HUMATE-P
-
human coagulation factor viii/von willebrand factor complex
CSL BEHRING LLC
----------
Antihemophilic Factor/von Willebrand Factor Complex (Human), Dried, PasteurizedHumate-P®
Manufactured by:
CSL Behring GmbH
35041 Marburg, Germany
US License No. 1765
Distributed by:
CSL Behring LLC
Kankakee, IL 60901 USA
Rx only
DESCRIPTION
Antihemophilic Factor/von Willebrand Factor Complex (Human), Dried, Pasteurized, Humate-P®, is a stable, purified, sterile, lyophilized concentrate of Antihemophilic Factor (Human) and von Willebrand Factor (VWF) (Human) to be administered by the intravenous route in the treatment of patients with classical hemophilia (hemophilia A) and von Willebrand disease (VWD) (see CLINICAL PHARMACOLOGY).
Humate-P® is purified from the cold insoluble fraction of pooled human fresh-frozen plasma and contains highly purified and concentrated Antihemophilic Factor/von Willebrand Factor Complex (Human). Humate-P® has a high degree of purity with a low amount of non-factor proteins. Fibrinogen is less than or equal to 0.2 mg/mL. Humate-P® has a higher Factor potency than cryoprecipitate preparations. Each vial of Humate-P® contains the labeled amount of Factor VIII activity in international units (IU). Additionally, each vial of Humate-P® also contains the labeled amount of von Willebrand Factor:Ristocetin Cofactor (VWF:RCo) activity expressed in IU (see DOSAGE AND ADMINISTRATION). An IU is defined by the current international standard established by the World Health Organization. One IU Factor VIII or 1 IU VWF:RCo is approximately equal to the level of Factor VIII or VWF:RCo found in 1.0 mL of fresh-pooled human plasma.
Upon reconstitution with the volume of diluent provided (Sterile Diluent for Humate-P®), each mL of Humate-P® contains 40 to 80 IU Factor VIII activity, 72 to 224 IU VWF:RCo activity1, 15 to 33 mg of glycine, 3.5 to 9.3 mg of sodium citrate, 2 to 5.3 mg of sodium chloride, 8 to 16 mg of Albumin (Human), 2 to 14 mg of other proteins and 10 to 20 mg of total proteins.
Humate-P® has been demonstrated in several studies to contain the high molecular weight multimers of VWF. This component is considered to be important for correcting the coagulation defect in patients with VWD.1-5 When administered to patients with VWD (types 1, 2, or 3)6, bleeding time decreased.2,5,7-9 This effect was correlated with the presence of a multimeric composition of VWF similar to that found in normal plasma.2,4,5,7,9
Humate-P® contains anti-A and anti-B blood group isoagglutinins (see PRECAUTIONS, Laboratory Tests).
This product is prepared from pooled human plasma collected from U.S. licensed facilities in the U.S.
All Source Plasma used in the manufacture of this product was tested by FDA-licensed Nucleic Acid Tests (NAT) for HCV and HIV-1 and found to be nonreactive (negative).
An investigational NAT for HBV was also performed on all Source Plasma used in the manufacture of this product and found to be nonreactive (negative). The aim of the HBV test is to detect low levels of viral material, however, the significance of a nonreactive (negative) result has not been established.
- 1
- This correlates to a VWF:RCo to Factor VIII activity average ratio of 2.4 which is used to calculate the nominal values of VWF:RCo activity and is the average VWF:RCo activity.
Virus Reduction Capacity
The manufacturing procedure for Humate-P® includes multiple processing steps that reduce the risk of virus transmission. The virus reduction capacity of the manufacturing process was evaluated in a series of in vitro spiking experiments; the steps were: 1) cryoprecipitation; 2) Al(OH)3 adsorption, glycine precipitation and NaCl precipitation, studied in combination; and 3) pasteurization in aqueous solution at 60°C for 10 hours. Total mean cumulative virus reductions ranged from 6.0 to ≥ 11.3 log10 as shown in Table 1.
| Virus Studied | Cryoprecipitation | Al(OH)3 adsorption / glycine precipitation / NaCl precipitation | Pasteurization | Total Cumulative |
|---|---|---|---|---|
| [log10] | [log10] | [log10] | [log10] | |
| N.D.: Not determined; N.A.: Not applicable HIV-1: Human immunodeficiency virus type 1, model for HIV types 1 and 2 BVDV: Bovine viral diarrhea virus, model for HCV and WNV PRV: Pseudorabies virus, model for large enveloped DNA viruses (e.g., herpes virus) WNV: West Nile virus HAV: Hepatitis A virus CPV: Canine parvovirus, model for parvovirus B19 B19V: Parvovirus B19 |
||||
|
||||
| Enveloped Viruses | ||||
| HIV-1 | N.D. | 3.6 | ≥ 6.4 | ≥ 10.0 |
| BVDV | N.D. | 2.4 | ≥ 8.9 | ≥ 11.3 |
| PRV | 1.6 | 3.7 | 4.6 | 9.9 |
| WNV | N.D. | N.D. | ≥ 7.8 | N.A. |
| Non-Enveloped Viruses | ||||
| HAV | 1.5 | 2.4 | 4.2 | 8.1 |
| CPV | 1.5 | 3.4 | 1.1 | 6.0 |
| B19V | N.D. | N.D. | ≥ 3.9* | N.A. |
CLINICAL PHARMACOLOGY
General
The Antihemophilic Factor/von Willebrand Factor Complex consists of two different noncovalently bound proteins (Factor VIII and von Willebrand factor). Factor VIII is an essential cofactor in activation of Factor X leading ultimately to formation of thrombin and fibrin. The VWF promotes platelet aggregation and platelet adhesion on damaged vascular endothelium; it also serves as a stabilizing carrier protein for the procoagulant protein Factor VIII.10,11 The activity of VWF is measured as VWF:RCo.
Pharmacokinetics in Hemophilia A
After intravenous injection of Antihemophilic Factor/von Willebrand Factor Complex (Human), Dried, Pasteurized, Humate-P®, in humans, there is a rapid increase of plasma Factor VIII activity (FVIII:C) followed by a rapid decrease in activity and a subsequent slower rate of decrease in activity. Studies with Humate-P® in hemophilic subjects have demonstrated a mean half-life of 12.2 hours (range: 8.4 to 17.4 hours).
Pharmacokinetics in von Willebrand disease
Pharmacokinetic studies of Humate-P® have been performed with cohorts of subjects in the nonbleeding state. Wide inter-subject variability was observed in pharmacokinetic values obtained from these studies.
