CYANOKIT- hydroxocobalamin injection, powder, lyophilized, for solution
Meridian Medical Technologies, Inc.
----------
HIGHLIGHTS OF PRESCRIBING INFORMATIONThese highlights do not include all the information needed to use Cyanokit safely and effectively. See full prescribing information for Cyanokit.
Cyanokit® (hydroxocobalamin for injection) 5 g for intravenous infusion Initial U.S. Approval: 1975 RECENT MAJOR CHANGESInterference with Clinical Laboratory Evaluations and Clinical Methods (5.5) 4/2011 INDICATIONS AND USAGECyanokit contains hydroxocobalamin, an antidote indicated for the treatment of known or suspected cyanide poisoning. (1.1) DOSAGE AND ADMINISTRATION
DOSAGE FORMS AND STRENGTHSCONTRAINDICATIONSNone (4) WARNINGS AND PRECAUTIONS
ADVERSE REACTIONSMost common adverse reactions (>5%) include transient chromaturia, erythema, rash, increased blood pressure, nausea, headache, and injection site reactions. (6) To report SUSPECTED ADVERSE REACTIONS contact Meridian Medical Technologies TM , Inc. at 1-800-776-3637, or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. USE IN SPECIFIC POPULATIONS
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling. Revised: 4/2011 |
FULL PRESCRIBING INFORMATION
1 INDICATIONS AND USAGE
1.2 Identifying Patients with Cyanide Poisoning
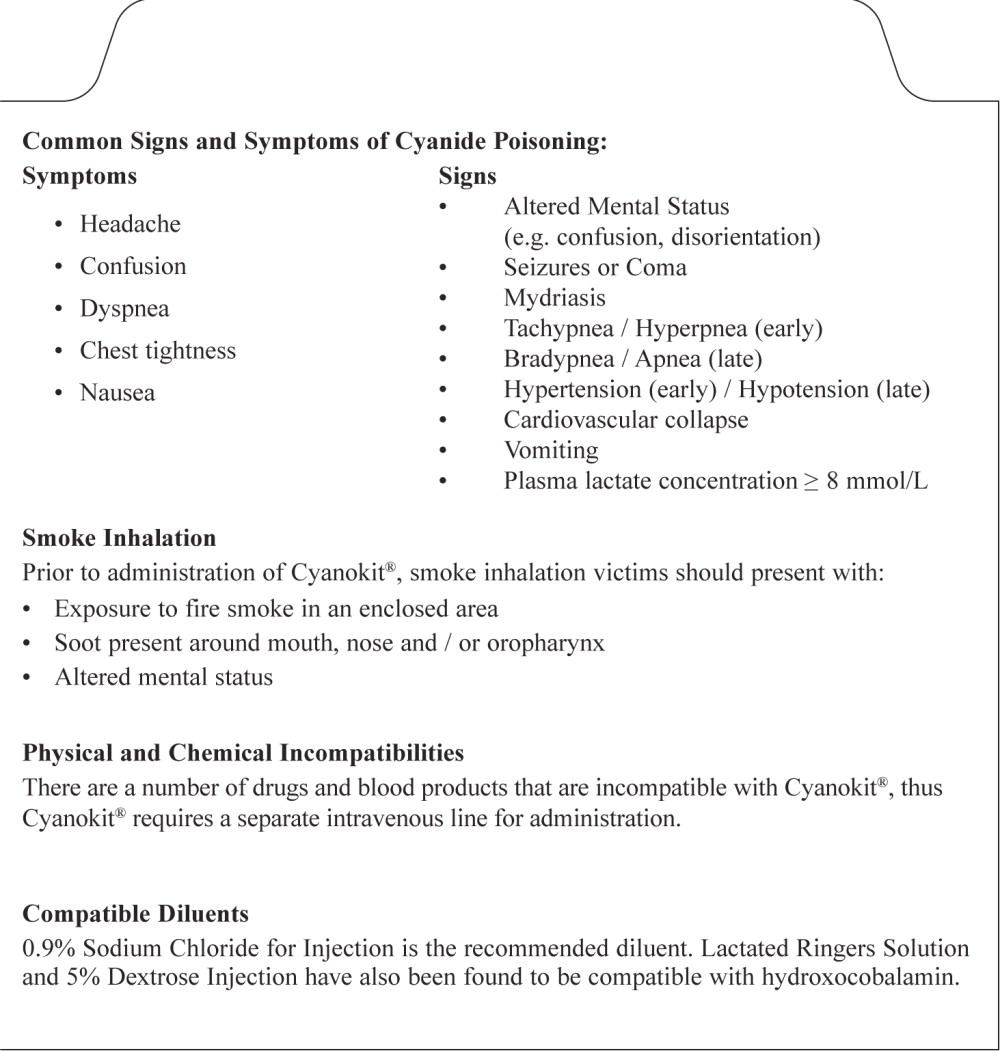
Cyanide poisoning may result from inhalation, ingestion, or dermal exposure to various cyanide-containing compounds, including smoke from closed-space fires. Sources of cyanide poisoning include hydrogen cyanide and its salts, cyanogenic plants, aliphatic nitriles, and prolonged exposure to sodium nitroprusside.
The presence and extent of cyanide poisoning are often initially unknown. There is no widely available, rapid, confirmatory cyanide blood test. Treatment decisions must be made on the basis of clinical history and signs and symptoms of cyanide intoxication. If clinical suspicion of cyanide poisoning is high, Cyanokit should be administered without delay.
| Symptoms | Signs |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
In some settings, panic symptoms including tachypnea and vomiting may mimic early cyanide poisoning signs. The presence of altered mental status (e.g., confusion and disorientation) and/or mydriasis is suggestive of true cyanide poisoning although these signs can occur with other toxic exposures as well.
The expert advice of a regional poison control center may be obtained by calling 1-800-222-1222.
