VYTORIN- ezetimibe simvastin tablet
Lake Erie Medical DBA Quality Care Products LLC
----------
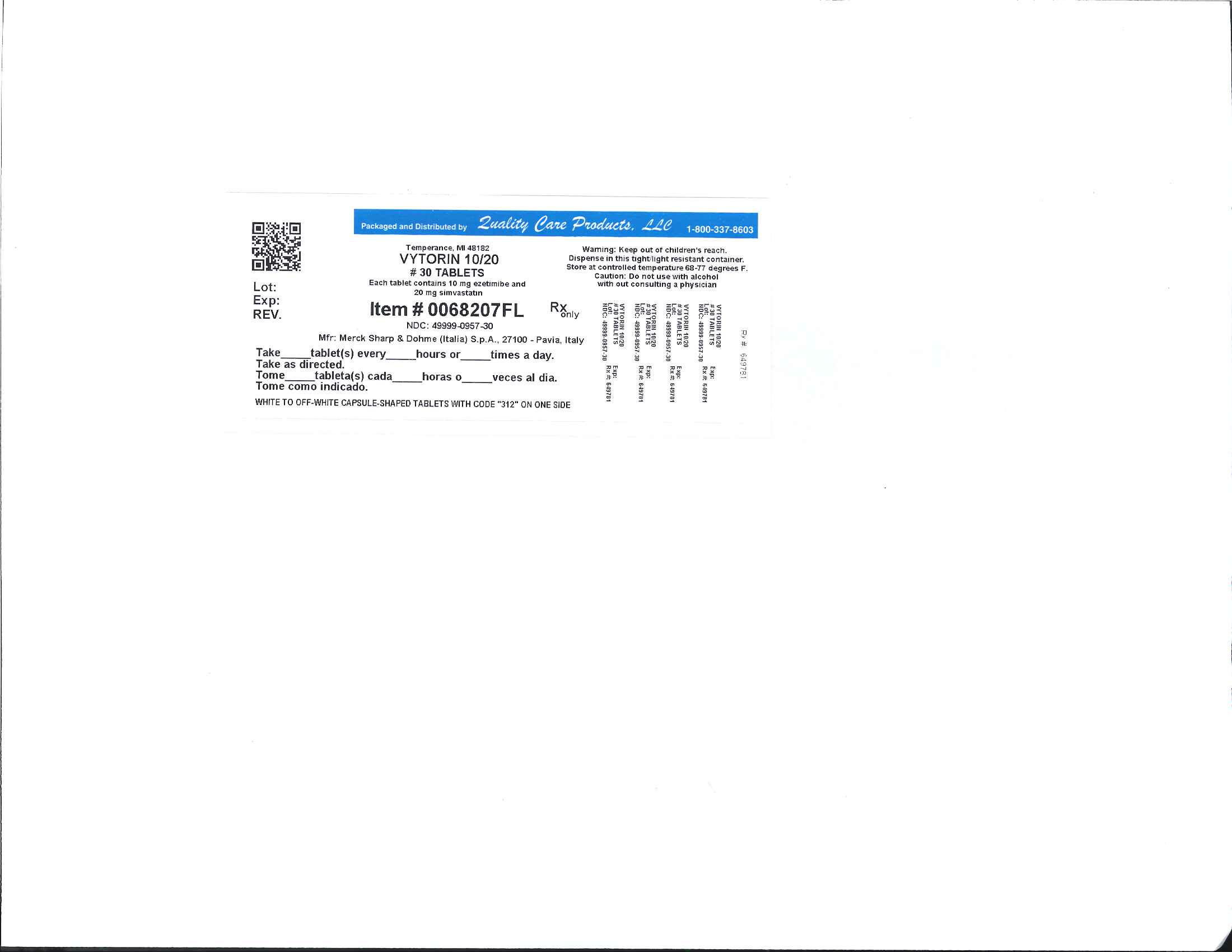
Vytorin 10/20 mg
11 DESCRIPTION
VYTORIN contains ezetimibe, a selective inhibitor of intestinal cholesterol and related phytosterol absorption, and simvastatin, an HMG-CoA reductase inhibitor.
The chemical name of ezetimibe is 1-(4-fluorophenyl)-3(R)-[3-(4-fluorophenyl)-3(S)-hydroxypropyl]-4(S)-(4-hydroxyphenyl)-2-azetidinone. The empirical formula is C24H21F2NO3 and its molecular weight is 409.4.
Ezetimibe is a white, crystalline powder that is freely to very soluble in ethanol, methanol, and acetone and practically insoluble in water. Its structural formula is:
Simvastatin, an inactive lactone, is hydrolyzed to the corresponding β-hydroxyacid form, which is an inhibitor of HMGCoA reductase. Simvastatin is butanoic acid, 2,2-dimethyl-,1,2,3,7,8,8a-hexahydro-3,7-dimethyl-8-[2-(tetrahydro-4-hydroxy-6-oxo-2H-pyran-2-yl)-ethyl]-1-naphthalenyl ester, [1S-[1α,3α,7β,8β(2S*,4S*),-8aβ]]. The empirical formula of simvastatin is C25H38O5 and its molecular weight is 418.57.
Simvastatin is a white to off-white, nonhygroscopic, crystalline powder that is practically insoluble in water and freely soluble in chloroform, methanol and ethanol. Its structural formula is:
YTORIN is available for oral use as tablets containing 10 mg of ezetimibe, and 10 mg of simvastatin (VYTORIN 10/10), 20 mg of simvastatin (VYTORIN 10/20), 40 mg of simvastatin (VYTORIN 10/40), or 80 mg of simvastatin (VYTORIN 10/80). Each tablet contains the following inactive ingredients: butylated hydroxyanisole NF, citric acid monohydrate USP, croscarmellose sodium NF, hypromellose USP, lactose monohydrate NF, magnesium stearate NF, microcrystalline cellulose NF, and propyl gallate NF.
