Label: FLUCONAZOLE tablet
- NDC Code(s): 61919-380-03, 61919-493-03
- Packager: Direct Rx
- This is a repackaged label.
- Source NDC Code(s): 68462-104, 70710-1140
- Category: HUMAN PRESCRIPTION DRUG LABEL
- DEA Schedule: None
- Marketing Status: Abbreviated New Drug Application
Drug Label Information
Updated January 9, 2024
If you are a consumer or patient please visit this version.
- Download DRUG LABEL INFO: PDF XML
- Official Label (Printer Friendly)
- INDICATIONS & USAGE
- CONTRAINDICATIONS
- WARNINGS
- PRECAUTIONS
- OVERDOSAGE
- HOW SUPPLIED
- REFERENCES
-
CLINICAL PHARMACOLOGY
Pharmacokinetics and Metabolism
The pharmacokinetic properties of fluconazole are similar following administration by the intravenous or oral routes. In normal volunteers, the bioavailability of orally administered fluconazole is over 90% compared with intravenous administration.
Peak plasma concentrations (Cmax) in fasted normal volunteers occur between 1 and 2 hours with a terminal plasma elimination half-life of approximately 30 hours (range: 20 to 50 hours) after oral administration.
In fasted normal volunteers, administration of a single oral 400 mg dose of fluconazole leads to a mean Cmax of 6.72 mcg/mL (range: 4.12 to 8.08 mcg/mL) and after single oral doses of 50 to 400 mg, fluconazole plasma concentrations and AUC (area under the plasma concentration-time curve) are dose proportional.
The Cmax and AUC data from a food-effect study involving administration of fluconazole tablets to healthy volunteers under fasting conditions and with a high-fat meal indicated that exposure to the drug is not affected by food. Therefore, fluconazole may be taken without regard to meals. (See DOSAGE AND ADMINISTRATION.)
Administration of a single oral 150 mg tablet of fluconazole to ten lactating women resulted in a mean Cmax of 2.61 mcg/mL (range: 1.57 to 3.65 mcg/mL).
Steady-state concentrations are reached within 5 to 10 days following oral doses of 50 to 400 mg given once daily. Administration of a loading dose (on day 1) of twice the usual daily dose results in plasma concentrations close to steady-state by the second day. The apparent volume of distribution of fluconazole approximates that of total body water. Plasma protein binding is low (11 to 12%). Following either single- or multiple-oral doses for up to 14 days, fluconazole penetrates into all body fluids studied (see table below). In normal volunteers, saliva concentrations of fluconazole were equal to or slightly greater than plasma concentrations regardless of dose, route, or duration of dosing. In patients with bronchiectasis, sputum concentrations of fluconazole following a single 150 mg oral dose were equal to plasma concentrations at both 4 and 24 hours post dose. In patients with fungal meningitis, fluconazole concentrations in the CSF are approximately 80% of the corresponding plasma concentrations.
A single oral 150 mg dose of fluconazole administered to 27 patients penetrated into vaginal tissue, resulting in tissue: plasma ratios ranging from 0.94 to 1.14 over the first 48 hours following dosing.
A single oral 150 mg dose of fluconazole administered to 14 patients penetrated into vaginal fluid, resulting in fluid: plasma ratios ranging from 0.36 to 0.71 over the first 72 hours following dosing.
[undefined]
* Relative to concurrent concentrations in plasma in subjects with normal renal function. † Independent of degree of meningeal inflammation.
In normal volunteers, fluconazole is cleared primarily by renal excretion, with approximately 80% of the administered dose appearing in the urine as unchanged drug. About 11% of the dose is excreted in the urine as metabolites.The pharmacokinetics of fluconazole are markedly affected by reduction in renal function. There is an inverse relationship between the elimination half-life and creatinine clearance. The dose of fluconazole may need to be reduced in patients with impaired renal function. (See DOSAGE AND ADMINISTRATION.) A 3-hour hemodialysis session decreases plasma concentrations by approximately 50%.
In normal volunteers, fluconazole administration (doses ranging from 200 mg to 400 mg once daily for up to 14 days) was associated with small and inconsistent effects on testosterone concentrations, endogenous corticosteroid concentrations, and the ACTH-stimulated cortisol response.
Pharmacokinetics in Children
In children, the following pharmacokinetic data {Mean (% cv)} have been reported:
[undefined]
Clearance corrected for body weight was not affected by age in these studies. Mean body clearance in adults is reported to be 0.23 (17%) mL/min/kg.In premature newborns (gestational age 26 to 29 weeks), the mean (%cv) clearance within 36 hours of birth was 0.180 (35%, N=7) mL/min/kg, which increased with time to a mean of 0.218 (31%, N=9) mL/min/kg six days later and 0.333 (56%, N=4) mL/min/kg 12 days later. Similarly, the half-life was 73.6 hours, which decreased with time to a mean of 53.2 hours six days later and 46.6 hours 12 days later.
Pharmacokinetics in Elderly
A pharmacokinetic study was conducted in 22 subjects, 65 years of age or older receiving a single 50 mg oral dose of fluconazole. Ten of these patients were concomitantly receiving diuretics. The Cmax was 1.54 mcg/mL and occurred at 1.3 hours post dose. The mean AUC was 76.4 + 20.3 mcg∙h/mL, and the mean terminal half-life was 46.2 hours. These pharmacokinetic parameter values are higher than analogous values reported for normal young male volunteers. Coadministration of diuretics did not significantly alter AUC or Cmax. In addition, creatinine clearance (74 mL/min), the percent of drug recovered unchanged in urine (0 to 24 hr, 22%), and the fluconazole renal clearance estimates (0.124 mL/min/kg) for the elderly were generally lower than those of younger volunteers. Thus, the alteration of fluconazole disposition in the elderly appears to be related to reduced renal function characteristic of this group. A plot of each subject's terminal elimination half-life versus creatinine clearance compared with the predicted half-life – creatinine clearance curve derived from normal subjects and subjects with varying degrees of renal insufficiency indicated that 21 of 22 subjects fell within the 95% confidence limit of the predicted half-life – creatinine clearance curves. These results are consistent with the hypothesis that higher values for the pharmacokinetic parameters observed in the elderly subjects compared with normal young male volunteers are due to the decreased kidney function that is expected in the elderly.
Drug Interaction Studies
Oral contraceptives: Oral contraceptives were administered as a single dose both before and after the oral administration of fluconazole 50 mg once daily for 10 days in 10 healthy women. There was no significant difference in ethinyl estradiol or levonorgestrel AUC after the administration of 50 mg of fluconazole. The mean increase in ethinyl estradiol AUC was 6% (range: -47 to 108%) and levonorgestrel AUC increased 17% (range: -33 to 141%).
