HEPARIN SODIUM IN SODIUM CHLORIDE
-
heparin sodium injection
B. Braun Medical Inc.
----------
Heparin Sodium in
0.9% Sodium Chloride Injection
Do not admix with other drugs.
DESCRIPTION
Heparin Sodium (2 units/mL) in 0.9% Sodium Chloride Injection is a sterile, nonpyrogenic solution prepared from Heparin Sodium USP (derived from porcine intestinal mucosa and standardized for use as an anticoagulant) in 0.9% Sodium Chloride Injection. It is to be administered by intravenous injection. The potency is determined by a biological assay using a USP reference standard based on units of heparin activity per milligram.
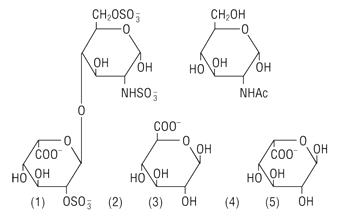
Heparin is a heterogenous group of straight-chain anionic mucopolysaccharides, called glycosaminoglycans having anticoagulant properties. Although others may be present, the main sugars occurring in heparin are: (1) alpha-L-iduronic acid 2-sulfate, (2) 2-deoxy-2-sulfamino-alpha-D-glucose 6-sulfate, (3) beta-D-glucuronic acid, (4) 2-acetamido-2-deoxy- alpha-D-glucose, and (5) alpha-L-iduronic acid. These sugars are present in decreasing amounts, usually in the order (2) > (1) > (4) > (3) > (5), and are joined by glycosidic linkages, forming polymers of varying sizes. Heparin is strongly acidic because of its content of covalently linked sulfate and carboxylic acid groups. In heparin sodium, the acidic protons of the sulfate units are partially replaced by sodium ions.
Structure of Heparin Sodium (representative subunits):
The formulas of the inactive ingredients are:
| Ingredients | Molecular Formula | Molcular Weight |
|---|---|---|
| Sodium Chloride USP | NaCl | 58.44 |
| Dibasic Sodium Phosphate Heptahydrate USP | Na2HPO4•7H2O | 268.07 |
| Citric Acid Anhydrous USP | CH2(COOH)C(OH)(COOH)CH2COOH | 192.12 |
Each 100 mL contains 0.43 g Dibasic Sodium Phosphate•7H2O USP and 0.037 g Citric Acid Anhydrous USP as a buffer system, 0.9 g Sodium Chloride USP, and Water for Injection USP qs.
pH: 7.0 (6.8–7.2); Calculated Osmolarity: 360 mOsmol/liter
Concentration of Electrolytes (mEq/liter): Sodium 186; Chloride 154; Phosphate (HPO ) 32; Citrate 6
) 32; Citrate 6
The EXCEL® Container is Latex-free; PVC-free; and DEHP-free.
The plastic container is made from a multilayered film specifically developed for parenteral drugs. It contains no plasticizers and exhibits virtually no leachables. The solution contact layer is a rubberized copolymer of ethylene and propylene. The container is nontoxic and biologically inert. The container-solution unit is a closed system and is not dependent upon entry of external air during administration. The container is overwrapped to provide protection from the physical environment and to provide an additional moisture barrier when necessary.
The closure system has two ports; the one for the administration set has a tamper evident plastic protector. Refer to the Directions for Use of the container.
CLINICAL PHARMACOLOGY
Heparin inhibits reactions that lead to the clotting of blood and the formation of fibrin clots both in vitro and in vivo. Heparin acts at multiple sites in the normal coagulation system. Small amounts of heparin in combination with antithrombin III (heparin cofactor) can inhibit thrombosis by inactivating activated Factor X and inhibiting the conversion of prothrombin to thrombin. Once active thrombosis has developed, larger amounts of heparin can inhibit further coagulation by inactivating thrombin and preventing the conversion of fibrinogen to fibrin. Heparin also prevents the formation of a stable fibrin clot by inhibiting the activation of the fibrin stabilizing factor.
