NASONEX
-
mometasone furoate spray, metered
Schering Corporation
- 1
- calculated on the anhydrous basis
----------
NASONEX®
(mometasone furoate monohydrate)
Nasal Spray, 50 mcg1
FOR INTRANASAL USE ONLY
1
PRODUCT INFORMATION
DESCRIPTION
Mometasone furoate monohydrate, the active component of NASONEX Nasal Spray, 50 mcg, is an anti-inflammatory corticosteroid having the chemical name, 9,21-Dichloro-11β,17-dihydroxy-16α-methylpregna-1,4-diene-3,20-dione 17-(2 furoate) monohydrate, and the following chemical structure:
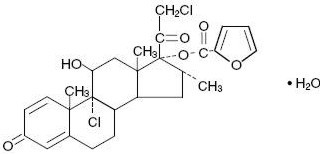
Mometasone furoate monohydrate is a white powder, with an empirical formula of C27H30Cl2O6•H2O, and a molecular weight of 539.45. It is practically insoluble in water; slightly soluble in methanol, ethanol, and isopropanol; soluble in acetone and chloroform; and freely soluble in tetrahydrofuran. Its partition coefficient between octanol and water is greater than 5000.
NASONEX Nasal Spray, 50 mcg is a metered-dose, manual pump spray unit containing an aqueous suspension of mometasone furoate monohydrate equivalent to 0.05% w/w mometasone furoate calculated on the anhydrous basis; in an aqueous medium containing glycerin, microcrystalline cellulose and carboxymethylcellulose sodium, sodium citrate, citric acid, benzalkonium chloride, and polysorbate 80. The pH is between 4.3 and 4.9.
After initial priming (10 actuations), each actuation of the pump delivers a metered spray containing 100 mg of suspension containing mometasone furoate monohydrate equivalent to 50 mcg of mometasone furoate calculated on the anhydrous basis. Each bottle of NASONEX Nasal Spray, 50 mcg provides 120 sprays.
CLINICAL PHARMACOLOGY
NASONEX Nasal Spray, 50 mcg is a corticosteroid demonstrating anti-inflammatory properties. The precise mechanism of corticosteroid action on allergic rhinitis is not known. Corticosteroids have been shown to have a wide range of effects on multiple cell types (eg, mast cells, eosinophils, neutrophils, macrophages, and lymphocytes) and mediators (eg, histamine, eicosanoids, leukotrienes, and cytokines) involved in inflammation.
In two clinical studies utilizing nasal antigen challenge, NASONEX Nasal Spray, 50 mcg decreased some markers of the early- and late-phase allergic response. These observations included decreases (vs placebo) in histamine and eosinophil cationic protein levels, and reductions (vs baseline) in eosinophils, neutrophils, and epithelial cell adhesion proteins. The clinical significance of these findings is not known.
The effect of NASONEX Nasal Spray, 50 mcg on nasal mucosa following 12 months of treatment was examined in 46 patients with allergic rhinitis. There was no evidence of atrophy and there was a marked reduction in intraepithelial eosinophilia and inflammatory cell infiltration (eg, eosinophils, lymphocytes, monocytes, neutrophils, and plasma cells).
Pharmacokinetics
Absorption
Mometasone furoate monohydrate administered as a nasal spray is virtually undetectable in plasma from adult and pediatric subjects despite the use of a sensitive assay with a lower quantitation limit (LOQ) of 50 pcg/mL.
Distribution
The in vitro protein binding for mometasone furoate was reported to be 98% to 99% in concentration range of 5 to 500 ng/mL.
Metabolism
Studies have shown that any portion of a mometasone furoate dose which is swallowed and absorbed undergoes extensive metabolism to multiple metabolites. There are no major metabolites detectable in plasma. Upon in vitro incubation, one of the minor metabolites formed is 6β-hydroxy-mometasone furoate. In human liver microsomes, the formation of the metabolite is regulated by cytochrome P-450 3A4 (CYP3A4).
Elimination
Following intravenous administration, the effective plasma elimination half-life of mometasone furoate is 5.8 hours. Any absorbed drug is excreted as metabolites mostly via the bile, and to a limited extent, into the urine.
Special Populations
The effects of renal impairment, hepatic impairment, age, or gender on mometasone furoate pharmacokinetics have not been adequately investigated.
Pharmacodynamics
Four clinical pharmacology studies have been conducted in humans to assess the effect of NASONEX Nasal Spray, 50 mcg at various doses on adrenal function. In one study, daily doses of 200 and 400 mcg of NASONEX Nasal Spray, 50 mcg and 10 mg of prednisone were compared to placebo in 64 patients with allergic rhinitis. Adrenal function before and after 36 consecutive days of treatment was assessed by measuring plasma cortisol levels following a 6-hour Cortrosyn (ACTH) infusion and by measuring 24-hour urinary-free cortisol levels. NASONEX Nasal Spray, 50 mcg, at both the 200- and 400-mcg dose, was not associated with a statistically significant decrease in mean plasma cortisol levels post-Cortrosyn infusion or a statistically significant decrease in the 24-hour urinary-free cortisol levels compared to placebo. A statistically significant decrease in the mean plasma cortisol levels post-Cortrosyn infusion and 24-hour urinary-free cortisol levels was detected in the prednisone treatment group compared to placebo.
A second study assessed adrenal response to NASONEX Nasal Spray, 50 mcg (400 and 1600 mcg/day), prednisone (10 mg/day), and placebo, administered for 29 days in 48 male volunteers. The 24-hour plasma cortisol area under the curve (AUC0–24), during and after an 8-hour Cortrosyn infusion and 24-hour urinary-free cortisol levels were determined at baseline and after 29 days of treatment. No statistically significant differences of adrenal function were observed with NASONEX Nasal Spray, 50 mcg compared to placebo.