In a second study, twenty-five normal females received daily doses of both 200 mg fluconazole tablets or placebo for two, ten-day periods. The treatment cycles were one month apart with all subjects receiving fluconazole during one cycle and placebo during the other. The order of study treatment was random. Single doses of an oral contraceptive tablet containing levonorgestrel and ethinyl estradiol were administered on the final treatment day (day 10) of both cycles. Following administration of 200 mg of fluconazole, the mean percentage increase of AUC for levonorgestrel compared to placebo was 25% (range: -12 to 82%) and the mean percentage increase for ethinyl estradiol compared to placebo was 38% (range: -11 to 101%). Both of these increases were statistically significantly different from placebo.
A third study evaluated the potential interaction of once weekly dosing of fluconazole 300 mg to 21 normal females taking an oral contraceptive containing ethinyl estradiol and norethindrone. In this placebo-controlled, double-blind, randomized, two-way crossover study carried out over three cycles of oral contraceptive treatment, fluconazole dosing resulted in small increases in the mean AUCs of ethinyl estradiol and norethindrone compared to similar placebo dosing. The mean AUCs of ethinyl estradiol and norethindrone increased by 24% (95% C.I. range: 18 to 31%) and 13% (95% C.I. range: 8 to 18%), respectively, relative to placebo. Fluconazole treatment did not cause a decrease in the ethinyl estradiol AUC of any individual subject in this study compared to placebo dosing. The individual AUC individual values of norethindrone decreased very slightly (<5%) in 3 of the 21 subjects after fluconazole treatment.
Cimetidine: Fluconazole 100 mg was administered as a single oral dose alone and two hours after a single dose of cimetidine 400 mg to six healthy male volunteers. After the administration of cimetidine, there was a significant decrease in fluconazole AUC and Cmax. There was a mean ± SD decrease in fluconazole AUC of 13% ± 11% (range: -3.4 to -31%) and Cmax decreased 19% ± 14% (range: -5 to -40%). However, the administration of cimetidine 600 mg to 900 mg intravenously over a four-hour period (from one hour before to 3 hours after a single oral dose of fluconazole 200 mg) did not affect the bioavailability or pharmacokinetics of fluconazole in 24 healthy male volunteers.
Antacid: Administration of Maalox® (20 mL) to 14 normal male volunteers immediately prior to a single dose of fluconazole 100 mg had no effect on the absorption or elimination of fluconazole.
Hydrochlorothiazide: Concomitant oral administration of 100 mg fluconazole and 50 mg hydrochlorothiazide for 10 days in 13 normal volunteers resulted in a significant increase in fluconazole AUC and Cmax compared to fluconazole given alone. There was a mean ± SD increase in fluconazole AUC and Cmax of 45% ± 31% (range: 19 to 114%) and 43% ± 31% (range: 19 to 122%), respectively. These changes are attributed to a mean ± SD reduction in renal clearance of 30% ± 12% (range: -10 to -50%).
Rifampin: Administration of a single oral 200 mg dose of fluconazole after 15 days of rifampin administered as 600 mg daily in eight healthy male volunteers resulted in a significant decrease in fluconazole AUC and a significant increase in apparent oral clearance of fluconazole. There was a mean ± SD reduction in fluconazole AUC of 23% ± 9% (range: -13 to -42%). Apparent oral clearance of fluconazole increased 32% ± 17% (range: 16 to 72%). Fluconazole half-life decreased from 33.4 ± 4.4 hours to 26.8 ± 3.9 hours. (See PRECAUTIONS.)
Warfarin: There was a significant increase in prothrombin time response (area under the prothrombin time-time curve) following a single dose of warfarin (15 mg) administered to 13 normal male volunteers following oral fluconazole 200 mg administered daily for 14 days as compared to the administration of warfarin alone. There was a mean ± SD increase in the prothrombin time response (area under the prothrombin time-time curve) of 7% ± 4% (range: -2 to 13%). (See PRECAUTIONS.) Mean is based on data from 12 subjects as one of 13 subjects experienced a 2-fold increase in his prothrombin time response.
Phenytoin: Phenytoin AUC was determined after 4 days of phenytoin dosing (200 mg daily, orally for 3 days followed by 250 mg intravenously for one dose) both with and without the administration of fluconazole (oral fluconazole 200 mg daily for 16 days) in 10 normal male volunteers. There was a significant increase in phenytoin AUC. The mean ± SD increase in phenytoin AUC was 88% ± 68% (range: 16 to 247%). The absolute magnitude of this interaction is unknown because of the intrinsically nonlinear disposition of phenytoin. (See PRECAUTIONS.)
Cyclosporine: Cyclosporine AUC and Cmax were determined before and after the administration of fluconazole 200 mg daily for 14 days in eight renal transplant patients who had been on cyclosporine therapy for at least 6 months and on a stable cyclosporine dose for at least 6 weeks. There was a significant increase in cyclosporine AUC, Cmax, Cmin (24-hour concentration), and a significant reduction in apparent oral clearance following the administration of fluconazole. The mean ± SD increase in AUC was 92% ± 43% (range: 18 to 147%). The Cmax increased 60% ± 48% (range: -5 to 133%). The Cmin increased 157% ± 96% (range: 33 to 360%). The apparent oral clearance decreased 45% ± 15% (range: -15 to -60%). (See PRECAUTIONS.)
Zidovudine: Plasma zidovudine concentrations were determined on two occasions (before and following fluconazole 200 mg daily for 15 days) in 13 volunteers with AIDS or ARC who were on a stable zidovudine dose for at least two weeks. There was a significant increase in zidovudine AUC following the administration of fluconazole. The mean ± SD increase in AUC was 20% ± 32% (range: -27 to 104%). The metabolite, GZDV, to parent drug ratio significantly decreased after the administration of fluconazole, from 7.6 ± 3.6 to 5.7 ± 2.2.
Theophylline: The pharmacokinetics of theophylline were determined from a single intravenous dose of aminophylline (6 mg/kg) before and after the oral administration of fluconazole 200 mg daily for 14 days in 16 normal male volunteers. There were significant increases in theophylline AUC, Cmax, and half-life with a corresponding decrease in clearance. The mean ± SD theophylline AUC increased 21% ± 16% (range: -5 to 48%). The Cmax increased 13% ± 17% (range: -13 to 40%). Theophylline clearance decreased 16% ± 11% (range: -32 to 5%). The half-life of theophylline increased from 6.6 ± 1.7 hours to 7.9 ± 1.5 hours. (See PRECAUTIONS.)