Smoke Inhalation
Not all smoke inhalation victims will have cyanide poisoning and may present with burns, trauma, and exposure to other toxic substances making a diagnosis of cyanide poisoning particularly difficult. Prior to administration of Cyanokit, smoke-inhalation victims should be assessed for the following:
- Exposure to fire or smoke in an enclosed area
- Presence of soot around the mouth, nose or oropharynx
- Altered mental status
Although hypotension is highly suggestive of cyanide poisoning, it is only present in a small percentage of cyanide-poisoned smoke inhalation victims. Also indicative of cyanide poisoning is a plasma lactate concentration ≥ 10 mmol/L (a value higher than that typically listed in the table of signs and symptoms of isolated cyanide poisoning because carbon monoxide associated with smoke inhalation also contributes to lactic acidemia). If cyanide poisoning is suspected, treatment should not be delayed to obtain a plasma lactate concentration.
1.3 Use with Other Cyanide Antidotes
Caution should be exercised when administering other cyanide antidotes simultaneously with Cyanokit, as the safety of co-administration has not been established. If a decision is made to administer another cyanide antidote with Cyanokit, these drugs should not be administered concurrently in the same intravenous line. [see Dosage and Administration (2.3)].
2 DOSAGE AND ADMINISTRATION
Comprehensive treatment of acute cyanide intoxication requires support of vital functions. Cyanokit should be administered in conjunction with appropriate airway, ventilatory and circulatory support.
2.1 Recommended Dosing
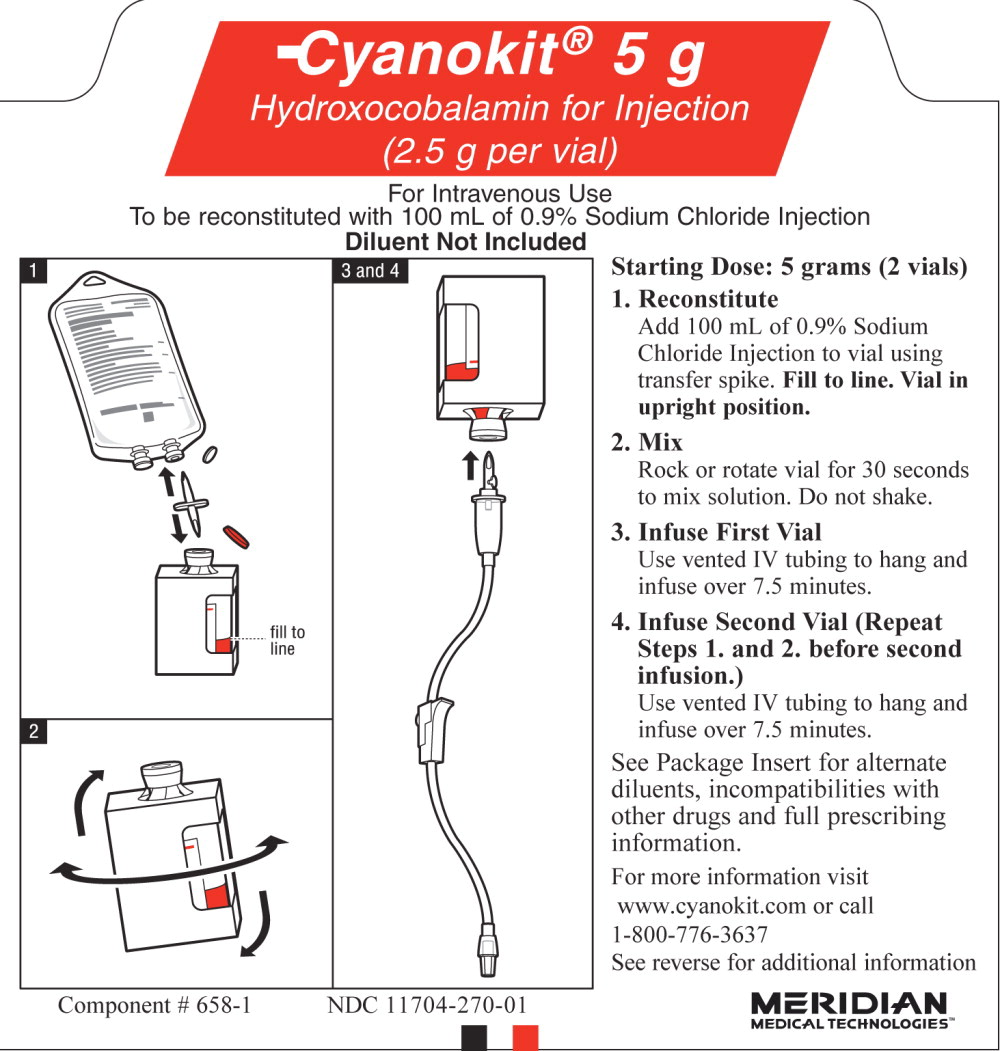
The starting dose of hydroxocobalamin for adults is 5 g (i.e., both 2.5 g vials) administered as an intravenous infusion over 15 minutes (approximately 15 mL/min), i.e., 7.5 minutes/vial. Depending upon the severity of the poisoning and the clinical response, a second dose of 5 g may be administered by intravenous infusion for a total dose of 10 g. The rate of infusion for the second dose may range from 15 minutes (for patients in extremis) to two hours, as clinically indicated.
2.2 Preparation of Solution for Infusion
Each 2.5 g vial of hydroxocobalamin for injection is to be reconstituted with 100 mL of diluent (not provided with Cyanokit) using the supplied sterile transfer spike. The recommended diluent is 0.9% Sodium Chloride injection (0.9% NaCl). Lactated Ringers injection and 5% Dextrose injection (D5W) have also been found to be compatible with hydroxocobalamin and may be used if 0.9% NaCl is not readily available. The line on each vial label represents 100 mL volume of diluent. Following the addition of diluent to the lyophilized powder, each vial should be repeatedly inverted or rocked, not shaken, for at least 30 seconds prior to infusion.
Hydroxocobalamin solutions should be visually inspected for particulate matter and color prior to administration. If the reconstituted solution is not dark red or if particulate matter is seen after the solution has been appropriately mixed, the solution should be discarded.
2.3 Incompatibility Information
Physical incompatibility (particle formation) and chemical incompatibility were observed with the mixture of hydroxocobalamin in solution with selected drugs that are frequently used in resuscitation efforts. Hydroxocobalamin is also chemically incompatible with sodium thiosulfate and sodium nitrite and has been reported to be incompatible with ascorbic acid. Therefore, these and other drugs should not be administered simultaneously through the same intravenous line as hydroxocobalamin.
