is statistically significantly less than the prespecified clinically relevant decrease of 10.0 percentage points at the 1-sided alpha = 0.025 level.
Measles
% ≥255 mIU/mL406 97.3% 204 99.5% -2.2 (-4.6, 0.2) Mumps
% ≥10 Ab units/mL403 96.6% 208 98.6% -1.9 (-4.5, 1.0) Rubella
% ≥10 IU/mL377 98.7% 195 97.9% 0.9 (-1.3, 4.1) Varicella
% ≥5 gpELISA units/mL379 92.5% 192 87.9% 4.5 (-0.4, 10.4) Table 16: Statistical Analysis of Non-Inferiority in GMTs to S. pneumoniae Serotypes at 6 Weeks Postvaccination in the ProQuad + PCV7* Treatment Group and the PCV7 Followed by ProQuad Control Group (Per-Protocol Analysis) Group 1
ProQuad + PCV7 (N=510)Group 2
PCV7 followed by ProQuad (N=258)Serotype Parameter n Estimated Response† n Estimated Response† Fold-Difference*,‡ (95% CI) N = Number of subjects vaccinated in each treatment group; n = Number of subjects contributing to the per-protocol analysis for the given serotype; GMT = geometric mean titer; CI = Confidence interval. - *
- PCV7 = Pneumococcal 7-valent conjugate vaccine.
- †
- Estimated responses and their fold-difference were based on statistical analysis models adjusting for study center and prevaccination titer.
- ‡
- ProQuad + PCV7 / PCV7 followed by ProQuad.
The conclusion of non-inferiority is based on the lower bound of the 2-sided 95% CI on the fold-difference being greater than 0.5, (i.e., excluding a decrease of 2-fold or more). This indicates that the fold-difference is statistically significantly less than the pre-specified clinically relevant 2-fold difference at the 1-sided alpha = 0.025 level.
4 GMT 410 1.5 193 1.3 1.2 (1.0, 1.4) 6B GMT 410 8.9 192 8.4 1.1 (0.9, 1.2) 9V GMT 409 2.9 193 2.5 1.2 (1.0, 1.3) 14 GMT 408 6.5 193 5.7 1.1 (1.0, 1.3) 18C GMT 408 2.3 193 2.0 1.2 (1.0, 1.3) 19F GMT 408 3.5 192 3.1 1.1 (1.0, 1.3) 23F GMT 413 4.1 197 3.7 1.1 (1.0, 1.3) In a clinical trial, 653 healthy children 12 to 15 months of age were randomized to receive VAQTA, ProQuad subcutaneously, and pneumococcal 7-valent conjugate vaccine concomitantly (N=330) or ProQuad subcutaneously, and pneumococcal 7-valent conjugate vaccine concomitantly followed by VAQTA 6 weeks later (N=323) [see Adverse Reactions (6.1) for ethnicity and gender information]. Statistical analysis of non-inferiority of the response rate for varicella antibody at 6 weeks postvaccination among subjects who received VAQTA concomitantly or non-concomitantly with ProQuad and pneumococcal 7-valent conjugate vaccine is shown in Table 17. For the varicella component of ProQuad, in subjects with baseline antibody titers <1.25 gpELISA units/mL, the proportion with a titer ≥5 gpELISA units/mL 6 weeks after their first dose of ProQuad was non-inferior when ProQuad was administered with VAQTA and pneumococcal 7-valent conjugate vaccine as compared to the proportion with a titer ≥5 gpELISA units/mL when ProQuad was administered with pneumococcal 7-valent conjugate vaccine alone. Statistical analysis of non-inferiority of the seropositivity rate for hepatitis A antibody at 4 weeks postdose 2 of VAQTA among subjects who received VAQTA concomitantly or non-concomitantly with ProQuad and pneumococcal 7-valent conjugate vaccine is shown in Table 18. The seropositivity rate to hepatitis A 4 weeks after a second dose of VAQTA given concomitantly with ProQuad and pneumococcal 7-valent conjugate vaccine (defined as the percent of subjects with a titer ≥10 mIU/mL) was non-inferior to the seropositivity rate observed when VAQTA was administered separately from ProQuad and pneumococcal 7-valent conjugate vaccine. Statistical analysis of non-inferiority in GMT to S. pneumoniae serotypes at 6 weeks postvaccination among subjects who received VAQTA concomitantly or non-concomitantly with ProQuad and pneumococcal 7-valent conjugate vaccine is shown in Table 19. Additionally, the GMTs for S. pneumoniae types 4, 6B, 9V, 14, 18C, 19F, and 23F 6 weeks after vaccination with pneumococcal 7-valent conjugate vaccine administered concomitantly with ProQuad and VAQTA were non-inferior as compared to GMTs observed in the group given pneumococcal 7-valent conjugate vaccine with ProQuad alone. An earlier clinical study involving 617 healthy children provided data that indicated that the seroresponse rates 6 weeks post vaccination for measles, mumps, and rubella in those given M-M-R II and VAQTA concomitantly (N=309) were non-inferior as compared to historical controls.
