DIPHTHERIA AND TETANUS TOXOIDS ADSORBED- corynebacterium diphtheriae toxoid antigen (formaldehyde inactivated) and clostridium tetani toxoid antigen (formaldehyde inactivated) injection, suspension
Sanofi Pasteur Inc.
----------
DESCRIPTION
Diphtheria and Tetanus Toxoids Adsorbed USP (For Pediatric Use) (DT), for intramuscular use, is a sterile suspension of alum-precipitated (aluminum potassium sulfate) toxoid in an isotonic sodium chloride solution. The vaccine, after shaking, is a turbid liquid, whitish-gray in color.
Corynebacterium diphtheriae cultures are grown in a modified Mueller and Miller medium.1 Clostridium tetani cultures are grown in a peptone-based medium containing bovine extract. The meat used in this medium is US sourced. Both toxins are detoxified with formaldehyde. The detoxified materials are then separately purified by serial ammonium sulfate fractionation and diafiltration. The 1 dose vial of vaccine is formulated without preservatives but contains a trace amount of thimerosal (a mercury [Hg] containing compound) from the manufacturing process (≤0.3 µg Hg/0.5 mL dose).
Each 0.5 mL dose is formulated to contain 6.7 Lf of diphtheria toxoid, 5 Lf of tetanus toxoid, and not more than 0.17 mg of aluminum. The residual formaldehyde content, by assay, is less than 0.02%. Both toxoids induce at least 2 units of antitoxin per mL in the guinea pig potency test.
CLINICAL PHARMACOLOGY
DIPHTHERIA
Corynebacterium diphtheriae may cause both localized and generalized disease. Systemic intoxication is caused by diphtheria exotoxin, an extracellular protein metabolite of toxigenic strains of C diphtheriae. Protection against disease is due to the development of neutralizing antibodies to diphtheria toxin.
At one time, diphtheria was common in the United States (US). More than 200,000 cases, primarily among young children, were reported in 1921. Approximately 5% to 10% of cases were fatal; the highest case-fatality ratios were recorded for the very young and the elderly. Reported cases of diphtheria of all types declined from 306 in 1975 to 59 in 1979; most were cutaneous diphtheria reported from a single state. After 1979, cutaneous diphtheria was no longer a notifiable disease. From 1980 to 1989, only 24 cases of respiratory diphtheria were reported; two cases were fatal, and 18 (75%) occurred among persons 20 years of age or older.2
Diphtheria is currently a rare disease in the US primarily because of the high level of appropriate vaccination among children (97% of children entering school have received ≥three doses of diphtheria and tetanus toxoids and pertussis vaccine adsorbed [DTP]) and because of an apparent reduction in the prevalence of toxigenic strains of C diphtheriae. Most cases occur among unvaccinated or inadequately immunized persons.2
Both toxigenic and nontoxigenic strains of C diphtheriae can cause disease, but only strains that produce toxin cause myocarditis and neuritis. Toxigenic strains are more often associated with severe or fatal illness in noncutaneous (respiratory or other mucosal surface) infections and are more commonly recovered in association with respiratory than from cutaneous infections.2
A complete vaccination series substantially reduces the risk of developing diphtheria, and vaccinated persons who develop disease have milder illness. Protection lasts at least 10 years. Vaccination does not, however, eliminate carriage of C diphtheriae in the pharynx or nose or on the skin.2
Protection against diphtheria and tetanus can be provided by circulating protective levels of diphtheria and tetanus antitoxin which can be induced by the administration of Diphtheria and Tetanus Toxoids Adsorbed USP (For Pediatric Use) (DT).