Simultaneous administration of hydroxocobalamin and blood products (whole blood, packed red cells, platelet concentrate and/or fresh frozen plasma) through the same intravenous line is not recommended. However, blood products and hydroxocobalamin can be administered simultaneously using separate intravenous lines (preferably on contralateral extremities, if peripheral lines are being used).
3 DOSAGE FORMS AND STRENGTHS
Cyanokit (hydroxocobalamin for injection) 5 g for intravenous infusion consists of 2 vials, each containing 2.5 g lyophilized hydroxocobalamin dark red crystalline powder for injection. After reconstitution, each vial contains hydroxocobalamin for injection, 25 mg/mL. Administration of both vials constitutes a single dose [see How Supplied/Storage and Handling (16) for full kit description].
5 WARNINGS AND PRECAUTIONS
5.1 Emergency Patient Management
In addition to Cyanokit, treatment of cyanide poisoning must include immediate attention to airway patency, adequacy of oxygenation and hydration, cardiovascular support, and management of any seizure activity. Consideration should be given to decontamination measures based on the route of exposure.
5.2 Allergic Reactions
Use caution in the management of patients with known anaphylactic reactions to hydroxocobalamin or cyanocobalamin. Consideration should be given to use of alternative therapies, if available.
Allergic reactions may include: anaphylaxis, chest tightness, edema, urticaria, pruritus, dyspnea, and rash.
Allergic reactions including angioneurotic edema have also been reported in postmarketing experience.
5.3 Blood Pressure Increase
Many patients with cyanide poisoning will be hypotensive; however, elevations in blood pressure have also been observed in known or suspected cyanide poisoning victims.
Elevations in blood pressure (≥ 180 mmHg systolic or ≥ 110 mmHg diastolic) were observed in approximately 18% of healthy subjects (not exposed to cyanide) receiving hydroxocobalamin 5 g and 28% of subjects receiving 10 g. Increases in blood pressure were noted shortly after the infusions were started; the maximal increase in blood pressure was observed toward the end of the infusion. These elevations were generally transient and returned to baseline levels within 4 hours of dosing.
5.4 Use of Blood Cyanide Assay
While determination of blood cyanide concentration is not required for management of cyanide poisoning and should not delay treatment with Cyanokit, collecting a pretreatment blood sample may be useful for documenting cyanide poisoning as sampling post-Cyanokit use may be inaccurate.
5.5 Interference with Clinical Laboratory Evaluations and Clinical Methods
Clinical Laboratory Evaluations
Because of its deep red color, hydroxocobalamin has been found to interfere with colorimetric determination of certain laboratory parameters (e.g., clinical chemistry, hematology, coagulation, and urine parameters). In-vitro tests indicated that the extent and duration of the interference are dependent on numerous factors such as the dose of hydroxocobalamin, analyte, methodology, analyzer, hydroxocobalamin concentration, and partially on the time between sampling and measurement.
Based on in-vitro studies and pharmacokinetic data obtained in healthy volunteers, the following table (Table 2) describes laboratory interference that may be observed following a 5 g dose of hydroxocobalamin. Interference following a 10 g dose can be expected to last up to an additional 24 hours. The extent and duration of interference in cyanide-poisoned patients may differ. Results may vary substantially from one analyzer to another; therefore, caution should be used when reporting and interpreting laboratory results.
| Laboratory | No Interference | Artificially | Artificially | Un-predictable | Duration of |
|---|---|---|---|---|---|
| Parameter | Observed | Increased * | Decreased * | Interference | |
|
* ≥10% interference observed on at least 1 analyzer |
|||||
|
Analyzers used: ACL Futura (Instrumentation Laboratory), AxSYM®/ArchitectTM (Abbott), BM Coasys110 (Boehringer Mannheim), CellDyn 3700® (Abbott), Clinitek® 500 (Bayer), Cobas Integra® 700, 400 (Roche), Gen-S Coultronics, Hitachi 917, STA® Compact, Vitros® 950 (Ortho Diagnostics) |
|||||
| Clinical | Calcium | Creatinine | ALT | Phosphate | 24 hours with the exception of bilirubin (up to 4 days) |
| Chemistry | Sodium | Bilirubin | Amylase | Uric Acid | |
| Potassium | Triglycerides | AST | |||
| Chloride | Cholesterol | CK | |||
| Urea | Total protein | CKMB | |||
| GGT | Glucose Albumin Alkaline phosphatase | LDH | |||
| Hematology | erythrocytes Hematocrit MCV Leukocytes Lymphocytes Monocytes Eosinophils Neutrophils Platelets | Hemoglobin MCH MCHC Basophils | 12 - 16 hours | ||
| Coagulation | aPTT PT (Quick or INR) | 24 - 48 hours | |||
| Urinalysis | pH (with all doses) | pH (with equivalent doses of <5 g) | 48 hours up to 8 days; color changes may persist up to 28 days | ||
| Glucose | |||||
| Protein Erythrocytes Leukocytes Ketones Bilirubin Urobilinogen Nitrite | |||||
6 ADVERSE REACTIONS
Serious adverse reactions with hydroxocobalamin include allergic reactions and increases in blood pressure [see Warnings and Precautions (5.2, 5.3)].
6.1 Clinical Studies Experience
Because clinical trials were conducted under widely varying conditions, adverse reaction rates observed in the clinical trials may not reflect the rates observed in practice.