Terfenadine: Six healthy volunteers received terfenadine 60 mg BID for 15 days. Fluconazole 200 mg was administered daily from days 9 through 15. Fluconazole did not affect terfenadine plasma concentrations. Terfenadine acid metabolite AUC increased 36% ± 36% (range: 7 to 102%) from day 8 to day 15 with the concomitant administration of fluconazole. There was no change in cardiac repolarization as measured by Holter QTc intervals. Another study at a 400 mg and 800 mg daily dose of fluconazole demonstrated that fluconazole taken in doses of 400 mg per day or greater significantly increases plasma levels of terfenadine when taken concomitantly. (See CONTRAINDICATIONSand PRECAUTIONS.)
Quinidine: Although not studied in vitro or in vivo, concomitant administration of fluconazole with quinidine may result in inhibition of quinidine metabolism. Use of quinidine has been associated with QT prolongation and rare occurrences of torsades de pointes.Coadministration of fluconazole and quinidine is contraindicated.(See CONTRAINDICATIONSand PRECAUTIONS.)
Oral hypoglycemics: The effects of fluconazole on the pharmacokinetics of the sulfonylurea oral hypoglycemic agents tolbutamide, glipizide, and glyburide were evaluated in three placebo-controlled studies in normal volunteers. All subjects received the sulfonylurea alone as a single dose and again as a single dose following the administration of fluconazole 100 mg daily for 7 days. In these three studies, 22/46 (47.8%) of fluconazole treated patients and 9/22 (40.1%) of placebo treated patients experienced symptoms consistent with hypoglycemia. (See PRECAUTIONS.)
Tolbutamide: In 13 normal male volunteers, there was significant increase in tolbutamide (500 mg single dose) AUC and Cmax following the administration of fluconazole. There was a mean ± SD increase in tolbutamide AUC of 26% ± 9% (range: 12 to 39%). Tolbutamide Cmax increased 11% ± 9% (range: -6 to 27%). (See PRECAUTIONS.)
Glipizide: The AUC and Cmax of glipizide (2.5 mg single dose) were significantly increased following the administration of fluconazole in 13 normal male volunteers. There was a mean ± SD increase in AUC of 49% ± 13% (range: 27 to 73%) and an increase in Cmax of 19% ± 23% (range: -11 to 79%). (See PRECAUTIONS.)
Glyburide: The AUC and Cmax of glyburide (5 mg single dose) were significantly increased following the administration of fluconazole in 20 normal male volunteers. There was a mean ± SD increase in AUC of 44% ± 29% (range: -13 to 115%) and Cmax increased 19% ± 19% (range: -23 to 62%). Five subjects required oral glucose following the ingestion of glyburide after 7 days of fluconazole administration. (See PRECAUTIONS.)
Rifabutin: There have been published reports that an interaction exists when fluconazole is administered concomitantly with rifabutin, leading to increased serum levels of rifabutin. (See PRECAUTIONS.)
Tacrolimus: There have been published reports that an interaction exists when fluconazole is administered concomitantly with tacrolimus, leading to increased serum levels of tacrolimus. (See PRECAUTIONS.)
Cisapride: A placebo-controlled, randomized, multiple-dose study examined the potential interaction of fluconazole with cisapride. Two groups of 10 normal subjects were administered fluconazole 200 mg daily or placebo. Cisapride 20 mg four times daily was started after 7 days of fluconazole or placebo dosing. Following a single dose of fluconazole, there was a 101% increase in the cisapride AUC and a 91% increase in the cisapride Cmax. Following multiple doses of fluconazole, there was a 192% increase in the cisapride AUC and a 154% increase in the cisapride Cmax. Fluconazole significantly increased the QTc interval in subjects receiving cisapride 20 mg four times daily for 5 days. (See CONTRAINDICATIONSand PRECAUTIONS.)
Midazolam: The effect of fluconazole on the pharmacokinetics and pharmacodynamics of midazolam was examined in a randomized, cross-over study in 12 volunteers. In the study, subjects ingested placebo or 400 mg fluconazole on Day 1 followed by 200 mg daily from Day 2 to Day 6. In addition, a 7.5 mg dose of midazolam was orally ingested on the first day, 0.05 mg/kg was administered intravenously on the fourth day, and 7.5 mg orally on the sixth day. Fluconazole reduced the clearance of IV midazolam by 51%. On the first day of dosing, fluconazole increased the midazolam AUC and Cmax by 259% and 150%, respectively. On the sixth day of dosing, fluconazole increased the midazolam AUC and Cmax by 259% and 74%, respectively. The psychomotor effects of midazolam were significantly increased after oral administration of midazolam but not significantly affected following intravenous midazolam.
A second randomized, double-dummy, placebo-controlled, cross over study in three phases was performed to determine the effect of route of administration of fluconazole on the interaction between fluconazole and midazolam. In each phase the subjects were given oral fluconazole 400 mg and intravenous saline; oral placebo and intravenous fluconazole 400 mg; and oral placebo and IV saline. An oral dose of 7.5 mg of midazolam was ingested after fluconazole/placebo. The AUC and Cmax of midazolam were significantly higher after oral than IV administration of fluconazole. Oral fluconazole increased the midazolam AUC and Cmax by 272% and 129%, respectively. IV fluconazole increased the midazolam AUC and Cmax by 244% and 79%, respectively. Both oral and IV fluconazole increased the pharmacodynamic effects of midazolam. (See PRECAUTIONS.)
Azithromycin: An open-label, randomized, three-way crossover study in 18 healthy subjects assessed the effect of a single 800 mg oral dose of fluconazole on the pharmacokinetics of a single 1200 mg oral dose of azithromycin as well as the effects of azithromycin on the pharmacokinetics of fluconazole. There was no significant pharmacokinetic interaction between fluconazole and azithromycin.