A third study evaluated single, rising doses of NASONEX Nasal Spray, 50 mcg (1000, 2000, and 4000 mcg/day), orally administered mometasone furoate (2000, 4000, and 8000 mcg/day), orally administered dexamethasone (200, 400, and 800 mcg/day), and placebo (administered at the end of each series of doses) in 24 male volunteers. Dose administrations were separated by at least 72 hours. Determination of serial plasma cortisol levels at 8 AM and for the 24-hour period following each treatment were used to calculate the plasma cortisol area under the curve (AUC0–24). In addition, 24-hour urinary-free cortisol levels were collected prior to initial treatment administration and during the period immediately following each dose. No statistically significant decreases in the plasma cortisol AUC, 8 AM cortisol levels, or 24-hour urinary-free cortisol levels were observed in volunteers treated with either NASONEX Nasal Spray, 50 mcg or oral mometasone, as compared with placebo treatment. Conversely, nearly all volunteers treated with the three doses of dexamethasone demonstrated abnormal 8 AM cortisol levels (defined as a cortisol level <10 mcg/dL), reduced 24-hour plasma AUC values, and decreased 24-hour urinary-free cortisol levels, as compared to placebo treatment.
In a fourth study, adrenal function was assessed in 213 patients with nasal polyps before and after 4 months of treatment with either NASONEX Nasal Spray, 50 mcg, (200 mcg once or twice daily) or placebo by measuring 24-hour urinary-free cortisol levels. NASONEX Nasal Spray, 50 mcg, at both doses (200 and 400 mcg/day), was not associated with statistically significant decreases in the 24-hour urinary-free cortisol levels compared to placebo.
Three clinical pharmacology studies have been conducted in pediatric patients to assess the effect of mometasone furoate nasal spray on the adrenal function at daily doses of 50, 100, and 200 mcg vs placebo. In one study, adrenal function before and after 7 consecutive days of treatment was assessed in 48 pediatric patients with allergic rhinitis (ages 6 to 11 years) by measuring morning plasma cortisol and 24-hour urinary-free cortisol levels. Mometasone furoate nasal spray, at all three doses, was not associated with a statistically significant decrease in mean plasma cortisol levels or a statistically significant decrease in the 24-hour urinary-free cortisol levels compared to placebo. In the second study, adrenal function before and after 14 consecutive days of treatment was assessed in 48 pediatric patients (ages 3 to 5 years) with allergic rhinitis by measuring plasma cortisol levels following a 30-minute Cortrosyn infusion. Mometasone furoate nasal spray, 50 mcg, at all three doses (50, 100, and 200 mcg/day), was not associated with a statistically significant decrease in mean plasma cortisol levels post-Cortrosyn infusion compared to placebo. All patients had a normal response to Cortrosyn. In the third study, adrenal function before and after up to 42 consecutive days of once-daily treatment was assessed in 52 patients with allergic rhinitis (ages 2 to 5 years), 28 of whom received mometasone furoate nasal spray, 50 mcg per nostril (total daily dose 100 mcg), by measuring morning plasma cortisol and 24-hour urinary-free cortisol levels. Mometasone furoate nasal spray was not associated with a statistically significant decrease in mean plasma cortisol levels or a statistically significant decrease in the 24-hour urinary-free cortisol levels compared to placebo.
Clinical Studies
Allergic Rhinitis
The efficacy and safety of NASONEX Nasal Spray, 50 mcg in the prophylaxis and treatment of seasonal allergic rhinitis and the treatment of perennial allergic rhinitis have been evaluated in 18 controlled trials, and one uncontrolled clinical trial, in approximately 3000 adults (ages 17 to 85 years) and adolescents (ages 12 to 16 years). This included 1757 males and 1453 females, including a total of 283 adolescents (182 boys and 101 girls) with seasonal allergic or perennial allergic rhinitis, treated with NASONEX Nasal Spray, 50 mcg at doses ranging from 50 to 800 mcg/day. The majority of patients were treated with 200 mcg/day. These trials evaluated the total nasal symptom scores that included stuffiness, rhinorrhea, itching, and sneezing. Patients treated with NASONEX Nasal Spray, 50 mcg, 200 mcg/day had a significant decrease in total nasal symptom scores compared to placebo-treated patients. No additional benefit was observed for mometasone furoate doses greater than 200 mcg/day. A total of 350 patients have been treated with NASONEX Nasal Spray, 50 mcg for 1 year or longer.
The efficacy and safety of NASONEX Nasal Spray, 50 mcg in the treatment of seasonal allergic and perennial allergic rhinitis in pediatric patients (ages 3 to 11 years) have been evaluated in four controlled trials. This included approximately 990 pediatric patients ages 3 to 11 years (606 males and 384 females) with seasonal allergic or perennial allergic rhinitis treated with mometasone furoate nasal spray at doses ranging from 25 to 200 mcg/day. Pediatric patients treated with NASONEX Nasal Spray, 50 mcg (100 mcg total daily dose, 374 patients) had a significant decrease in total nasal symptom (congestion, rhinorrhea, itching, and sneezing) scores, compared to placebo-treated patients. No additional benefit was observed for the 200-mcg mometasone furoate total daily dose in pediatric patients (ages 3 to 11 years). A total of 163 pediatric patients have been treated for 1 year.