Experience in Healthy Subjects
A double-blind, randomized, placebo-controlled, single-ascending-dose (2.5, 5, 7.5, and 10 g) study was conducted to assess the safety, tolerability, and pharmacokinetics of hydroxocobalamin in 136 healthy adult subjects. Because of the dark red color of hydroxocobalamin, the two most frequently occurring adverse reactions were chromaturia (red-colored urine) which was reported in all subjects receiving a 5 g dose or greater; and erythema (skin redness), which occurred in most subjects receiving a 5 g dose or greater. Adverse reactions reported in at least 5% of the 5 g dose group and corresponding rates in the 10 g and placebo groups are shown in Table 3.
|
* Rashes were predominantly acneiform |
||||
| 5 g Dose Group | 10 g Dose Group | |||
|
ADR |
Hydroxocobalamin N=66 n (%) |
Placebo N=22 n (%) |
Hydroxocobalamin N=18 n (%) |
Placebo N=6 n (%) |
| Chromaturia (red colored urine) | 66 (100) | 0 | 18 (100) | 0 |
| Erythema | 62 (94) | 0 | 18 (100) | 0 |
| Rash* | 13 (20) | 0 | 8 (44) | 0 |
| Blood pressure increased | 12 (18) | 0 | 5 (28) | 0 |
| Nausea | 4 (6) | 1 (5) | 2 (11) | 0 |
| Headache | 4 (6) | 1 (5) | 6 (33) | 0 |
| Lymphocyte percent decreased | 5 (8) | 0 | 3 (17) | 0 |
| Infusion site reaction | 4 (6) | 0 | 7 (39) | 0 |
In this study, the following adverse reactions were reported to have occurred in a dose-dependent fashion and with greater frequency than observed in placebo-treated cohorts: increased blood pressure (particularly diastolic blood pressure), rash, nausea, headache and infusion site reactions. All were mild to moderate in severity and resolved spontaneously when the infusion was terminated or with standard supportive therapies.
Other adverse reactions reported in this study and considered clinically relevant were:
- Eye disorders: swelling, irritation, redness
- Gastrointestinal disorders: dysphagia, abdominal discomfort, vomiting, diarrhea, dyspepsia, hematochezia
- General disorders and administration site conditions: peripheral edema, chest discomfort
- Immune system disorders: allergic reaction
- Nervous system disorders: memory impairment, dizziness
- Psychiatric disorders: restlessness
- Respiratory, thoracic and mediastinal disorders: dyspnea, throat tightness, dry throat
- Skin and subcutaneous tissue disorders: urticaria, pruritus
- Vascular disorders: hot flush
Experience in Known or Suspected Cyanide Poisoning Victims
Four open-label, uncontrolled, clinical studies (one of which was prospective and three of which were retrospective) were conducted in known or suspected cyanide-poisoning victims. A total of 245 patients received hydroxocobalamin treatment in these studies. Systematic collection of adverse events was not done in all of these studies and interpretation of causality is limited due to the lack of a control group and due to circumstances of administration (e.g., use in fire victims). Adverse reactions reported in these studies listed by system organ class included:
- Cardiac disorders: ventricular extrasystoles
- Investigations: electrocardiogram repolarization abnormality, heart rate increased
- Respiratory, thoracic, and mediastinal disorders: pleural effusion
Adverse reactions common to both the studies in known or suspected cyanide poisoning victims and the study in healthy volunteers are listed in the healthy volunteer section only and are not duplicated in this list.
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category C. There are no adequate and well controlled studies of Cyanokit in pregnant women. In animal studies, hydroxocobalamin caused skeletal and visceral (soft tissue) abnormalities at exposures (based on AUC) similar to human exposures at the therapeutic dose. Cyanokit should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. Because cyanide readily crosses the placenta, maternal cyanide poisoning results in fetal cyanide poisoning. Timely treatment of the pregnant mother may be lifesaving for both mother and fetus.
In animal studies, pregnant rats and rabbits received Cyanokit (75, 150, or 300 mg/kg/d) during the period of organogenesis. Following intraperitoneal dosing in rats and intravenous dosing in rabbits, maternal exposures were equivalent to 0.5, 1, or 2 times the human exposure at the therapeutic dose (based on AUC). In the high dose groups for both species, maternal toxicity occurred, and there was a reduced number of live fetuses due to embryofetal resorptions. In addition, decreased live fetal weight occurred in high dose rats, but not in rabbits. Incomplete skeletal ossification occurred in both rats and rabbits. In rats, two fetuses of the high dose group and two fetuses of the mid dose group (each from a different litter) had short, rudimentary or small front or hind legs. Rabbit litters and fetuses exhibited a dose dependant increase in various gross soft tissue and skeletal anomalies. The main findings in rabbits were flexed, rigid flexor or medially rotated forelimbs or hindlimbs and domed heads at external examination; enlarged anterior or posterior fontanelles of the ventricles of the brain and flat, bowed or large ribs at skeletal examination; and dilated ventricles of the brain, and thick wall of the stomach at visceral examination.
8.3 Nursing Mothers
It is not known whether hydroxocobalamin is excreted in human milk. Cyanokit may be administered in life-threatening situations, and therefore, breastfeeding is not a contraindication to its use. Because of the unknown potential for adverse reactions in nursing infants, the patient should discontinue nursing after receiving Cyanokit.
8.4 Pediatric Use
Safety and effectiveness of Cyanokit have not been established in this population. In non-US marketing experience, a dose of 70 mg/kg has been used to treat pediatric patients.
8.5 Geriatric Use
Approximately 50 known or suspected cyanide victims aged 65 or older received hydroxocobalamin in clinical studies. In general, the safety and effectiveness of hydroxocobalamin in these patients was similar to that of younger patients. No adjustment of dose is required in elderly patients.
8.6 Renal Impairment
The safety and effectiveness of Cyanokit have not been studied in patients with renal impairment.
Hydroxocobalamin and cyanocobalamin are eliminated unchanged by the kidneys. Oxalate crystals have been observed in the urine of both healthy subjects given hydroxocobalamin and patients treated with hydroxocobalamin following suspected cyanide poisoning.
10 OVERDOSAGE
No data are available about overdose with Cyanokit in adults. Should overdose occur, treatment should be directed to the management of symptoms. Hemodialysis may be effective in such a circumstance, but is only indicated in the event of significant hydroxocobalamin-related toxicity. Because of its deep red color, hydroxocobalamin may interfere with the performance of hemodialysis machines [see Warnings and Precautions (5.5)].