The pharmacokinetics of Humate-P® were evaluated in 41 subjects in a prospective US study in the nonbleeding state prior to a surgical procedure. Subjects received 60 IU VWF:RCo/kg body weight of Humate-P®. Sixteen subjects had type 1 VWD, two had type 2A, four had type 2B, six had type 2M, and 13 had type 3. The median terminal half-life of VWF:RCo was 11 hours (range: 3.5 to 33.6 hours), excluding five subjects with a half-life exceeding the blood sampling time of 24 or 48 hours. The median clearance and volume of distribution at steady state were 3.1 mL/hr/kg (range: 1 to 16.6 mL/hr/kg) and 53 mL/kg (range: 29 to 141 mL/kg), respectively. The median in vivo recovery for VWF:RCo activity was 2.4 IU/dL per IU/kg (range: 1.1 to 4.2). High molecular weight multimers were measured in 13 subjects with type 3 VWD; 11 had absent or barely detectable multimers at baseline. Of those 11 subjects, all had some high molecular weight multimers present 24 hours after infusion of Humate-P®.
Pharmacokinetics were also evaluated in 28 subjects in a European study in the nonbleeding state prior to a surgical procedure. Subjects received 80 IU VWF:RCo/kg body weight of Humate-P®. Ten subjects had type 1 VWD, 10 had type 2A, one had type 2M, and seven had type 3. The median terminal half-life of VWF:RCo was 10 hours (range: 2.8 to 28.3 hours), excluding one subject with a half-life exceeding the blood sampling time of 48 hours. The median clearance and volume of distribution at steady state were 4.8 mL/hr/kg (range: 2.1 to 53 mL/hr/kg) and 59 mL/kg (range: 32 to 290 mL/kg), respectively. The median in vivo recovery for VWF:RCo activity was 1.9 IU/dL per IU/kg (range: 0.6 to 4.5). Infusion of Humate-P® corrected the defect of the multimer pattern in subjects with types 2A and 3 VWD. High molecular weight multimers were detectable until at least 8 hours after infusion.
Based on the small sample size evaluation, it appears that age, sex, and types of VWD have no impact on the pharmacokinetics of VWF:RCo.
CLINICAL STUDIES
Clinical efficacy of Humate-P® in the control of bleeding in subjects with VWD was determined by a retrospective review of clinical safety and efficacy data obtained from 97 Canadian VWD subjects who were provided with product under an Emergency Drug Release Program. Dosage schedule and duration of therapy were determined by the judgment of the medical practitioner.
There were 514 requests for product use for surgery, bleeding or prophylaxis in the 97 Canadian subjects. Of these, product was not used in 151 cases, and follow-up safety and/or efficacy information was available for 303 (83%) of the remaining 363 requests. In many cases, product from one request was used for several treatment courses in one subject. Therefore, there are more reported treatment courses than requests.
Humate-P® was administered to 97 subjects, in 530 treatment courses: 73 for surgery, 344 for treatment of bleeding and 20 for prophylaxis of bleeding. For 93 "other" uses, the majority involved dental procedures, diagnostic procedures, prophylaxis prior to a procedure, or a test dose.
A summary of the number of subjects and bleeding episodes treated, by VWD type, and corresponding efficacy rating is provided in Table 2. The efficacy rating was excellent/good in 100% of bleeding episodes treated in type 1, 2A and 2B subjects. In type 3 subjects, 95% of the bleeding episodes were rated as excellent/good and a poor (or no) response was observed in the remaining 5% of bleeding episodes treated.
| Diagnosis | ||||||||
|---|---|---|---|---|---|---|---|---|
| Type 1 VWD | Type 2A VWD | Type 2B VWD | Type 3 VWD | |||||
| NUMBER OF SUBJECTS | 13 | - | 2 | - | 10 | - | 21 | - |
| Excellent/good | 13 | 100% | 2 | 100% | 10 | 100% | 18 | 86% |
| Poor/none | - | - | - | - | - | - | 3 | 14% |
| NUMBER OF EVENTS | 32 | - | 17 | - | 60 | - | 208 | - |
| Excellent/good | 32 | 100% | 17 | 100% | 60 | 100% | 198 | 95% |
| Poor/none | - | - | - | - | - | - | 10 | 5% |
For pediatric subjects a summary of the number of subjects and bleeding episodes treated, by VWD type, and corresponding efficacy rating is provided in Table 3. The efficacy rating was excellent/good in 100% of bleeding episodes treated in infants (types 2A, 3), children (types 1, 2A, 2B) and adolescents (types 1, 2B). In type 3 children and adolescents, 90% and 96% of the bleeding episodes were rated as excellent/good and a poor/none response was observed in the remaining 10% and 4% of the bleeding episodes, respectively.
| Diagnosis | ||||||||
|---|---|---|---|---|---|---|---|---|
| Type 1 VWD | Type 2A VWD | Type 2B VWD | Type 3 VWD | |||||
| NUMBER OF SUBJECTS | 4 | - | 2 | - | 5 | - | 12 | - |
| Excellent/good | 4 | 100% | 2 | 100% | 5 | 100% | 9 | 75% |
| Poor/none | - | - | - | - | - | - | 3 | 25% |
| NUMBER OF EVENTS | 8 | - | 17 | - | 22 | - | 138 | - |
| Excellent/good | 8 | 100% | 17 | 100% | 22 | 100% | 128 | 93% |
| Poor/none | - | - | - | - | - | - | 10 | 7% |
The dosing information (all subjects) for bleeding events is summarized in Table 4.
| Type/Location | ||||||
|---|---|---|---|---|---|---|
| Digestive System | Nose+Mouth +Pharynx | Integument System | Female Genital System | Musculo-skeletal | ||
| No. of Subjects | 14 | 29 | 11 | 4 | 22 | |
| Loading Dose | Mean Dose (SD)* | 62.1 (31.1) | 66.9 (24.3) | 73.4 (37.7) | 88.5 (28.3) | 50.2 (24.9) |
| No. of Infusions† | 37 | 127 | 22 | 7 | 107 | |
| Maintenance Dose | Mean Dose (SD) | 61.5 (38.0) | 67.5 (22.4) | 56.5 (63.3) | 74.5 (17.7) | 63.8 (28.8) |
| No. of Infusions† | 250 | 55 | 4 | 15 | 121 | |
| No. of Treatment | Mean (SD) | 4.6 (3.6) | 1.4 (1.2) | 1.1 (0.4) | 2.8 (2.9) | 2.0 (1.9) |
| Days/Bleeding | No. of Events | 49 | 130 | 22 | 9 | 108 |
| Event | ||||||
| No. of Infusions/day (in relation to first treatment day) | ||||||
| No. of Subjects | 14 | 29 | 11 | 4 | 22 | |
| Day 1‡ | Mean (SD) | 1.2 (0.4) | 1.1 (0.2) | 1.0 (0.2) | 1.0 (0.0) | 1.0 (0.1) |
| No. of Events | 49 | 130 | 22 | 9 | 108 | |
| No. of Subjects | 13 | 9 | 3 | 1 | 15 | |
| Day 2 | Mean (SD) | 1.2 (0.6) | 1.3 (0.5) | 1.0 (0.0) | 1.0 (-) | 1.2 (0.5) |
| No. of Events | 41 | 12 | 3 | 1 | 26 | |
| No. of Subjects | 12 | 6 | - | 2 | 10 | |
| Day 3 | Mean (SD) | 1.5 (0.8) | 1.4 (0.7) | - | 1.0 (0.0) | 1.2 (0.4) |
| No. of Events | 25 | 9 | - | 3 | 18 | |
Two clinical studies, one in the US and one in Europe, investigated the safety and hemostatic efficacy of Humate-P® in subjects with VWD undergoing surgery.