In patients with seasonal allergic rhinitis, NASONEX Nasal Spray, 50 mcg, demonstrated improvement in nasal symptoms (vs placebo) within 11 hours after the first dose based on one single-dose, parallel-group study of patients in an outdoor "park" setting (park study) and one environmental exposure unit (EEU) study, and within 2 days in two randomized, double-blind, placebo-controlled, parallel-group seasonal allergic rhinitis studies. Maximum benefit is usually achieved within 1 to 2 weeks after initiation of dosing.
Prophylaxis of seasonal allergic rhinitis for patients 12 years of age and older with NASONEX Nasal Spray, 50 mcg, given at a dose of 200 mcg/day, was evaluated in two clinical studies in 284 patients. These studies were designed such that patients received 4 weeks of prophylaxis with NASONEX Nasal Spray, 50 mcg prior to the anticipated onset of the pollen season; however, some patients received only 2 to 3 weeks of prophylaxis. Patients receiving 2 to 4 weeks of prophylaxis with NASONEX Nasal Spray, 50 mcg demonstrated a statistically significantly smaller mean increase in total nasal symptom scores with onset of the pollen season as compared to placebo patients.
Nasal Polyps
Two studies were performed to evaluate the efficacy and safety of NASONEX Nasal Spray in the treatment of nasal polyps. These studies involved 664 patients with nasal polyps, 441 of whom received NASONEX Nasal Spray. These studies were randomized, double-blind, placebo-controlled, parallel group, multicenter studies in patients 18 to 86 years of age with bilateral nasal polyps. Patients were randomized to receive NASONEX Nasal Spray 200 mcg once daily, 200 mcg twice daily or placebo for a period of 4 months. The co-primary efficacy endpoints were 1) change from baseline in nasal congestion/obstruction averaged over the first month of treatment; and 2) change from baseline to last assessment in bilateral polyp grade during the entire 4 months of treatment as assessed by endoscopy. Efficacy was demonstrated in both studies at a dose of 200 mcg twice daily and in one study at a dose of 200 mcg once a day (see table below).
| NASONEX 200 mcg qd | NASONEX 200 mcg bid | Placebo | P value for NASONEX 200 mcg qd vs placebo | P value for NASONEX 200 mcg bid vs placebo |
|
|---|---|---|---|---|---|
|
|||||
| Study 1 | N = 115 | N = 122 | N = 117 | ||
| Baseline bilateral polyp grade* | 4.21 | 4.27 | 4.25 | ||
| Mean change from baseline in bilateral polyp grade | -1.15 | -0.96 | -0.50 | <0.001 | 0.01 |
| Baseline nasal congestion† | 2.29 | 2.35 | 2.28 | ||
| Mean change from baseline in nasal congestion | -0.47 | -0.61 | -0.24 | 0.001 | <0.001 |
| Study 2 | N = 102 | N = 102 | N = 106 | ||
| Baseline bilateral polyp grade* | 4.00 | 4.10 | 4.17 | ||
| Mean change from baseline in bilateral polyp grade | -0.78 | -0.96 | -0.62 | 0.33 | 0.04 |
| Baseline nasal congestion† | 2.23 | 2.20 | 2.18 | ||
| Mean change from baseline in nasal congestion | -0.42 | -0.66 | -0.23 | 0.01 | <0.001 |
There were no clinically relevant differences in the effectiveness of NASONEX Nasal Spray, 50 mcg, in the studies evaluating treatment of nasal polyps across subgroups of patients defined by gender, age, or race.
INDICATIONS AND USAGE
NASONEX Nasal Spray, 50 mcg is indicated for the treatment of the nasal symptoms of seasonal allergic and perennial allergic rhinitis, in adults and pediatric patients 2 years of age and older. NASONEX Nasal Spray, 50 mcg is indicated for the prophylaxis of the nasal symptoms of seasonal allergic rhinitis in adult and adolescent patients 12 years and older. In patients with a known seasonal allergen that precipitates nasal symptoms of seasonal allergic rhinitis, initiation of prophylaxis with NASONEX Nasal Spray, 50 mcg is recommended 2 to 4 weeks prior to the anticipated start of the pollen season. Safety and effectiveness of NASONEX Nasal Spray, 50 mcg in pediatric patients less than 2 years of age have not been established.
NASONEX Nasal Spray, 50 mcg, is indicated for the treatment of nasal polyps in patients 18 years of age and older. Safety and effectiveness of NASONEX Nasal Spray, 50 mcg, for the treatment of nasal polyps in pediatric patients less than 18 years of age have not been established.
CONTRAINDICATIONS
Hypersensitivity to any of the ingredients of this preparation contraindicates its use.
WARNINGS
The replacement of a systemic corticosteroid with a topical corticosteroid can be accompanied by signs of adrenal insufficiency and, in addition, some patients may experience symptoms of withdrawal; ie, joint and/or muscular pain, lassitude, and depression. Careful attention must be given when patients previously treated for prolonged periods with systemic corticosteroids are transferred to topical corticosteroids, with careful monitoring for acute adrenal insufficiency in response to stress. This is particularly important in those patients who have associated asthma or other clinical conditions where too rapid a decrease in systemic corticosteroid dosing may cause a severe exacerbation of their symptoms.
If recommended doses of intranasal corticosteroids are exceeded or if individuals are particularly sensitive or predisposed by virtue of recent systemic steroid therapy, symptoms of hypercorticism may occur, including very rare cases of menstrual irregularities, acneiform lesions, and cushingoid features. If such changes occur, topical corticosteroids should be discontinued slowly, consistent with accepted procedures for discontinuing oral steroid therapy.