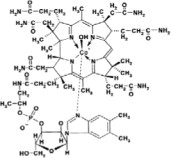
11 DESCRIPTION
Hydroxocobalamin, the active ingredient in Cyanokit, is cobinamide dihydroxide dihydrogen phosphate (ester), mono (inner salt), 3'-ester with 5,6-dimethyl-1-α-D-ribofuranosyl-1H-benzimidazole. The drug substance is the hydroxylated active form of vitamin B12 and is a large molecule in which a trivalent cobalt ion is coordinated in four positions by a tetrapyrol (or corrin) ring. It is a hygroscopic, odorless, dark red, crystalline powder that is freely soluble in water and ethanol, and practically insoluble in acetone and diethyl ether. Hydroxocobalamin has a molecular weight of 1346.36 atomic mass units, an empirical formula of C62H89CoN13O15P and the following structural formula:
Cyanokit (hydroxocobalamin for injection) 5 g for intravenous infusion is a cyanide antidote package which contains two colorless 250 mL glass vials, each of which contains 2.5 g dark red lyophilized hydroxocobalamin, pH adjusted with hydrochloric acid, two transfer spikes, one intravenous administration set, one quick use reference guide and one package insert.
Each 2.5 g vial of hydroxocobalamin for injection is to be reconstituted with 100 mL of 0.9% NaCl, to give a dark red injectable solution (25 mg/mL). If 0.9% NaCl is not readily available, 100 mL of either Lactated Ringers injection or 5% Dextrose injection (D5W) may be used as the diluent. Diluent is not included in the Cyanokit. The pH of the reconstituted product ranges from 3.5 to 6.0.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Cyanide is an extremely toxic poison. In the absence of rapid and adequate treatment, exposure to a high dose of cyanide can result in death within minutes due to the inhibition of cytochrome oxidase resulting in arrest of cellular respiration. Specifically, cyanide binds rapidly with cytochrome a3, a component of the cytochrome c oxidase complex in mitochondria. Inhibition of cytochrome a3 prevents the cell from using oxygen and forces anaerobic metabolism, resulting in lactate production, cellular hypoxia and metabolic acidosis. In massive acute cyanide poisoning, the mechanism of toxicity may involve other enzyme systems as well. Signs and symptoms of acute systemic cyanide poisoning may develop rapidly within minutes, depending on the route and extent of cyanide exposure.
The action of Cyanokit in the treatment of cyanide poisoning is based on its ability to bind cyanide ions. Each hydroxocobalamin molecule can bind one cyanide ion by substituting it for the hydroxo ligand linked to the trivalent cobalt ion, to form cyanocobalamin, which is then excreted in the urine.
12.2 Pharmacodynamics
Administration of Cyanokit to cyanide-poisoned patients with the attendant formation of cyanocobalamin resulted in increases in blood pressure and variable changes in heart rate upon initiation of hydroxocobalamin infusions.
12.3 Pharmacokinetics
Following intravenous administration of hydroxocobalamin significant binding to plasma proteins and low molecular weight physiological compounds occurs, forming various cobalamin-(III) complexes by replacing the hydroxo ligand. The low molecular weight cobalamins-(III) formed, including hydroxocobalamin, are termed “free cobalamins-(III)”; the sum of free and protein-bound cobalamins is termed “total cobalamins-(III)”. In order to reflect the exposure to the sum of all derivatives, pharmacokinetics of cobalamins-(III) (i.e. cobalamin-(III) entity without specific ligand) were investigated instead of hydroxocobalamin alone, using the concentration unit μg eq/mL.
Dose-proportional pharmacokinetics were observed following single dose intravenous administration of 2.5 to 10 g of hydroxocobalamin in healthy volunteers. Mean free and total cobalamins-(III) Cmax values of 113 and 579 μg eq/mL, respectively, were determined following a dose of 5 g of hydroxocobalamin. Similarly, mean free and total cobalamins-(III) Cmax values of 197 and 995 μg eq/mL, respectively, were determined following the dose of 10 g of hydroxocobalamin. The predominant mean half-life of free and total cobalamins-(III) was found to be approximately 26 to 31 hours at both the 5 g and 10 g dose level.
The mean total amount of cobalamins-(III) excreted in urine during the collection period of 72 hours was about 60% of a 5 g dose and about 50% of a 10 g dose of hydroxocobalamin. Overall, the total urinary excretion was calculated to be at least 60 to 70% of the administered dose. The majority of the urinary excretion occurred during the first 24 hours, but red-colored urine was observed for up to 35 days following the intravenous infusion.
When normalized for body weight, male and female subjects revealed no major differences in pharmacokinetic parameters of free and total cobalamins-(III) following the administration of 5 and 10 g of hydroxocobalamin.
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Long-term animal studies have not been performed to evaluate the carcinogenic potential of hydroxocobalamin. Hydroxocobalamin was negative in the following mutagenicity assays: in vitro bacterial reverse mutation assay using Salmonella typhimurium and Escherichia coli strains, an in-vitro assay of the tk locus in mouse lymphoma cells, and an in-vivo rat micronucleus assay.
The effect of hydroxocobalamin on fertility has not been evaluated.
13.2 Animal Pharmacology
Evidence of the effectiveness of hydroxocobalamin for treatment of cyanide poisoning was obtained primarily from studies in animals due to the ethical considerations of performing such controlled studies in humans. While the results of these animal studies cannot be extrapolated to humans with certainty, the extrapolation is supported by the understanding of the pathophysiologic mechanisms of the toxicity of cyanide and the mechanisms of the protective effect of hydroxocobalamin as examined in dogs. In addition, the results of uncontrolled human studies and the animal study establish that hydroxocobalamin is likely to produce clinical benefit in humans.
The effectiveness of hydroxocobalamin was examined in a randomized, placebo-controlled, blinded study in cyanide-poisoned adult dogs assigned to treatment with vehicle (0.9% saline), or 75 or 150 mg/kg hydroxocobalamin. Anesthetized dogs were poisoned by intravenous administration of a lethal dose of potassium cyanide. Dogs then received vehicle or 75 or 150 mg/kg hydroxocobalamin, administered intravenously over 7.5 minutes. The 75 and 150 mg/kg doses are approximately equivalent to 5 and 10 g of hydroxocobalamin (respectively) in humans based on both body weight and the Cmax of hydroxocobalamin (total cobalamins-(III)). Survival at 4 hours and at 14 days was significantly greater in low-and high-dose groups compared with dogs receiving vehicle alone (Table 4). Hydroxocobalamin reduced whole blood cyanide concentrations by approximately 50% by the end of the infusion compared with vehicle.
|
Parameter | Treatment | ||
|---|---|---|---|
|
Vehicle N=17 | Cyanokit | ||
| 75 mg/kg
N=19 | 150 mg/kg
N=18 |
||
| Survival at Hour 4, n (%) | 7 (41) | 18 (95) | 18 (100) |
| Survival at Day 14, n (%) | 3 (18) | 15 (79) | 18 (100) |
Histopathology revealed brain lesions that were consistent with cyanide-induced hypoxia. The incidence of brain lesions was markedly lower in hydroxocobalamin treated animals compared to vehicle treated groups.