Voriconazole: Voriconazole is a substrate for both CYP2C9 and CYP3A4 isoenzymes. Concurrent administration of oral Voriconazole (400 mg Q12h for 1 day, then 200 mg Q12h for 2.5 days) and oral fluconazole (400 mg on day 1, then 200 mg Q24h for 4 days) to 6 healthy male subjects resulted in an increase in Cmax and AUCt of voriconazole by an average of 57% (90% CI: 20%, 107%) and 79% (90% CI: 40%, 128%), respectively. In a follow-on clinical study involving 8 healthy male subjects, reduced dosing and/or frequency of voriconazole and fluconazole did not eliminate or diminish this effect. Concomitant administration of voriconazole and fluconazole at any dose is not recommended. Close monitoring for adverse events related to voriconazole is recommended if voriconazole is used sequentially after fluconazole, especially within 24 h of the last dose of fluconazole. (See PRECAUTIONS)
Tofacitinib: Co-administration of fluconazole (400 mg on Day 1 and 200 mg once daily for 6 days [Days 2 to 7]) and tofacitinib (30 mg single dose on Day 5) in healthy subjects resulted in increased mean tofacitinib AUC and Cmax values of approximately 79% (90% CI: 64% to 96%) and 27% (90% CI: 12% to 44%), respectively, compared to administration of tofacitinib alone. (See PRECAUTIONS)
Microbiology
Mechanism of action section
Fluconazole is a highly selective inhibitor of fungal cytochrome P450 dependent enzyme lanosterol 14-α-demethylase. This enzyme functions to convert lanosterol to ergosterol. The subsequent loss of normal sterols correlates with the accumulation of 14-α-methyl sterols in fungi and may be responsible for the fungistatic activity of fluconazole. Mammalian cell demethylation is much less sensitive to fluconazole inhibition.
Drug Resistance
Fluconazole resistance may arise from a modification in the quality or quantity of the target enzyme (lanosterol 14-α-demethylase), reduced access to the drug target, or some combination of these mechanisms.
Point mutations in the gene (ERG11) encoding for the target enzyme lead to an altered target with decreased affinity for azoles. Overexpression of ERG11 results in the production of high concentrations of the target enzyme, creating the need for higher intracellular drug concentrations to inhibit all of the enzyme molecules in the cell.
The second major mechanism of drug resistance involves active efflux of fluconazole out of the cell through the activation of two types of multidrug efflux transporters; the major facilitators (encoded by MDR genes) and those of the ATP-binding cassette superfamily (encoded by CDR genes). Upregulation of the MDR gene leads to fluconazole resistance, whereas, upregulation of CDR genes may lead to resistance to multiple azoles.
Resistance in Candida glabrata usually includes upregulation of CDR genes resulting in resistance to multiple azoles. For an isolate where the MIC is categorized as Intermediate (16 to 32 mcg/mL), the highest fluconazole dose is recommended.
Candida krusei should be considered to be resistant to fluconazole. Resistance in C. krusei appears to be mediated by reduced sensitivity of the target enzyme to inhibition by the agent.
There have been reports of cases of superinfection with Candida species other than C. albicans, which are often inherently not susceptible to fluconazole (e.g., Candida krusei). Such cases may require alternative antifungal therapy.
Activity In Vitro and In Clinical Infections
Fluconazole has been shown to be active against most strains of the following microorganisms both in vitro and in clinical infections.
Candida albicans
Candida glabrata (Many strains are intermediately susceptible)*
Candida parapsilosis
Candida tropicalis
Cryptococcus neoformans
* In a majority of the studies, fluconazole MIC90 values against C. glabrata were above the susceptible breakpoint (≥16 mcg/ml). Resistance in Candida glabrata usually includes upregulation of CDR genes resulting in resistance to multiple azoles. For an isolate where the MIC is categorized as intermediate (16 to 32 mcg/mL, see Table 1), the highest dose is recommended (see DOSAGE AND ADMINISTRATION). For resistant isolates alternative therapy is recommended.
The following in vitro data are available, but their clinical significance is unknown.
Fluconazole exhibits in vitro minimum inhibitory concentrations (MIC values) of 8 mcg/mL or less against most (≥90%) strains of the following microorganisms, however, the safety and effectiveness of fluconazole in treating clinical infections due to these microorganisms have not been established in adequate and well-controlled trials.
Candida dubliniensis
Candida guilliermondii
Candida kefyr
Candida lusitaniae
Candida krusei should be considered to be resistant to fluconazole. Resistance in C. krusei appears to be mediated by reduced sensitivity of the target enzyme to inhibition by the agent.
There have been reports of cases of superinfection with Candida species other than C. albicans, which are often inherently not susceptible to fluconazole (e.g., Candida krusei). Such cases may require alternative antifungal therapy.
Susceptibility Testing Methods
Cryptococcus neoformans and filamentous fungi:
No interpretive criteria have been established for Cryptococcus neoformans and filamentous fungi.
Candida species:
Broth Dilution Techniques: Quantitative methods are used to determine antifungal minimum inhibitory concentrations (MICs). These MICs provide estimates of the susceptibility of Candida spp. to antifungal agents. MICs should be determined using a standardized procedure. Standardized procedures are based on a dilution method (broth)1 with standardized inoculum concentrations of fluconazole powder. The MIC values should be interpreted according to the criteria provided in Table 1.
Diffusion Techniques: Qualitative methods that require measurement of zone diameters also provide reproducible estimates of the susceptibility of Candida spp. to an antifungal agent. One such standardized procedure2 requires the use of standardized inoculum concentrations. This procedure uses paper disks impregnated with 25 mcg of fluconazole to test the susceptibility of yeasts to fluconazole. Disk diffusion interpretive criteria are also provided in Table 1.
Table 1: Susceptibility Interpretive Criteria for Fluconazole
[undefined]
* Isolates of C. krusei are assumed to be intrinsically resistant to fluconazole and their MICs and/or zone diameters should not be interpreted using this scale.** The intermediate category is sometimes called Susceptible-Dose Dependent (SDD) and both categories are equivalent for fluconazole.
The susceptible category implies that isolates are inhibited by the usually achievable concentrations of antifungal agent tested when the recommended dosage is used. The intermediate category implies that an infection due to the isolate may be appropriately treated in body sites where the drugs are physiologically concentrated or when a high dosage of drug is used. The resistant category implies that isolates are not inhibited by the usually achievable concentrations of the agent with normal dosage schedules and clinical efficacy of the agent against the isolate has not been reliably shown in treatment studies.
Quality Control
Standardized susceptibility test procedures require the use of quality control organisms to control the technical aspects of the test procedures. Standardized fluconazole powder and 25 mcg disks should provide the following range of values noted in Table 2. NOTE: Quality control microorganisms are specific strains of organisms with intrinsic biological properties relating to resistance mechanisms and their genetic expression within fungi; the specific strains used for microbiological control are not clinically significant.