The US clinical study investigated the safety and hemostatic efficacy of Humate-P® in 35 subjects (21 females and 14 males) with VWD undergoing surgery. Subjects ranged from 3 to 75 years old (mean 32.9); seven were 15 years old or younger, and two were 65 years old or older. Twelve had type 1 VWD, two had type 2A, three had type 2B, five had type 2M, and 13 had type 3. Twenty-eight of the surgical procedures were classified as major (e.g., orthopedic joint replacement, intracranial surgery, multiple tooth extractions, laparoscopic cholecystectomy), four as minor (e.g., placement of intravenous access device), and three subjects had oral surgery2. Seven of the 13 subjects with type 3 VWD had major surgery.
The first 15 subjects received a loading dose of Humate-P® corresponding to 1.5 times the "full dose" (defined as the dose predicted to achieve a peak VWF:RCo level of 100 IU/dL as determined by each subject's calculated in vivo recovery (IVR) and baseline VWF:RCo levels); the loading dose did not vary with the type of surgery performed (i.e., major, minor, or oral). The remaining 20 subjects were dosed based on individual pharmacokinetic assessments and target peak VWF:RCo levels of 80 to 100 IU/dL for major surgery and 50 to 60 IU/dL for minor or oral surgery, respectively. All 35 subjects received initial maintenance doses corresponding to 0.5 times the full dose at intervals of 6, 8, or 12 hours after surgery as determined by their individual half-lives for VWF:RCo; subsequent maintenance doses were adjusted based on regular measurements of trough VWF:RCo and FVIII:C levels. The median duration of treatment was 1 day (range: 1 to 2 days) for oral surgery, 5 days (range: 3 to 7 days) for minor surgery, and 5.5 days (range: 2 to 26 days) for major surgery.
The European clinical study also investigated the safety and hemostatic efficacy of Humate-P® in 27 subjects (18 females and nine males) with VWD undergoing surgery. This study did not have a pre-stated hypothesis to evaluate hemostatic efficacy. The ages of these subjects ranged from 5 to 81 years old (median 46); one was 5 years old, and five were above 65 years old. Ten subjects had type 1 VWD, nine had type 2A, one had type 2M, and seven had type 3. Sixteen of the surgical procedures were classified as major (orthopedic joint replacement, hysterectomy, multiple tooth extractions, laparoscopic adnexectomy, laparoscopic cholecystectomy, and basal cell carcinoma excision). Six of the seven subjects with type 3 VWD had major surgery.
Dosing was individualized based on a pharmacokinetic assessment performed before surgery. The median duration of treatment was 3.5 days (range: 1 to 17 days) for minor surgery and 9 days (range: 1 to 17 days) for major surgery.
In both the US and European studies, assessments of hemostatic efficacy were performed at the end of surgery, 24 hours after the last Humate-P® infusion, and at the end of the study (14 days following surgery). The investigators judged hemostatic efficacy at the end of surgery as "effective" (excellent/good) in 32 (91.4%) (95% CI: 78.5% to 97.6%) of the 35 subjects in the US study and in 25 (96%) (95% CI: 82% to 99.8%) of the 26 subjects in the European study for whom data were available.
In the US study, the hemostatic efficacy of Humate-P® was classified by investigators as excellent/good for all surgical subjects. In the European study, hemostatic efficacy as assessed by the investigator at the end of the study (Day 14) was either excellent or good in all cases.
A summary of the overall hemostatic efficacy of Humate-P® in preventing excessive bleeding in subjects participating in either the US or European study is presented in Table 5. Humate-P® was effective in preventing excessive bleeding during and after surgery.
| Hemostatic Assessment | |||
|---|---|---|---|
| Number of Subjects | Effective (Excellent / Good) | 95% CI for Effective Proportion* | |
|
|||
| US study† | 35 | 35 (100%) | 91.3% – 100% |
| European study‡ | 27 | 26 (96.3%) | 82.5% – 99.8% |
In the US study, all efficacy assessments were reviewed by an independent Data Safety Monitoring Board (DSMB). The DSMB agreed with the investigators' assessments of the overall hemostatic efficacy for all but two subjects (neither of whom had type 3 VWD). Based on this, the DSMB judged hemostatic efficacy as "effective" in 33 (94.3%) (95% CI: 81.1% to 99.0%) of the 35 subjects.
In the US study, the median actual estimated blood loss did not exceed the median expected blood loss, regardless of the type of surgery. Table 6 shows the median expected and actual estimated blood loss during surgery in the US study.
| Estimated Blood Loss | Oral Surgery (n=3) | Minor Surgery (n=4) | Major Surgery (n=28) | Total (n=35) |
|---|---|---|---|---|
| Expected – Median (range) mL | 10 (5-50) | 8 (0-15) | 50 (0-300)* | 20 (0-300)* |
| Actual – Median (range) mL | 3 (0-15) | 3 (0-10) | 26 (0-300)† | 18 (0-300)† |
In the US study, four subjects received transfusions, three due to adverse events and one due to pre-existing anemia. In the European study, one subject received transfusions to treat pre-existing anemia.
- 2
- Oral surgery is defined as removal of fewer than three teeth, if the teeth are non-molars and have no bony involvement. Removal of more than one impacted wisdom tooth is considered major surgery due to the expected difficulty of the surgery and the expected blood loss, particularly in subjects with type 2A or type 3 VWD. Removal of more than two teeth is considered major surgery in all patients.
Viral Safety
Clinical evidence of the viral safety of Humate-P® was obtained in additional studies. In one study, all evaluable subjects (31 of 67) who received Humate-P® remained HBs-antigen negative. None of the 31 subjects developed hepatitis B infection or showed clinical signs of NANB hepatitis infection.12
In an additional study, a total of 32 lots of Humate-P® were administered to a cohort of 26 hemophilic or VWD subjects who had not previously received any blood products. Markers for hepatitis B virus and liver enzymes (ALT and AST) were tested at regular intervals as recommended by the International Committee on Thrombosis and Hemostasis. The study showed no significant elevation in liver enzyme levels over an observation period ranging from 2 months to 12 months. The 10 subjects not previously vaccinated remained seronegative for markers of hepatitis B infection as well as for markers of infection with hepatitis A virus, CMV, Epstein-Barr virus and HIV. No subject developed any signs of an infectious disease.13
In a retrospective study, all 155 subjects evaluated remained negative for the presence of HIV-1 antibodies for time periods ranging from four months to nine years from initial administration of product. Sixty-seven of these subjects were also tested for HIV-2 antibodies and all remained seronegative.14
INDICATIONS AND USAGE
Antihemophilic Factor/von Willebrand Factor Complex (Human), Dried, Pasteurized, Humate-P®, is indicated in adult patients for treatment and prevention of bleeding in hemophilia A (classical hemophilia). Humate-P® is also indicated in adult and pediatric patients with von Willebrand disease for (1) treatment of spontaneous and trauma-induced bleeding episodes and (2) prevention of excessive bleeding during and after surgery. This applies to patients with severe VWD as well as patients with mild to moderate VWD where use of desmopressin is known or suspected to be inadequate.