A clinical study was performed in 20 children under one year of age to determine the serological responses and the adverse reactions when Sanofi Pasteur Inc. DT was administered as a primary series of three doses. Protective levels of diphtheria and tetanus antitoxins (0.01 AU/mL) were detected in 100% of the children following two doses of the vaccine. However, maternal antibody may have contributed to the total neutralizing antibody in some of these infants. Protective levels of antitoxin were observed in 100% of these infants following three doses of DT. No local or systemic reactions were observed in approximately half of the infants and only mild or moderate reactions were observed in the remainder of the DT study group. (TABLE 1)3
| Post 2 Doses* | Post 3 Doses | |
|---|---|---|
|
||
| Diphtheria Antitoxin (>0.01 units/mL) | 20/20 (100%) | 20/20 (100%) |
| Tetanus Antitoxin (>0.01 units/mL) | 20/20 (100%) | 20/20 (100%) |
Another clinical study to evaluate serological responses and adverse reactions of Sanofi Pasteur Inc.'s DT was performed in 40 children under one year of age. One group of 20 children received 0.5 mL doses of DTP, DT, DTP at two, four and six months of age, respectively. The second group of 20 children received 0.5 mL doses of DTP, DTP, and DT, respectively, at the same ages.4
The immunologic protection as measured by toxin neutralization induced by DT was comparable when administered as either a second or third dose (TABLE 2).4
| Antibody | DTP, DT, DTP Group | DTP, DTP, DT Group |
|---|---|---|
| Diphtheria Antitoxin (>0.01 units/mL) | 18/18 (100%) | 19/19 (100%) |
| Tetanus Antitoxin (>0.01 units/mL) | 18/18 (100%) | 19/19 (100%) |
The reaction rates following Sanofi Pasteur Inc. whole-cell DTP vaccination closely correlated with the rates observed with other commercially available whole-cell DTP vaccines.5 The incidence of adverse reactions was significantly lower following DT administration (p <0.05). Although the number of vaccinees was small, no persistent screaming episodes or severe neurological reactions such as seizures or encephalopathy were observed with either vaccine in this study.4
As with any vaccine, vaccination with DT may not protect 100% of individuals.
TETANUS
Tetanus is an intoxication manifested primarily by neuromuscular dysfunction caused by a potent exotoxin elaborated by Clostridium tetani.
The occurrence of tetanus in the US has decreased dramatically from 560 reported cases in 1947 to a record low of 48 reported cases in 1987. Tetanus in the US is primarily a disease of older adults. Of 99 tetanus patients with complete information reported to the Centers for Disease Control and Prevention (CDC) during 1987 and 1988, 68% were ≥50 years of age, while only six were <20 years of age. Overall, the case-fatality rate was 21%.2 In 1992, 45 cases were reported of which 82% were ≥50 years of age.6 The disease continues to occur almost exclusively among persons who are unvaccinated or inadequately vaccinated or whose vaccination histories are unknown or uncertain.2
In 4% of tetanus cases reported during 1987 and 1988, no wound or other condition was implicated. Non-acute skin lesions, such as ulcers, or medical conditions such as abscesses, were reported in association with 14% of cases.2
Spores of C tetani are ubiquitous. Serologic tests indicate that naturally acquired immunity to tetanus toxin does not occur in the US.2 Thus, universal primary vaccination, with subsequent maintenance of adequate antitoxin levels by means of appropriately timed boosters, is necessary to protect persons among all age-groups. Tetanus toxoid is a highly effective antigen, and a completed primary series generally induces protective levels of neutralizing antibodies to tetanus toxin that persist for ≥10 years.2
The potency of diphtheria and tetanus toxoids was determined on the basis of immunogenicity studies with a comparison to a serological correlate of protection (0.01 antitoxin units/mL) established by the Panel on Review of Bacterial Vaccines & Toxoids.7
INDICATIONS AND USAGE
Diphtheria and Tetanus Toxoids Adsorbed (For Pediatric Use) (DT) is indicated for active immunization of children up to age 7 years against diphtheria and tetanus. Diphtheria and Tetanus Toxoids and Acellular Pertussis Vaccine (DTaP) – Tripedia®, or DTP is recommended for primary immunization of infants and persons up to 7 years of age. However, in instances where the pertussis vaccine component is contraindicated, or where the physician decides that pertussis vaccine is not to be administered, DT should be used.2 Immunization should be started at 6 weeks to 2 months of age and be completed before the seventh birthday. Immunization always should be started at once if diphtheria is present in the community.
This vaccine is NOT to be used for the treatment of diphtheria or tetanus infection.
