|
|
||||||||||||||||||||||
FULL PRESCRIBING INFORMATION
WARNING: CARDIOMYOPATHY, INFUSION REACTIONS, AND PULMONARY TOXICITY
Cardiomyopathy
Herceptin can result in sub‑clinical and clinical cardiac failure manifesting as CHF and decreased LVEF. The incidence and severity of left ventricular cardiac dysfunction was highest in patients who received Herceptin concurrently with anthracycline containing chemotherapy regimens.
Evaluate left ventricular function in all patients prior to and during treatment with Herceptin. Discontinue Herceptin treatment in patients receiving adjuvant therapy and strongly consider discontinuation of Herceptin treatment in patients with metastatic breast cancer for clinically significant decrease in left ventricular function. [see Warnings and Precautions ( 5.1) and Dosage and Administration ( 2.2)]
Infusion Reactions; Pulmonary Toxicity
Herceptin administration can result in serious infusion reactions and pulmonary toxicity. Fatal infusion reactions have been reported. In most cases, symptoms occurred during or within 24 hours of administration of Herceptin. Herceptin infusion should be interrupted for patients experiencing dyspnea or clinically significant hypotension. Patients should be monitored until signs and symptoms completely resolve. Discontinue Herceptin for infusion reactions manifesting as anaphylaxis, angioedema, interstitial pneumonitis, or acute respiratory distress syndrome. [see Warnings and Precautions ( 5.2, 5.4)]
1 INDICATIONS AND USAGE
1.1 Adjuvant Breast Cancer
Herceptin is indicated for adjuvant treatment of HER2 overexpressing node positive or node negative (ER/PR negative or with one high risk feature [see Clinical Studies ( 14.1)]) breast cancer
- as part of a treatment regimen consisting of doxorubicin, cyclophosphamide, and either paclitaxel or docetaxel
- with docetaxel and carboplatin
- As a single agent following multi-modality anthracycline based therapy.
1.2 Metastatic Breast Cancer
Herceptin is indicated:
- As a single agent for treatment of HER2‑overexpressing breast cancer in patients who have received one or more chemotherapy regimens for metastatic disease.
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Doses and Schedules
Do not administer as an intravenous push or bolus. Do not mix Herceptin with other drugs
Adjuvant Treatment, Breast Cancer:
Administer according to one of the following doses and schedules for a total of 52 weeks of Herceptin therapy:
During and following paclitaxel, docetaxel, or docetaxel/carboplatin:
- Initial dose of 4mg/kg as an intravenous infusion over 90 minutes then at 2 mg/kg as an intravenous infusion over 30 minutes weekly during chemotherapy for the first 12 weeks (paclitaxel or docetaxel) or 18 weeks (docetaxel/carboplatin).
- One week following the last weekly dose of Herceptin, administer Herceptin at 6 mg/kg as an intravenous infusion over 30‑60 minutes every three weeks.
As a single agent within three weeks following completion of multi‑modality, anthracycline‑based chemotherapy regimens.
- Initial dose at 8 mg/kg as an intravenous infusion over 90 minutes
- Subsequent doses at 6 mg/kg as an intravenous infusion over 30‑minutes every three weeks.
Metastatic Treatment, Breast Cancer:
- Administer Herceptin, alone or in combination with paclitaxel, at an initial dose of 4 mg/kg as a 90 minute intravenous infusion followed by subsequent once weekly doses of 2 mg/kg as 30 minute intravenous infusions until disease progression.
2.2 Dose Modifications
Infusion Reactions
[see Boxed Warning, Warnings and Precautions ( 5.2)]
- Decrease the rate of infusion for mild or moderate infusion reactions
- Interrupt the infusion in patients with dyspnea or clinically significant hypotension
- Discontinue Herceptin for severe or life‑threatening infusion reactions
Cardiomyopathy
[see Boxed Warning, Warnings and Precautions ( 5.1)].
Assess left ventricular ejection fraction (LVEF) prior to initiation of Herceptin and at regular intervals during treatment. Withhold Herceptin dosing for at least 4 weeks for either of the following:
- ≥ 16% absolute decrease in LVEF from pre‑treatment values
- LVEF below institutional limits of normal and ≥ 10% absolute decrease in LVEF from pretreatment values.