7 DRUG INTERACTIONS
[See Clinical Pharmacology (12.3).]
VYTORIN
7.1 CYP3A4 Interactions
The risk of myopathy is increased by reducing the elimination of the simvastatin component of VYTORIN. Hence when VYTORIN is used with an inhibitor of CYP3A4 (e.g., as listed below), elevated plasma levels of HMG-CoA reductase inhibitory activity can increase the risk of myopathy and rhabdomyolysis, particularly with higher doses of VYTORIN. [See Warnings and Precautions (5.1) and Clinical Pharmacology (12.3).]
Itraconazole, ketoconazole, and other antifungal azoles
Macrolide antibiotics erythromycin, clarithromycin, and the ketolide antibiotic telithromycin
HIV protease inhibitors
Antidepressant nefazodone
Grapefruit juice in large quantities (>1 quart daily)
Concomitant use of these drugs and any medication labeled as having a strong inhibitory effect on CYP3A4 should be avoided unless the benefits of combined therapy outweigh the increased risk. If treatment with itraconazole, ketoconazole, erythromycin, clarithromycin or telithromycin is unavoidable, therapy with VYTORIN should be suspended during the course of treatment.
7.2 Lipid-Lowering Drugs That Can Cause Myopathy When Given Alone
The risk of myopathy is increased by gemfibrozil and to a lesser extent by other fibrates [see Warnings and Precautions (5.1)].
7.3 Amiodarone, Verapamil, or Diltiazem
The risk of myopathy/rhabdomyolysis is increased by concomitant administration of amiodarone, verapamil, or diltiazem with higher doses of VYTORIN [see Warnings and Precautions (5.1)].
7.4 Niacin
Cases of myopathy/rhabdomyolysis have been observed with simvastatin coadministered with lipid-modifying doses (≥1 g/day niacin) of niacin-containing products. In particular, caution should be used when treating Chinese patients with VYTORIN coadministered with lipid-modifying doses of niacin-containing products. Because the risk for myopathy is dose-related, Chinese patients should not receive VYTORIN 10/80 mg coadministered with lipid-modifying doses of niacin-containing products. [See Warnings and Precautions (5.1).]
7.5 Cholestyramine
Concomitant cholestyramine administration decreased the mean AUC of total ezetimibe approximately 55%. The incremental LDL-C reduction due to adding VYTORIN to cholestyramine may be reduced by this interaction.
7.6 Cyclosporine or Danazol
The risk of myopathy/rhabdomyolysis is increased by concomitant administration of cyclosporine or danazol particularly with higher doses of VYTORIN [see Warnings and Precautions (5.1) and Clinical Pharmacology (12.3)].
Caution should be exercised when using VYTORIN and cyclosporine concomitantly due to increased exposure to both ezetimibe and cyclosporine [see Dosage and Administration (2.7)]. Cyclosporine concentrations should be monitored in patients receiving VYTORIN and cyclosporine [see Clinical Pharmacology (12.3)].
The degree of increase in ezetimibe exposure may be greater in patients with severe renal impairment. In patients treated with cyclosporine, the potential effects of the increased exposure to ezetimibe from concomitant use should be carefully weighed against the benefits of alterations in lipid levels provided by ezetimibe. [See Warnings and Precautions (5.1) and Clinical Pharmacology (12.3).]
7.7 Digoxin
In one study, concomitant administration of digoxin with simvastatin resulted in a slight elevation in plasma digoxin concentrations. Patients taking digoxin should be monitored appropriately when VYTORIN is initiated.
7.8 Fibrates
The safety and effectiveness of VYTORIN administered with fibrates have not been established.
Fibrates may increase cholesterol excretion into the bile, leading to cholelithiasis. In a preclinical study in dogs, ezetimibe increased cholesterol in the gallbladder bile [see Animal Toxicology and/or Pharmacology (13.2)]. Coadministration of VYTORIN with fibrates is not recommended until use in patients is studied. [See Warnings and Precautions (5.1).]
7.9 Coumarin Anticoagulants
Simvastatin 20-40 mg/day modestly potentiated the effect of coumarin anticoagulants: the prothrombin time, reported as International Normalized Ratio (INR), increased from a baseline of 1.7 to 1.8 and from 2.6 to 3.4 in a normal volunteer study and in a hypercholesterolemic patient study, respectively. With other statins, clinically evident bleeding and/or increased prothrombin time has been reported in a few patients taking coumarin anticoagulants concomitantly. In such patients, prothrombin time should be determined before starting VYTORIN and frequently enough during early therapy to ensure that no significant alteration of prothrombin time occurs. Once a stable prothrombin time has been documented, prothrombin times can be monitored at the intervals usually recommended for patients on coumarin anticoagulants. If the dose of VYTORIN is changed or discontinued, the same procedure should be repeated. Simvastatin therapy has not been associated with bleeding or with changes in prothrombin time in patients not taking anticoagulants.
Concomitant administration of ezetimibe (10 mg once daily) had no significant effect on bioavailability of warfarin and prothrombin time in a study of twelve healthy adult males. There have been post-marketing reports of increased INR in patients who had ezetimibe added to warfarin. Most of these patients were also on other medications.
The effect of VYTORIN on the prothrombin time has not been studied.