Controlled clinical trials to evaluate the safety and efficacy of prophylactic dosing with Humate-P® to prevent spontaneous bleeding have not been conducted in VWD subjects. Adequate data are not presently available on which to evaluate or to base dosing recommendations in this setting.
CONTRAINDICATIONS
Antihemophilic Factor/von Willebrand Factor Complex (Human), Dried, Pasteurized, Humate-P®, is contraindicated in individuals with a history of anaphylactic or severe systemic response to antihemophilic factor or von Willebrand factor preparations. It is also contraindicated in individuals with a known hypersensitivity to any of its components.
WARNINGS
Thromboembolic events have been reported in VWD patients receiving Antihemophilic Factor/von Willebrand Factor Complex replacement therapy, especially in the setting of known risk factors for thrombosis.15,16,17 Early reports might indicate a higher incidence in females. In addition, endogenous high levels of FVIII have also been associated with thrombosis but no causal relationship has been established. In all VWD patients in situations of high thrombotic risk receiving coagulation factor replacement therapy, caution should be exercised and antithrombotic measures should be considered. See also DOSAGE AND ADMINISTRATION.
Antihemophilic Factor/von Willebrand Factor Complex (Human), Dried, Pasteurized, Humate-P®, is made from human plasma. Products made from human plasma may contain infectious agents, such as viruses, that can cause disease. Because Humate-P® is made from human blood, it may carry a risk of transmitting infectious agents, e.g., viruses, and theoretically, the Creutzfeldt-Jakob disease (CJD) agent. The risk that such products will transmit an infectious agent has been reduced by screening plasma donors for prior exposure to certain viruses, by testing for the presence of certain current viral infections and by inactivating and/or removing certain viruses during manufacture. Stringent procedures, utilized at plasma collection centers, plasma testing laboratories, and fractionation facilities are designed to reduce the risk of virus transmission. The primary virus reduction step of the Humate-P® manufacturing process is the heat treatment of the purified, stabilized aqueous solution at 60°C for 10 hours (i.e., pasteurization). In addition, the purification procedure, which includes several precipitation steps and an adsorption step, used in the manufacture of Humate-P® also provides virus reduction capacity (see DESCRIPTION section for virus reduction factors). Despite these measures, such products may still potentially contain human pathogenic agents, including those not yet known or identified. Thus the risk of transmission of infectious agents cannot be totally eliminated. Any infections thought by a physician possibly to have been transmitted by this product should be reported by the physician or other healthcare provider to CSL Behring at 1-800-504-5434 (in the U.S. and Canada). The physician should discuss the risks and benefits of this product with the patient.
PRECAUTIONS
It is important to determine that the coagulation disorder is caused by factor VIII or VWF deficiency, since no benefit in treating other deficiencies can be expected.
Thromboembolic events have been reported in VWD patients receiving coagulation factor replacement therapy, especially in the setting of known risk factors for thrombosis. In these patients, caution should be exercised and antithrombotic measures should be considered.
As a precaution, the administration equipment and any unused Humate-P® should be discarded after use.
Information for Patients
Some viruses, such as parvovirus B19 or hepatitis A, are particularly difficult to remove or inactivate at this time. Parvovirus B19 may most seriously affect pregnant women, or immune-compromised individuals.
Although the overwhelming number of hepatitis A and parvovirus B19 cases are community acquired, there have been reports of these infections associated with the use of some plasma-derived products. Therefore, physicians should be alert to the potential symptoms of parvovirus B19 and hepatitis A infections and inform patients under their supervision receiving plasma-derived products to report potential symptoms promptly.
Symptoms of parvovirus B19 may include low-grade fever, rash, arthralgias and transient symmetric, nondestructive arthritis. Diagnosis is often established by measuring B19 specific IgM and IgG antibodies. Symptoms of hepatitis A include low grade fever, anorexia, nausea, vomiting, fatigue and jaundice. A diagnosis may be established by determination of specific IgM antibodies.
Laboratory Tests
Antihemophilic Factor/von Willebrand Factor (Human), Dried, Pasteurized, Humate-P®, contains blood group isoagglutinins (anti-A and anti-B). When very large or frequently repeated doses are needed, as when inhibitors are present or when pre- and post-surgical care is involved, patients of blood groups A, B and AB should be monitored for signs of intravascular hemolysis and decreasing hematocrit values and be treated appropriately, as required.
The Factor VIII levels of VWD patients receiving Humate-P® should be monitored using standard coagulation tests, especially in cases of surgery. Strong consideration should also be given to monitoring VWF:RCo levels in VWD patients receiving Humate-P® for the prevention of excessive bleeding during and after surgery. It is advisable to monitor trough VWF:RCo and FVIII:C levels at least once daily in order to adjust the dosage of Humate-P® as needed to avoid excessive accumulation of coagulation factors (see DOSAGE AND ADMINISTRATION).
Pregnancy Category C
Animal reproduction studies have not been conducted with Antihemophilic Factor/von Willebrand Factor (Human). It is also not known whether Humate-P® can cause fetal harm when administered to a pregnant woman or can affect reproduction capacity. Humate-P® should be given to a pregnant woman only if clearly needed.
Pediatric Use
Hemophilia A
Adequate and well-controlled studies with long-term evaluation of joint damage have not been done in pediatric subjects. Joint damage may result from suboptimal treatment of hemarthroses. For immediate control of bleeding for Hemophilia A, the general recommendations for dosing and administration for adults, found in the DOSAGE AND ADMINISTRATION section, may be referenced.
Von Willebrand Disease
The safety and effectiveness of Humate-P® for the treatment of von Willebrand disease was demonstrated in 26 pediatric subjects, including infants, children and adolescents but has not been evaluated in neonates. The safety of Humate-P® for the prevention of excessive bleeding during and after surgery was demonstrated in 8 pediatric subjects (ages 3 through 15) with VWD. Of the 34 pediatric subjects studied for both treatment of VWD and prevention of excessive bleeding during and after surgery, four were infants (1 month to under 2 years of age), 23 were children (2 through 12 years), and 7 were adolescents (13 through 15 years).
As in adults, pediatric patients should be dosed based upon weight (kg) in accordance with information in the DOSAGE AND ADMINISTRATION section.