Table 2: Acceptable Quality Control Ranges for Fluconazole to be Used in Validation of Susceptibility Test Results
[undefined]
---* Quality control ranges have not been established for this strain/antifungal agent combination due to their extensive interlaboratory variation during initial quality control studies.
-
CLINICAL STUDIES
Cryptococcal MeningitisIn a multicenter study comparing fluconazole (200 mg/day) to amphotericin B (0.3 mg/kg/day) for treatment of cryptococcal meningitis in patients with AIDS, a multivariate analysis revealed three pretreatment factors that predicted death during the course of therapy: abnormal mental status, cerebrospinal fluid cryptococcal antigen titer greater than 1:1024, and cerebrospinal fluid white blood cell count of less than 20 cells/mm3. Mortality among high risk patients was 33% and 40% for amphotericin B and fluconazole patients, respectively (p=0.58), with overall deaths 14% (9 of 63 subjects) and 18% (24 of 131 subjects) for the 2 arms of the study (p=0.48). Optimal doses and regimens for patients with acute cryptococcal meningitis and at high risk for treatment failure remain to be determined. (Saag, et al. N Engl J Med 1992; 326:83-9.)
Vaginal Candidiasis
Two adequate and well-controlled studies were conducted in the U.S. using the 150 mg tablet. In both, the results of the fluconazole regimen were comparable to the control regimen (clotrimazole or miconazole intravaginally for 7 days) both clinically and statistically at the one month post-treatment evaluation.
The therapeutic cure rate, defined as a complete resolution of signs and symptoms of vaginal candidiasis (clinical cure), along with a negative KOH examination and negative culture for Candida (microbiologic eradication), was 55% in both the fluconazole group and the vaginal products group.
[undefined]
Approximately three-fourths of the enrolled patients had acute vaginitis (<4 episodes/12 months) and achieved 80% clinical cure, 67% mycologic eradication, and 59% therapeutic cure when treated with a 150 mg fluconazole tablet administered orally. These rates were comparable to control products. The remaining one-fourth of enrolled patients had recurrent vaginitis (≥4 episodes/12 months) and achieved 57% clinical cure, 47% mycologic eradication, and 40% therapeutic cure. The numbers are too small to make meaningful clinical or statistical comparisons with vaginal products in the treatment of patients with recurrent vaginitis.
Substantially more gastrointestinal events were reported in the fluconazole group compared to the vaginal product group. Most of the events were mild to moderate. Because fluconazole was given as a single dose, no discontinuations occurred.
[undefined]
Pediatric Studies
Oropharyngeal Candidiasis: An open-label, comparative study of the efficacy and safety of fluconazole (2 to 3 mg/kg/day) and oral nystatin (400,000 I.U. 4 times daily) in immunocompromised children with oropharyngeal candidiasis was conducted. Clinical and mycological response rates were higher in the children treated with fluconazole.
Clinical cure at the end of treatment was reported for 86% of fluconazole treated patients compared to 46% of nystatin treated patients. Mycologically, 76% of fluconazole treated patients had the infecting organism eradicated compared to 11% for nystatin treated patients.
[undefined]
The proportion of patients with clinical relapse 2 weeks after the end of treatment was 14% for subjects receiving fluconazole and 16% for subjects receiving nystatin. At 4 weeks after the end of treatment, the percentages of patients with clinical relapse were 22% for fluconazole and 23% for nystatin.
-
ADVERSE REACTIONS
Fluconazole is generally well tolerated.
In some patients, particularly those with serious underlying diseases such as AIDS and cancer, changes in renal and hematological function test results and hepatic abnormalities have been observed during treatment with fluconazole and comparative agents, but the clinical significance and relationship to treatment is uncertain.
In Patients Receiving a Single Dose for Vaginal Candidiasis
During comparative clinical studies conducted in the United States, 448 patients with vaginal candidiasis were treated with fluconazole, 150 mg single dose. The overall incidence of side effects possibly related to fluconazole was 26%. In 422 patients receiving active comparative agents, the incidence was 16%. The most common treatment-related adverse events reported in the patients who received 150 mg single dose fluconazole for vaginitis were headache (13%), nausea (7%), and abdominal pain (6%). Other side effects reported with an incidence equal to or greater than 1% included diarrhea (3%), dyspepsia (1%), dizziness (1%), and taste perversion (1%). Most of the reported side effects were mild to moderate in severity. Rarely, angioedema and anaphylactic reaction have been reported in marketing experience.
In Patients Receiving Multiple Doses for Other Infections
Sixteen percent of over 4000 patients treated with fluconazole in clinical trials of 7 days or more experienced adverse events. Treatment was discontinued in 1.5% of patients due to adverse clinical events and in 1.3% of patients due to laboratory test abnormalities.
Clinical adverse events were reported more frequently in HIV infected patients (21%) than in non-HIV infected patients (13%); however, the patterns in HIV infected and non-HIV infected patients were similar. The proportions of patients discontinuing therapy due to clinical adverse events were similar in the two groups (1.5%).
The following treatment-related clinical adverse events occurred at an incidence of 1% or greater in 4048 patients receiving fluconazole for 7 or more days in clinical trials: nausea 3.7%, headache 1.9%, skin rash 1.8%, vomiting 1.7%, abdominal pain 1.7%, and diarrhea 1.5%.
Hepatobiliary: In combined clinical trials and marketing experience, there have been rare cases of serious hepatic reactions during treatment with fluconazole. (See WARNINGS.) The spectrum of these hepatic reactions has ranged from mild transient elevations in transaminases to clinical hepatitis, cholestasis and fulminant hepatic failure, including fatalities. Instances of fatal hepatic reactions were noted to occur primarily in patients with serious underlying medical conditions (predominantly AIDS or malignancy) and often while taking multiple concomitant medications. Transient hepatic reactions, including hepatitis and jaundice, have occurred among patients with no other identifiable risk factors. In each of these cases, liver function returned to baseline on discontinuation of fluconazole.
In two comparative trials evaluating the efficacy of fluconazole for the suppression of relapse of cryptococcal meningitis, a statistically significant increase was observed in median AST (SGOT) levels from a baseline value of 30 IU/L to 41 IU/L in one trial and 34 IU/L to 66 IU/L in the other. The overall rate of serum transaminase elevations of more than 8 times the upper limit of normal was approximately 1% in fluconazole-treated patients in clinical trials. These elevations occurred in patients with severe underlying disease, predominantly AIDS or malignancies, most of whom were receiving multiple concomitant medications, including many known to be hepatotoxic. The incidence of abnormally elevated serum transaminases was greater in patients taking fluconazole concomitantly with one or more of the following medications: rifampin, phenytoin, isoniazid, valproic acid, or oral sulfonylurea hypoglycemic agents.