13 NONCLINICAL TOXICOLOGY13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
VYTORIN
No animal carcinogenicity or fertility studies have been conducted with the combination of ezetimibe and simvastatin. The combination of ezetimibe with simvastatin did not show evidence of mutagenicity in vitro in a microbial mutagenicity (Ames) test with Salmonella typhimurium and Escherichia coli with or without metabolic activation. No evidence of clastogenicity was observed in vitro in a chromosomal aberration assay in human peripheral blood lymphocytes with ezetimibe and simvastatin with or without metabolic activation. There was no evidence of genotoxicity at doses up to 600 mg/kg with the combination of ezetimibe and simvastatin (1:1) in the in vivo mouse micronucleus test.
Ezetimibe
A 104-week dietary carcinogenicity study with ezetimibe was conducted in rats at doses up to 1500 mg/kg/day (males) and 500 mg/kg/day (females) (~20 times the human exposure at 10 mg daily based on AUC0-24hr for total ezetimibe). A 104-week dietary carcinogenicity study with ezetimibe was also conducted in mice at doses up to 500 mg/kg/day (>150 times the human exposure at 10 mg daily based on AUC0-24hr for total ezetimibe). There were no statistically significant increases in tumor incidences in drug-treated rats or mice.
No evidence of mutagenicity was observed in vitro in a microbial mutagenicity (Ames) test with Salmonella typhimurium and Escherichia coli with or without metabolic activation. No evidence of clastogenicity was observed in vitro in a chromosomal aberration assay in human peripheral blood lymphocytes with or without metabolic activation. In addition, there was no evidence of genotoxicity in the in vivo mouse micronucleus test.
In oral (gavage) fertility studies of ezetimibe conducted in rats, there was no evidence of reproductive toxicity at doses up to 1000 mg/kg/day in male or female rats (~7 times the human exposure at 10 mg daily based on AUC0-24hr for total ezetimibe).
Simvastatin
In a 72-week carcinogenicity study, mice were administered daily doses of simvastatin of 25, 100, and 400 mg/kg body weight, which resulted in mean plasma drug levels approximately 1, 4, and 8 times higher than the mean human plasma drug level, respectively, (as total inhibitory activity based on AUC) after an 80-mg oral dose. Liver carcinomas were significantly increased in high-dose females and mid- and high-dose males with a maximum incidence of 90% in males. The incidence of adenomas of the liver was significantly increased in mid- and high-dose females. Drug treatment also significantly increased the incidence of lung adenomas in mid- and high-dose males and females. Adenomas of the Harderian gland (a gland of the eye of rodents) were significantly higher in high-dose mice than in controls. No evidence of a tumorigenic effect was observed at 25 mg/kg/day.
In a separate 92-week carcinogenicity study in mice at doses up to 25 mg/kg/day, no evidence of a tumorigenic effect was observed (mean plasma drug levels were 1 times higher than humans given 80 mg simvastatin as measured by AUC).
In a two-year study in rats at 25 mg/kg/day, there was a statistically significant increase in the incidence of thyroid follicular adenomas in female rats exposed to approximately 11 times higher levels of simvastatin than in humans given 80 mg simvastatin (as measured by AUC).
A second two-year rat carcinogenicity study with doses of 50 and 100 mg/kg/day produced hepatocellular adenomas and carcinomas (in female rats at both doses and in males at 100 mg/kg/day). Thyroid follicular cell adenomas were increased in males and females at both doses; thyroid follicular cell carcinomas were increased in females at 100 mg/kg/day. The increased incidence of thyroid neoplasms appears to be consistent with findings from other statins. These treatment levels represented plasma drug levels (AUC) of approximately 7 and 15 times (males) and 22 and 25 times (females) the mean human plasma drug exposure after an 80-mg daily dose.
No evidence of mutagenicity was observed in a microbial mutagenicity (Ames) test with or without rat or mouse liver metabolic activation. In addition, no evidence of damage to genetic material was noted in an in vitro alkaline elution assay using rat hepatocytes, a V-79 mammalian cell forward mutation study, an in vitro chromosome aberration study in CHO cells, or an in vivo chromosomal aberration assay in mouse bone marrow.
There was decreased fertility in male rats treated with simvastatin for 34 weeks at 25 mg/kg body weight (4 times the maximum human exposure level, based on AUC, in patients receiving 80 mg/day); however, this effect was not observed during a subsequent fertility study in which simvastatin was administered at this same dose level to male rats for 11 weeks (the entire cycle of spermatogenesis including epididymal maturation). No microscopic changes were observed in the testes of rats from either study. At 180 mg/kg/day, (which produces exposure levels 22 times higher than those in humans taking 80 mg/day based on surface area, mg/m2), seminiferous tubule degeneration (necrosis and loss of spermatogenic epithelium) was observed. In dogs, there was drug-related testicular atrophy, decreased spermatogenesis, spermatocytic degeneration and giant cell formation at 10 mg/kg/day (approximately 2 times the human exposure, based on AUC, at 80 mg/day). The clinical significance of these findings is unclear.
13.2 Animal Toxicology and/or Pharmacology
CNS Toxicity
Optic nerve degeneration was seen in clinically normal dogs treated with simvastatin for 14 weeks at 180 mg/kg/day, a dose that produced mean plasma drug levels about 12 times higher than the mean plasma drug level in humans taking 80 mg/day.