Geriatric Use
Clinical studies of Humate-P® did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. As for all patients, dosing for geriatric patients should be appropriate to their overall situation.
ADVERSE REACTIONS
The most serious adverse reaction observed in patients receiving Antihemophilic Factor/von Willebrand Factor Complex (Human), Dried, Pasteurized, Humate-P®, is anaphylaxis. Thromboembolic events have also been observed in patients receiving Humate-P® for the treatment of VWD (see WARNINGS). Reports of thromboembolic events in VWD patients with other thrombotic risk factors receiving coagulation factor replacement therapy have been obtained from spontaneous reports, published literature, and a European clinical study. Early reports might indicate a higher incidence in females. In some cases, inhibitors to coagulation factors may occur. However, no inhibitor formation was observed in any of the clinical trials.
Although few adverse reactions have been reported in clinical studies and in the postmarketing setting in patients receiving Humate-P® for treatment of hemophilia A and VWD, the most commonly reported are allergic-anaphylactic reactions (including urticaria, chest tightness, rash, pruritus, edema, and shock). For patients undergoing surgery, the most common adverse reactions are postoperative wound or injection-site bleeding.
Adverse Reactions in Clinical Trials
Because clinical trials are conducted under widely varying conditions, the adverse reaction rates observed cannot be directly compared to rates in other clinical trials and may not reflect the rates observed in practice.
von Willebrand Disease
Treatment of VWD
Allergic symptoms, including allergic reaction, urticaria, chest tightness, rash, pruritus, and edema, were reported in 6 of 97 (6%) subjects in a Canadian retrospective study. Four of 97 (4%) subjects experienced seven adverse events that were considered to have a possible or probable relationship to the product. These included chills, phlebitis, vasodilation, paresthesia, pruritus, rash, and urticaria. All were mild in intensity with the exception of a moderate case of pruritus.
In a prospective, open-label safety and efficacy study of Humate-P® in VWD subjects with serious life- or limb-threatening bleeding or undergoing emergency surgery, seven of 71 (10%) subjects experienced nine adverse reactions. These were mild vasodilation (1/9), allergic reactions (2/9), pruritus (1/9), and paresthesia (2/9); moderate peripheral edema (1/9) and extremity pain (1/9); and severe pseudothrombocytopenia (platelet clumping with a false low reading) (1/9). Humate-P® was discontinued in the subject who experienced the peripheral edema and extremity pain.
VWD Subjects Undergoing Surgery
Among the 63 VWD subjects who received Humate-P® for prevention of excessive bleeding during and after surgery, including 1 subject who underwent colonoscopy without the planned polypectomy, the most common adverse events were postoperative hemorrhage (35 events in 19 subjects with five subjects experiencing bleeding at up to three different sites), postoperative nausea (15 subjects), and postoperative pain (11 subjects). Postoperative hemorrhagic adverse events are shown in Table 7.
| Adverse Event | Surgical Procedure Category | Number of Subjects/Events | Onset*
(Number of Events) | Severity (Number of Events) |
|||
|---|---|---|---|---|---|---|---|
| On | Post | Mild | Mod | Severe | |||
|
|||||||
| Wound/injection site bleeding | Major | 8/11 | 7 | 4 | 9 | – | 2 |
| Minor | 2/2 | 2 | – | 1 | 1 | – | |
| Oral | 2/6 | – | 6 | 3 | 3 | – | |
| Epistaxis | Major | 4/4 | 2 | 2 | 3 | 1 | – |
| Minor | 1/1 | 1 | – | 1 | – | – | |
| Cerebral hemorrhage/ subdural hematoma | Major | 1/2 | 2† | – | – | 2 | – |
| Gastrointestinal bleeding | Major | 1/3 | 3‡ | – | – | 2 | 1 |
| Menorrhagia | Major | 1/1 | 1§ | – | – | 1 | – |
| Groin bleed | Oral | 1/1 | – | 1 | 1 | – | – |
| Ear bleed | Major | 1/1 | 1 | – | 1 | – | – |
| Hemoptysis | Major | 1/1 | 1 | – | 1 | – | – |
| Hematuria | Major | 1/1 | 1 | – | 1 | – | – |
| Shoulder bleed | Major | 1/1 | 1 | – | 1 | – | – |
Table 8 lists the non-hemorrhagic adverse events reported in at least two subjects, regardless of causality, and the adverse events that were possibly related to Humate-P®. Pulmonary embolus that was considered possibly related to Humate-P® occurred in one elderly subject who underwent bilateral knee replacement.
| Body System | Adverse Event | Number of Subjects with an AE Possibly Related to Humate-P® | Number of Subjects with an AE Regardless of Causality* |
|---|---|---|---|
| Body as a Whole | Pain | – | 11 |
| Fever | – | 4 | |
| Abdominal Pain | – | 3 | |
| Infection | – | 3 | |
| Surgery | – | 3 | |
| Back Pain | – | 2 | |
| Facial Edema | – | 2 | |
| Cardiovascular | Chest Pain | – | 3 |
| Pulmonary Embolus† | 1 | 1 | |
| Thrombophlebitis† | 1 | 1 | |
| Digestive | Nausea | 1 | 15 |
| Constipation | – | 7 | |
| Vomiting | 1 | 3 | |
| Sore Throat | – | 2 | |
| Hemic and Lymphatic System | Anemia / Decreased Hemoglobin | – | 2 |
| Metabolic/Nutritional | Increased SGPT | 1 | 1 |
| Nervous | Dizziness | 1 | 5 |
| Headache | 1 | 4 | |
| Increased Sweating | – | 3 | |
| Insomnia | – | 2 | |
| Skin and Appendages | Pruritus | – | 3 |
| Rash | 1 | 1 | |
| Urogenital | Urinary Retention | – | 4 |
| Urinary Tract Infection | – | 2 | |
Eight subjects experienced 10 postoperative serious adverse events: one with subdural hematoma and intracerebral bleeding following intracranial surgery related to an underlying cerebrovascular abnormality; one with two occurrences of gastrointestinal bleeding following gastrojejunal bypass; and one each with sepsis, facial edema, infection, menorrhagia requiring hysterectomy following hysteroscopy and dilation and curettage, pyelonephritis, and pulmonary embolus.
Postmarketing Experience
The following adverse reactions have been identified during postapproval use of Humate-P®. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to Humate-P® exposure.
Adverse reactions reported in patients receiving Humate-P® for treatment of VWD or hemophilia A are allergic-anaphylactic reactions (including urticaria, chest tightness, rash, pruritus, edema, and shock), development of inhibitors to Factor VIII, and hemolysis. Additional adverse reactions reported for VWD are thromboembolic complications, chills and fever, and hypervolemia.
Evaluation and interpretation of these postmarketing events is confounded by underlying diagnoses, concomitant medications, pre-existing conditions, and inherent limitations of passive surveillance.