Table 17: Statistical Analysis of Non-Inferiority of the Response Rate for Varicella Antibody at 6 Weeks Postvaccination Among Subjects Who Received VAQTA Concomitantly or Non-Concomitantly With ProQuad and PCV7* (Per-Protocol Analysis Set) Group 1: Concomitant VAQTA with ProQuad + PCV7 (N=330) Group 2: Non-concomitant VAQTA separate from ProQuad + PCV7 (N=323) Difference† (percentage points): Group 1 – Group 2 (95% CI) Parameter n Estimated Response† n Estimated Response† N = Number of subjects enrolled/randomized; n = Number of subjects contributing to the per-protocol analysis for varicella; CI = Confidence interval. - *
- PCV7 = Pneumococcal 7-valent conjugate vaccine.
- †
- Estimated responses and their differences were based on a statistical analysis model adjusting for combined study center.
- ‡
- 6 weeks following Dose 1.
- §
- Initial Serostatus <1.25 gpELISA units/ mL.
The conclusion of similarity (non-inferiority) was based on the lower bound of the 2-sided 95% CI on the risk difference excluding a decrease of 10 percentage points or more (lower bound >-10.0). This indicated that the risk difference was statistically significantly greater than the pre-specified clinically relevant difference of -10 percentage points at the 1-sided alpha = 0.025 level.
% ≥5 gpELISA units/mL‡ 225§ 93.2% 232§ 98.3% -5.1 (-9.3, -1.4) Table 18: Statistical Analysis of Non-Inferiority of the Seropositivity Rate (SPR) for Hepatitis A Antibody at 4 Weeks Postdose 2 of VAQTA Among Subjects Who Received VAQTA Concomitantly or Non-Concomitantly With ProQuad and PCV7* (Per-Protocol Analysis Set) Group 1: Concomitant VAQTA with ProQuad + PCV7
(N=330)Group 2: Non-concomitant VAQTA separate from ProQuad + PCV7 (N=323) Difference† (percentage points): Group 1 - Group 2 (95% CI) Parameter n Estimated Response† n Estimated Response† CI = Confidence interval; N = Number of subjects enrolled/randomized; n = Number of subjects contributing to the per-protocol analysis for hepatitis A. - *
- PCV7 = Pneumococcal 7-valent conjugate vaccine.
- †
- Estimated responses and their differences were based on a statistical analysis model adjusting for combined study center.
- ‡
- 4 weeks following receipt of 2 doses of VAQTA.
- §
- Regardless of initial serostatus.
The conclusion of non-inferiority was based on the lower bound of the 2-sided 95% CI on the risk difference being greater than -10 percentage points (i.e., excluding a decrease of 10 percentage points or more) (lower bound >-10.0). This indicated that the risk difference was statistically significantly greater than the pre-specified clinically relevant difference of -10 percentage points at the 1-sided alpha = 0.025 level.
% ≥10 mIU/mL‡ 182§ 100.0% 159§ 99.3% 0.7 (-1.4, 3.8) Table 19: Statistical Analysis of Non-Inferiority in Geometric Mean Titers (GMT) to S. pneumoniae Serotypes at 6 Weeks Postvaccination Among Subjects Who Received VAQTA Concomitantly or Non-Concomitantly With ProQuad and PCV7* (Per-Protocol Analysis Set) Group 1: Concomitant VAQTA with ProQuad + PCV7 (N=330) Group 2: Non-concomitant VAQTA separate from ProQuad + PCV7 (N=323) Serotype n Estimated Response† n Estimated Response† Fold-Difference†
(95% CI)CI = Confidence interval; GMT = Geometric mean titer; N = Number of subjects enrolled/randomized; n = Number of subjects contributing to the per-protocol analysis for S. pneumoniae serotypes. - *
- PCV7 = Pneumococcal 7-valent conjugate vaccine.
- †
- Estimated responses and their fold-difference were based on statistical analysis models adjusting for combined study center and prevaccination titer.
The conclusion of non-inferiority was based on the lower bound of the 2-sided 95% CI on the fold-difference being greater than 0.5 (i.e., excluding a decrease of 2-fold or more). This indicates that the fold-difference was statistically significantly less than the prespecified clinically relevant 2-fold difference at the 1-sided alpha = 0.025 level.