Herceptin may be resumed if, within 4—8 weeks, the LVEF returns to normal limits and the absolute decrease from baseline is ≤ 15%.
Permanently discontinue Herceptin for a persistent ( > 8 weeks) LVEF decline or for suspension of Herceptin dosing on more than 3 occasions for cardiomyopathy.
2.3 Preparation for Administration
Reconstitution
Reconstitute each 440 mg vial of Herceptin with 20 mL of Bacteriostatic Water for Injection (BWFI), USP, containing 1.1% benzyl alcohol as a preservative to yield a multi‑dose solution containing 21 mg/mL trastuzumab. In patients with known hypersensitivity to benzyl alcohol, reconstitute with 20 mL of Sterile Water for Injection (SWFI) without preservative to yield a single use solution.
Use appropriate aseptic technique when performing the following reconstitution steps:
- Using a sterile syringe, slowly inject the 20 mL of diluent into the vial containing the lyophilized cake of Herceptin. The stream of diluent should be directed into the lyophilized cake.
- Swirl the vial gently to aid reconstitution. DO NOT SHAKE.
- Slight foaming of the product may be present upon reconstitution. Allow the vial to stand undisturbed for approximately 5 minutes.
- Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit. Inspect visually for particulates and discoloration. The solution should be free of visible particulates, clear to slightly opalescent and colorless to pale yellow.
- Store reconstituted Herceptin at 2—8° C; discard unused Herceptin after 28 days. If Herceptin is reconstituted with SWFI without preservative, use immediately and discard any unused portion.
Dilution
- Determine the dose (mg) of Herceptin [see Dosage and Administration
( 2.1)]. Calculate the volume of the
21 mg/mL reconstituted Herceptin solution needed,
withdraw this amount from the vial and add it to an infusion
bag containing 250 mL of
0.9% Sodium Chloride Injection, USP.
DO NOT USE DEXTROSE (5%) SOLUTION. - Gently invert the bag to mix the solution
3 DOSAGE FORMS AND STRENGTHS
440 mg lyophilized powder per multi‑use vial.
4 CONTRAINDICATIONS
None.
5 WARNINGS AND PRECAUTIONS
5.1 Cardiomyopathy
Herceptin can cause left ventricular cardiac dysfunction, arrhythmias, hypertension, disabling cardiac failure, cardiomyopathy, and cardiac death [see Boxed Warning: Cardiomyopathy]. Herceptin can also cause a symptomatic decline in left ventricular ejection fraction (LVEF).
There is a 4—6 fold increase in the incidence of symptomatic myocardial dysfunction among patients receiving Herceptin as a single agent or in combination therapy compared with those not receiving Herceptin. The highest absolute incidence occurs when Herceptin is administered with an anthracycline.
Withhold Herceptin for ≥ 16% absolute decrease in LVEF from pre‑treatment values or an LVEF value below institutional limits of normal and ≥ 10% absolute decrease in LVEF from pretreatment values. [see Dosage and Administration ( 2.2)] The safety of continuation or resumption of Herceptin in patients with Herceptin‑induced left ventricular cardiac dysfunction has not been studied.
Cardiac Monitoring
Conduct thorough cardiac assessment, including history, physical examination, and determination of LVEF by echocardiogram or MUGA scan. The following schedule is recommended:
- Baseline LVEF measurement immediately prior to initiation of Herceptin
- LVEF measurements every 3 months during and upon completion of Herceptin
- Repeat LVEF measurement at 4 week intervals if Herceptin is withheld for significant left ventricular cardiac dysfunction [ see Dosage and Administration ( 2.2)]
- LVEF measurements every 6 months for at least 2 years following completion of Herceptin as a component of adjuvant therapy.
In Study 1, 16% (136/844) of patients discontinued Herceptin due to clinical evidence of myocardial dysfunction or significant decline in LVEF. In Study 3, the number of patients who discontinued Herceptin due to cardiac toxicity was 2.6% (44/1678). In Study 4, a total of 2.9% (31/1056) patients in the TCH arm (1.5% during the chemotherapy phase and 1.4% during the monotherapy phase) and 5.7% (61/1068) patients in the AC‑TH arm (1.5% during the chemotherapy phase and 4.2% during the monotherapy phase) discontinued Herceptin due to cardiac toxicity.