Healthcare professionals should report serious adverse events possibly associated with the use of Humate-P® to CSL Behring at 1-800-504-5434 or FDA's MedWatch reporting system at 1-800-FDA-1088.
DOSAGE AND ADMINISTRATION
General
Physicians should strongly consider administration of hepatitis A and hepatitis B vaccines to individuals receiving plasma derivatives. Potential risks and benefits of vaccination should be carefully weighed by the physician and discussed with the patient.
Antihemophilic Factor/von Willebrand (Human), Dried, Pasteurized, Humate-P®, is for intravenous administration only.
Each vial of Humate-P® contains the labeled amount of Factor VIII activity in IU for the treatment of hemophilia A. Additionally, each vial of Humate-P® also contains VWF:RCo activity in IU for the treatment of VWD.
Therapy for Hemophilia A
As a general rule, 1 IU of Factor VIII activity per kg body weight will increase the circulating Factor VIII level by approximately 2 IU/dL. Adequacy of treatment must be judged by the clinical effects; thus, the dosage may vary with individual cases. Although dosage must be individualized according to the needs of the patient (weight, severity of hemorrhage, presence of inhibitors), the general dosages in Table 9 are recommended for adult patients:18
| Hemorrhagic Event | Dosage (IU FVIII:C/kg body weight) |
|---|---|
Minor hemorrhage:
| Loading dose 15 IU FVIII:C/kg to achieve FVIII:C plasma level of approximately 30% of normal; one infusion may be sufficient. If needed, half of the loading dose may be given once or twice daily for 1 - 2 days. |
Moderate hemorrhage:
| Loading dose 25 IU FVIII:C/kg to achieve FVIII:C plasma level of approximately 50% of normal, followed by 15 IU FVIII:C/kg every 8-12 hours for first 1 – 2 days to maintain FVIII:C plasma level at 30% of normal, and then the same dose once or twice a day for a total of up to 7 days, or until adequate wound healing. |
Life-threatening hemorrhage:
| Initially 40 to 50 IU FVIII:C/kg, followed by 20 – 25 IU FVIII:C/kg every 8 hours to maintain FVIII:C plasma level at 80-100% of normal for 7 days, then continue the same dose once or twice a day for another 7 days in order to maintain the FVIII:C level at 30-50% of normal. |
In all cases, the dose should be adjusted individually by clinical judgment of the potential for compromise of a vital structure, and by frequent monitoring of factor VIII activity in the patient's plasma.
For use in pediatric hemophilia A patients, see PRECAUTIONS, Pediatric Use.
Therapy for von Willebrand Disease
The dosage should be adjusted according to the extent and location of bleeding. As a rule, 40-80 IU VWF:RCo (corresponding to 17 to 33 IU factor VIII in Humate-P®) per kg body weight are given every 8 to 12 hours. Repeat doses are administered for as long as needed based on repeat monitoring of appropriate clinical and laboratory measures. Expected levels of VWF:RCo are based on an expected in vivo recovery of 2.0 IU/dL rise per IU/kg VWF:RCo administered. The administration of 1 IU of Factor VIII per kg body weight can be expected to lead to a rise in circulating VWF:RCo of approximately 5 IU/dL.
Table 10 provides dosing guidelines for pediatric and adult patients.19
| Classification of VWD | Hemorrhage | Dosage (IU VWF:RCo/kg body weight) |
|---|---|---|
| Type 1 | ||
| Major (e.g. severe or refractory epistaxis, GI bleeding, CNS trauma, or traumatic hemorrhage) | Loading dose 40 to 60 IU/kg, then 40 to 50 IU/kg every 8 to 12 hours for 3 days to keep the trough level of VWF:RCo >50%; then 40 to 50 IU/kg daily for a total of up to 7 days of treatment. |
| Minor (e.g. epistaxis, oral bleeding, menorrhagia) | 40 to 50 IU/kg (1 or 2 doses) |
| Major (e.g. severe or refractory epistaxis, GI bleeding, CNS trauma, hemarthrosis or traumatic hemorrhage) | Loading dose 50 to 75 IU/kg, then 40 to 60 IU/kg every 8 to 12 hours for 3 days to keep the trough level of VWF:RCo >50%; then 40 to 60 IU/kg daily for a total of up to 7 days of treatment. Factor VIII:C levels should be monitored and maintained according to the guidelines for hemophilia A therapy, Table 9. | |
| Types 2 (all variants) and 3 | Minor (clinical indications above) | 40 to 50 IU/kg (1 or 2 doses) |
| Major (clinical indications above) | Loading dose of 60 to 80 IU/kg, then 40 to 60 IU/kg every 8 to 12 hours for 3 days to keep the trough level of VWF:RCo >50%; then 40 to 60 IU/kg daily for a total of up to 7 days of treatment. Factor VIII:C levels should be monitored and maintained according to the guidelines for hemophilia A therapy, Table 9. |
Prevention of Excessive Bleeding During and After Surgery in VWD
The following information provides guidelines for calculating loading and maintenance doses of Humate-P® for patients undergoing surgery. However in the case of emergency surgery, administer a loading dose of 50 to 60 IU/kg and, subsequently, closely monitor the patient's trough coagulation factor levels.
When possible, it is recommended that the incremental in vivo recovery (IVR) be measured and that baseline plasma VWF:RCo and FVIII:C be assessed in all patients prior to surgery. Measure IVR as follows:
- Measure baseline plasma VWF:RCo.
- Infuse 60 IU VWF:RCo/kg product intravenously at time 0.
- At time +30 minutes, measure plasma VWF:RCo.
IVR = (Plasma VWF:RCotime +30 min – Plasma VWF:RCobaseline) / 60 IU kg
Calculation of the loading dose requires four values: the target peak plasma VWF:RCo level, the baseline VWF:RCo level, body weight (BW) in kilograms, and IVR. When individual recovery values are not available, a standardized loading dose can be used based on an assumed VWF:RCo IVR of 2.0 IU/dL per IU/kg of VWF:RCo product administered.