14 CLINICAL STUDIES
Due to ethical considerations, no controlled human efficacy studies have been performed. A controlled animal study demonstrated efficacy in cyanide-poisoned adult dogs [see Animal Pharmacology (13.2)].
14.1 Smoke Inhalation Victims
A prospective, uncontrolled, -open-label study was carried out in 69 subjects who had been exposed to smoke inhalation from fires. Subjects had to be over 15 years of age, present with soot in the mouth and expectoration (to indicate significant smoke exposure), and have altered neurological status. The median hydroxocobalamin dose was 5 g with a range from 4 to 15 g.
Fifty of 69 subjects (73%) survived following treatment with hydroxocobalamin. Nineteen subjects treated with hydroxocobalamin did not survive. Fifteen patients treated with hydroxocobalamin were in cardiac arrest initially at the scene; 13 of these subjects died and 2 survived.
Of the 42 subjects with pretreatment cyanide levels considered to be potentially toxic, 28 (67%) survived. Of the 19 subjects whose pretreatment cyanide levels were considered potentially lethal, 11 (58%) survived. Of the 50 subjects who survived, 9 subjects (18%) had neurological sequelae at hospital discharge. These included dementia, confusion, psychomotor retardation, anterograde amnesia, intellectual deterioration moderate cerebellar syndrome, aphasia, and memory impairment.
Two additional retrospective, uncontrolled studies were carried out in subjects who had been exposed to cyanide from fire or smoke inhalation. Subjects were treated with up to 15 g of hydroxocobalamin. Survival in these two studies was 34 of 61 (56%) for one study, and 30 of 72 (42%) for the second.
14.2 Cyanide Poisoning by Ingestion or Inhalation
A retrospective, uncontrolled study was carried out in 14 subjects who had been exposed to cyanide from sources other than from fire or smoke (i.e., ingestion or inhalation). Subjects were treated with 5 to 20 g of hydroxocobalamin. Eleven of 12 subjects whose blood cyanide concentration was known had initial blood cyanide levels considered to be above the lethal threshold.
Ten of 14 subjects (71%) survived, following administration of hydroxocobalamin. One of the four subjects who died had presented in cardiac arrest. Of the 10 subjects who survived, only 1 subject had neurological sequelae at hospital discharge. This subject had post-anoxic encephalopathy, with memory impairment, considered to be due to cyanide poisoning.
14.3 Cross-Study Findings
Experience with Dosing Greater than 10 g of Hydroxocobalamin
Across all four uncontrolled studies, 10 patients who did not demonstrate a full response to 5 or 10 g-doses of hydroxocobalamin were treated with more than 10 g of hydroxocobalamin. One of these 10 patients survived with unspecified neurological sequelae.
16 HOW SUPPLIED/STORAGE AND HANDLING
Each Cyanokit carton (NDC 11704-270-01) consists of the following:
- Two 250 mL glass vials, each containing lyophilized hydroxocobalamin for injection, 2.5 g
- Two sterile transfer spikes
- One sterile intravenous infusion set
- One quick use reference guide
- One package insert
Diluent is not included
Lyophilized form: Store at 25°C (77°F); excursions permitted to 15-30°C (59 to 86°F) [see USP Controlled Room Temperature].
Cyanokit may be exposed during short periods to the temperature variations of usual transport (15 days submitted to temperatures ranging from 5 to 40°C (41 to 104°F), transport in the desert (4 days submitted to temperatures ranging from 5 to 60°C (41 to 140°F)) and freezing/defrosting cycles (15 days submitted to temperatures ranging from -20 to 40°C (-4 to 104°F)).
17 PATIENT COUNSELING INFORMATION
Cyanokit is indicated for cyanide poisoning and in this setting, patients will likely be unresponsive or may have difficulty in comprehending counseling information.
17.1 Erythema and Chromaturia
Patients should be advised that skin redness may last up to 2 weeks and urine coloration may last for up to 5 weeks after administration of Cyanokit. While it is not known if the skin redness predisposes to photosensitivity, patients should be advised to avoid direct sun while their skin remains discolored.
17.2 Rash
In some patients an acneiform rash may appear anywhere from 7 to 28 days following hydroxocobalamin treatment. This rash will usually resolve without treatment within a few weeks.
17.3 Pregnancy and Breastfeeding
Patients should be advised that maternal cyanide poisoning results in fetal cyanide poisoning. Treatment for cyanide poisoning may be lifesaving for both mother and fetus. Patients should notify their physician if they were pregnant during therapy with Cyanokit [see Use In Specific Populations (8.1)]. It is not known whether hydroxocobalamin is excreted in human milk.
Patient Information
Cyanokit (hydroxocobalamin for injection) 5 g for intravenous infusion
Treatment for known or suspected cyanide poisoning
What is Cyanokit?
Cyanokit is an emergency treatment (antidote) used in patients with known or suspected cyanide poisoning. Cyanide is a chemical poison. Cyanide poisoning can happen from:
- breathing smoke from household and industrial fires
- breathing or swallowing cyanide
- having your skin exposed to cyanide
Cyanide poisoning is a life-threatening condition because cyanide stops your body from being able to use oxygen. You can die if your body does not have enough oxygen.
Cyanokit was approved for the treatment of known or suspected cyanide poisoning based on testing:
- how well it worked in animals (It is not ethical to poison people with cyanide in order to test a treatment.)
- its safety in people with cyanide poisoning
How is Cyanokit used?
Cyanokit is given through a vein (intravenous) over 15 minutes by an emergency care provider or doctor. A second dose may be given to you if needed.
What are possible side effects with Cyanokit?
Serious side effects may include:
- allergic reactions Signs of a serious allergic reaction include chest tightness, trouble breathing, swelling, hives, itching, and a rash.