Among 32 patients receiving adjuvant chemotherapy (Studies 1 and 2) who developed congestive heart failure, one patient died of cardiomyopathy and all other patients were receiving cardiac medication at last follow‑up. Approximately half of the surviving patients had recovery to a normal LVEF (defined as ≥50%) on continuing medical management at the time of last follow‑up. Incidence of congestive heart failure is presented in Table 1. The safety of continuation or resumption of Herceptin in patients with Herceptin‑induced left ventricular cardiac dysfunction has not been studied.
| Incidence of CHF | |||
|---|---|---|---|
| Study | Regimen | Herceptin | Control |
| 1 & 2* | AC† → Paclitaxel+Herceptin | 2% (32/1677) | 0.4% (7/1600) |
| 3 | Chemo → Herceptin | 2% (30/1678) | 0.3% (5/1708) |
| 4 | AC† → Docetaxel+Herceptin | 2% (20/1068) | 0.3% (3/1050) |
| 4 | Docetaxel+Carbo+Herceptin | 0.4% (4/1056) | 0.3% (3/1050) |
| Incidence | |||||
|---|---|---|---|---|---|
| NYHA I‑IV | NYHA III‑IV | ||||
| Study | Event | Herceptin | Control | Herceptin | Control |
| 5 (AC)† | Cardiac Dysfunction | 28% | 7% | 19% | 3% |
| 5 (paclitaxel) | Cardiac Dysfunction | 11% | 1% | 4% | 1% |
| 6 | Cardiac Dysfunction‡ | 7% | N/A | 5% | N/A |
In Study 4, the incidence of NCI‑CTC Grade 3/4 cardiac ischemia/infarction was higher in the Herceptin containing regimens: (AC‑TH: 0.3% (3/1068) and TCH 0.2% (: 2/1056)) as compared to none in AC‑T.
5.2 Infusion Reactions
Infusion reactions consist of a symptom complex characterized by fever and chills, and on occasion included nausea, vomiting, pain (in some cases at tumor sites), headache, dizziness, dyspnea, hypotension, rash, and asthenia [see Adverse Reactions ( 6.1)].
In postmarketing reports, serious and fatal infusion reactions have been reported. Severe reactions which include bronchospasm, anaphylaxis, angioedema, hypoxia, and severe hypotension, were usually reported during or immediately following the initial infusion. However, the onset and clinical course were variable including progressive worsening, initial improvement followed by clinical deterioration, or delayed post‑infusion events with rapid clinical deterioration. For fatal events, death occurred within hours to days following a serious infusion reaction
Interrupt Herceptin infusion in all patients experiencing dyspnea, clinically significant hypotension, and intervention of medical therapy administered, which may include: epinephrine, corticosteroids, diphenhydramine, bronchodilators, and oxygen. Patients should be evaluated and carefully monitored until complete resolution of signs and symptoms. Permanent discontinuation should be strongly considered in all patients with severe infusion reactions.
There are no data regarding the most appropriate method of identification of patients who may safely be retreated with Herceptin after experiencing a severe infusion reaction. Prior to resumption of Herceptin infusion, the majority of patients who experienced a severe infusion reaction were pre‑medicated with antihistamines and/or corticosteroids. While some patients tolerated Herceptin infusions, others had recurrent severe infusion reactions despite pre‑medications.
5.3 Exacerbation of Chemotherapy‑Induced Neutropenia
In randomized, controlled clinical trials in women with metastatic breast cancer, the per‑patient incidences of NCI CTC Grade 3—4 neutropenia and of febrile neutropenia were higher in patients receiving Herceptin in combination with myelosuppressive chemotherapy as compared to those who received chemotherapy alone. The incidence of septic death was not significantly increased. [ see Adverse Reactions ( 6.1)].