Bleeding time is usually unaffected by heparin. Clotting time is prolonged by full therapeutic doses of heparin; in most cases it is not measurably affected by low doses of heparin.
Patients over 60 years of age, following similar doses of heparin, may have higher plasma levels of heparin and longer activated partial thromboplastin times (APTTs) compared with patients under 60 years of age.
Peak plasma levels of heparin are achieved 2–4 hours following subcutaneous administration, although there are considerable individual variations. Loglinear plots of heparin plasma concentrations with time for a wide range of dose levels are linear which suggests the absence of zero order processes. Liver and the reticuloendothelial system are the sites of biotransformation. The biphasic elimination curve, a rapidly declining alpha phase (t½ = 10 minutes) and after the age of 40 a slower beta phase, indicates uptake in organs. The absence of a relationship between anticoagulant half-life and concentration half-life may reflect factors such as protein binding of heparin.
Heparin does not have fibrinolytic activity; therefore, it will not lyse existing clots.
Sodium, the major cation of the extracellular fluid, functions primarily in the control of water distribution, fluid balance, and osmotic pressure of body fluids. Sodium is also associated with chloride and bicarbonate in the regulation of the acid-base equilibrium of body fluid. Chloride, the major extracellular anion, closely follows the metabolism of sodium, and changes in the acid-base balance of the body are reflected in the chloride concentration.
INDICATIONS AND USAGE
Heparin Sodium Injection in 0.9% Sodium Chloride at the concentration of 2 units/mL is indicated as an anticoagulant to maintain catheter patency.
CONTRAINDICATIONS
Heparin sodium should not be used in patients:
With severe thrombocytopenia;
In whom suitable blood coagulation tests - e.g., the whole blood clotting time, partial thromboplastin time, etc., - cannot be performed at appropriate intervals (this contraindication refers to full-dose heparin; there is usually no need to monitor coagulation parameters in patients receiving low-dose heparin);
With an uncontrollable active bleeding state (see WARNINGS), except when this is due to disseminated intravascular coagulation.
This solution is contraindicated where the administration of sodium or chloride could be clinically detrimental.
WARNINGS
Heparin is not intended for intramuscular use.
Fatal Medication Errors
Do not use Heparin Sodium in 0.9% Sodium Chloride Injection as a "catheter lock flush" product. Heparin is supplied in a wide range of strengths. Fatal hemorrhages have occurred in infants and pediatric patients due to medication errors in which 1 mL Heparin Sodium Injection vials were confused with 1 mL "catheter lock flush" vials. Carefully examine all heparin products to ensure that the proper strength is selected for administration.
Hypersensitivity
Patients with documented hypersensitivity to heparin should be given the drug only in clearly life-threatening situations.
Hemorrhage
Hemorrhage can occur at virtually any site in patients receiving heparin. An unexplained fall in hematocrit, fall in blood pressure, or any other unexplained symptom should lead to serious consideration of a hemorrhagic event.
Heparin sodium should be used with extreme caution in disease states in which there is increased danger of hemorrhage. Some of the conditions in which increased danger of hemorrhage exists are:
Cardiovascular - Subacute bacterial endocarditis. Severe hypertension.
Surgical - During and immediately following (a) spinal tap or spinal anesthesia or (b) major surgery, especially involving the brain, spinal cord, or eye.
Hematologic - Conditions associated with increased bleeding tendencies, such as hemophilia, thrombocytopenia and some vascular purpuras.
Gastrointestinal - Ulcerative lesions and continuous tube drainage of the stomach or small intestine.
Other - Menstruation, liver disease with impaired hemostasis.
Coagulation Testing
When heparin sodium is administered in therapeutic amounts, its dosage should be regulated by frequent blood coagulation tests. If the coagulation test is unduly prolonged or if hemorrhage occurs, heparin sodium should be discontinued promptly (see OVERDOSAGE).