- increased blood pressure
Other side effects may include:
- red colored urine
- red colored skin and mucous membranes, acne-like rash
- nausea, vomiting, diarrhea, bloody stools, trouble swallowing, stomach pain
- throat tightness, dry throat
- headache, dizziness, memory problems, restlessness
- infusion site reaction
- eye swelling, irritation, or redness
- swelling of feet and ankles
- irregular heart beat, increased heart rate
- fluid in lungs
These are not all the side effects with Cyanokit.
After treatment with Cyanokit:
- Skin and urine redness. Skin redness may last up to 2 weeks. Avoid sun exposure while your skin is red. Urine redness may last up to 5 weeks.
- Acne-like rash. An acne-like rash may appear 7 to 28 days after treatment with Cyanokit. This rash usually goes away without any treatment.
- Pregnancy. Be sure to tell your doctor immediately if you were pregnant or think you may have been pregnant during treatment with Cyanokit. Treatment for cyanide poisoning may save your life and the life of your unborn baby.
- Breastfeeding. Talk to your doctor if you breastfeed your child. The ingredient in Cyanokit may pass into your breast milk.
Talk to your doctor about any side effect that bothers you or that does not go away.
Manufactured by:
Merck Santé s.a.s.,
Semoy, France
Distributed by
Meridian Medical Technologies™, Inc.
Columbia, MD 21046
A wholly-owned subsidiary of King Pharmaceuticals®, Inc.
1-800-776-3637
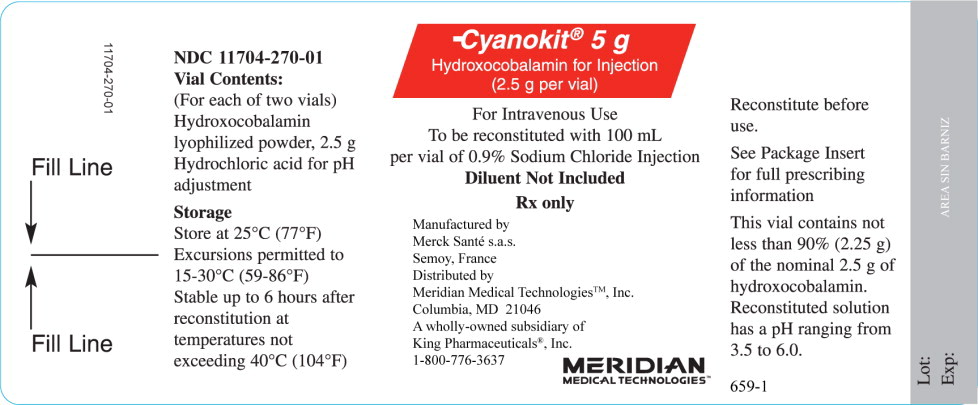
PACKAGE LABEL – PRINCIPAL DISPLAY PANEL – 5 g BOTTLE LABEL
Cyanokit ® 5 g
Hydroxocobalamin for Injection
(2.5 g per vial)
For Intravenous Use
To be reconstituted with 100 mL
per vial of 0.9% Sodium Chloride Injection
Diluent Not Included
Rx Only
Manufactured by:
Merck Santé s.a.s.,
Semoy, France
Distributed by
Meridian Medical TechnologiesTM, Inc.
Columbia, MD 21046
A wholly-owned subsidiary of King Pharmaceuticals®, Inc.
1-800-776-3637
MERIDIAN
MEDICAL TECHNOLOGIES™
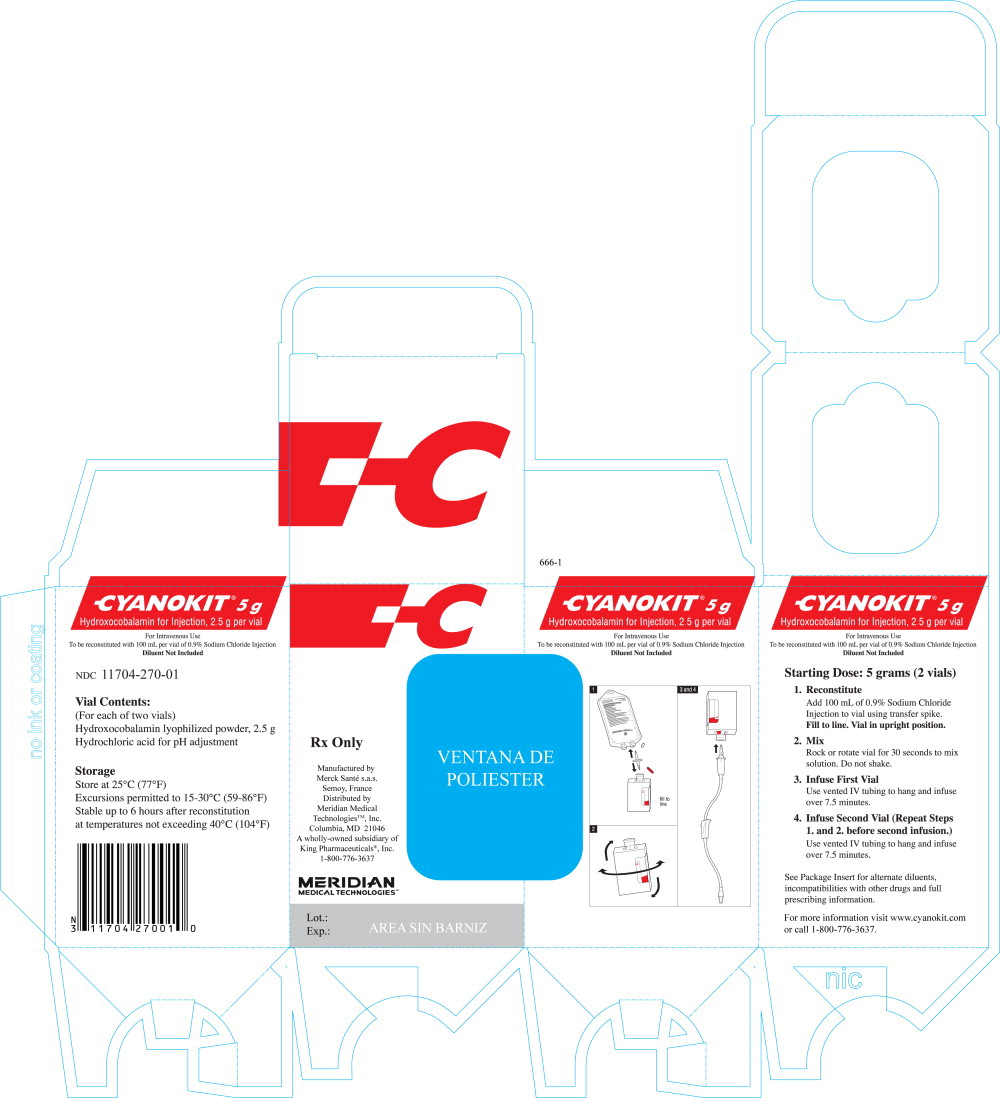
PACKAGE LABEL – PRINCIPAL DISPLAY PANEL – 5 g INNER CARTON
Cyanokit ® 5 g
Hydroxocobalamin for Injection
(2.5 g per vial)
For Intravenous Use
To be reconstituted with 100 mL
per vial of 0.9% Sodium Chloride Injection
Diluent Not Included
Rx Only
Manufactured by:
Merck Santé s.a.s.,
Semoy, France
Distributed by
Meridian Medical TechnologiesTM, Inc.