5.4 Pulmonary Toxicity
Herceptin use can result in serious and fatal pulmonary toxicity. Pulmonary toxicity includes dyspnea, interstitial pneumonitis, pulmonary infiltrates, pleural effusions, non‑cardiogenic pulmonary edema, pulmonary insufficiency and hypoxia, acute respiratory distress syndrome, and pulmonary fibrosis. Such events can occur as sequelae of infusion reactions [see Warnings and Precautions ( 5.2)]. Patients with symptomatic intrinsic lung disease or with extensive tumor involvement of the lungs, resulting in dyspnea at rest, appear to have more severe toxicity.
5.5 HER2 Testing
Detection of HER2 protein overexpression is necessary for selection of patients appropriate for Herceptin therapy because these are the only patients studied and for whom benefit has been shown. Assessment for HER2 overexpression and of HER2 gene amplification should be performed by laboratories with demonstrated proficiency in the specific technology being utilized. Improper assay performance, including use of suboptimally fixed tissue, failure to utilize specified reagents, deviation from specific assay instructions, and failure to include appropriate controls for assay validation, can lead to unreliable results.
Several FDA‑approved commercial assays are available to aid in the selection of patients for Herceptin therapy. These include HercepTest™ and Pathway® HER‑2/neu (IHC assays) and PathVysion® and HER2 FISH pharmDx™ (FISH assays). Users should refer to the package inserts of specific assay kits for information on the validation and performance of each assay.
Limitations in assay precision (particularly for the IHC method) and in the direct linkage between assay result and overexpression of the Herceptin target (for the FISH method) make it inadvisable to rely on a single method to rule out potential Herceptin benefit. A negative FISH result does not rule out HER2 overexpression and potential benefit from Herceptin. Treatment outcomes for metastatic breast cancer (Study 5) as a function of IHC and FISH testing are provided in Table 9. Treatment outcomes for adjuvant breast cancer (Studies 2 and 3) as a function of IHC and FISH testing are provided in Table 7.
HER2 Protein Overexpression Detection Methods
HER2 protein overexpression can be established by measuring HER2 protein using an IHC method. HercepTest®, one test approved for this use, was assessed for concordance with the Clinical Trial Assay (CTA), using tumor specimens collected and stored independently from those obtained in Herceptin clinical studies in women with metastatic breast cancer. Data are provided in the package insert for HercepTest®.
HER2 Gene Amplification Detection Method
The presence of HER2 protein overexpression and gene amplification are highly correlated, therefore the use of FISH to detect gene amplification may be employed for selection of patients appropriate for Herceptin therapy. PathVysion®, one test approved for this use, was evaluated in an exploratory, retrospective assessment of available CTA 2+ or 3+ tumor specimens collected as part of patient screening for clinical studies in metastatic breast cancer (Studies 5 and 6). Data are provided in the package insert for PathVysion®.
5.6 Embryo‑Fetal Toxicity (Pregnancy Category D)
Herceptin can cause fetal harm when administered to a pregnant woman. Post‑marketing case reports suggest that Herceptin use during pregnancy increases the risk of oligohydramnios during the second and third trimesters. If Herceptin is used during pregnancy or if a woman becomes pregnant while taking Herceptin, she should be apprised of the potential hazard to a fetus. [ see Use in Specific Populations ( 8.1)].
6 ADVERSE REACTIONS
The following adverse reactions are discussed in greater detail in other sections of the label:
- Cardiomyopathy [ see Warnings and Precautions ( 5.1)]
- Infusion reactions [see Warnings and Precautions ( 5.2)]
- Exacerbation of chemotherapy‑induced neutropenia [see Warnings and Precautions ( 5.3)]
- Pulmonary toxicity [see Warnings and Precautions (5.4)]
The most common adverse reactions in patients receiving Herceptin are fever, nausea, vomiting, infusion reactions, diarrhea, infections, increased cough, headache, fatigue, dyspnea, rash, neutropenia, anemia, and myalgia. Adverse reactions requiring interruption or discontinuation of Herceptin treatment include CHF, significant decline in left ventricular cardiac function, severe infusion reactions, and pulmonary toxicity [see Dosage and Administration (2.2)].