A chemically similar drug in this class also produced optic nerve degeneration (Wallerian degeneration of retinogeniculate fibers) in clinically normal dogs in a dose-dependent fashion starting at 60 mg/kg/day, a dose that produced mean plasma drug levels about 30 times higher than the mean plasma drug level in humans taking the highest recommended dose (as measured by total enzyme inhibitory activity). This same drug also produced vestibulocochlear Wallerian-like degeneration and retinal ganglion cell chromatolysis in dogs treated for 14 weeks at 180 mg/kg/day, a dose that resulted in a mean plasma drug level similar to that seen with the 60 mg/kg/day dose.
CNS vascular lesions, characterized by perivascular hemorrhage and edema, mononuclear cell infiltration of perivascular spaces, perivascular fibrin deposits and necrosis of small vessels were seen in dogs treated with simvastatin at a dose of 360 mg/kg/day, a dose that produced mean plasma drug levels that were about 14 times higher than the mean plasma drug levels in humans taking 80 mg/day. Similar CNS vascular lesions have been observed with several other drugs of this class.
There were cataracts in female rats after two years of treatment with 50 and 100 mg/kg/day (22 and 25 times the human AUC at 80 mg/day, respectively) and in dogs after three months at 90 mg/kg/day (19 times) and at two years at 50 mg/kg/day (5 times).
Ezetimibe
The hypocholesterolemic effect of ezetimibe was evaluated in cholesterol-fed Rhesus monkeys, dogs, rats, and mouse models of human cholesterol metabolism. Ezetimibe was found to have an ED50 value of 0.5 μg/kg/day for inhibiting the rise in plasma cholesterol levels in monkeys. The ED50 values in dogs, rats, and mice were 7, 30, and 700 μg/kg/day, respectively. These results are consistent with ezetimibe being a potent cholesterol absorption inhibitor.
In a rat model, where the glucuronide metabolite of ezetimibe (ezetimibe-glucuronide) was administered intraduodenally, the metabolite was as potent as ezetimibe in inhibiting the absorption of cholesterol, suggesting that the glucuronide metabolite had activity similar to the parent drug.
In 1-month studies in dogs given ezetimibe (0.03 to 300 mg/kg/day), the concentration of cholesterol in gallbladder bile increased ~2- to 4-fold. However, a dose of 300 mg/kg/day administered to dogs for one year did not result in gallstone formation or any other adverse hepatobiliary effects. In a 14-day study in mice given ezetimibe (0.3 to 5 mg/kg/day) and fed a low-fat or cholesterol-rich diet, the concentration of cholesterol in gallbladder bile was either unaffected or reduced to normal levels, respectively.
A series of acute preclinical studies was performed to determine the selectivity of ezetimibe for inhibiting cholesterol absorption. Ezetimibe inhibited the absorption of 14C-cholesterol with no effect on the absorption of triglycerides, fatty acids, bile acids, progesterone, ethinyl estradiol, or the fat-soluble vitamins A and D.
In 4- to 12-week toxicity studies in mice, ezetimibe did not induce cytochrome P450 drug-metabolizing enzymes. In toxicity studies, a pharmacokinetic interaction of ezetimibe with statins (parents or their active hydroxy acid metabolites) was seen in rats, dogs, and rabbits.
1 INDICATIONS AND USAGE
Therapy with lipid-altering agents should be only one component of multiple risk factor intervention in individuals at significantly increased risk for atherosclerotic vascular disease due to hypercholesterolemia. Drug therapy is indicated as an adjunct to diet when the response to a diet restricted in saturated fat and cholesterol and other nonpharmacologic measures alone has been inadequate.
1.1 Primary Hyperlipidemia
VYTORIN is indicated for the reduction of elevated total cholesterol (total-C), low-density lipoprotein cholesterol (LDL-C), apolipoprotein B (Apo B), triglycerides (TG), and non-high-density lipoprotein cholesterol (non-HDL-C), and to increase high-density lipoprotein cholesterol (HDL-C) in patients with primary (heterozygous familial and non-familial) hyperlipidemia or mixed hyperlipidemia.
1.2 Homozygous Familial Hypercholesterolemia (HoFH)
VYTORIN is indicated for the reduction of elevated total-C and LDL-C in patients with homozygous familial hypercholesterolemia, as an adjunct to other lipid-lowering treatments (e.g., LDL apheresis) or if such treatments are unavailable.
1.3 Limitations of Use
No incremental benefit of VYTORIN on cardiovascular morbidity and mortality over and above that demonstrated for simvastatin has been established. VYTORIN has not been studied in Fredrickson type I, III, IV, and V dyslipidemias.
4 CONTRAINDICATIONS
Hypersensitivity to any component of this medication [see Adverse Reactions (6.2)].
Active liver disease or unexplained persistent elevations in hepatic transaminase levels [see Warnings and Precautions (5.2)].
Women who are pregnant or may become pregnant. Serum cholesterol and triglycerides increase during normal pregnancy, and cholesterol or cholesterol derivatives are essential for fetal development. Because HMG-CoA reductase inhibitors (statins), such as simvastatin, decrease cholesterol synthesis and possibly the synthesis of other biologically active substances derived from cholesterol, VYTORIN may cause fetal harm when administered to a pregnant woman. Atherosclerosis is a chronic process and the discontinuation of lipid-lowering drugs during pregnancy should have little impact on the outcome of long-term therapy of primary hypercholesterolemia. There are no adequate and well-controlled studies of VYTORIN use during pregnancy; however, in rare reports congenital anomalies were observed following intrauterine exposure to statins. In rat and rabbit animal reproduction studies, simvastatin revealed no evidence of teratogenicity. VYTORIN should be administered to women of childbearing age only when such patients are highly unlikely to conceive. If the patient becomes pregnant while taking this drug, VYTORIN should be discontinued immediately and the patient should be apprised of the potential hazard to the fetus [see Use in Specific Populations (8.1)].