This vaccine should NOT be used for immunizing persons 7 years of age and older. For persons 7 years of age and older, the recommended vaccine is Tetanus and Diphtheria Toxoids Adsorbed for Adult Use (Td).
As with any vaccine, vaccination with DT may not protect 100% of individuals.
If passive immunization is required, Tetanus Immune Globulin (Human) (TIG) and/or equine Diphtheria Antitoxin are the products of choice for tetanus and diphtheria, respectively (see DRUG INTERACTIONS and DOSAGE AND ADMINISTRATION sections).
CONTRAINDICATIONS
HYPERSENSITIVITY TO ANY COMPONENT OF THE VACCINE, INCLUDING THIMEROSAL, A MERCURY DERIVATIVE, IS A CONTRAINDICATION FOR FURTHER USE OF THIS VACCINE.
It is a contraindication to use this or any other related vaccine after an immediate anaphylactic reaction associated with a previous dose.
A history of systemic allergic or neurologic reactions following a previous dose of DT is an absolute contraindication for further use.2
If a contraindication to using tetanus toxoid-containing preparations exists in a person who has not completed a primary immunizing course of tetanus toxoid and other than a clean, minor wound is sustained, only passive immunization should be given using TIG (Human).2
Immunization should be deferred during the course of an acute illness. Vaccination of infants and children with severe, febrile illness should generally be deferred until these persons have recovered. However, the presence of minor illnesses such as mild upper respiratory infections with or without low grade fever should not preclude vaccination.2
Elective immunization procedures should be deferred during an outbreak of poliomyelitis.8
WARNINGS
This product contains dry natural latex rubber as follows: The stopper to the vial contains dry natural latex rubber.
Persons who experienced Arthus-type hypersensitivity reactions or a temperature of >103°F (>39.4°C) following a prior dose of tetanus toxoid usually have high serum tetanus antitoxin levels and should not be given even emergency doses of Td more frequently than every 10 years, even if they have a wound that is neither clean nor minor.2
Because intramuscular injection can cause injection site hematoma, DT should not be given to persons with any bleeding disorder, such as hemophilia or thrombocytopenia, or to persons on anticoagulant therapy unless the potential benefits clearly outweigh the risk of administration. If the decision is made to administer DT in such persons, it should be given with caution, with steps taken to avoid the risk of hematoma formation following injection.9
This vaccine is not to be administered to persons 7 years of age and older, since adverse reactions to the quantity of diphtheria toxoid contained in DT may be more severe in this age group than in young children.
Deaths have been reported in temporal association with the administration of DT vaccine; however, no causal relationship was proven10 (see ADVERSE REACTIONS section).
PRECAUTIONS
GENERAL
Care is to be taken by the health-care provider for the safe and effective use of DT.
EPINEPHRINE INJECTION (1:1000) MUST BE IMMEDIATELY AVAILABLE SHOULD AN ACUTE ANAPHYLACTIC REACTION OCCUR DUE TO ANY COMPONENT OF THE VACCINE.
There is an increased incidence of local and systemic reactions to booster doses of tetanus toxoid when given to previously immunized persons. (Refer to DOSAGE AND ADMINISTRATION section for timing of recall injections.) Prior to an injection of any vaccine, all known precautions should be taken to prevent adverse reactions. This should include a review of the patient's history with respect to possible sensitivity and any previous adverse reactions (see CONTRAINDICATIONS section) to the vaccine or similar vaccines and to possible sensitivity to dry natural latex rubber, and a current knowledge of the literature concerning the use of the vaccine under consideration.
Special care should be taken to ensure that the injection does not enter a blood vessel.
Immunosuppressive therapies including radiation, corticosteroids, antimetabolites, alkylating agents, and cytotoxic drugs may reduce the immune response to vaccines. Therefore, routine vaccination should be deferred, if possible, while patients are receiving such therapy.2 If DT has been administered to persons receiving immunosuppressive therapy, or having an immunodeficiency disorder, an adequate antibody response may not be obtained.2 When possible, immunosuppressive treatment should be interrupted when immunization is required due to a tetanus-prone wound.