4 246 1.9 247 1.7 1.1 (0.9, 1.3) 6B 246 9.9 246 9.9 1.0 (0.8, 1.2) 9V 247 3.7 247 4.2 0.9 (0.8, 1.0) 14 248 7.8 247 7.6 1.0 (0.9, 1.2) 18C 247 2.9 247 2.7 1.1 (0.9, 1.3) 19F 248 4.0 248 3.8 1.1 (0.9, 1.2) 23F 247 5.1 247 4.4 1.1 (1.0, 1.3) ProQuad Administered with Diphtheria and Tetanus Toxoids and Acellular Pertussis Vaccine Adsorbed (DTaP) and Haemophilus influenzae type b Conjugate (Meningococcal Protein Conjugate) and Hepatitis B (Recombinant) Vaccine
In a clinical trial, 1913 healthy children 12 to 15 months of age were randomized to receive ProQuad subcutaneously plus diphtheria and tetanus toxoids and acellular pertussis vaccine adsorbed (DTaP) and Haemophilus influenzae type b conjugate (meningococcal protein conjugate) and hepatitis B (recombinant) vaccine concomitantly at separate injection sites (N=949), ProQuad at the initial visit followed by DTaP and Haemophilus b conjugate and hepatitis B (recombinant) vaccine given concomitantly 6 weeks later (N=485), or M-M-R II and VARIVAX given concomitantly at separate injection sites (N=479) at the first visit [see Adverse Reactions (6.1) for ethnicity and gender information]. Seroconversion rates and antibody titers for measles, mumps, rubella, varicella, anti-PRP, and hepatitis B were comparable between the 2 groups given ProQuad at approximately 6 weeks postvaccination indicating that ProQuad and Haemophilus b conjugate (meningococcal protein conjugate) and hepatitis B (recombinant) vaccine may be administered concomitantly at separate injection sites (see Table 20 below). Response rates for measles, mumps, rubella, varicella, Haemophilus influenzae type b, and hepatitis B were not inferior in children given ProQuad plus Haemophilus influenzae type b conjugate (meningococcal protein conjugate) and hepatitis B (recombinant) vaccines concomitantly when compared to ProQuad at the initial visit and Haemophilus influenzae type b conjugate (meningococcal protein conjugate) and hepatitis B (recombinant) vaccines given concomitantly 6 weeks later. There are insufficient data to support concomitant vaccination with diphtheria and tetanus toxoids and acellular pertussis vaccine adsorbed (data not shown).
Table 20: Summary of the Comparison of the Immunogenicity Endpoints for Measles, Mumps, Rubella, Varicella, Haemophilus influenzae type b, and Hepatitis B Responses Following Vaccination with ProQuad, Haemophilus influenzae type b Conjugate (Meningococcal Protein Conjugate), and Hepatitis B (Recombinant) Vaccine and DTaP Administered Concomitantly Versus Non-Concomitant Vaccination with ProQuad Followed by These Vaccines Concomitant Group Non-Concomitant Group N=949 N=485 Vaccine Antigen Parameter Response Response Risk Difference
(95% CI)Criterion for Non-inferiority HiB-PRP = Haemophilus influenzae type b, polyribosyl phosphate; HepB = hepatitis B; LB = lower bound, limit for non-inferiority comparison. Measles % ≥120 mIU/mL 97.8% 98.7% -0.9
(-2.3, 0.6)LB >-5.0 Mumps % ≥10 ELISA Ab units/mL 95.4% 95.1% 0.3
(-1.7, 2.6)LB >-5.0 Rubella % ≥10 IU/mL 98.6% 99.3% -0.7
(-1.8, 0.5)LB >-5.0 Varicella % ≥5 gpELISA units/mL 89.6% 90.8% -1.2
(-4.1, 2.0)LB >-10.0 HiB-PRP % ≥1.0 mcg/mL 94.6% 96.5% -1.9
(-4.1, 0.8)LB >-10.0 HepB % ≥10 mIU/mL 95.9% 98.8% -2.8
(-4.8, -0.8)LB >10.0 -
15 REFERENCES
- Kelso, J.M.; Jones, R.T.; Yunginger, J.W.: Anaphylaxis to measles, mumps, and rubella vaccine mediated by IgE to gelatin, J. Allergy Clin. Immunol. 91: 867-872, 1993.
- Bitnum, A.; et al: Measles Inclusion Body Encephalitis Caused by the Vaccine Strain of Measles Virus. Clin. Infect. Dis. 29: 855-861, 1999. 5.
- Angel, J.B.; et al: Vaccine Associated Measles Pneumonitis in an Adult with AIDS. Annals of Internal Medicine, 129: 104-106, 1998.
- Levy O, et al. Disseminated varicella infection due to the vaccine strain of varicella-zoster virus, in a patient with a novel deficiency in natural killer T cells. J Infect Dis. 188(7):948-53, 2003.
- Committee on Infectious Diseases, American Academy of Pediatrics. In: Pickering LK, Baker CJ, Overturf GD, et al., eds. Red Book: 2003 Report of the Committee on Infectious Diseases. 26th ed. Elk Grove Village, IL: American Academy of Pediatrics. 419-29, 2003.