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Adjuvant Breast Cancer Studies
The data below reflect exposure to Herceptin across three randomized, open‑label studies, Studies 1, 2, and 3, with (n= 3355) or without (n= 3308) trastuzumab in the adjuvant treatment of breast cancer.
The data summarized in Table 3 below, from Study 3, reflect exposure to Herceptin in 1678 patients; the median treatment duration was 51 weeks and median number of infusions was 18. Among the 3386 patients enrolled in Study 3, the median age was 49 years (range: 21 to 80 years), 83% of patients were Caucasian, and 13% were Asian.
| MedDRA (v. 7.1) | 1 Year Herceptin | Observation |
|---|---|---|
| Adverse Event Preferred Term | (n=1678) | (n=1708) |
| Cardiac | ||
| Hypertension | 64 (4%) | 35 (2%) |
| Dizziness | 60 (4%) | 29 (2%) |
| Ejection Fraction Decreased | 58 (3.5%) | 11 (0.6%) |
| Palpitations | 48 (3%) | 12 (0.7%) |
| Cardiac Arrhythmias† | 40 (3%) | 17 (1%) |
| Cardiac Failure Congestive | 30 (2%) | 5 (0.3%) |
| Cardiac Failure | 9 (0.5%) | 4 (0.2%) |
| Cardiac Disorder | 5 (0.3%) | 0 (0%) |
| Ventricular Dysfunction | 4 (0.2%) | 0 (0%) |
| Respiratory Thoracic Mediastinal Disorders | ||
| Nasopharyngitis | 135 (8%) | 43 (3%) |
| Cough | 81 (5%) | 34 (2%) |
| Influenza | 70 (4%) | 9 (0.5%) |
| Dyspnea | 57 (3%) | 26 (2%) |
| URI | 46 (3%) | 20 (1%) |
| Rhinitis | 36 (2%) | 6 (0.4%) |
| Pharyngolaryngeal Pain | 32 (2%) | 8 (0.5%) |
| Sinusitis | 26 (2%) | 5 (0.3%) |
| Epistaxis | 25 (2%) | 1 (0.06%) |
| Pulmonary Hypertension | 4 (0.2%) | 0 (0%) |
| Interstitial Pneumonitis | 4 (0.2%) | 0 (0%) |
| Gastrointestinal Disorders | ||
| Diarrhea | 123 (7%) | 16 (1%) |
| Nausea | 108 (6%) | 19 (1%) |
| Vomiting | 58 (3.5%) | 10 (0.6%) |
| Constipation | 33 (2%) | 17 (1%) |
| Dyspepsia | 30 (2%) | 9 (0.5%) |
| Upper Abdominal Pain | 29 (2%) | 15 (1%) |
| Musculoskeletal & Connective Tissue Disorders | ||
| Arthralgia | 137 (8%) | 98 (6%) |
| Back Pain | 91 (5%) | 58 (3%) |
| Myalgia | 63 (4%) | 17 (1%) |
| Bone Pain | 49 (3%) | 26 (2%) |
| Muscle Spasm | 46 (3%) | 3 (0.2%) |
| Nervous System Disorders | ||
| Headache | 162 (10%) | 49 (3%) |
| Paraesthesia | 29 (2%) | 11 (0.6%) |
| Skin & Subcutaneous Tissue Disorders | ||
| Rash | 70 (4%) | 10 (0.6%) |
| Nail Disorders | 43 (2%) | 0 (0%) |
| Pruritis | 40 (2%) | 10 (0.6%) |
| General disorders | ||
| Pyrexia | 100 (6%) | 6 (0.4%) |
| Edema Peripheral | 79 (5%) | 37 (2%) |
| Chills | 85 (5%) | 0 (0%) |
| Aesthenia | 75 (4.5%) | 30 (2%) |
| Influenza‑like Illness | 40 (2%) | 3 (0.2%) |
| Sudden Death | 1 (0.06%) | 0 (0%) |
| Infections | ||
| Nasopharyngitis | 135 (8%) | 43 (3%) |
| UTI | 39 (3%) | 13 (0.8%) |
| Immune System Disorders | ||
| Hypersensitivity | 10 (0.6%) | 1 (0.06%) |
| Autoimmune Thyroiditis | 4 (0.3%) | 0 (0%) |
The data from Studies 1 and 2 were obtained from 3206 patients enrolled, of which 1635 patients received Herceptin; the median treatment duration was 50 weeks. The median age was 49.0 years (range: 24—80); 84% of patients were White, and 7% were Black, 4% were Hispanic, and 4% were Asian.