Administration of DT is not contraindicated in individuals with HIV infection.9
A separate, sterile syringe and needle or a sterile disposable unit should be used for each patient to prevent transmission of hepatitis or other infectious agents from person to person. Needles should not be recapped and should be disposed of according to biohazard waste guidelines.
INFORMATION FOR PATIENTS
Prior to administration of DT, health-care personnel should inform the parent or guardian of the patient the benefits and risks of immunization, and also inquire about the recent health status of the patient to be injected.
As part of the child's permanent immunization record, the date, lot number and manufacturer of the vaccine administered MUST be recorded.11,12,13
The health-care provider should inform the parent or guardian of the patient about the potential for adverse reactions that have been temporally associated with DT administration. The parent or guardian should be instructed to report any serious adverse reactions to their health-care provider.
IT IS EXTREMELY IMPORTANT WHEN THE CHILD RETURNS FOR THE NEXT DOSE IN THE SERIES, THAT THE PARENT OR GUARDIAN OF THE PATIENT SHOULD BE QUESTIONED CONCERNING OCCURRENCE OF ANY SYMPTOMS AND/OR SIGNS OF AN ADVERSE REACTION AFTER PREVIOUS DOSE (see CONTRAINDICATIONS and ADVERSE REACTIONS sections).
The health-care provider should inform the parent or guardian of the patient the importance of completing the immunization series.
The health-care provider should provide the Vaccine Information Statements (VISs) which are required to be given with each immunization.
DRUG INTERACTIONS
If passive immunization for tetanus is needed, TIG (Human) is the product of choice for tetanus. It provides longer protection than antitoxin of animal origin and causes few adverse reactions. The currently recommended prophylactic dose of TIG (Human) for wounds of average severity is 250 units intramuscularly. When tetanus toxoid and TIG (Human) are given concurrently, separate syringes and separate sites should be used. The ACIP recommends the use of only adsorbed toxoid in this situation.2
Diphtheria Antitoxin (equine) is available for treatment of the acute phases of diphtheria. When DT and Diphtheria Antitoxin are used together, they must be given at different sites using separate needles and syringes.
As with other intramuscular injections, use with caution in patients on anticoagulant therapy.
Immunosuppressive therapies may reduce the response to vaccines (see PRECAUTIONS – GENERAL section).
CARCINOGENESIS, MUTAGENESIS, IMPAIRMENT OF FERTILITY
No studies have been performed to evaluate carcinogenicity, mutagenic potential, or impact on fertility.
PEDIATRIC USE
SAFETY AND EFFECTIVENESS OF DT VACCINE IN INFANTS BELOW THE AGE OF SIX WEEKS HAVE NOT BEEN ESTABLISHED.
This vaccine is recommended for immunizing children 6 weeks of age through 6 years of age (up to the seventh birthday). Diphtheria and Tetanus Toxoids and Acellular Pertussis Vaccine (DTaP) – Tripedia®, or DTP are the preferred vaccines in this age group, but in those situations where an absolute contraindication to pertussis vaccination exists, or where in the opinion of the physician the pertussis vaccine should not be administered, DT is the appropriate alternative.