Persons who are on drugs which suppress the immune system are more susceptible to infections than healthy individuals. Chickenpox and measles, for example, can have a more serious or even fatal course in nonimmune children or adults on corticosteroids. In such children or adults who have not had these diseases, particular care should be taken to avoid exposure. How the dose, route, and duration of corticosteroid administration affects the risk of developing a disseminated infection is not known. The contribution of the underlying disease and/or prior corticosteroid treatment to the risk is also not known. If exposed to chickenpox, prophylaxis with varicella zoster immune globin (VZIG) may be indicated. If exposed to measles, prophylaxis with pooled intramuscular immunoglobulin (IG) may be indicated. (See the respective package inserts for complete VZIG and IG prescribing information.) If chickenpox develops, treatment with antiviral agents may be considered.
PRECAUTIONS
General
Intranasal corticosteroids may cause a reduction in growth velocity when administered to pediatric patients (see PRECAUTIONS, Pediatric Use section). In clinical studies with NASONEX Nasal Spray, 50 mcg, the development of localized infections of the nose and pharynx with Candida albicans has occurred only rarely. When such an infection develops, use of NASONEX Nasal Spray, 50 mcg should be discontinued and appropriate local or systemic therapy instituted, if needed.
Nasal corticosteroids should be used with caution, if at all, in patients with active or quiescent tuberculous infection of the respiratory tract, or in untreated fungal, bacterial, systemic viral infections, or ocular herpes simplex.
Rarely, immediate hypersensitivity reactions may occur after the intranasal administration of mometasone furoate monohydrate. Extremely rare instances of wheezing have been reported.
Rare instances of nasal septum perforation and increased intraocular pressure have also been reported following the intranasal application of aerosolized corticosteroids. As with any long-term topical treatment of the nasal cavity, patients using NASONEX Nasal Spray, 50 mcg over several months or longer should be examined periodically for possible changes in the nasal mucosa.
Because of the inhibitory effect of corticosteroids on wound healing, patients who have experienced recent nasal septum ulcers, nasal surgery, or nasal trauma should not use a nasal corticosteroid until healing has occurred.
Glaucoma and cataract formation was evaluated in one controlled study of 12 weeks' duration and one uncontrolled study of 12 months' duration in patients treated with NASONEX Nasal Spray, 50 mcg at 200 mcg/day, using intraocular pressure measurements and slit lamp examination. No significant change from baseline was noted in the mean intraocular pressure measurements for the 141 NASONEX-treated patients in the 12-week study, as compared with 141 placebo-treated patients. No individual NASONEX-treated patient was noted to have developed a significant elevation in intraocular pressure or cataracts in this 12-week study. Likewise, no significant change from baseline was noted in the mean intraocular pressure measurements for the 139 NASONEX-treated patients in the 12-month study and again, no cataracts were detected in these patients. Nonetheless, nasal and inhaled corticosteroids have been associated with the development of glaucoma and/or cataracts. Therefore, close follow-up is warranted in patients with a change in vision and with a history of glaucoma and/or cataracts.
When nasal corticosteroids are used at excessive doses, systemic corticosteroid effects such as hypercorticism and adrenal suppression may appear. If such changes occur, NASONEX Nasal Spray, 50 mcg should be discontinued slowly, consistent with accepted procedures for discontinuing oral steroid therapy.
Information for Patients
Patients being treated with NASONEX Nasal Spray, 50 mcg should be given the following information and instructions. This information is intended to aid in the safe and effective use of this medication. It is not a disclosure of all intended or possible adverse effects. Patients should use NASONEX Nasal Spray, 50 mcg at regular intervals (see DOSAGE AND ADMINISTRATION) since its effectiveness depends on regular use. Improvement in nasal symptoms of allergic rhinitis has been shown to occur within 11 hours after the first dose based on one single-dose, parallel-group study of patients in an outdoor "park" setting (park study) and one environmental exposure unit (EEU) study and within 2 days after the first dose in two randomized, double-blind, placebo-controlled, parallel-group seasonal allergic rhinitis studies. Maximum benefit is usually achieved within 1 to 2 weeks after initiation of dosing. Patients should take the medication as directed and should not increase the prescribed dosage in an attempt to increase its effectiveness. Patients should contact their physician if symptoms do not improve, or if the condition worsens. To assure proper use of this nasal spray, and to attain maximum benefit, patients should read and follow the accompanying Patient's Instructions for Use carefully. Administration to young children should be aided by an adult.
Patients should be cautioned not to spray NASONEX Nasal Spray, 50 mcg into the eyes or directly onto the nasal septum.
Persons who are on immunosuppressant doses of corticosteroids should be warned to avoid exposure to chickenpox or measles, and patients should also be advised that if they are exposed, medical advice should be sought without delay.
Carcinogenesis, Mutagenesis, Impairment of Fertility
In a 2-year carcinogenicity study in Sprague Dawley rats, mometasone furoate demonstrated no statistically significant increase in the incidence of tumors at inhalation doses up to 67 mcg/kg (approximately 1 and 2 times the maximum recommended daily intranasal dose [MRDID] in adults [400 mcg] and children [100 mcg], respectively, on a mcg/m2 basis). In a 19-month carcinogenicity study in Swiss CD-1 mice, mometasone furoate demonstrated no statistically significant increase in the incidence of tumors at inhalation doses up to 160 mcg/kg (approximately 2 times the MRDID in adults and children, respectively, on a mcg/m2 basis).
Mometasone furoate increased chromosomal aberrations in an in vitro Chinese hamster ovary-cell assay, but did not increase chromosomal aberrations in an in vitro Chinese hamster lung cell assay. Mometasone furoate was not mutagenic in the Ames test or mouse-lymphoma assay, and was not clastogenic in an in vivo mouse micronucleus assay and a rat bone marrow chromosomal aberration assay or a mouse male germ-cell chromosomal aberration assay. Mometasone furoate also did not induce unscheduled DNA synthesis in vivo in rat hepatocytes.