Post-Marketing Experience
In addition, the following adverse events have occurred during postmarketing experience.
Immunologic: In rare cases, anaphylaxis (including angioedema, face edema and pruritus) has been reported.
Body as a Whole: Asthenia, fatigue, fever, malaise. Cardiovascular: QT prolongation, torsade de pointes. (See PRECAUTIONS.)
Central Nervous System: Seizures, dizziness.
Hematopoietic and Lymphatic: Leukopenia, including neutropenia and agranulocytosis, thrombocytopenia.
Metabolic: Hypercholesterolemia, hypertriglyceridemia, hypokalemia.
Gastrointestinal: Cholestasis, dry mouth, hepatocellular damage, dyspepsia, vomiting.
Other Senses: Taste perversion.
Musculoskeletal System: myalgia.
Nervous System: Insomnia, paresthesia, somnolence, tremor, vertigo.
Skin and Appendages: Acute generalized exanthematous-pustulosis, drug eruption, increased sweating, exfoliative skin disorders including Stevens-Johnson syndrome and toxic epidermal necrolysis (see WARNINGS), alopecia.
Adverse Reactions in Children
The pattern and incidence of adverse events and laboratory abnormalities recorded during pediatric clinical trials are comparable to those seen in adults.
In Phase II/III clinical trials conducted in the United States and in Europe, 577 pediatric patients, ages 1 day to 17 years were treated with fluconazole at doses up to 15 mg/kg/day for up to 1,616 days. Thirteen percent of children experienced treatment related adverse events. The most commonly reported events were vomiting (5%), abdominal pain (3%), nausea (2%), and diarrhea (2%). Treatment was discontinued in 2.3% of patients due to adverse clinical events and in 1.4% of patients due to laboratory test abnormalities. The majority of treatment-related laboratory abnormalities were elevations of transaminases or alkaline phosphatase.
[undefined]
-
PATIENT PACKAGE INSERT
PATIENT INFORMATION
FLUCONAZOLE TABLET USP, 150 mg
This leaflet contains important information about fluconazole tablet. It is not meant to take the place of your doctor's instructions. Read this information carefully before you take fluconazole tablet. Ask your doctor or pharmacist if you do not understand any of this information or if you want to know more about fluconazole tablet.
What Is Fluconazole Tablet?
Fluconazole is a tablet you swallow to treat vaginal yeast infections caused by a yeast called Candida. Fluconazole tablet helps stop too much yeast from growing in the vagina so the yeast infection goes away.
Fluconazole tablet is different from other treatments for vaginal yeast infections because it is a tablet taken by mouth. Fluconazole tablet is also used for other conditions. However, this leaflet is only about using fluconazole tablet for vaginal yeast infections. For information about using fluconazole tablet for other reasons, ask your doctor or pharmacist. See the section of this leaflet for information about vaginal yeast infections.
What Is a Vaginal Yeast Infection?
It is normal for a certain amount of yeast to be found in the vagina. Sometimes too much yeast starts to grow in the vagina and this can cause a yeast infection. Vaginal yeast infections are common. About three out of every four adult women will have at least one vaginal yeast infection during their life.
Some medicines and medical conditions can increase your chance of getting a yeast infection. If you are pregnant, have diabetes, use birth control pills, or take antibiotics you may get yeast infections more often than other women. Personal hygiene and certain types of clothing may increase your chances of getting a yeast infection. Ask your doctor for tips on what you can do to help prevent vaginal yeast infections.
If you get a vaginal yeast infection, you may have any of the following symptoms:
itching
a burning feeling when you urinate
redness
soreness
a thick white vaginal discharge that looks like cottage cheeseWhat To Tell Your Doctor Before You Start Fluconazole Tablet?
Do not take fluconazole tablet if you take certain medicines. They can cause serious problems. Therefore, tell your doctor about all the medicines you take including:
diabetes medicines such as glyburide, tolbutamide, glipizide
blood pressure medicines like hydrochlorothiazide, losartan, amlodipine, nifedipine or felodipine
blood thinners such as warfarin
cyclosporine, tacrolimus or sirolimus (used to prevent rejection of organ transplants)
rifampin or rifabutin for tuberculosis
astemizole for allergies
phenytoin or carbamazepine to control seizures
theophylline to control asthma
cisapride for heartburn
quinidine (used to correct disturbances in heart rhythm)
amitriptyline or nortriptyline for depression
pimozide for psychiatric illness
amphotericin B or voriconazole for fungal infections
erythromycin for bacterial infections
cyclophosphamide or vinca alkaloids such as vincristine or vinblastine for treatment of cancer
fentanyl, afentanil or methadone for chronic pain
halofantrine for malaria
lipid lowering drugs such as atorvastatin, simvastatin, and fluvastatin
non-steroidal anti-inflammatory drugs including celecoxib, ibuprofen, and naproxen
prednisone, a steroid used to treat skin, gastrointestinal, hematological or respiratory disorders
antiviral medications used to treat HIV like saquinavir or zidovudine
tofacitinib for rheumatoid arthritis
vitamin A nutritional supplement
Since there are many brand names for these medicines, check with your doctor or pharmacist if you have any questions.
are taking any over-the-counter medicines you can buy without a prescription, including natural or herbal remedies
have any liver problems.
have any other medical conditions
are pregnant, plan to become pregnant, or think you might be pregnant. Your doctor will discuss whether fluconazole tablet is right for you.
are breast-feeding. Fluconazole tablet can pass through breast milk to the baby.
are allergic to any other medicines including those used to treat yeast and other fungal infections.
are allergic to any of the ingredients in fluconazole tablet. The main ingredient of fluconazole tablet is fluconazole. If you need to know the inactive ingredients, ask your doctor or pharmacist.Who Should Not Take Fluconazole Tablet?
To avoid a possible serious reaction, do NOT take fluconazole tablet if you are taking erythromycin, astemizole, pimozide, quinidine, and cisapride (Propulsid®) since it can cause changes in heartbeat in some people if taken with fluconazole tablet.
How Should I Take Fluconazole Tablet
Take fluconazole tablet by mouth with or without food. You can take fluconazole tablet at any time of the day.
Fluconazole tablet keeps working for several days to treat the infection. Generally the symptoms start to go away after 24 hours. However, it may take several days for your symptoms to go away completely. If there is no change in your symptoms after a few days, call your doctor.