- Cecinati V, et al. Vaccine administration and the development of immune thrombocytopenic purpura in children. Human Vaccines & Immunotherapeutics 9:5, 2013.
- Mantadakis E, Farmaki E, Buchanan GR. Thrombocytopenic Purpura after Measles-Mumps-Rubella Vaccination: A Systematic Review of the Literature and Guidance for Management J Ped 156 (4): 2010.
- Andrews N, Stowe J, Miller E, Svanstrom H, Johansen K, Bonhoeffer J, et al. A collaborative approach to investigating the risk of thrombocytopenic purpura after measles-mumps-rubella vaccination in England and Denmark. Vaccine. 2012;30:3042-6.
- Rubella Prevention: Recommendation of the Immunization Practices Advisory Committee (ACIP), MMWR 39(RR-15): 1-18, November 23, 1990.
- Peter, G.; et al (eds): Report of the Committee on Infectious Diseases, Twenty-fourth Edition, American Academy of Pediatrics, 344-357, 1997.
- Measles Prevention: Recommendations of the Immunization Practices Advisory Committee (ACIP), MMWR 38(S-9): 5-22, December 29, 1989.
- Recommendations of the Immunization Practices Advisory Committee (ACIP), Mumps Prevention. MMWR. 38(22):388-392, 397-400, 1989.
- Rubella vaccination during pregnancy--United States, 1971-1986. MMWR Morb Mortal Wkly Rep. 36(28):457-61, 1987.
- Rynn L, Cragan J, Correa A. Update on overall prevalence of major birth defects Atlanta, 1978-2005. CDC MMWR. 57(01):1-5, January 11, 2008.
- American College of Obstetricians and Gynecologists Frequently Asked Questions: Miscarriage and Molar Pregnancy, 2011.
- Bohlke K, Galil K, Jackson LA, et al. Postpartum varicella vaccination: Is the vaccine virus excreted in breast milk? Obstetrics and Gynecology. 102(5):970-977, 2003.
- Dolbear GL, Moffat J, Falkner C and Wojtowycz M. A Pilot Study: Is attenuated varicella virus present in breast milk after postpartum immunization? Obstetrics and Gynecology. 101(4 Suppl.):47S-47S, 2003.
- Weibel RE, et al. Clinical and laboratory studies of combined live measles, mumps, and rubella vaccines using the RA 27/3 rubella virus. Proc Soc Exp Biol Med. 165(2):323-326, 1980.
- Watson, J.C.; Pearson, J.S.; Erdman, D.D.; et al: An Evaluation of Measles Revaccination Among School-Entry Age Children, 31st Interscience Conference on Antimicrobial Agents and Chemotherapy, Abstract #268, 143, 1991.
- Unpublished data from the files of Research Laboratories of Merck Sharp & Dohme LLC, Rahway, NJ, USA.
- Davidkin, I.; Jokinen, S.; Broman, M. et al.: Persistence of Measles, Mumps, and Rubella Antibodies in an MMR-Vaccinated Cohort: A 20-Year Follow-up, JID 197:950–6, April 2008.
- LeBaron, W.; Beeler J.; Sullivan, B.; et al.: Persistence of Measles Antibodies After 2 Doses of Measles Vaccine in a Postelimination Environment, Arch Pediatr Adolesc Med. 161:294-301, March 2007.
- LeBaron, C.; Forghani, B.; Beck, C. et al.: Persistence of Mumps Antibodies after 2 Doses of Measles-Mumps-Rubella Vaccine, JID 199:552– 60 , February 2009.
- LeBaron, W.; Forghani, B.; Matter, L. et al.: Persistence of Rubella Antibodies after 2 Doses of Measles-Mumps-Rubella Vaccine, JID 200:888–99, September 2009.
- Hilleman MR, Stokes J, Jr., Buynak EB, Weibel R, Halenda R, Goldner H. Studies of live attenuated measles virus vaccine in man: II. appraisal of efficacy. Am J Public Health. 52(2):44-56, 1962.
- Krugman S, Giles JP, Jacobs AM. Studies on an attenuated measles-virus vaccine: VI. clinical, antigenic and prophylactic effects of vaccine in institutionalized children. N Engl J Med. 263(4):174-7, 1960.
- Hilleman MR, Weibel RE, Buynak EB, Stokes J, Jr., Whitman JE, Jr. Live, attenuated mumps-virus vaccine. 4. Protective efficacy as measured in a field evaluation. N Engl J Med. 276(5):252-8, 1967.
- Sugg WC, Finger JA, Levine RH, Pagano JS. Field evaluation of live virus mumps vaccine. J Pediatr. 72(4):461-6, 1968.
- The Benevento and Compobasso Pediatricians Network for the Control of Vaccine-Preventable Diseases, D'Argenio P, Citarella A, Selvaggi MTM. Field evaluation of the clinical effectiveness of vaccines against pertussis, measles, rubella and mumps. Vaccine. 16(8):818-22, 1998.