In reproductive studies in rats, impairment of fertility was not produced by subcutaneous doses up to 15 mcg/kg (less than the MRDID in adults on a mcg/m2 basis).
Pregnancy
Teratogenic Effects
Pregnancy Category C
When administered to pregnant mice, rats, and rabbits, mometasone furoate increased fetal malformations. The doses that produced malformations also decreased fetal growth, as measured by lower fetal weights and/or delayed ossification. Mometasone furoate also caused dystocia and related complications when administered to rats during the end of pregnancy.
In mice, mometasone furoate caused cleft palate at subcutaneous doses of 60 mcg/kg and above (less than the MRDID in adults on a mcg/m2 basis). Fetal survival was reduced at 180 mcg/kg (approximately 2 times the MRDID in adults on a mcg/m2 basis). No toxicity was observed at 20 mcg/kg (less than the MRDID in adults on a mcg/m2 basis).
In rats, mometasone furoate produced umbilical hernia at topical dermal doses of 600 mcg/kg and above (approximately 10 times the MRDID in adults on a mcg/m2 basis). A dose of 300 mcg/kg (approximately 6 times the MRDID in adults on a mcg/m2 basis) produced delays in ossification, but no malformations.
In rabbits, mometasone furoate caused multiple malformations (eg, flexed front paws, gallbladder agenesis, umbilical hernia, hydrocephaly) at topical dermal doses of 150 mcg/kg and above (approximately 6 times the MRDID in adults on a mcg/m2 basis). In an oral study, mometasone furoate increased resorptions and caused cleft palate and/or head malformations (hydrocephaly or domed head) at 700 mcg/kg (approximately 30 times the MRDID in adults on a mcg/m2 basis). At 2800 mcg/kg (approximately 110 times the MRDID in adults on a mcg/m2 basis), most litters were aborted or resorbed. No toxicity was observed at 140 mcg/kg (approximately 6 times the MRDID in adults on a mcg/m2 basis).
When rats received subcutaneous doses of mometasone furoate throughout pregnancy or during the later stages of pregnancy, 15 mcg/kg (less than the MRDID in adults on a mcg/m2 basis) caused prolonged and difficult labor and reduced the number of live births, birth weight, and early pup survival. Similar effects were not observed at 7.5 mcg/kg (less than the MRDID in adults on a mcg/m2 basis).
There are no adequate and well-controlled studies in pregnant women. NASONEX Nasal Spray, 50 mcg, like other corticosteroids, should be used during pregnancy only if the potential benefits justify the potential risk to the fetus. Experience with oral corticosteroids since their introduction in pharmacologic, as opposed to physiologic, doses suggests that rodents are more prone to teratogenic effects from corticosteroids than humans. In addition, because there is a natural increase in corticosteroid production during pregnancy, most women will require a lower exogenous corticosteroid dose and many will not need corticosteroid treatment during pregnancy.
Nonteratogenic Effects
Hypoadrenalism may occur in infants born to women receiving corticosteroids during pregnancy. Such infants should be carefully monitored.
Nursing Mothers
It is not known if mometasone furoate is excreted in human milk. Because other corticosteroids are excreted in human milk, caution should be used when NASONEX Nasal Spray, 50 mcg is administered to nursing women.
Pediatric Use
Controlled clinical studies have shown intranasal corticosteroids may cause a reduction in growth velocity in pediatric patients. This effect has been observed in the absence of laboratory evidence of hypothalamic-pituitary-adrenal (HPA) axis suppression, suggesting that growth velocity is a more sensitive indicator of systemic corticosteroid exposure in pediatric patients than some commonly used tests of HPA axis function. The long-term effects of this reduction in growth velocity associated with intranasal corticosteroids, including the impact on final adult height, are unknown. The potential for "catch up" growth following discontinuation of treatment with intranasal corticosteroids has not been adequately studied. The growth of pediatric patients receiving intranasal corticosteroids, including NASONEX Nasal Spray, 50 mcg, should be monitored routinely (eg, via stadiometry). The potential growth effects of prolonged treatment should be weighed against clinical benefits obtained and the availability of safe and effective noncorticosteroid treatment alternatives. To minimize the systemic effects of intranasal corticosteroids, including NASONEX Nasal Spray, 50 mcg, each patient should be titrated to his/her lowest effective dose.
Seven hundred and twenty (720) patients 3 to 11 years of age with allergic rhinitis were treated with mometasone furoate nasal spray, 50 mcg (100 mcg total daily dose) in controlled clinical trials (see CLINICAL PHARMACOLOGY, Clinical Studies section). Twenty-eight (28) patients 2 to 5 years of age with allergic rhinitis were treated with mometasone furoate nasal spray, 50 mcg (100 mcg total daily dose) in a controlled trial to evaluate safety (see CLINICAL PHARMACOLOGY, Pharmacokinetics section). Safety and effectiveness in children less than 2 years of age with allergic rhinitis and in children less than 18 years of age with nasal polyps have not been established.
A clinical study has been conducted for 1 year in pediatric patients with allergic rhinitis (ages 3 to 9 years) to assess the effect of NASONEX Nasal Spray, 50 mcg (100 mcg total daily dose) on growth velocity. No statistically significant effect on growth velocity was observed for NASONEX Nasal Spray, 50 mcg compared to placebo. No evidence of clinically relevant HPA axis suppression was observed following a 30-minute cosyntropin infusion.
The potential of NASONEX Nasal Spray, 50 mcg to cause growth suppression in susceptible patients or when given at higher doses cannot be ruled out.