Table 11 provides guidelines for calculating the loading dose for adult and pediatric patients.
| Type of Surgery | VWF:RCo Target Peak Plasma Level | FVIII:C Target Peak Plasma Level | Calculation of Loading Dose (to be administered 1 to 2 hours before surgery) |
|---|---|---|---|
|
|||
| Major | 100 IU/dL | 80-100 IU/dL | Δ* VWF:RCo × BW (kg) / IVR† = IU VWF:RCo required |
| If the incremental IVR is not available, assume an IVR of 2 IU/dL per IU/kg and calculate the loading dose as follows: | |||
| (100 – baseline plasma VWF:RCo) × BW (kg) / 2.0 | |||
| In the case of emergency surgery, administer a dose of 50-60 IU/kg. | |||
| Minor / oral‡ | 50-60 IU/dL | 40-50 IU/dL | Δ* VWF:RCo × BW (kg) / IVR† = IU VWF:RCo required |
For example, the loading dose of Humate-P® required assuming a target VWF:RCo level of 100 IU/dL, baseline VWF:RCo level of 20 IU/dL, an IVR of 2.0 (IU/dL)/(IU/kg), Δ of 80 IU/dL, and a body weight of 70 kg would be calculated as follows:
| 80 IU/dL × 70 kg | = 2,800 IU VWF:RCo required |
| 2 (IU/dL)/(IU/kg) |
Attaining a target peak FVIII:C plasma level of 80 to 100 IU FVIII:C/dL for major surgery and 40 to 50 IU FVIII:C/dL for minor surgery or oral surgery might require additional dosing with Humate-P®. Because the ratio of VWF:RCo to FVIII:C activity in Humate-P® is 2.4 to 1, any additional dosing will increase VWF:RCo proportionally more than FVIII:C. Assuming an incremental IVR of 2.0 IU VWF:RCo/dL per IU/kg infused, additional dosing to increase FVIII:C in plasma will also increase plasma VWF:RCo by approximately 5 IU/dL for each IU/kg of FVIII administered.
The initial maintenance dose for the prevention of excessive bleeding during and after surgery should be half the loading dose, irrespective of additional dosing required to meet FVIII:C targets. Table 12 provides recommendations for target trough plasma levels (based on type of surgery and number of days following surgery) and minimum duration of treatment for subsequent maintenance doses. These recommendations apply to both adult and pediatric patients.
| Type of Surgery | VWF:RCo Target Trough Plasma Levels* | FVIII:C Target Trough Plasma Levels* | Minimum Duration of Treatment | ||
|---|---|---|---|---|---|
| Up to 3 days following surgery | After Day 3 | Up to 3 days following surgery | After Day 3 | ||
|
|||||
| Major | >50 IU/dL | >30 IU/dL | >50 IU/dL | >30 IU/dL | 72 hours |
| Minor | ≥30 IU/dL | – | – | >30 IU/dL | 48 hours |
| Oral† | ≥30 IU/dL | – | – | >30 IU/dL | 8-12 hours‡ |
Based on individual pharmacokinetic-derived half-lives, the frequency of maintenance doses is generally every 8 or 12 hours; patients with shorter half-lives may require dosing every 6 hours. In the absence of pharmacokinetic data, it is recommended that Humate-P® be administered initially every 8 hours with further adjustments determined by monitoring trough coagulation factor levels. When hemostatic levels are judged insufficient or trough levels are outside the recommended range, consider modifying the administration interval and/or the dose.
It is advisable to monitor trough VWF:RCo and FVIII:C levels at least once daily in order to adjust Humate-P® dosing as needed to avoid excessive accumulation of coagulation factors. The duration of treatment generally depends on the type of surgery performed, but must be assessed for individual patients based on their hemostatic response (see CLINICAL STUDIES).
For use in pediatric VWD patients, see PRECAUTIONS, Pediatric Use.
Reconstitution
Plastic disposable syringes are recommended for withdrawal and administration of Humate-P® solution. Protein solutions of this type tend to adhere to the ground glass surface of all-glass syringes.
- Before infusion, ensure that Humate-P® and diluent are at room temperature.
- Remove caps from both vials to expose central portions of the rubber stoppers.
- Treat surface of rubber stoppers with the alcohol swab provided and allow to dry prior to opening the Mix2Vial™ package.
- Open the Mix2Vial™ package by peeling away the lid (Fig. 1). To maintain sterility, leave the Mix2Vial™ in the clear outer packaging. Place the diluent vial on an even surface and hold the vial tight. Grip the Mix2Vial™ together with the clear packaging and firmly snap the blue end onto the diluent stopper (Fig. 2).
- While holding onto the diluent vial, carefully remove the clear outer packaging from the Mix2Vial™ set. Make sure that you only pull up the clear outer packaging and not the Mix2Vial™ set (Fig. 3).
- With the product vial firmly on a surface, invert the diluent vial with set attached and firmly snap the transparent adapter onto the product vial stopper (Fig. 4). The diluent will automatically transfer into the product vial.
- With the diluent and product vial still attached, gently swirl the product vial to ensure the product is fully dissolved (Fig. 5). Do not shake vial.
- With one hand grasp the product-side of the Mix2Vial™ set and with the other hand grasp the blue diluent-side of the Mix2Vial™ set and unscrew the set into two pieces (Fig. 6).
- Draw air into an empty, sterile syringe. While the product vial is upright, screw the syringe to the Mix2Vial™ set. Inject air into the product vial. While keeping the syringe plunger pressed, invert the system upside down and draw the concentrate into the syringe by pulling the plunger back slowly (Fig. 7).
- Now that the concentrate has been transferred into the syringe, firmly grasp the barrel of the syringe (keeping the syringe plunger facing down) and unscrew the syringe from the Mix2Vial™ (Fig. 8). Attach the syringe to a venipuncture set.
- If the same patient is to receive concentrate from more than one vial, the contents of two vials may be drawn into the same syringe through a separate unused Mix2Vial™ set before attaching the vein needle.
- Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit. When the reconstitution procedure is precisely followed, it is not uncommon for a few small flakes or particles to remain. The Mix2Vial™ set provided with Humate-P® should remove those particles and this should not influence dosage calculations.
 |  |  |  |
| Fig. 1 | Fig. 2 | Fig. 3 | Fig. 4 |
 |  |  |  |
| Fig. 5 | Fig. 6 | Fig. 7 | Fig. 8 |
Do not refrigerate after reconstitution. To assure product sterility, Humate-P® should be administered within three hours after reconstitution.
Administration
Intravenous Injection
Slowly inject the solution (maximally 4 mL/minute) intravenously with a venipuncture set or with another suitable injection set.
Discard the administration equipment and any unused Humate-P® after use.
HOW SUPPLIED
Antihemophilic Factor/von Willebrand Factor Complex (Human), Dried, Pasteurized, Humate-P®, is supplied in a single dose vial with a vial of diluent (Sterile Diluent for Humate-P®), Mix2Vial™ filter transfer set and alcohol swabs. International unit activity of Factor VIII and VWF:RCo is stated on the carton and label of each vial and supplied as listed below. Note: Use either the Mix2Vial™ transfer set provided or a commercially available double ended needle and vented filter spike.
| FVIII/vial | Dosage | VWF:RCo/vial | Diluent | |
|---|---|---|---|---|
| NDC 0053-7615-05 | 250 IU | LOW | 600 IU | 5 mL |
| NDC 0053-7615-10 | 500 IU | MID | 1200 IU | 10 mL |
| NDC 0053-7615-20 | 1000 IU | HIGH | 2400 IU | 15 mL |
STORAGE
When stored up to 25°C (up to 77°F), Humate-P® is stable up to the expiration date printed on its label. Avoid freezing.