- Furukawa T, Miyata T, Kondo K, Kuno K, Isomura S, Takekoshi T. Rubella vaccination during an epidemic. JAMA. 213(6):987-90, 1970.
- Vazquez M, et al. The effectiveness of the varicella vaccine in clinical practice. N Engl J Med. 344(13):955-960, 2001.
- Kuter B, et al. Ten year follow-up of healthy children who received one or two injections of varicella vaccine. Pediatr Infect Dis J. 23(2):132-137, 2004.
-
16 HOW SUPPLIED/STORAGE AND HANDLING
ProQuad is supplied as follows:
(1) a package of 10 single-dose vials of lyophilized vaccine, NDC 0006-4171-00 (package A)
(2) a separate package of 10 prefilled syringes of sterile diluent, NDC 0006-4175-88 (package B) OR a separate package of 10 vials of sterile diluent, NDC 0006-4309-00 (package B)
Storage
Vaccine Vial
To maintain potency, ProQuad must be stored frozen between -58°F and +5°F (-50°C to -15°C). Use of dry ice may subject ProQuad to temperatures colder than -58°F (-50°C).
Before reconstitution, store the lyophilized vaccine in a freezer at a temperature between −58°F and +5°F (−50°C and −15°C) for up to 18 months. Any freezer (e.g., chest, frost-free) that reliably maintains an average temperature between −58°F and +5°F (−50°C and −15°C) and has a separate sealed freezer door is acceptable for storing ProQuad. Routine defrost cycling of a frost-free freezer is acceptable.
ProQuad may be stored at refrigerator temperature (36° to 46°F, 2° to 8°C) for up to 72 hours prior to reconstitution. Discard any ProQuad vaccine stored at 36° to 46°F which is not used within 72 hours of removal from 5°F (-15°C) storage.
Protect the vaccine from light at all times since such exposure may inactivate the vaccine viruses.
Sterile Diluent
The sterile diluent should be stored at room temperature (68° to 77°F, 20° to 25°C), or in a refrigerator (36° to 46°F, 2° to 8°C).
IF NOT USED IMMEDIATELY, THE RECONSTITUTED VACCINE MAY BE STORED AT ROOM TEMPERATURE, PROTECTED FROM LIGHT, FOR UP TO 30 MINUTES.
DISCARD RECONSTITUTED VACCINE IF IT IS NOT USED WITHIN 30 MINUTES.
DO NOT FREEZE RECONSTITUTED VACCINE.
For information regarding the product or questions regarding storage conditions, call 1-800-637-2590.
-
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Patient Information).
Instructions
Provide the required vaccine information to the patient, parent, or guardian.
Inform the patient, parent, or guardian of the benefits and risks associated with vaccination.
Inform the patient, parent, or guardian that the vaccine recipient should avoid use of salicylates for 6 weeks after vaccination with ProQuad [see Warnings and Precautions (5.8) and Drug Interactions (7.2)].
Instruct postpubertal females to avoid pregnancy for 3 months following vaccination [see Indications and Usage (1), Contraindications (4.5) and Use in Specific Populations (8.1)].
Inform patients, parents, or guardians that vaccination with ProQuad may not offer 100% protection from measles, mumps, rubella, and varicella infection.
Instruct patients, parents, or guardians to report any adverse reactions to their health care provider. The U.S. Department of Health and Human Services has established a Vaccine Adverse Event Reporting System (VAERS) to accept all reports of suspected adverse events after the administration of any vaccine, including but not limited to the reporting of events required by the National Childhood Vaccine Injury Act of 1986. For information or a copy of the vaccine reporting form, call the VAERS toll-free number at 1-800-822-7967, or report online at www.vaers.hhs.gov .
-
SPL UNCLASSIFIED SECTION
Dist. by: Merck Sharp & Dohme LLC
Rahway, NJ 07065, USAFor patent information: www.msd.com/research/patent
Copyright © 2005-2023 Merck & Co., Inc., Rahway, NJ, USA, and its affiliates.
All rights reserved.uspi-v221-i-fro-rha-2308r015
-
PATIENT PACKAGE INSERT
Patient Information
ProQuad® (pronounced “pro kwod”)
Measles, Mumps, Rubella, Varicella Virus Vaccine Live
Frozen FormulationThis is a summary of information about ProQuad®. You should read it before your child receives each dose of the vaccine. If you have any questions about the vaccine after reading this leaflet, you should ask your healthcare provider. This information does not take the place of talking about ProQuad with your healthcare provider.
What is ProQuad?
- ProQuad is a vaccine that helps prevent measles (rubeola), mumps, rubella (German measles), and chickenpox (varicella).
- It is for children 12 months to 12 years of age.