Columbia, MD 21046
A wholly-owned subsidiary of King Pharmaceuticals®, Inc.
1-800-776-3637
MERIDIAN
MEDICAL TECHNOLOGIES™
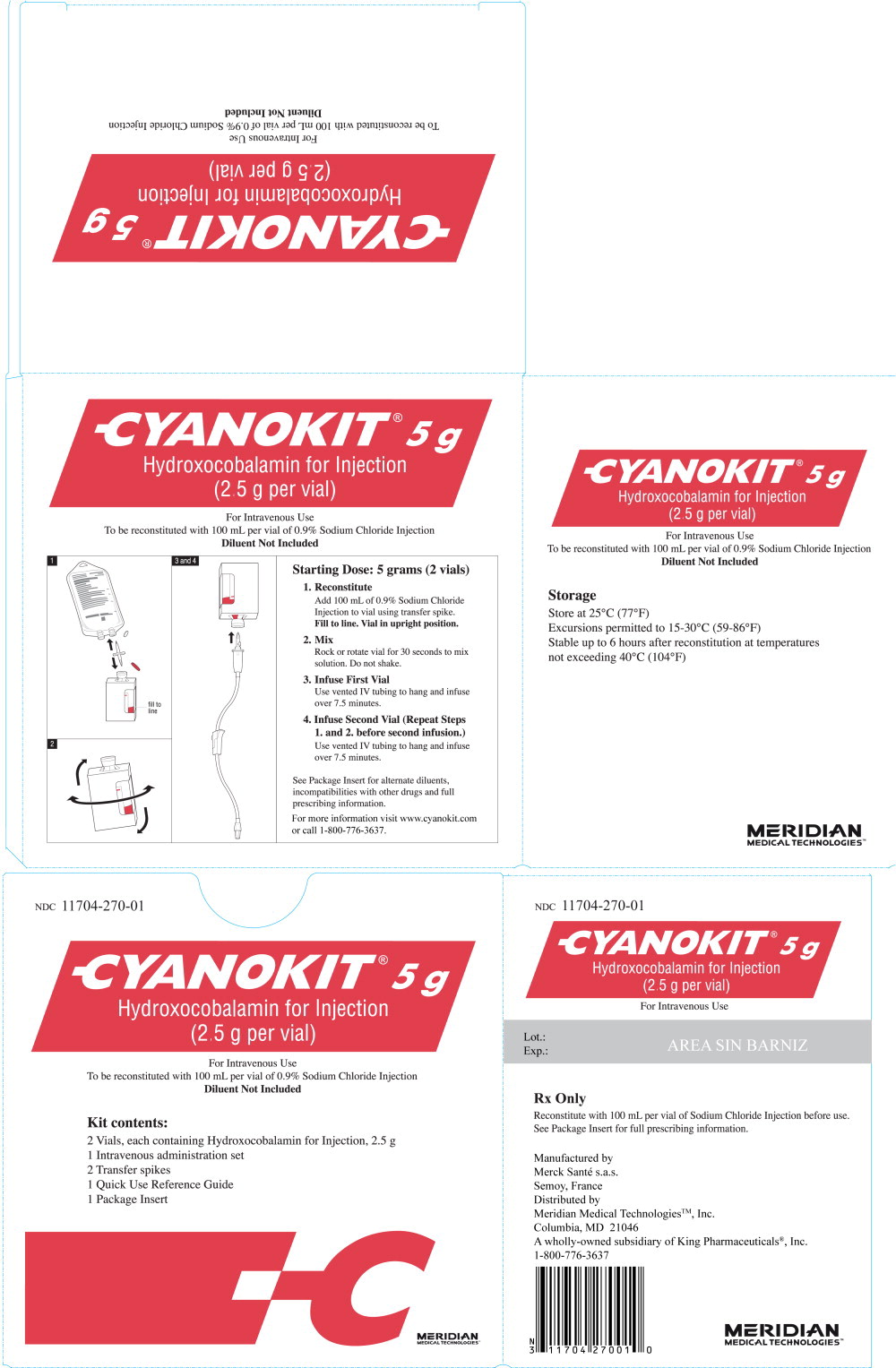
PACKAGE LABEL – PRINCIPAL DISPLAY PANEL – 5 g OUTER CARTON
Cyanokit ® 5 g
Hydroxocobalamin for Injection
(2.5 g per vial)
For Intravenous Use
To be reconstituted with 100 mL
per vial of 0.9% Sodium Chloride Injection
Diluent Not Included
Rx Only
Manufactured by:
Merck Santé s.a.s.,
Semoy, France
Distributed by
Meridian Medical TechnologiesTM, Inc.
Columbia, MD 21046
A wholly-owned subsidiary of King Pharmaceuticals®, Inc.
1-800-776-3637
MERIDIAN
MEDICAL TECHNOLOGIES™
| CYANOKIT
hydroxocobalamin injection, powder, lyophilized, for solution |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| Labeler - Meridian Medical Technologies, Inc. (167671341) |
| Registrant - Merck Santé s.a.s (384953134) |