In Study 1, only Grade 3—5 adverse events, treatment‑related Grade 2 events, and Grade 2—5 dyspnea were collected during and for up to 3 months following protocol‑specified treatment. The following non‑cardiac adverse reactions of Grade 2—5 occurred at an incidence of at least 2% greater among patients randomized to Herceptin plus chemotherapy as compared to chemotherapy alone: arthralgia (31% vs. 28%), fatigue (28% vs. 22%), infection (22% vs. 14%), hot flashes (17% vs. 15%), anemia (13% vs. 7%), dyspnea (12% vs. 4%), rash/desquamation (11% vs. 7%), neutropenia (7% vs. 5%), headache (6% vs. 4%), and insomnia (3.7% vs. 1.5%). The majority of these events were Grade 2 in severity.
In Study 2, data collection was limited to the following investigator‑attributed treatment‑related adverse reactions NCI‑CTC Grade 4 and 5 hematologic toxicities, Grade 3—5 non‑hematologic toxicities, selected Grade 2—5 toxicities associated with taxanes (myalgia, arthralgias, nail changes, motor neuropathy, sensory neuropathy) and Grade 1—5 cardiac toxicities occurring during chemotherapy and/or Herceptin treatment. The following non‑cardiac adverse reactions of Grade 2—5 occurred at an incidence of at least 2% greater among patients randomized to Herceptin plus chemotherapy as compared to chemotherapy alone: arthralgia (11% vs. 8.4%), myalgia (10% vs. 8%), nail changes (9% vs. 7%), and dyspnea (2.5% vs. 0.1%). The majority of these events were Grade 2 in severity.
Safety data from Study 4 reflect exposure to Herceptin as part of an adjuvant treatment regimen from 2124 patients receiving at least one dose of study treatment [AC‑TH: n = 1068; TCH: n = 1056]. The overall median treatment duration was 54 weeks in both the AC‑TH and TCH arms. The median number of infusions was 26 in the AC‑TH arm and 30 in the TCH arm, including weekly infusions during the chemotherapy phase and every three week dosing in the monotherapy period. Among these patients, the median age was 49 years (range 22 to 74 years). In Study 4, the toxicity profile was similar to that reported in Studies 1, 2, and 3 with the exception of a low incidence of CHF in the TCH arm .
Metastatic Breast Cancer Studies
The data below reflect exposure to Herceptin in one randomized, open‑label study, Study 5, of chemotherapy with (n=235) or without (n=234) trastuzumab in patients with metastatic breast cancer, and one single‑arm study (Study 6; n=222) in patients with metastatic breast cancer. Data in Table 5 are based on Studies 5 and 6.
Among the 464 patients treated in Study 5, the median age was 52 years (range: 25—77 years). Eighty‑nine percent were White, 5% Black, 1% Asian and 5% other racial/ethnic groups. All patients received 4 mg/kg initial dose of Herceptin followed by 2 mg/kg weekly. The percentages of patients who received Herceptin treatment for ≥ 6 months and ≥ 12 months were 58% and 9%, respectively.
Among the 352 patients treated in single agent studies (213 patients from Study 6), the median age was 50 years (range 28—86 years), 100% had breast cancer, 86% were White, 3% were Black, 3% were Asian, and 8% in other racial/ethnic groups. Most of the patients received 4 mg/kg initial dose of Herceptin followed by 2 mg/kg weekly. The percentages of patients who received Herceptin treatment for ≥ 6 months and ≥ 12 months were 31% and 16%, respectively.