[undefined]
Just swallow 1 fluconazole tablet to treat your vaginal yeast infection.
What Should I Avoid while Taking Fluconazole Tablet?
Some medicines can affect how well fluconazole tablet works. Check with your doctor before starting any new medicines within seven days of taking fluconazole tablet.
What Are the Possible Side Effects of Fluconazole Tablet?
Like all medicines, fluconazole tablet may cause some side effects that are usually mild to moderate.
The most common side effects of fluconazole tablet are:
headache
diarrhea
nausea or upset stomach
dizziness
stomach pain
changes in the way food tastesAllergic reactions to fluconazole tablet are rare, but they can be very serious if not treated right away by a doctor. If you cannot reach your doctor, go to the nearest hospital emergency room. Signs of an allergic reaction can include shortness of breath; coughing; wheezing; fever; chills; throbbing of the heart or ears; swelling of the eyelids, face, mouth, neck, or any other part of the body; or skin rash, hives, blisters or skin peeling.
Fluconazole tablet has been linked to rare cases of serious liver damage, including deaths, mostly in patients with serious medical problems. Call your doctor if your skin or eyes become yellow, your urine turns a darker color, your stools (bowel movements) are light-colored, or if you vomit or feel like vomiting or if you have severe skin itching.
In patients with serious conditions such as AIDS or cancer, rare cases of severe rashes with skin peeling have been reported. Tell your doctor right away if you get a rash while taking fluconazole tablet.
Fluconazole tablet may cause other less common side effects besides those listed here. If you develop any side effects that concern you, call your doctor. For a list of all side effects, ask your doctor or pharmacist.
What to Do For an Overdose
In case of an accidental overdose, call your doctor right away or go to the nearest emergency room.
How to Store Fluconazole Tablet
Keep fluconazole tablet and all medicines out of the reach of children.
General Advice about Prescription Medicines
Medicines are sometimes prescribed for conditions that are mentioned in patient information leaflets. Do not use fluconazole tablet for a condition for which it was not prescribed. Do not give fluconazole tablet to other people, even if they have the same symptoms you have. It may harm them.
This leaflet summarizes the most important information about fluconazole tablet. If you would like more information, talk with your doctor. You can ask your pharmacist or doctor for information about fluconazole tablet that is written for health professionals.
To reorder additional Patient Information Sheets, contact Dr. Reddy’s Customer Service at
1-866-733-3952.
Rx Only
Manufactured by:
Dr. Reddy’s Laboratories Limited
Bachupally – 500 090 INDIA
Revised: 0114
-
DOSAGE & ADMINISTRATION
Dosage and Administration in AdultsSingle Dose
Vaginal candidiasis: The recommended dosage of fluconazole for vaginal candidiasis is 150 mg as a single oral dose.
Multiple Dose
SINCE ORAL ABSORPTION IS RAPID AND ALMOST COMPLETE, THE DAILY DOSE OF FLUCONAZOLE IS THE SAME FOR ORAL AND INTRAVENOUS ADMINISTRATION. In general, a loading dose of twice the daily dose is recommended on the first day of therapy to result in plasma concentrations close to steady-state by the second day of therapy.
The daily dose of fluconazole for the treatment of infections other than vaginal candidiasis should be based on the infecting organism and the patient’s response to therapy. Treatment should be continued until clinical parameters or laboratory tests indicate that active fungal infection has subsided. An inadequate period of treatment may lead to recurrence of active infection. Patients with AIDS and cryptococcal meningitis or recurrent oropharyngeal candidiasis usually require maintenance therapy to prevent relapse.
Oropharyngeal candidiasis: The recommended dosage of fluconazole for oropharyngeal candidiasis is 200 mg on the first day, followed by 100 mg once daily. Clinical evidence of oropharyngeal candidiasis generally resolves within several days, but treatment should be continued for at least 2 weeks to decrease the likelihood of relapse.
Esophageal candidiasis: The recommended dosage of fluconazole for esophageal candidiasis is 200 mg on the first day, followed by 100 mg once daily. Doses up to 400 mg/day may be used, based on medical judgment of the patient’s response to therapy. Patients with esophageal candidiasis should be treated for a minimum of three weeks and for at least two weeks following resolution of symptoms.
Systemic Candida infections: For systemic Candida infections including candidemia, disseminated candidiasis, and pneumonia, optimal therapeutic dosage and duration of therapy have not been established. In open, noncomparative studies of small numbers of patients, doses of up to 400 mg daily have been used.
Urinary tract infections and peritonitis: For the treatment of Candida urinary tract infections and peritonitis, daily doses of 50 to 200 mg have been used in open, noncomparative studies of small numbers of patients.
Cryptococcal meningitis: The recommended dosage for treatment of acute cryptococcal meningitis is 400 mg on the first day, followed by 200 mg once daily. A dosage of 400 mg once daily may be used, based on medical judgment of the patient’s response to therapy. The recommended duration of treatment for initial therapy of cryptococcal meningitis is 10 to 12 weeks after the cerebrospinal fluid becomes culture negative. The recommended dosage of fluconazole for suppression of relapse of cryptococcal meningitis in patients with AIDS is 200 mg once daily.
Prophylaxis in patients undergoing bone marrow transplantation: The recommended fluconazole daily dosage for the prevention of candidiasis in patients undergoing bone marrow transplantation is 400 mg, once daily. Patients who are anticipated to have severe granulocytopenia (less than 500 neutrophils per cu mm) should start fluconazole prophylaxis several days before the anticipated onset of neutropenia, and continue for 7 days after the neutrophil count rises above 1000 cells per cu mm.
Dosage and Administration in Children
The following dose equivalency scheme should generally provide equivalent exposure in pediatric and adult patients:
[undefined]
Experience with fluconazole in neonates is limited to pharmacokinetic studies in premature newborns. (See CLINICAL PHARMACOLOGY.) Based on the prolonged half-life seen in premature newborns (gestational age 26 to 29 weeks), these children, in the first two weeks of life, should receive the same dosage (mg/kg) as in older children, but administered every 72 hours. After the first two weeks, these children should be dosed once daily. No information regarding fluconazole pharmacokinetics in full-term newborns is available.Dosage in Patients With Impaired Renal Function
Fluconazole is cleared primarily by renal excretion as unchanged drug. There is no need to adjust single dose therapy for vaginal candidiasis because of impaired renal function. In patients with impaired renal function who will receive multiple doses of fluconazole, an initial loading dose of 50 to 400 mg should be given. After the loading dose, the daily dose (according to indication) should be based on the following table:
[undefined]
These are suggested dose adjustments based on pharmacokinetics following administration of multiple doses. Further adjustment may be needed depending upon clinical condition.When serum creatinine is the only measure of renal function available, the following formula (based on sex, weight, and age of the patient) should be used to estimate the creatinine clearance in adults:
Males: Weight (kg) × (140-age)
72 × serum creatinine (mg/100 mL)Females: 0.85 × above value
Although the pharmacokinetics of fluconazole has not been studied in children with renal insufficiency, dosage reduction in children with renal insufficiency should parallel that recommended for adults. The following formula may be used to estimate creatinine clearance in children:
K × linear length or height (cm)
serum creatinine (mg/100 mL)
(Where K=0.55 for children older than 1 year and 0.45 for infants.)Administration
Fluconazole tablets are administered orally. Fluconazole tablets can be taken with or without food.