REFERENCES
- Berntorp E, Nilsson IM. Biochemical and in vivo properties of commercial virus-inactivated factor VIII concentrates. Eur J Haematol. 40:205-214, 1988.
- Berntorp E, and Nilsson IM. Use of a high-purity Factor VIII Concentrate (Humate-P) in von Willebrand disease. Vox Sang 56:212-217, 1989.
- Mannucci PM, Tenconi PM, Castaman G, Rodeghiero F. Comparison of four virus-inactivated plasma concentrates for treatment of severe von Willebrand disease: A cross-over randomized trial. Blood 79:3130-3137, 1992.
- Berntorp E. Plasma product treatment in various types of von Willebrand's disease. Haemostasis 24:289-297, 1994.
- Scharrer I, Vigh T, Aygörn-Pürsün E. Experience with Haemate-P in von Willebrand's disease in adults. Haemostasis 24:298-303, 1994.
- Sadler JE. For the Subcommittee on von Willebrand Factor of the Scientific and Standardization Committee of the International Society on Thrombosis and Haemostasis. Thrombosis and Hemostasis 71(4):520-525, 1994.
- Fukui H, Nishino M, Terada S, et al. Hemostatic effect of 2 heat-treated factor VIII concentrate (Haemate-P) in von Willebrand disease. Blut 56:171-178, 1988.
- Rose E, Forster A and Aledort LM. Correction of prolonged bleeding time in von Willebrand's disease with Humate-P®. Transfusion 30(4):381, 1990.
- Kreuz W, Mentzer D, Becker S, Scharrer I, Kornhuber B. Haemate P in children with von Willebrand's disease. Haemostasis 24:304-310, 1994.
- Hoyer LW. The Factor VIII complex: Structure and function. Blood 58:1-13, 1981.
- Meyer D, and Girma J-P. von Willebrand factor: Structure and function. Thromb Haemostas. 70:99-104, 1993.
- Heimburger N, Karges HE, Mauler R, Nováková-Banet A, Hilfenhaus J, Wiedmann E. Factor VIII concentrate: Hepatitis-safe preparation, virus inactivation and clinical experience. Proc. 4th Int. Symp. Hemophilia Treatment, Tokyo 1984, pp. 107-115.
- Schimpf K, et al. Absence of hepatitis after treatment with a pasteurized Factor VIII concentrate in patients with hemophilia and no previous transfusions. New Engl J Med 316:918-922, 1987.
- Schimpf K, et al. Absence of anti-human immunodeficiency virus types 1 and 2 seroconversion after treatment of hemophilia or von Willebrand disease with pasteurized Factor VIII concentrates. New Engl J Med 321:1148-1152, 1989.
- Mannucci, PM. Venous Thromboembolism in Von Willebrand Disease. Thrombosis and Haemostasis 88:378-379, 2002.
- Markis M, et al. Venous Thrombosis Following the Use of Intermediate Purity FVIII Concentrate to Treat Patients with von Willebrand's Disease. Thrombosis and Haemostasis 88:387-388, 2002.
- Data on File.
- Levine PH, Brettler DB. Clinical aspects and therapy for hemophilia A. In: Hoffman R, Benz JB, Shattil SJ, Furie B, Cohen HJ, eds. Hematology - Basic Principles and Practice, Churchill Livingstone Inc.; 1991, pp.1296-1297.
- Scott JP, Montgomery RT. Therapy of von Willebrand disease. Seminars in Thrombosis and Hemostasis 19(1):37-47, 1993.
Revised: October 2007
OBKF G46 01327 (19572A)
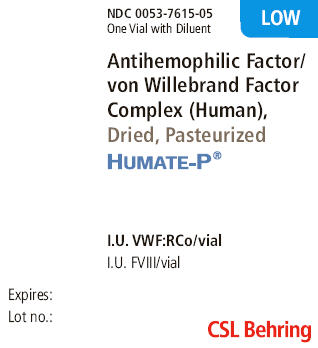
Package Label - Principal Display Panel - LOW
NDC 0053-7615-05
One Vial with Diluent
Antihemophilic Factor/
von Willebrand Factor
Complex (Human),
Dried, Pasteurized
HUMATE-P®
I.U. VWF:RCo/vial
I.U. FVIII/vial
Expires:
Lot no.:
CSL Behring
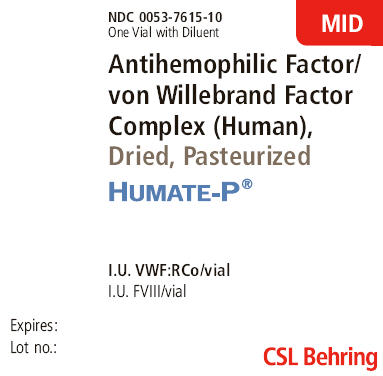
Package Label - Principal Display Panel - MID
NDC 0053-7615-10
One Vial with Diluent
Antihemophilic Factor/
von Willebrand Factor
Complex (Human),
Dried, Pasteurized
HUMATE-P®
I.U. VWF:RCo/vial
I.U. FVIII/vial
Expires:
Lot no.:
CSL Behring
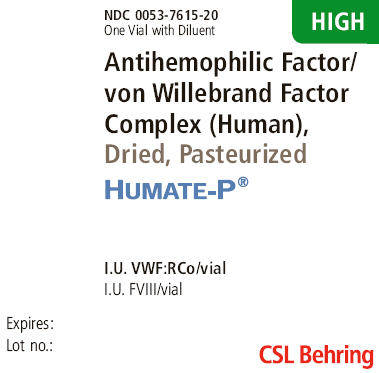
Package Label - Principal Display Panel - HIGH
NDC 0053-7615-20
One Vial with Diluent
Antihemophilic Factor/
von Willebrand Factor
Complex (Human),
Dried, Pasteurized
HUMATE-P®
I.U. VWF:RCo/vial
I.U. FVIII/vial
Expires:
Lot no.:
CSL Behring
| HUMATE-P
human coagulation factor viii/von willebrand factor complex kit |
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
| Marketing Information | |||
| Marketing Category | Application Number or Monograph Citation | Marketing Start Date | Marketing End Date |
| BLA | BLA103960 | 05/01/1986 | |
| HUMATE-P
human coagulation factor viii/von willebrand factor complex kit |
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
| Marketing Information | |||
| Marketing Category | Application Number or Monograph Citation | Marketing Start Date | Marketing End Date |
| BLA | BLA103960 | 05/01/1986 | |
| HUMATE-P
human coagulation factor viii/von willebrand factor complex kit |
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
| Marketing Information | |||
| Marketing Category | Application Number or Monograph Citation | Marketing Start Date | Marketing End Date |
| BLA | BLA103960 | 05/01/1986 | |
| Labeler - CSL BEHRING LLC (931896963) |
| Establishment | |||
| Name | Address | ID/FEI | Operations |
| CSL Behring GmbH | 306530474 | MANUFACTURE | |