Geriatric Use
A total of 280 patients above 64 years of age with allergic rhinitis or nasal polyps (age range 64 to 86 years) have been treated with NASONEX Nasal Spray, 50 mcg for up to 3 or 4 months, respectively. The adverse reactions reported in this population were similar in type and incidence to those reported by younger patients.
ADVERSE REACTIONS
Allergic Rhinitis
In controlled US and international clinical studies, a total of 3210 adult and adolescent patients ages 12 years and older with allergic rhinitis received treatment with NASONEX Nasal Spray, 50 mcg at doses of 50 to 800 mcg/day. The majority of patients (n = 2103) were treated with 200 mcg/day. In controlled US and international studies, a total of 990 pediatric patients (ages 3 to 11 years) with allergic rhinitis received treatment with NASONEX Nasal Spray, 50 mcg, at doses of 25 to 200 mcg/day. The majority of pediatric patients (720) were treated with 100 mcg/day. A total of 513 adult, adolescent, and pediatric patients have been treated for 1 year or longer. The overall incidence of adverse events for patients treated with NASONEX Nasal Spray, 50 mcg was comparable to patients treated with the vehicle placebo. Also, adverse events did not differ significantly based on age, sex, or race. Three percent or less of patients in clinical trials discontinued treatment because of adverse events; this rate was similar for the vehicle and active comparators.
All adverse events (regardless of relationship to treatment) reported by 5% or more of adult and adolescent patients ages 12 years and older who received NASONEX Nasal Spray, 50 mcg, 200 mcg/day and by pediatric patients ages 3 to 11 years who received NASONEX Nasal Spray, 50 mcg, 100 mcg/day in clinical trials vs placebo and that were more common with NASONEX Nasal Spray, 50 mcg than placebo, are displayed in the table below.
| Adult and Adolescent Patients | Pediatric Patients | |||
|---|---|---|---|---|
| 12 years and older | Ages 3 to 11 years | |||
| NASONEX | VEHICLE | NASONEX | VEHICLE | |
| 200 mcg | PLACEBO | 100 mcg | PLACEBO | |
| (n = 2103) | (n = 1671) | (n = 374) | (n = 376) | |
| Headache | 26 | 22 | 17 | 18 |
| Viral Infection | 14 | 11 | 8 | 9 |
| Pharyngitis | 12 | 10 | 10 | 10 |
| Epistaxis/Blood-Tinged Mucus | 11 | 6 | 8 | 9 |
| Coughing | 7 | 6 | 13 | 15 |
| Upper Respiratory Tract Infection | 6 | 2 | 5 | 4 |
| Dysmenorrhea | 5 | 3 | 1 | 0 |
| Musculoskeletal Pain | 5 | 3 | 1 | 1 |
| Sinusitis | 5 | 3 | 4 | 4 |
| Vomiting | 1 | 1 | 5 | 4 |
Other adverse events which occurred in less than 5% but greater than or equal to 2% of mometasone furoate adult and adolescent patients (ages 12 years and older) treated with 200-mcg doses (regardless of relationship to treatment), and more frequently than in the placebo group included: arthralgia, asthma, bronchitis, chest pain, conjunctivitis, diarrhea, dyspepsia, earache, flu-like symptoms, myalgia, nausea, and rhinitis.
Other adverse events which occurred in less than 5% but greater than or equal to 2% of mometasone furoate pediatric patients ages 3 to 11 years treated with 100-mcg doses vs placebo (regardless of relationship to treatment) and more frequently than in the placebo group included: diarrhea, nasal irritation, otitis media, and wheezing.
The adverse event (regardless of relationship to treatment) reported by 5% of pediatric patients ages 2 to 5 years who received NASONEX Nasal Spray, 50 mcg, 100 mcg/day in a clinical trial vs placebo including 56 subjects (28 each NASONEX Nasal Spray, 50 mcg and placebo) and that was more common with NASONEX Nasal Spray, 50 mcg than placebo, included: upper respiratory tract infection (7% vs 0%, respectively). The other adverse event which occurred in less than 5% but greater than or equal to 2% of mometasone furoate pediatric patients ages 2 to 5 years treated with 100-mcg doses vs placebo (regardless of relationship to treatment) and more frequently than in the placebo group included: skin trauma.
Nasal Polyps
In controlled clinical studies, the types of adverse events observed in patients with nasal polyps were similar to those observed for patients with allergic rhinitis. A total of 594 adult patients (ages 18 to 86 years) received NASONEX Nasal Spray, 50 mcg, at doses of 200 mcg once or twice daily for up to 4 months for treatment of nasal polyps. The overall incidence of adverse events for patients treated with NASONEX Nasal Spray, 50 mcg was comparable to patients treated with the placebo except for epistaxis, which was 9% for 200 mcg once daily, 13% for 200 mcg twice daily, and 5% for placebo.
Rare cases of nasal ulcers and nasal and oral candidiasis were also reported in patients treated with NASONEX Nasal Spray, 50 mcg, primarily in patients treated for longer than 4 weeks.
In postmarketing surveillance of this product, cases of nasal burning and irritation, anaphylaxis and angioedema, and rare cases of nasal septal perforation have been reported. Disturbances of taste and smell have been reported very rarely.
OVERDOSAGE
There are no data available on the effects of acute or chronic overdosage with NASONEX Nasal Spray, 50 mcg. Because of low systemic bioavailability, and an absence of acute drug-related systemic findings in clinical studies, overdose is unlikely to require any therapy other than observation. Intranasal administration of 1600 mcg (4 times the recommended dose of NASONEX Nasal Spray, 50 mcg) daily for 29 days, to healthy human volunteers, was well tolerated with no increased incidence of adverse events. Single intranasal doses up to 4000 mcg have been studied in human volunteers with no adverse effects reported. Single oral doses up to 8000 mcg have been studied in human volunteers with no adverse effects reported. Chronic overdosage with any corticosteroid may result in signs or symptoms of hypercorticism (see PRECAUTIONS). Acute overdosage with this dosage form is unlikely since one bottle of NASONEX Nasal Spray, 50 mcg contains approximately 8500 mcg of mometasone furoate.