ADVERSE REACTIONS
BODY SYSTEM AS A WHOLE
Adverse reactions may be local and include redness, warmth, edema, induration, with or without tenderness, as well as urticaria, and rash. Malaise, transient fever, pain, hypotension, nausea and arthralgia may develop in some patients after the injection. Arthus-type hypersensitivity reactions, characterized by severe local reactions (generally starting 2 to 8 hours after an injection) may occur, particularly in persons who have received multiple prior boosters.2
Rarely, an anaphylactic reaction (ie, hives, swelling of the mouth, difficulty breathing, hypotension, or shock) and death have been reported after receiving preparations containing diphtheria and tetanus antigens.2
The vaccine was well tolerated clinically. No local or systemic reactions were observed in approximately half of the infants and only mild or moderate reactions were observed in the remainder of the study group (TABLE 3).3
| Category of Reactions | ||||
|---|---|---|---|---|
| None | Mild* | Moderate † | Severe | |
| Post Dose 1 | 9/20 (45%) | 11 (55%) | 0 | 0 |
| Post Dose 2 | 11/20 (55%) | 7 (35%) | 2/20 (10%) | 0 |
| Post Dose 3 | 11/20 (55%) | 9 (45%) | 0 | 0 |
Deaths due to causes other than SIDS, including deaths from serious infections, have been reported in temporal association with the administration of diphtheria and tetanus toxoids containing vaccines. On rare occasion, anaphylaxis has been reported following administration of products containing diphtheria and tetanus toxoids. Upon review, a report by the Institute of Medicine (IOM) concluded the evidence established a causal relationship between diphtheria and tetanus toxoids and anaphylaxis.10
NERVOUS SYSTEM
The following neurologic illnesses have been reported as temporally associated with vaccine containing tetanus toxoid: neurological complications14 including cochlear lesion,15 brachial plexus neuropathies,15,16 paralysis of the radial nerve,17 paralysis of the recurrent nerve,15 accommodation paresis, Guillain-Barré syndrome (GBS), and EEG disturbances with encephalopathy.18 The IOM following review of the reports of neurologic events following vaccination with tetanus toxoid, Td or DT, concluded the evidence favored acceptance of a causal relationship between tetanus toxoid and brachial neuritis and GBS.10,19
EPINEPHRINE INJECTION (1:1000) MUST BE IMMEDIATELY AVAILABLE SHOULD AN ACUTE ANAPHYLACTIC REACTION OCCUR DUE TO ANY COMPONENT OF THE VACCINE.
Reporting of Adverse Events
The National Vaccine Injury Compensation Program, established by the National Childhood Vaccine Injury Act of 1986, requires physicians and other health-care providers who administer vaccines to maintain permanent vaccination records and to report occurrences of certain adverse events to the US Department of Health and Human Services. Reportable events include those listed in the Act for each vaccine and events specified in the package insert as contraindications to further doses of the vaccine.12,13
Reporting by parents or guardians of all adverse events after vaccine administration should be encouraged. Adverse events following immunization with vaccine should be reported by health-care providers to the US Department of Health and Human Services (DHHS) Vaccine Adverse Event Reporting System (VAERS). Reporting forms and information about reporting requirements or completion of the form can be obtained from VAERS through a toll-free number 1-800-822-7967.11,12,13
Health-care providers also should report these events to the Pharmacovigilance Department, Sanofi Pasteur Inc., Discovery Drive, Swiftwater, PA 18370, or call 1-800-822-2463.
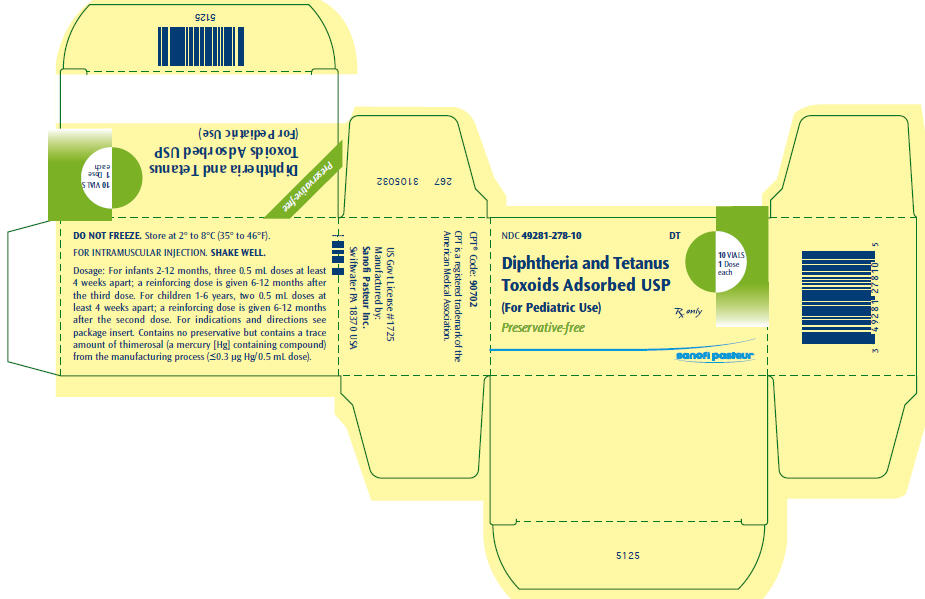
DOSAGE AND ADMINISTRATION2
Parenteral drug products should be inspected visually for extraneous particulate matter and/or discoloration prior to administration whenever solution and container permit. If these conditions exist, the vaccine should not be administered.