Thrombocytopenia
Thrombocytopenia has been reported to occur in patients receiving heparin with a reported incidence of 0 to 30%. Platelet counts should be obtained at baseline and periodically during heparin administration. Mild thrombocytopenia (count greater than 100,000/mm3) may remain stable or reverse even if heparin is continued. However, thrombocytopenia of any degree should be monitored closely. If the count falls below 100,000/mm3 or if recurrent thrombosis develops (see WARNINGS, Heparin-induced Thrombocytopenia and Heparin-induced Thrombocytopenia and Thrombosis, and PRECAUTIONS, General, White Clot Syndrome), the heparin product should be discontinued, and, if necessary, an alternative anticoagulant administered. If continued heparin therapy is essential, administration of heparin from a different organ source can be reinstituted with caution.
Heparin-induced Thrombocytopenia (HIT) and Heparin-induced Thrombocytopenia and Thrombosis (HITT)
Heparin-induced Thrombocytopenia (HIT) is a serious antibody-mediated reaction resulting from irreversible aggregation of platelets. HIT may progress to the development of venous and arterial thromboses, a condition referred to as Heparin-induced Thrombocytopenia and Thrombosis (HITT). Thrombotic events may also be the initial presentation for HITT. These serious thromboembolic events include deep vein thrombosis, pulmonary embolism, cerebral vein thrombosis, limb ischemia, stroke, myocardial infarction, mesenteric thrombosis, renal arterial thrombosis, skin necrosis, gangrene of the extremities that may lead to amputation, and possibly death. Thrombocytopenia of any degree should be monitored closely. If the platelet count falls below 100,000/mm3 or if recurrent thrombosis develops, the heparin product should be promptly discontinued and alternative anticoagulants considered if patients require continued anticoagulation.
Delayed Onset of HIT and HITT
Heparin-induced Thrombocytopenia and Heparin-induced Thrombocytopenia and Thrombosis can occur up to several weeks after the discontinuation of heparin therapy. Patients presenting with thrombocytopenia or thrombosis after discontinuation of heparin should be evaluated for HIT and HITT.
The administration of intravenous solutions can cause fluid and/or solute overload resulting in dilution of serum electrolyte concentrations, overhydration, congested states or pulmonary edema. The risk of dilutional states is inversely proportional to the electrolyte concentration. The risk of solute overload causing congested states with peripheral and pulmonary edema is directly proportional to the electrolyte concentration.
Solution containing sodium ions should be used with great care, if at all, in patients with congestive heart failure, severe renal insufficiency, and in clinical states in which there is sodium retention with edema. In patients with diminished renal function, administration of solutions containing sodium ions may result in sodium retention.
Excessive administration of potassium-free solutions may result in significant hypokalemia.
Because dosages of this drug are titrated to response (see DOSAGE AND ADMINISTRATION), no additives should be made to Heparin Sodium in 0.9% Sodium Chloride Injection.
Use in Neonates
Carefully examine all heparin drug product containers to confirm choice of the correct strength prior to administration of the drug. Pediatric patients, including neonates, have died as a result of medication errors in which Heparin Sodium Injection vials have been confused with "catheter lock flush" vials. (See WARNINGS, Fatal Medication Errors.)
PRECAUTIONS
General
- a.
-
White Clot Syndrome:
It has been reported that patients on heparin may develop new thrombus formation in association with thrombocytopenia resulting from irreversible aggregation of platelets induced by heparin, the so-called "white clot syndrome." The process may lead to severe thromboembolic complications like skin necrosis, gangrene of the extremities that may lead to amputation, myocardial infarction, pulmonary embolism, stroke, and possibly death. Therefore, heparin administration should be promptly discontinued if a patient develops new thrombosis in association with thrombocytopenia. - b.
-
Heparin Resistance:
Increased resistance to heparin is frequently encountered in fever, thrombosis, thrombophlebitis, infections with thrombosing tendencies, myocardial infarction, cancer and in postsurgical patients. - c.