- ProQuad contains weakened live forms of measles virus, mumps virus, rubella virus, and chickenpox virus.
- ProQuad works by helping the immune system protect your child from getting measles, mumps, rubella, or chickenpox.
- ProQuad may not protect everyone who gets the vaccine.
- ProQuad does not treat measles, mumps, rubella, or chickenpox once your child has them.
What are measles, mumps, rubella, and chickenpox?
Measles is also known as rubeola. It is a serious illness. Measles virus can be passed to others if you have it. Measles can give you a high fever, cough, and a rash. The illness can last for 1 to 2 weeks. In rare cases, it can also cause an infection of the brain. This could lead to seizures, hearing loss, intellectual disability, and even death.
Mumps can also be passed to others. This virus can cause fever and headache. It can also make the glands under your jaw swell and be painful. The illness often lasts for several days. Sometimes, mumps can make the testicles swell and be painful. In some cases, it can cause meningitis, which is a swelling of the coverings of the brain and spinal cord.
Rubella is also known as German measles. It is often a mild illness. Rubella virus can cause a mild fever, swollen glands in the neck, pain and swelling in the joints, and a rash that lasts for a short time. It can be very dangerous if a pregnant woman catches it. Women who catch German measles when they are pregnant can have babies who are stillborn. Also, the babies may be blind or deaf, or have heart disease or intellectual disability.
Chickenpox is an illness that occurs most often in children who are 5 to 9 years old. It can be passed to others. The illness can include headache, fever, and general discomfort. Then an itchy rash occurs, which can turn into blisters. The most common complication is that the blisters can get infected. Less common but very serious complications can occur. These include pneumonia, inflammation of the brain, Reye syndrome (which affects the liver and the brain), and death. Severe disease and serious complications are more likely to occur in adolescents and adults.
Who should not get ProQuad?
Your child should not get ProQuad if he or she:
- is allergic to ProQuad or any of its ingredients. This includes gelatin or neomycin. (See the ingredient list at the end of this leaflet.)
- has a weakened immune system (which includes taking high doses of steroids by mouth or in a shot).
- has a fever.
- has active tuberculosis that is not treated.
- is pregnant or plans to get pregnant within the next 3 months.
What should I tell my child’s healthcare provider before my child gets ProQuad?
Tell your healthcare provider if your child:
- has or had any medical problems.
- has a history of seizures or someone in your family has a history of seizures.
- has received blood or plasma transfusions or human serum globulin.
- takes any medicines. (This includes non-prescription medicines and dietary supplements.)
- has any allergies. (This includes allergies to neomycin or gelatin.)
- had an allergic reaction to any other vaccine.
- has or had a low blood platelet count.
- is allergic to eggs.
- has a family member with a weakened immune system.
How is ProQuad given?
ProQuad is a shot given in the arm or thigh.
Your child will get 2 doses on two different dates:
- The first shot is given at 12 to 15 months old but may be given anytime through 12 years old.
- The second shot is given at 4 to 6 years old.
There should be at least 1 month between a dose of a measles-containing vaccine and a dose of ProQuad. There should be at least 3 months between a dose of a varicella-containing vaccine and a dose of ProQuad.
Your healthcare provider will decide the best time and number of shots by using official recommendations.
If a dose is missed, your healthcare provider will let you know when your child should get it.
What should my child avoid when getting ProQuad?
Do not take aspirin or aspirin-containing products for 6 weeks after getting ProQuad.
It is possible to catch chickenpox from a person who has been vaccinated with ProQuad. For 6 weeks after getting ProQuad, your child should avoid close contact with the following:
- people who are not vaccinated or who didn’t have chickenpox.
- people who have a weakened immune system.
- pregnant women who have never had chickenpox.
- newborn babies whose mothers have never had chickenpox.
- newborn babies born at less than 28 weeks of pregnancy.
What are the possible side effects of ProQuad?
The most common side effects reported after getting ProQuad are:
- pain, tenderness, soreness, redness, or swelling at the site of the shot
- fever
- irritability
- rash (including measles-like rash and chickenpox-like rash)
If your child has any of the following problems, tell your healthcare provider right away because these may be signs of an allergic reaction:
- trouble breathing
- wheezing
- hives
- rash
If your child has any side effects that worry you or seem to get worse, tell your healthcare provider right away.
These are not all the possible side effects of ProQuad. For more information, ask your healthcare provider. Contact your healthcare provider if your child has any new or unusual symptoms after receiving ProQuad.
Report the following to your healthcare provider.
- any side effects following vaccination
- exposure to ProQuad during pregnancy
- exposure to ProQuad during the 3 months before getting pregnant
You may also report any side effects directly to the Vaccine Adverse Event Reporting System (VAERS) at 1-800-822-7967 or www.vaers.hhs.gov , or to Merck Sharp and Dohme LLC at 1-877-888-4231.