SHAKE VIAL WELL before withdrawing each dose. Discard vial of vaccine if it cannot be resuspended.
Inject 0.5 mL intramuscularly only. The preferred injection sites are the anterolateral aspect of the thigh and the deltoid muscle of the upper arm. The vaccine should not be injected into the gluteal area or areas where there may be a major nerve trunk. During the course of primary immunizations, injections should not be made more than once at the same site.
The following guidelines are derived from the Advisory Committee on Immunization Practices (ACIP).2
PRIMARY IMMUNIZATION
This vaccine is recommended for children 6 weeks through 6 years (up to the seventh birthday), ideally beginning when the infant is 6 weeks to 2 months of age.
For infants 6 weeks through 12 months, the primary series consists of 4 doses: administer three 0.5 mL doses intramuscularly 4 to 8 weeks apart. A reinforcing dose is given 6 to 12 months after the third injection.
For children 1 year through 6 years (up to the seventh birthday), the primary series consists of 3 doses: administer two 0.5 mL doses intramuscularly 4 to 8 weeks apart. A reinforcing dose is given 6 to 12 months after the second injection. In the event the final immunizing dose would be given after the seventh birthday, use Tetanus and Diphtheria Toxoids Adsorbed For Adult Use.
BOOSTER IMMUNIZATION
For children between 4 and 6 years of age (preferably at time of kindergarten or elementary school entrance), a booster of 0.5 mL should be administered intramuscularly. Those who receive all four primary immunizing doses before their fourth birthday should receive a single dose of DT just before entering kindergarten or elementary school. This booster dose is not necessary if the fourth dose in the primary series was given after the fourth birthday. Thereafter, routine booster immunizations should be with Tetanus and Diphtheria Toxoids Adsorbed For Adult Use, at intervals of 10 years.
PERSONS 7 YEARS OF AGE AND OLDER SHOULD NOT BE IMMUNIZED WITH DIPHTHERIA AND TETANUS TOXOIDS ADSORBED (FOR PEDIATRIC USE).
Preterm infants should be vaccinated according to their chronological age from birth.2
Interruption of the recommended schedule with a delay between doses does not interfere with the final immunity achieved with DT. There is no need to start the series over again, regardless of the time elapsed between doses.
The simultaneous administration of DT, oral polio virus vaccine (OPV), and measles-mumps-rubella vaccine (MMR) has resulted in seroconversion rates and rates of side effects similar to those observed when the vaccines are administered separately. Simultaneous vaccination (at separate sites and separate syringes) with DT, MMR, OPV, or inactivated poliovirus vaccine (IPV), and Haemophilus b Conjugate Vaccine (HbCV) is also acceptable. The ACIP recommends the simultaneous administration, at separate sites and separate syringes, of all vaccines appropriate to the age and previous vaccination status of the recipients including the special circumstance of simultaneous administration of DT, OPV, HbCV, and MMR at ≥15 months of age.2
If passive immunization for tetanus is needed, TIG (Human) is the product of choice. It provides longer protection than antitoxin of animal origin and causes few adverse reactions. The currently recommended prophylactic dose of TIG (Human) for wounds of average severity is 250 units intramuscularly. When tetanus toxoid and TIG (Human) are given concurrently, separate syringes and separate sites should be used. The ACIP recommends the use of only adsorbed toxoid in this situation.2
HOW SUPPLIED
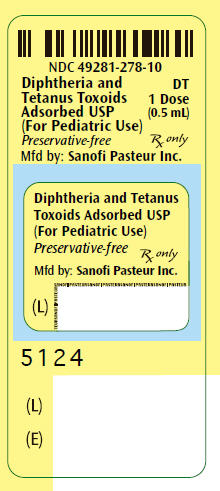
Vial, 1 Dose (contains NO preservative) (10 per package) – Product No. 49281-278-10
CPT® Code: 90702
CPT is a registered trademark of the American Medical Association.