-
Increased Risk to Older Patients, Especially Women:
A higher incidence of bleeding has been reported in patients, particularly women, over 60 years of age.
Clinical evaluation and periodic laboratory determinations are necessary to monitor changes in fluid balance and electrolyte concentrations during prolonged parenteral therapy or whenever the condition of the patient warrants such evaluation.
Extraordinary electrolyte losses such as may occur during protracted nasogastric suction, vomiting, diarrhea, or gastrointestinal fistula drainage may necessitate additional electrolyte supplementation.
Sodium-containing solutions should be administered with caution to patients receiving corticosteroids or corticotropin, or to other salt-retaining patients. Care should be exercised in administering solutions containing sodium to patients with renal or cardiovascular insufficiency, with or without congestive heart failure, particularly if they are postoperative or elderly.
Do not use plastic container in series connection.
If administration is controlled by a pumping device, care must be taken to discontinue pumping action before the container runs dry or air embolism may result.
These solutions are intended for intravenous administration using sterile equipment. It is recommended that any unused heparin solution and intravenous administration apparatus be replaced at least once every 24 hours.
Use only if solution is clear and container and seals are intact.
Laboratory Tests
Periodic platelet counts, hematocrits, and tests for occult blood in stool are recommended during the entire course of heparin therapy, regardless of the route of administration (see DOSAGE AND ADMINISTRATION).
Drug Interactions
Oral anticoagulants
Heparin sodium may prolong the one-stage prothrombin time. Therefore, when heparin sodium is given with dicumarol or warfarin sodium, a period of at least 5 hours after the last intravenous dose or 24 hours after the last subcutaneous dose should elapse before blood is drawn if a valid prothrombin time is to be obtained.
Platelet inhibitors
Drugs such as acetylsalicylic acid, dextran, phenylbutazone, ibuprofen, indomethacin, dipyridamole, hydroxychloroquine and others that interfere with platelet-aggregation reactions (the main hemostatic defense of heparinized patients) may induce bleeding and should be used with caution in patients receiving heparin sodium.
Other interactions
Digitalis, tetracyclines, nicotine, antihistamines, or IV nitroglycerin may partially counteract the anticoagulant action of heparin sodium.
Drug/Laboratory Tests Interactions
Hyperaminotransferasemia
Significant elevations of aminotransferase AST (SGOT) and ALT (SGPT) levels have occurred in a high percentage of patients (and healthy subjects) who have received heparin. Since aminotransferase determinations are important in the differential diagnosis of myocardial infarction, liver disease, and pulmonary emboli, rises that might be caused by drugs (like heparin) should be interpreted with caution.
Carcinogenesis, Mutagenesis, Impairment of Fertility
Long term studies in animals to evaluate the carcinogenic potential, reproduction studies in animals to determine effects on fertility of males and females, and studies to determine mutagenic potential have not been conducted with Heparin Sodium in Sodium Chloride Injection.
Pregnancy
Teratogenic Effects
Pregnancy Category C
Animal reproduction studies have not been conducted with Heparin Sodium in 0.9% Sodium Chloride Injection. It is also not known whether Heparin Sodium in 0.9% Sodium Chloride Injection can cause fetal harm when administered to a pregnant woman or can affect reproduction capacity. Heparin Sodium in 0.9% Sodium Chloride Injection should be given to a pregnant woman only if clearly needed.
Nonteratogenic Effects
Heparin does not cross the placental barrier.
Nursing Mothers
Heparin is not excreted in human milk.
Pediatric Use
Safety and effectiveness in pediatric patients have not been established.
Geriatric Use
A higher incidence of bleeding has been reported in patients over 60 years of age, especially women (see PRECAUTIONS, General). Clinical studies indicate that lower doses of heparin may be indicated in these patients (see CLINICAL PHARMACOLOGY and DOSAGE AND ADMINISTRATION).