What are the ingredients of ProQuad?
Active Ingredients: weakened forms of the measles, mumps, rubella, and varicella viruses.
Inactive Ingredients: sucrose, hydrolyzed gelatin, sodium chloride, sorbitol, monosodium L-glutamate, sodium phosphate dibasic, recombinant human albumin, sodium bicarbonate, potassium phosphate monobasic, potassium chloride, potassium phosphate dibasic, and residual components from the manufacturing process: MRC-5 cells including DNA and protein, neomycin, bovine calf serum, and other buffer and media ingredients.
ProQuad does not contain any preservatives.
What else should I know about ProQuad?
If you would like more information, talk to your healthcare provider or call 1-800-622-4477.
-
SPL UNCLASSIFIED SECTION
Dist. by: Merck Sharp & Dohme LLC
Rahway, NJ 07065, USAFor patent information: www.msd.com/research/patent
Copyright © 2005-2023 Merck & Co., Inc., Rahway, NJ, USA, and its affiliates.
All rights reserved.usppi-v221-i-fro-rha-2303r001
This Patient Information has been approved by the U.S. Food and Drug Administration.
Revised: 03/2023
-
PRINCIPAL DISPLAY PANEL - 0.5 mL Vial Carton
NDC 0006-4171-00
10 Single-dose 0.5-mL VialsA
Measles, Mumps, Rubella and Varicella
Virus Vaccine Live
ProQuad®STORE FROZEN
Measles vaccine: More attenuated Enders' Edmonston strain. Chick cell tissue culture origin.
Mumps vaccine: Jeryl Lynn™ strain. Chick cell tissue culture origin.
Rubella vaccine: Wistar RA 27/3 strain. Human diploid cell (WI-38) culture origin.
Varicella vaccine: Oka/Merck strain. Human diploid cell (MRC-5) culture origin.Contains no preservative. Contains trace quantities of neomycin.
Rx only
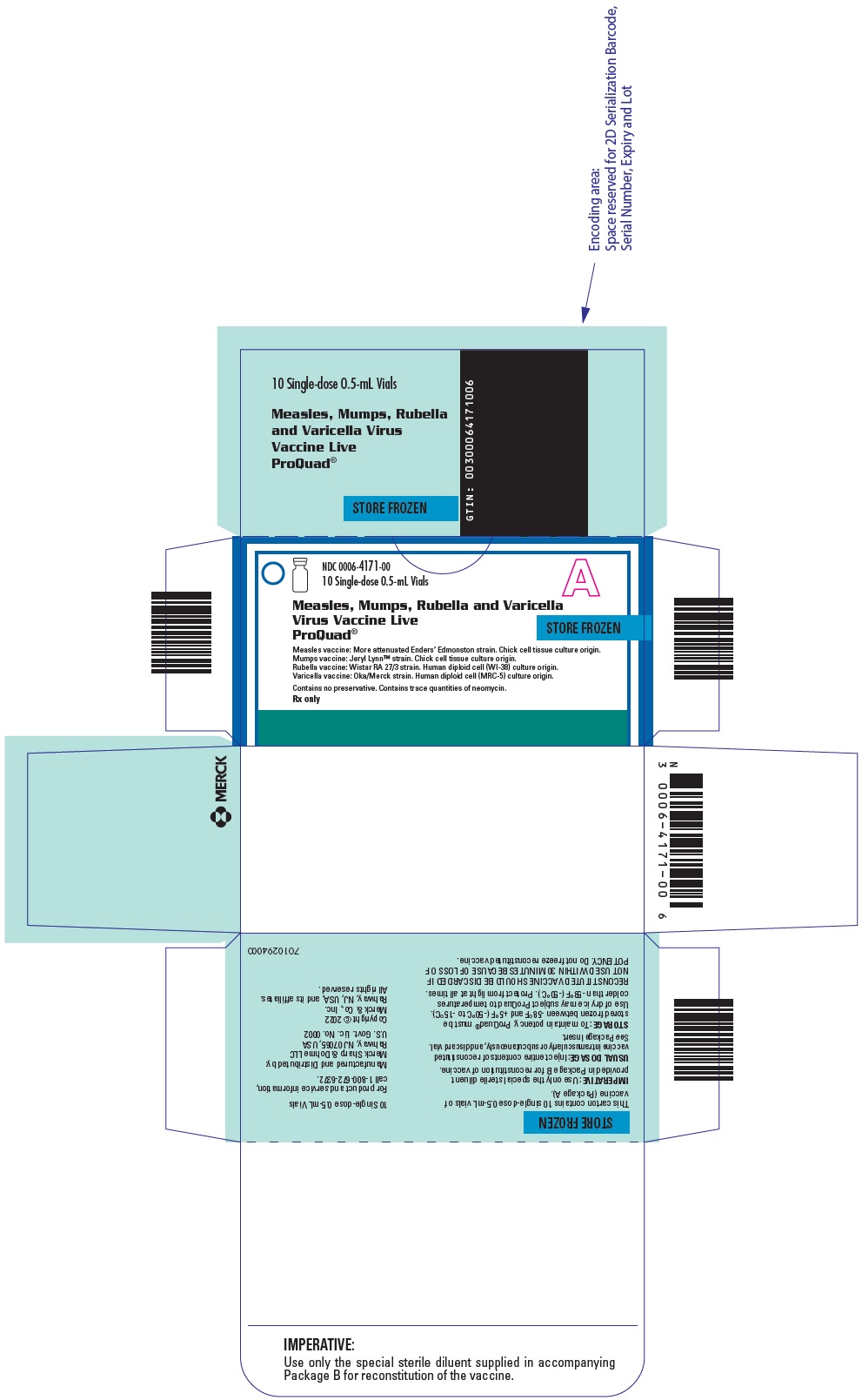
-
INGREDIENTS AND APPEARANCE
PROQUAD