Nursing mothers. It is not known whether simvastatin is excreted into human milk; however, a small amount of another drug in this class does pass into breast milk. Because statins have the potential for serious adverse reactions in nursing infants, women who require VYTORIN treatment should not breast-feed their infants [see Use in Specific Populations (8.3)].
6 ADVERSE REACTIONS
The following serious adverse reactions are discussed in greater detail in other sections of the label:
- Rhabdomyolysis and myopathy [see Warnings and Precautions (5.1)]
- Liver enzyme abnormalities [see Warnings and Precautions (5.2)]
6.1 Clinical Trials Experience
VYTORIN
Because clinical studies are conducted under widely varying conditions, adverse reaction rates observed in the clinical studies of a drug cannot be directly compared to rates in the clinical studies of another drug and may not reflect the rates observed in practice.
In the VYTORIN (ezetimibe/simvastatin) placebo-controlled clinical trials database of 1420 patients (age range 20-83 years, 52% women, 87% Caucasians, 3% Blacks, 5% Hispanics, 3% Asians) with a median treatment duration of 27 weeks, 5% of patients on VYTORIN and 2.2% of patients on placebo discontinued due to adverse reactions.
The most common adverse reactions in the group treated with VYTORIN that led to treatment discontinuation and occurred at a rate greater than placebo were:
- Increased ALT (0.9%)
- Myalgia (0.6%)
- Increased AST (0.4%)
- Back pain (0.4%)
The most commonly reported adverse reactions (incidence ≥2% and greater than placebo) in controlled clinical trials were: headache (5.8%), increased ALT (3.7%), myalgia (3.6%), upper respiratory tract infection (3.6%), and diarrhea (2.8%).
VYTORIN has been evaluated for safety in more than 10,189 patients in clinical trials.
Table 2 summarizes the frequency of clinical adverse reactions reported in ≥2% of patients treated with VYTORIN (n=1420) and at an incidence greater than placebo, regardless of causality assessment, from four placebo-controlled trials.
Ezetimibe
Other adverse reactions reported with ezetimibe in placebo-controlled studies, regardless of causality assessment: Musculoskeletal system disorders: arthralgia; Infections and infestations: sinusitis; Body as a whole – general disorders: fatigue.
Simvastatin
Other adverse reactions reported with simvastatin in placebo-controlled clinical studies, regardless of causality assessment: Cardiac disorders: atrial fibrillation; Ear and labyrinth disorders: vertigo; Gastrointestinal disorders: abdominal pain, constipation, dyspepsia, flatulence, gastritis; Skin and subcutaneous tissue disorders: eczema, rash; Endocrine disorders: diabetes mellitus; Infections and infestations: bronchitis, sinusitis, urinary tract infections; Body as a whole – general disorders: asthenia, edema/swelling; Psychiatric disorders: insomnia.
Laboratory Tests
Marked persistent increases of hepatic serum transaminases have been noted [see Warnings and Precautions (5.2)]. Elevated alkaline phosphatase and γ-glutamyl transpeptidase have been reported. About 5% of patients taking simvastatin had elevations of CK levels of 3 or more times the normal value on one or more occasions. This was attributable to the noncardiac fraction of CK [see Warnings and Precautions (5.1)].
6.2 Post-Marketing Experience
Because the below reactions are reported voluntarily from a population of uncertain size, it is generally not possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
The following adverse reactions have been reported in post-marketing experience for VYTORIN or ezetimibe or simvastatin: pruritus; alopecia; erythema multiforme; a variety of skin changes (e.g., nodules, discoloration, dryness of skin/mucous membranes, changes to hair/nails); dizziness; muscle cramps; myalgia; arthralgia; pancreatitis; memory impairment; paresthesia; peripheral neuropathy; vomiting; nausea; anemia; erectile dysfunction; interstitial lung disease; myopathy/rhabdomyolysis [see Warnings and Precautions (5.1)]; hepatitis/jaundice; hepatic failure; depression; cholelithiasis; cholecystitis; thrombocytopenia; elevations in liver transaminases; elevated creatine phosphokinase.
Hypersensitivity reactions, including anaphylaxis, angioedema, rash, and urticaria have been reported.
In addition, an apparent hypersensitivity syndrome has been reported rarely that has included one or more of the following features: anaphylaxis, angioedema, lupus erythematous-like syndrome, polymyalgia rheumatica, dermatomyositis, vasculitis, purpura, thrombocytopenia, leukopenia, hemolytic anemia, positive ANA, ESR increase, eosinophilia, arthritis, arthralgia, urticaria, asthenia, photosensitivity, fever, chills, flushing, malaise, dyspnea, toxic epidermal necrolysis, erythema multiforme, including Stevens-Johnson syndrome.
10 OVERDOSAGE
VYTORIN
No specific treatment of overdosage with VYTORIN can be recommended. In the event of an overdose, symptomatic and supportive measures should be employed.
Ezetimibe
In clinical studies, administration of ezetimibe, 50 mg/day to 15 healthy subjects for up to 14 days, or 40 mg/day to 18 patients with primary hyperlipidemia for up to 56 days, was generally well tolerated.
A few cases of overdosage have been reported; most have not been associated with adverse experiences. Reported adverse experiences have not been serious.
Simvastatin
Significant lethality was observed in mice after a single oral dose of 9 g/m2. No evidence of lethality was observed in rats or dogs treated with doses of 30 and 100 g/m2, respectively. No specific diagnostic signs were observed in rodents. At these doses the only signs seen in dogs were emesis and mucoid stools.