ADVERSE REACTIONS
Hemorrhage
Hemorrhage is the chief complication that may result from heparin therapy (see WARNINGS). An overly prolonged clotting time or minor bleeding during therapy can usually be controlled by withdrawing the drug (see OVERDOSAGE). It should be appreciated that gastrointestinal or urinary tract bleeding during anticoagulant therapy may indicate the presence of an underlying occult lesion. Bleeding can occur at any site but certain specific hemorrhagic complications may be difficult to detect:
- Adrenal hemorrhage, with resultant acute adrenal insufficiency, has occurred during anticoagulant therapy. Therefore, such treatment should be discontinued in patients who develop signs and symptoms of acute adrenal hemorrhage and insufficiency. Initiation of corrective therapy should not depend on laboratory confirmation of the diagnosis, since any delay in an acute situation may result in the patient's death.
- Ovarian (corpus luteum) hemorrhage developed in a number of women of reproductive age receiving short- or long-term anticoagulant therapy. This complication if unrecognized may be fatal.
- Retroperitoneal hemorrhage.
Thrombocytopenia, Heparin-induced Thrombocytopenia (HIT), Heparin-induced Thrombocytopenia and Thrombosis (HITT) and Delayed Onset of HIT and HITT
(See WARNINGS.)
Local Irritation
Local irritation, erythema, mild pain, hematoma or ulceration may follow deep subcutaneous (intrafat) injection of heparin sodium. These complications are much more common after intramuscular use, and such use is not recommended.
Hypersensitivity
Generalized hypersensitivity reactions have been reported, with chills, fever, and urticaria as the most usual manifestations, and asthma, rhinitis, lacrimation, headache, nausea and vomiting, and anaphylactoid reactions, including shock, occurring more rarely. Itching and burning, especially on the plantar site of the feet, may occur.
Thrombocytopenia has been reported to occur in patients receiving heparin with a reported incidence of 0–30%. While often mild and of no obvious clinical significance, such thrombocytopenia can be accompanied by severe thromboembolic complications such as skin necrosis, gangrene of the extremities that may lead to amputation, myocardial infarction, pulmonary embolism, stroke, and possibly death. (See WARNINGS and PRECAUTIONS.)
Certain episodes of painful, ischemic, and cyanosed limbs have in the past been attributed to allergic vasospastic reactions. Whether these are in fact identical to the thrombocytopenia associated complications remains to be determined.
Miscellaneous
Osteoporosis following long-term administration of high-doses of heparin, cutaneous necrosis after systemic administration, suppression of aldosterone synthesis, delayed transient alopecia, priapism, and rebound hyperlipemia on discontinuation of heparin sodium have also been reported.
Significant elevations of aminotransferase AST (SGOT) and ALT (SGPT) levels have occurred in a high percentage of patients (and healthy subjects) who have received heparin.
Reactions which may occur because of the solution or the technique of administration include febrile response, infection at the site of injection, venous thrombosis or phlebitis extending from the site of injection, extravasation, and hypervolemia.
Symptoms may result from an excess or deficit of one or more of the ions present in the solution; therefore, frequent monitoring of electrolyte levels is essential.
Hypernatremia may be associated with edema and exacerbation of congestive heart failure due to the retention of water, resulting in an expanded extracellular fluid volume.
If infused in large amounts, chloride ions may cause a loss of bicarbonate ions, resulting in an acidifying effect.
If an adverse reaction does occur, discontinue the infusion, evaluate the patient, institute appropriate therapeutic countermeasures and save the remainder of the fluid for examination if deemed necessary.
OVERDOSAGE
Symptoms
Bleeding is the chief sign of heparin overdosage. Nosebleeds, blood in urine or tarry stools may be noted as the first sign of bleeding. Easy bruising or petechial formations may precede frank bleeding.
Treatment
Neutralization of heparin effect.