DOSAGE AND ADMINISTRATION
Allergic Rhinitis
Adults and Children 12 Years of Age and Older
The recommended dose for prophylaxis and treatment of the nasal symptoms of seasonal allergic rhinitis and treatment of the nasal symptoms of perennial allergic rhinitis is two sprays (50 mcg of mometasone furoate in each spray) in each nostril once daily (total daily dose of 200 mcg).
In patients with a known seasonal allergen that precipitates nasal symptoms of seasonal allergic rhinitis, prophylaxis with NASONEX Nasal Spray, 50 mcg (200 mcg/day) is recommended 2 to 4 weeks prior to the anticipated start of the pollen season.
Children 2 to 11 Years of Age
The recommended dose for treatment of the nasal symptoms of seasonal allergic and perennial allergic rhinitis is one spray (50 mcg of mometasone furoate in each spray) in each nostril once daily (total daily dose of 100 mcg).
Improvement in nasal symptoms of allergic rhinitis has been shown to occur within 11 hours after the first dose based on one single-dose, parallel-group study of patients in an outdoor "park" setting (park study) and one environmental exposure unit (EEU) study and within 2 days after the first dose in two randomized, double-blind, placebo-controlled, parallel-group seasonal allergic rhinitis studies. Maximum benefit is usually achieved within 1 to 2 weeks. Patients should use NASONEX Nasal Spray, 50 mcg only once daily for allergic rhinitis at a regular interval.
Nasal Polyps
Adults 18 years of Age and Older
The recommended dose for nasal polyps is two sprays (50 mcg of mometasone furoate in each spray) in each nostril twice daily (total daily dose of 400 mcg). A dose of two sprays (50 mcg of mometasone furoate in each spray) in each nostril once daily (total daily dose of 200 mcg) is also effective in some patients.
Prior to initial use of NASONEX Nasal Spray, 50 mcg, the pump must be primed by actuating ten times or until a fine spray appears. The pump may be stored unused for up to 1 week without repriming. If unused for more than 1 week, reprime by actuating two times, or until a fine spray appears.
Directions for Use
Illustrated Patient's Instructions for Use accompany each package of NASONEX Nasal Spray, 50 mcg.
Directions for Cleaning
Illustrated Applicator Cleaning Instructions accompany each package of NASONEX Nasal Spray, 50 mcg.
HOW SUPPLIED
NASONEX (mometasone furoate monohydrate) Nasal Spray, 50 mcg is supplied in a white, high-density, polyethylene bottle fitted with a white metered-dose, manual spray pump, and blue cap. It contains 17 g of product formulation, 120 sprays, each delivering 50 mcg of mometasone furoate per actuation. Supplied with Patient's Instructions for Use (NDC 0085-1288-01).
Store at 25°C (77°F); excursions permitted to 15–30°C (59–86°F) [see USP Controlled Room Temperature]. Protect from light.
When NASONEX Nasal Spray, 50 mcg is removed from its cardboard container, prolonged exposure of the product to direct light should be avoided. Brief exposure to light, as with normal use, is acceptable.
SHAKE WELL BEFORE EACH USE.

Schering Corporation
Kenilworth, NJ 07033 USA
Copyright © 1997, 2003, 2005, Schering Corporation.
All rights reserved.
Rev. 9/05
26405289T
Patient's Instructions for Use
SHAKE WELL BEFORE EACH USE
NASONEX®
(mometasone furoate monohydrate)
Nasal Spray, 50 mcg2
Shake the bottle well before each use. Read complete instructions carefully and use only as directed.
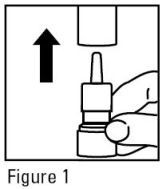
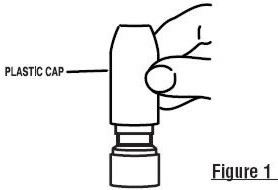
- Remove the plastic cap (Figure 1).
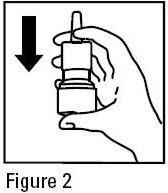
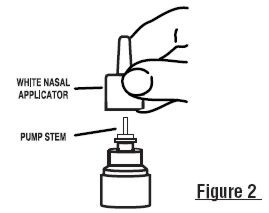
- The very first time the spray is used, prime the pump by pressing downward on the shoulders of the white applicator using your forefinger and middle finger while supporting the base of the bottle with your thumb (Figure 2). The actuator does not need to be pierced in order for the unit to function. Press down and release the pump ten times or until a fine spray appears. DO NOT spray into eyes. The pump is now ready to use. The pump may be stored unused for up to 1 week without repriming. If unused for more than 1 week, reprime by spraying two times or until a fine spray appears.
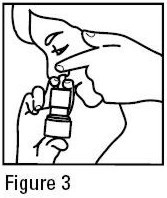
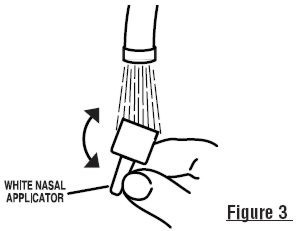
- Gently blow your nose to clear the nostrils. Close one nostril. Tilt your head forward slightly and, keeping the bottle upright, carefully insert the nasal applicator into the other nostril (Figure 3). DO NOT spray directly onto nasal septum, the wall between the two nostrils.