A few cases of overdosage with simvastatin have been reported; the maximum dose taken was 3.6 g. All patients recovered without sequelae.
The dialyzability of simvastatin and its metabolites in man is not known at present.
2 DOSAGE AND ADMINISTRATION2.1 Recommended Dosing
The dosage range is 10/10 mg/day through 10/80 mg/day. The recommended usual starting dose is 10/20 mg/day. VYTORIN should be taken as a single daily dose in the evening, with or without food. Initiation of therapy with 10/10 mg/day may be considered for patients requiring less aggressive LDL-C reductions. Patients who require a larger reduction in LDL-C (greater than 55%) may be started at 10/40 mg/day. After initiation or titration of VYTORIN, lipid levels may be analyzed after 2 or more weeks and dosage adjusted, if needed.
2.2 Patients with Homozygous Familial Hypercholesterolemia
The recommended dosage for patients with homozygous familial hypercholesterolemia is VYTORIN 10/40 mg/day or 10/80 mg/day in the evening. VYTORIN should be used as an adjunct to other lipid-lowering treatments (e.g., LDL apheresis) in these patients or if such treatments are unavailable.
2.3 Patients with Hepatic Impairment
No dosage adjustment is necessary in patients with mild hepatic impairment [see Warnings and Precautions (5.3)].
2.4 Patients with Renal Impairment
No dosage adjustment is necessary in patients with mild or moderate renal impairment. However, for patients with severe renal insufficiency, VYTORIN should not be started unless the patient has already tolerated treatment with simvastatin at a dose of 5 mg or higher. Caution should be exercised when VYTORIN is administered to these patients, and they should be closely monitored [see Warnings and Precautions (5.1); Clinical Pharmacology (12.3)].
2.5 Geriatric Patients
No dosage adjustment is necessary in geriatric patients [see Clinical Pharmacology (12.3)].
2.6 Chinese Patients Taking Lipid-Modifying Doses (≥1 g/day Niacin) of Niacin-Containing Products
Because of an increased risk for myopathy, caution should be used when treating Chinese patients with VYTORIN coadministered with lipid-modifying doses (≥1 g/day niacin) of niacin-containing products. Because the risk for myopathy is dose-related, Chinese patients should not receive VYTORIN 10/80 mg coadministered with lipid-modifying doses of niacin-containing products. The cause of the increased risk of myopathy is not known. It is also unknown if the risk for myopathy with coadministration of simvastatin with lipid-modifying doses of niacin-containing products observed in Chinese patients applies to other Asian patients. [See Warnings and Precautions (5.1).]
2.7 Coadministration with Other Drugs
[See Warnings and Precautions (5.1) and Drug Interactions (7).]
Bile Acid Sequestrants
Dosing of VYTORIN should occur either ≥2 hours before or ≥4 hours after administration of a bile acid sequestrant [see Drug Interactions (7.5)].
Cyclosporine or Danazol
Caution should be exercised when initiating VYTORIN in the setting of cyclosporine. In patients taking cyclosporine or danazol, VYTORIN should not be started unless the patient has already tolerated treatment with simvastatin at a dose of 5 mg or higher. The dose of VYTORIN should not exceed 10/10 mg/day [see Drug Interactions (7.6)].
Amiodarone or Verapamil
In patients taking amiodarone or verapamil concomitantly with VYTORIN, the dose should not exceed 10/20 mg/day [see Warnings and Precautions (5.1) and Drug Interactions (7.3)].
Diltiazem
The dose of VYTORIN should not exceed 10/40 mg/day [see Warnings and Precautions (5.1), Drug Interactions (7.3), and Clinical Pharmacology (12.3)].
Other Concomitant Lipid-Lowering Therapy
The safety and effectiveness of VYTORIN administered with fibrates have not been established. Therefore, the combination of VYTORIN and fibrates should be avoided [see Warnings and Precautions (5.1) and Drug Interactions (7.2 and 7.8)].
There is an increased risk of myopathy when simvastatin is used concomitantly with fibrates (especially gemfibrozil). Combination therapy with gemfibrozil should be avoided because of an increase in simvastatin exposure with concomitant use. [See Warnings and Precautions (5.1) and Drug Interactions (7.2 and 7.8).]
16 HOW SUPPLIED/STORAGE AND HANDLING
No. 3873 — Tablets VYTORIN 10/10 are white to off-white capsule-shaped tablets with code “311” on one side.
They are supplied as follows:
NDC 66582-311-31 bottles of 30
NDC 66582-311-54 bottles of 90
NDC 66582-311-82 bottles of 1000 (If repackaged in blisters, then opaque or light-resistant blisters should be used.)
NDC 66582-311-87 bottles of 10,000 (If repackaged in blisters, then opaque or light-resistant blisters should be used.)
NDC 66582-311-28 unit dose packages of 100.
No. 3874 — Tablets VYTORIN 10/20 are white to off-white capsule-shaped tablets with code “312” on one side.
They are supplied as follows:
NDC 66582-312-31 bottles of 30
NDC 66582-312-54 bottles of 90
NDC 66582-312-82 bottles of 1000 (If repackaged in blisters, then opaque or light-resistant blisters should be used.)
NDC 66582-312-87 bottles of 10,000 (If repackaged in blisters, then opaque or light-resistant blisters should be used.)
NDC 66582-312-28 unit dose packages of 100.
No. 3875 — Tablets VYTORIN 10/40 are white to off-white capsule-shaped tablets with code “313” on one side.
They are supplied as follows:
NDC 66582-313-31 bottles of 30
NDC 66582-313-54 bottles of 90
NDC 66582-313-74 bottles of 500 (If repackaged in blisters, then opaque or light-resistant blisters should be used.)