REFERENCES
- Mueller JH, et al. Production of diphtheria toxin of high potency (100 Lf) on a reproducible medium. J Immunol 40: 21-32, 1941
- Recommendations of the Advisory Committee on Immunization Practices (ACIP). Diphtheria, Tetanus, and Pertussis: Recommendations for vaccine use and other preventive measures. MMWR 40: No. RR-10, 1991
- Pichichero ME, et al. Pediatric diphtheria and tetanus toxoids-adsorbed vaccine: Immune response to the first booster following the diphtheria and tetanus toxoids vaccine primary series. Pediatr Infec Dis 5: 428-430, 1986
- Barkin RM, et al. Pediatric diphtheria and tetanus toxoids (DT) vaccine: Clinical and immunologic response when administered as the primary series. J Pediatr 106: 779-781, 1985
- Baraff L, et al. DTP – associated reactions: An analysis by injection site, manufacturer, prior reactions and dose. Pediatr 73: 31, 1984
- Centers for Disease Control and Prevention (CDC). Summary of Notifiable Diseases, United States 1992. MMWR 41: No. 55, 1993
- Department of Health and Human Services, Food and Drug Administration. Biologicals Products; Bacterial Vaccines and Toxoids; Implementation of Efficacy Review; Proposed Rule. Federal Register Vol 50 No 240, pp 51002-51117, 1985
- Wilson GS. The Hazards of Immunization. Provocation poliomyelitis. 270-274, 1967
- ACIP. General recommendations on immunization. Recommendations of the Advisory Committee on Immunization Practices (ACIP) and the American Academy of Family Physicians (AAFP). MMWR 2002;51(RR-02):1-36
- Stratton KR, et al. Adverse events associated with childhood vaccines. Evidence Bearing on Causality. National Academy Press, Washington, DC, 1994
- CDC. Vaccine Adverse Event Reporting System – United States. MMWR 39: 730-733, 1990
- CDC. National Childhood Vaccine Injury Act: requirements for permanent vaccination records and for reporting of selected events after vaccination. MMWR 37: 197-200, 1988
- Food and Drug Administration. New reporting requirements for vaccine adverse events. FDA Drug Bull 18 (2), 16-18, 1988
- Rutledge SL, et al. Neurological complications of immunizations. J Pediatr 109: 917-924, 1986
- Wilson GS. The Hazards of Immunization. Allergic manifestations: Post-vaccinal neuritis. pp 153-156, 1967
- Tsairis P, et al. Natural history of brachial plexus neuropathy. Arch Neurol 27: 109-117, 1972
- Blumstein GI, et al. Peripheral neuropathy following Tetanus toxoid administration. JAMA 198: 1030-1031, 1966
- Cody CL, et al. Nature and rates of adverse reactions associated with DTP and DT immunizations in infants and children. Pediatr 68: 650-660, 1981
- Pollard JD, et al. Relapsing neuropathy due to tetanus toxoid: report of a case. J Neurol Sci 37: 112-125, 1978
Product information
as of December 2005
Manufactured by:
Sanofi Pasteur Inc.
Swiftwater PA 18370 USA
267 3105033
5127
| DIPHTHERIA AND TETANUS TOXOIDS ADSORBED
corynebacterium diphtheriae toxoid antigen (formaldehyde inactivated) and clostridium tetani toxoid antigen (formaldehyde inactivated) injection, suspension |
|||||||||||||
|
|||||||||||||
|
|||||||||||||
|
|||||||||||||
|
|||||||||||||
|
|||||||||||||
| Labeler - Sanofi Pasteur Inc. (086723285) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
| Sanofi Pasteur Inc. | 086723285 | MANUFACTURE | |