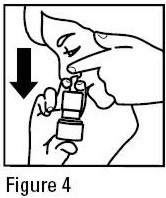
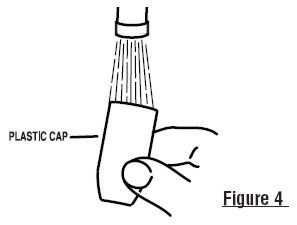
- For each spray, press firmly downward once on the shoulders of the white applicator using your forefinger and middle finger while supporting the base of the bottle with your thumb. Breathe gently inward through the nostril (Figure 4).
- Then breathe out through the mouth.
- Repeat in the other nostril.
- Wipe the nasal applicator with a clean tissue and replace the plastic cap.
Pediatric Use: Administration to young children should be aided by an adult. The Patient's Instructions for Use, Steps 1 to 7 should be followed.
The correct amount of medication in each spray can only be assured up to 120 sprays from the bottle even though the bottle is not completely empty. You should keep track of the number of sprays used from each bottle of NASONEX Nasal Spray, 50 mcg and discard the bottle after using 120 sprays.
Cleaning: Please see Applicator Cleaning Instructions on reverse.
Caution: NASONEX Nasal Spray, 50 mcg is formulated for once- or twice-daily dosing depending on your condition. You should use NASONEX Nasal Spray, 50 mcg once or twice daily as directed. Since NASONEX Nasal Spray, 50 mcg is not intended to give rapid relief of your nasal symptoms, the prescribed dosage should not be increased by using more often than your physician prescribed in an attempt to increase its effectiveness. NASONEX Nasal Spray, 50 mcg helps to control your condition so it is important that you use it regularly as directed by your physician.
NASONEX Nasal Spray treats seasonal and year-round nasal allergy symptoms in adults and children 2 years and older. Based on single-day studies done in a park during pollen season or in a controlled pollen exposure room, improvement in nasal allergy symptoms has been shown to occur within 11 hours after the first dose. In other studies that lasted up to 2 weeks, improvement in nasal symptoms of seasonal allergic rhinitis was shown to occur within 2 days after the first dose. The full benefit of NASONEX Nasal Spray, 50 mcg, in allergic rhinitis is usually achieved within 1 to 2 weeks. NASONEX Nasal Spray can also be used to help prevent seasonal nasal allergy symptoms in adults and children 12 years and older, when treatment starts 2 to 4 weeks before the allergy season.
In patients aged 18 years and older, NASONEX Nasal Spray is also used to treat nasal polyps.
Side effects were generally mild and included headache, viral infection, sore throat, nosebleeds, and coughing.
NASONEX Nasal Spray, 50 mcg should not be sprayed into the eyes. Spraying NASONEX Nasal Spray, 50 mcg directly onto the nasal septum should be avoided.
Store at 25°C (77°F); excursions permitted to 15–30°C (59–86°F) [see USP Controlled Room Temperature]. Protect from light.
When NASONEX Nasal Spray, 50 mcg is removed from its cardboard container, prolonged exposure of the product to direct light should be avoided. Brief exposure to light, as with normal use, is acceptable.
SHAKE WELL BEFORE EACH USE.
- 2
- calculated on the anhydrous basis

Schering Corporation
Kenilworth, NJ 07033 USA
Copyright © 1997, 2003, 2005, Schering Corporation. All rights reserved.
U.S. Patent Nos. D355,844; 5,837,699; 6,127,353; and 6,723,713 Rev. 9/05
APPLICATOR CLEANING INSTRUCTIONS
NASONEX®
(mometasone furoate monohydrate)
Nasal Spray, 50 mcg3
- To clean the nasal applicator, remove the plastic cap (Figure 1).
- Pull gently upward on the white nasal applicator so that it comes free (Figure 2).
- Soak the nasal applicator in cold tap water and/or rinse both ends of the nasal applicator under cold tap water and dry (Figure 3). Do not try to unblock the nasal applicator by inserting a pin or other sharp object.
- Rinse the plastic cap under cold water and dry (Figure 4).
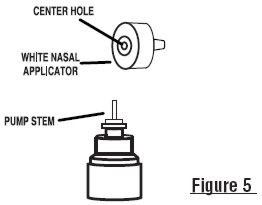
- Reassemble the nasal applicator being certain the pump stem is reinserted into the applicator's center hole (Figure 5).
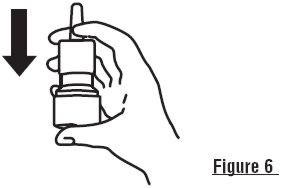
- Reprime the pump by pressing downward on the shoulders of the white applicator using your forefinger and middle finger while supporting the base of the bottle with your thumb. Press down and release the pump two times or until a fine spray appears. DO NOT spray into eyes. The pump is now ready to use. The pump may be stored unused for up to 1 week without repriming. If unused for more than 1 week, reprime by spraying two times or until a fine spray appears (Figure 6).
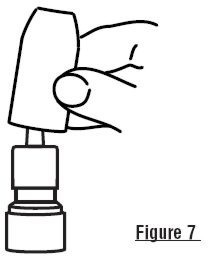
- Replace the plastic cap (Figure 7).
- 3
- calculated on the anhydrous basis

Schering Corporation
Kenilworth, NJ 07033 USA
Copyright © 1997, 2003, 2005, Schering Corporation. All rights reserved.
U.S. Patent Nos. D355,844; 5,837,699; 6,127,353; and 6,723,713 Rev. 9/05
| NASONEX
mometasone furoate monohydrate spray, metered |
|||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||
Revised: 11/2008Schering Corporation