NDC 66582-313-86 bottles of 5000 (If repackaged in blisters, then opaque or light-resistant blisters should be used.)
NDC 66582-313-52 unit dose packages of 50.
No. 3876 — Tablets VYTORIN 10/80 are white to off-white capsule-shaped tablets with code “315” on one side.
They are supplied as follows:
NDC 66582-315-31 bottles of 30
NDC 66582-315-54 bottles of 90
NDC 66582-315-74 bottles of 500 (If repackaged in blisters, then opaque or light-resistant blisters should be used.)
NDC 66582-315-66 bottles of 2500 (If repackaged in blisters, then opaque or light-resistant blisters should be used.)
NDC 66582-315-52 unit dose packages of 50.
Storage
Store at 20-25°C (68-77°F). [See USP Controlled Room Temperature.] Keep container tightly closed.
Storage of 10,000, 5000, and 2500 count bottles
Store bottle of 10,000 VYTORIN 10/10 and 10/20, 5000 VYTORIN 10/40, and 2500 VYTORIN 10/80 capsule-shaped tablets at 20-25°C (68-77°F). [See USP Controlled Room Temperature.] Store in original container until time of use. When product container is subdivided, repackage into a tightly-closed, light-resistant container. Entire contents must be repackaged immediately upon opening.
17 PATIENT COUNSELING INFORMATION
[See FDA-Approved Patient Labeling (17.5).]
Patients should be advised to adhere to their National Cholesterol Education Program (NCEP)-recommended diet, a regular exercise program, and periodic testing of a fasting lipid panel.
Patients should be advised about substances they should not take concomitantly with VYTORIN [see Warnings and Precautions (5.1)]. Patients should also be advised to inform other physicians prescribing a new medication that they are taking VYTORIN.
17.1 Muscle Pain
All patients starting therapy with VYTORIN should be advised of the risk of myopathy and told to report promptly any unexplained muscle pain, tenderness or weakness. The risk of this occurring is increased when taking certain types of medication or consuming larger quantities of grapefruit juice. They should discuss all medication, both prescription and over the counter, with their healthcare professional.
17.2 Liver Enzymes
It is recommended that liver function tests be performed before the initiation of VYTORIN, and thereafter when clinically indicated. Patients titrated to the 10/80-mg dose should receive an additional test prior to titration, 3 months after titration to the 10/80-mg dose, and periodically thereafter (e.g., semiannually) for the first year of treatment.
17.3 Pregnancy
Women of childbearing age should be advised to use an effective method of birth control to prevent pregnancy while using VYTORIN. Discuss future pregnancy plans with your patients, and discuss when to stop taking VYTORIN if they are trying to conceive. Patients should be advised that if they become pregnant they should stop taking VYTORIN and call their healthcare professional.
17.4 Breast-feeding
Women who are breast-feeding should be advised to not use VYTORIN. Patients who have a lipid disorder and are breast-feeding should be advised to discuss the options with their healthcare professional.
17.5 FDA-Approved Patient Labeling
VYTORIN® (ezetimibe/simvastatin) Tablets
Patient Information about VYTORIN (VI-tor-in)
Generic name: ezetimibe/simvastatin tablets
Read this information carefully before you start taking VYTORIN. Review this information each time you refill your prescription for VYTORIN as there may be new information. This information does not take the place of talking with your doctor about your medical condition or your treatment. If you have any questions about VYTORIN, ask your doctor. Only your doctor can determine if VYTORIN is right for you.
What is VYTORIN?
VYTORIN contains two cholesterol-lowering medications, ezetimibe and simvastatin, available as a tablet in four strengths:
- VYTORIN 10/10 (ezetimibe 10 mg/simvastatin 10 mg)
- VYTORIN 10/20 (ezetimibe 10 mg/simvastatin 20 mg)
- VYTORIN 10/40 (ezetimibe 10 mg/simvastatin 40 mg)
- VYTORIN 10/80 (ezetimibe 10 mg/simvastatin 80 mg)
VYTORIN is a medicine used to lower levels of total cholesterol, LDL (bad) cholesterol, and fatty substances called triglycerides in the blood. In addition, VYTORIN raises levels of HDL (good) cholesterol. VYTORIN is for patients who cannot control their cholesterol levels by diet and exercise alone. You should stay on a cholesterol-lowering diet while taking this medicine.
VYTORIN works to reduce your cholesterol in two ways. It reduces the cholesterol absorbed in your digestive tract, as well as the cholesterol your body makes by itself. VYTORIN does not help you lose weight. VYTORIN has not been shown to reduce heart attacks or strokes more than simvastatin alone.
For more information about cholesterol, see the section called “What should I know about high cholesterol?”
Who should not take VYTORIN?
Do not take VYTORIN:
- If you are allergic to ezetimibe or simvastatin, the active ingredients in VYTORIN, or to the inactive ingredients. For a list of inactive ingredients, see the “Inactive ingredients” section at the end of this information sheet.
- If you have active liver disease or repeated blood tests indicating possible liver problems.
- If you are pregnant, or think you may be pregnant, or planning to become pregnant or breast-feeding.
- If you are a woman of childbearing age, you should use an effective method of birth control to prevent pregnancy while using VYTORIN.
VYTORIN has not been studied in children under 10 years of age.
What should I tell my doctor before and while taking VYTORIN?
Tell your doctor right away if you experience unexplained muscle pain, tenderness, or weakness. This is because on rare occasions, muscle problems can be serious, including muscle breakdown resulting in kidney damage.