-
DESCRIPTION
Fluconazole, the first of a new subclass of synthetic triazole antifungal agents, is available as tablets for oral administration.
Fluconazole is designated chemically as 2,4-difluoro-α,α1-bis(1H-1,2,4-triazol-1-ylmethyl) benzyl alcohol with a molecular formula of C13H12F2N6O and molecular weight 306.3. The structural formula is:
Fluconazole USP is a white crystalline solid which is slightly soluble in water and saline.
Fluconazole tablets USP contain 50, 100, 150, or 200 mg of fluconazole USP and the following inactive ingredients: dibasic calcium phosphate anhydrous, ferric oxide (iron oxide, red), magnesium stearate, microcrystalline cellulose, povidone, sodium starch glycolate, and starch.
Fluconazole tablets meets USP Dissolution Test 2.
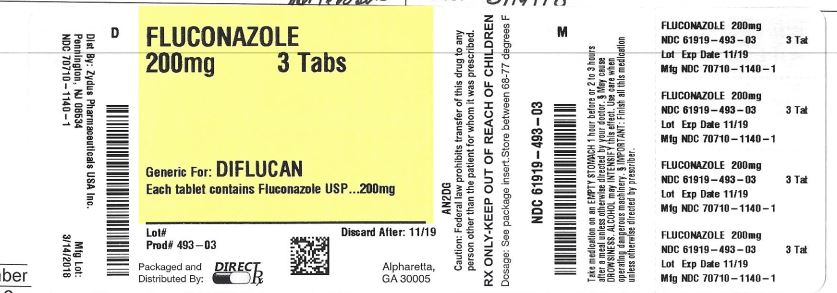
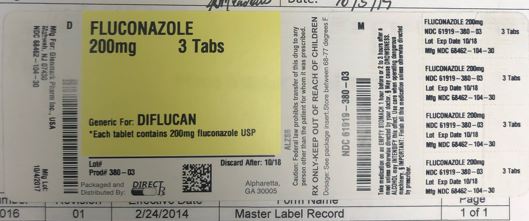
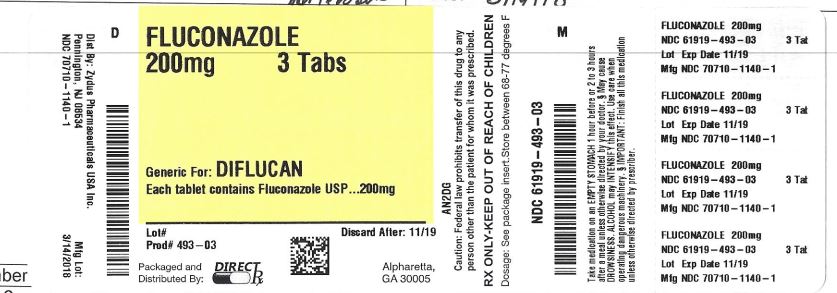
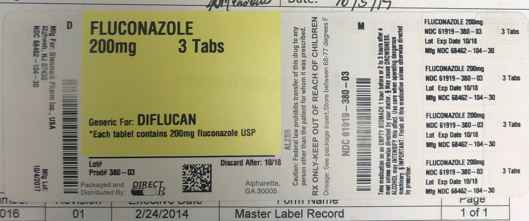
Close - PRINCIPAL DISPLAY PANEL
- PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
FLUCONAZOLE
fluconazole tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:61919-380(NDC:68462-104) Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength FLUCONAZOLE (UNII: 8VZV102JFY) (FLUCONAZOLE - UNII:8VZV102JFY) FLUCONAZOLE 200 mg Inactive Ingredients Ingredient Name Strength FERRIC OXIDE RED (UNII: 1K09F3G675) ANHYDROUS DIBASIC CALCIUM PHOSPHATE (UNII: L11K75P92J) MAGNESIUM STEARATE (UNII: 70097M6I30) CELLULOSE, MICROCRYSTALLINE (UNII: OP1R32D61U) POVIDONE (UNII: FZ989GH94E) SODIUM STARCH GLYCOLATE TYPE A POTATO (UNII: 5856J3G2A2) STARCH, CORN (UNII: O8232NY3SJ) Product Characteristics Color pink Score no score Shape TRAPEZOID Size 12mm Flavor Imprint Code 200 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:61919-380-03 3 in 1 BOTTLE; Type 0: Not a Combination Product 11/01/2017 12/31/2023 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA076658 11/01/2017 12/31/2023 FLUCONAZOLE
fluconazole tabletProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:61919-493(NDC:70710-1140) Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength FLUCONAZOLE (UNII: 8VZV102JFY) (FLUCONAZOLE - UNII:8VZV102JFY) FLUCONAZOLE 200 mg Inactive Ingredients Ingredient Name Strength POVIDONE K30 (UNII: U725QWY32X) ANHYDROUS DIBASIC CALCIUM PHOSPHATE (UNII: L11K75P92J) CELLULOSE, MICROCRYSTALLINE (UNII: OP1R32D61U) MAGNESIUM STEARATE (UNII: 70097M6I30) CROSCARMELLOSE SODIUM (UNII: M28OL1HH48) FD&C RED NO. 40 (UNII: WZB9127XOA) Product Characteristics Color pink (light pink to pink) Score no score Shape OVAL (modified oval) Size 12mm Flavor Imprint Code 1140 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:61919-493-03 3 in 1 BOTTLE; Type 0: Not a Combination Product 04/08/2019 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA208963 04/08/2019 Labeler - Direct Rx (079254320) Establishment Name Address ID/FEI Business Operations Direct Rx 079254320 repack(61919-380, 61919-493)