measles, mumps, rubella and varicella virus vaccine live injection, powder, lyophilized, for suspensionProduct Information Product Type VACCINE Item Code (Source) NDC:0006-4171 Route of Administration SUBCUTANEOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength MEASLES VIRUS STRAIN ENDERS' ATTENUATED EDMONSTON LIVE ANTIGEN (UNII: MFZ8I7277D) (MEASLES VIRUS STRAIN ENDERS' ATTENUATED EDMONSTON LIVE ANTIGEN - UNII:MFZ8I7277D) MEASLES VIRUS STRAIN ENDERS' ATTENUATED EDMONSTON LIVE ANTIGEN 1000 [TCID_50] in 0.5 mL MUMPS VIRUS STRAIN B LEVEL JERYL LYNN LIVE ANTIGEN (UNII: 47QB6MX9KU) (MUMPS VIRUS STRAIN B LEVEL JERYL LYNN LIVE ANTIGEN - UNII:47QB6MX9KU) MUMPS VIRUS STRAIN B LEVEL JERYL LYNN LIVE ANTIGEN 20000 [TCID_50] in 0.5 mL RUBELLA VIRUS STRAIN WISTAR RA 27/3 LIVE ANTIGEN (UNII: 52202H034Z) (RUBELLA VIRUS STRAIN WISTAR RA 27/3 LIVE ANTIGEN - UNII:52202H034Z) RUBELLA VIRUS STRAIN WISTAR RA 27/3 LIVE ANTIGEN 1000 [TCID_50] in 0.5 mL VARICELLA-ZOSTER VIRUS STRAIN OKA/MERCK LIVE ANTIGEN (UNII: GPV39ZGD8C) (VARICELLA-ZOSTER VIRUS STRAIN OKA/MERCK LIVE ANTIGEN - UNII:GPV39ZGD8C) VARICELLA-ZOSTER VIRUS STRAIN OKA/MERCK LIVE ANTIGEN 9772 [PFU] in 0.5 mL Inactive Ingredients Ingredient Name Strength ALBUMIN HUMAN (UNII: ZIF514RVZR) 0.31 mg in 0.5 mL ALBUMIN BOVINE (UNII: 27432CM55Q) 0.5 ug in 0.5 mL GELATIN, UNSPECIFIED (UNII: 2G86QN327L) 11 mg in 0.5 mL MONOSODIUM GLUTAMATE (UNII: W81N5U6R6U) 0.4 mg in 0.5 mL NEOMYCIN (UNII: I16QD7X297) 16 ug in 0.5 mL POTASSIUM CHLORIDE (UNII: 660YQ98I10) 60 ug in 0.5 mL DIBASIC POTASSIUM PHOSPHATE (UNII: CI71S98N1Z) 36 ug in 0.5 mL POTASSIUM PHOSPHATE, MONOBASIC (UNII: 4J9FJ0HL51) 72 ug in 0.5 mL SODIUM BICARBONATE (UNII: 8MDF5V39QO) 0.17 mg in 0.5 mL SODIUM CHLORIDE (UNII: 451W47IQ8X) 2.4 mg in 0.5 mL SODIUM PHOSPHATE, DIBASIC, UNSPECIFIED FORM (UNII: GR686LBA74) 0.34 mg in 0.5 mL SORBITOL (UNII: 506T60A25R) 1.8 mg in 0.5 mL SUCROSE (UNII: C151H8M554) 21 mg in 0.5 mL Product Characteristics Color YELLOW, PINK (clear pale yellow to light pink) Score Shape Size Flavor Imprint Code Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:0006-4171-00 10 in 1 CARTON 1 NDC:0006-4171-01 0.5 mL in 1 VIAL, SINGLE-DOSE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date BLA BLA125108 07/01/2015 Labeler - Merck Sharp & Dohme LLC (118446553)