The risk of muscle breakdown is greater at higher doses of VYTORIN.
The risk of muscle breakdown is greater in patients with kidney problems.
Taking VYTORIN with certain substances can increase the risk of muscle problems. It is particularly important to tell your doctor if you are taking any of the following:
- cyclosporine
- danazol
- antifungal agents (such as itraconazole or ketoconazole)
- fibric acid derivatives (such as gemfibrozil, bezafibrate, or fenofibrate)
- the antibiotics erythromycin, clarithromycin, and telithromycin
- HIV protease inhibitors (such as indinavir, nelfinavir, ritonavir, and saquinavir)
- the antidepressant nefazodone
- amiodarone (a drug used to treat an irregular heartbeat)
- verapamil or diltiazem (a drug used to treat high blood pressure, chest pain associated with heart disease, or other heart conditions)
- large quantities of grapefruit juice (>1 quart daily)
- large doses (≥1 g/day) of niacin or nicotinic acid
Tell your doctor if you are taking niacin or a niacin-containing product, as this may increase your risk of muscle problems, especially if you are Chinese.
It is also important to tell your doctor if you are taking coumarin anticoagulants (drugs that prevent blood clots, such as warfarin).
Tell your doctor about any prescription and nonprescription medicines you are taking or plan to take, including natural or herbal remedies.
Tell your doctor about all your medical conditions including allergies.
Tell your doctor if you:
- drink substantial quantities of alcohol or ever had liver problems. VYTORIN may not be right for you.
- are pregnant or plan to become pregnant. Do not use VYTORIN if you are pregnant, trying to become pregnant or suspect that you are pregnant. If you become pregnant while taking VYTORIN, stop taking it and contact your doctor immediately.
- are breast-feeding. Do not use VYTORIN if you are breast-feeding.
Tell other doctors prescribing a new medication that you are taking VYTORIN.
How should I take VYTORIN?
Your doctor has prescribed your dose of VYTORIN. The available doses of VYTORIN are 10/10, 10/20, 10/40, and 10/80. The usual daily starting dose is VYTORIN 10/20.
- Take VYTORIN once a day, in the evening, with or without food.
- Try to take VYTORIN as prescribed. If you miss a dose, do not take an extra dose. Just resume your usual schedule.
- Continue to follow a cholesterol-lowering diet while taking VYTORIN. Ask your doctor if you need diet information.
- Keep taking VYTORIN unless your doctor tells you to stop. If you stop taking VYTORIN, your cholesterol may rise again.
What should I do in case of an overdose?
Contact your doctor immediately.
What are the possible side effects of VYTORIN?
See your doctor regularly to check your cholesterol level and to check for side effects. Your doctor may do blood tests to check your liver before you start taking VYTORIN and during treatment.
In clinical studies patients reported the following common side effects while taking VYTORIN: headache, muscle pain, and diarrhea (see What should I tell my doctor before and while taking VYTORIN?).
The following side effects have been reported in general use with VYTORIN or with ezetimibe or simvastatin tablets (tablets that contain the active ingredients of VYTORIN):
- allergic reactions including swelling of the face, lips, tongue, and/or throat that may cause difficulty in breathing or swallowing (which may require treatment right away), rash, hives; raised red rash, sometimes with target-shaped lesions; joint pain; muscle pain; alterations in some laboratory blood tests; liver problems (sometimes serious); inflammation of the pancreas; nausea; dizziness; tingling sensation; depression; gallstones; inflammation of the gallbladder; trouble sleeping; poor memory; erectile dysfunction; breathing problems including persistent cough and/or shortness of breath or fever.
Tell your doctor if you are having these or any other medical problems while on VYTORIN. This is not a complete list of side effects. For a complete list, ask your doctor or pharmacist.
What should I know about high cholesterol?
Cholesterol is a type of fat found in your blood. Cholesterol comes from two sources. It is produced by your body and it comes from the food you eat. Your total cholesterol is made up of both LDL and HDL cholesterol.
LDL cholesterol is called “bad” cholesterol because it can build up in the wall of your arteries and form plaque. Over time, plaque build-up can cause a narrowing of the arteries. This narrowing can slow or block blood flow to your heart, brain, and other organs. High LDL cholesterol is a major cause of heart disease and one of the causes for stroke.
HDL cholesterol is called “good” cholesterol because it keeps the bad cholesterol from building up in the arteries.
Triglycerides also are fats found in your body.
General Information about VYTORIN
Medicines are sometimes prescribed for conditions that are not mentioned in patient information leaflets. Do not use VYTORIN for a condition for which it was not prescribed. Do not give VYTORIN to other people, even if they have the same condition you have. It may harm them.
This summarizes the most important information about VYTORIN. If you would like more information, talk with your doctor. You can ask your pharmacist or doctor for information about VYTORIN that is written for health professionals. For additional information, visit the following web site: vytorin.com.
Inactive ingredients:
Butylated hydroxyanisole NF, citric acid monohydrate USP, croscarmellose sodium NF, hypromellose USP, lactose monohydrate NF, magnesium stearate NF, microcrystalline cellulose NF, and propyl gallate NF.
Issued May 2010
9619517
Manufactured for:
Merck/Schering-Plough Pharmaceuticals
North Wales, PA 19454, USA
By:
MSD Technology Singapore Pte. Ltd.
Singapore 637766
| VYTORIN
ezetimibe simvastin tablet |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| Labeler - Lake Erie Medical DBA Quality Care Products LLC (831276758) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Lake Erie Medical DBA Quality Care Products LLC | 831276758 | relabel(49999-957) | |