When clinical circumstances (bleeding) require reversal of heparinization, protamine sulfate (1% solution) by slow infusion will neutralize heparin sodium. No more than 50 mg should be administered, very slowly, in any 10 minute period. Each mg of protamine sulfate neutralizes approximately 100 USP Heparin Units. The amount of protamine required decreases over time as heparin is metabolized. Although the metabolism of heparin is complex, it may, for the purpose of choosing a protamine dose, be assumed to have a half-life of about 1/2 hour after intravenous injection.
Administration of protamine sulfate can cause severe hypotensive and anaphylactoid reactions. Because fatal reactions often resembling anaphylaxis have been reported, the drug should be given only when resuscitation techniques and treatment of anaphylactoid shock are readily available.
For additional information the labeling of Protamine Sulfate Injection, USP products should be consulted.
DOSAGE AND ADMINISTRATION
Heparin Sodium is not effective by oral administration and Heparin Sodium in 0.9% Sodium Chloride Injection should not be given orally.
This product should be administered by intravenous infusion. Do not use Heparin Sodium in 0.9% Sodium Chloride Injection as a "catheter lock flush" product.
Confirm the choice of the correct heparin drug product and strength prior to administration of the drug to the patient (see WARNINGS, Fatal Medication Errors). Heparin sodium injection products must not be confused with "catheter lock flush" products.
This product should not be infused under pressure.
Note: Small doses of heparin can alter tests for activated partial thromboplastin time (APTT). A baseline value for APTT should be obtained prior to administration of this solution.
Maintenance of Catheter Patency
Although the rate of infusion of the 2 units/mL formulation is dependent upon the age, weight, clinical condition of the patient, and the procedure being employed, an infusion rate of 3 mL/hour has been found to be satisfactory.
Geriatric Use
Patients over 60 years of age may require lower doses of heparin. (See PRECAUTIONS.)
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
HOW SUPPLIED
Heparin Sodium in 0.9% Sodium Chloride Injection is supplied sterile and nonpyrogenic in Full Fill 500 mL EXCEL® Containers packaged 24 per case.
| NDC | Cat. No. | Size |
|---|---|---|
| Heparin Sodium 1,000 Units in 0.9% Sodium Chloride Injection (Canada DIN 01935933) | ||
| 0264-9872-10 | P8721 | 500 mL |
Exposure of pharmaceutical products to heat should be minimized. Avoid excessive heat. Protect from freezing. It is recommended that the product be stored at room temperature (25°C); however, brief exposure up to 40°C does not adversely affect the product.
Rx only
Revised: July 2008
EXCEL is a registered trademark of B. Braun Medical Inc.
Made in USA
Directions for Use of EXCEL® Container
Do not admix with other drugs.
Caution: Do not use plastic container in series connection.
To Open
Tear overwrap down at notch and remove solution container. Check for minute leaks by squeezing solution container firmly. If leaks are found, discard solution as sterility may be impaired.
| NOTE: | Before use, perform the following checks: |
| Inspect each container. Read the label. Ensure solution is the one ordered and is within the expiration date. |
|
| Invert container and carefully inspect the solution in good light for cloudiness, haze, or particulate matter. Any container which is suspect should not be used. |
|
| Use only if solution is clear and container and seals are intact. |
Preparation for Administration
- Remove plastic protector from sterile set port at bottom of container.
- Attach administration set. Refer to complete directions accompanying set.
B. Braun Medical Inc.
Irvine, CA USA 92614-5895
In Canada, distributed by:
B. Braun Medical Inc.
Scarborough, Ontario M1H 2W4
© 2008 B. Braun Medical Inc.
Y36-002-661
| HEPARIN SODIUM IN SODIUM CHLORIDE
heparin sodium injection |
||||||||||||||||||||||
|
||||||||||||||||||||||
|
||||||||||||||||||||||
|
||||||||||||||||||||||
|
||||||||||||||||||||||
Revised: 08/2008B. Braun Medical Inc.