| Single Agent* n = 352 | Herceptin +
Paclitaxel n = 91 | Paclitaxel
Alone n = 95 | Herceptin +
AC†
n = 143 | AC†
Alone n = 135 |
||
| Body as a Whole | ||||||
| Pain | 47 | 61 | 62 | 57 | 42 | |
| Asthenia | 42 | 62 | 57 | 54 | 55 | |
| Fever | 36 | 49 | 23 | 56 | 34 | |
| Chills | 32 | 41 | 4 | 35 | 11 | |
| Headache | 26 | 36 | 28 | 44 | 31 | |
| Abdominal pain | 22 | 34 | 22 | 23 | 18 | |
| Back pain | 22 | 34 | 30 | 27 | 15 | |
| Infection | 20 | 47 | 27 | 47 | 31 | |
| Flu syndrome | 10 | 12 | 5 | 12 | 6 | |
| Accidental injury | 6 | 13 | 3 | 9 | 4 | |
| Allergic reaction | 3 | 8 | 2 | 4 | 2 | |
| Cardiovascular | ||||||
| Tachycardia | 5 | 12 | 4 | 10 | 5 | |
| Congestive heart failure | 7 | 11 | 1 | 28 | 7 | |
| Digestive | ||||||
| Nausea | 33 | 51 | 9 | 76 | 77 | |
| Diarrhea | 25 | 45 | 29 | 45 | 26 | |
| Vomiting | 23 | 37 | 28 | 53 | 49 | |
| Nausea and vomiting | 8 | 14 | 11 | 18 | 9 | |
| Anorexia | 14 | 24 | 16 | 31 | 26 | |
| Heme & Lymphatic | ||||||
| Anemia | 4 | 14 | 9 | 36 | 26 | |
| Leukopenia | 3 | 24 | 17 | 52 | 34 | |
| Metabolic | ||||||
| Peripheral edema | 10 | 22 | 20 | 20 | 17 | |
| Edema | 8 | 10 | 8 | 11 | 5 | |
| Musculoskeletal | ||||||
| Bone pain | 7 | 24 | 18 | 7 | 7 | |
| Arthralgia | 6 | 37 | 21 | 8 | 9 | |
| Nervous | ||||||
| Insomnia | 14 | 25 | 13 | 29 | 15 | |
| Dizziness | 13 | 22 | 24 | 24 | 18 | |
| Paresthesia | 9 | 48 | 39 | 17 | 11 | |
| Depression | 6 | 12 | 13 | 20 | 12 | |
| Peripheral neuritis | 2 | 23 | 16 | 2 | 2 | |
| Neuropathy | 1 | 13 | 5 | 4 | 4 | |
| Respiratory | ||||||
| Cough increased | 26 | 41 | 22 | 43 | 29 | |
| Dyspnea | 22 | 27 | 26 | 42 | 25 | |
| Rhinitis | 14 | 22 | 5 | 22 | 16 | |
| Pharyngitis | 12 | 22 | 14 | 30 | 18 | |
| Sinusitis | 9 | 21 | 7 | 13 | 6 | |
| Skin | ||||||
| Rash | 18 | 38 | 18 | 27 | 17 | |
| Herpes simplex | 2 | 12 | 3 | 7 | 9 | |
| Acne | 2 | 11 | 3 | 3 | < 1 | |
| Urogenital | ||||||
| Urinary tract infection | 5 | 18 | 14 | 13 | 7 | |
The following subsections provide additional detail regarding adverse reactions observed in clinical trials of adjuvant breast, metastatic breast cancer, or post‑marketing experience.
Cardiomyopathy
Serial measurement of cardiac function (LVEF) was obtained in clinical trials in the adjuvant treatment of breast cancer. In Study 3, the median duration of follow‑up was 12.6 months (12.4 months in the observation arm; 12.6 months in the 1‑year Herceptin arm); and in Studies 1 and 2, 23 months in the AC‑T arm, 24 months in the AC‑TH arm. In Studies 1 and 2, 6% of patients were not permitted to initiate Herceptin following completion of AC chemotherapy due to cardiac dysfunction (LVEF < 50% or ≥ 15 point decline in LVEF from baseline to end of AC). Following initiation of Herceptin therapy, the incidence of new‑onset dose‑limiting myocardial dysfunction was higher among patients receiving Herceptin and paclitaxel as compared to those receiving paclitaxel alone in Studies 1 and 2, and in patients receiving Herceptin monotherapy compared to observation in Study 3 (see Table 5, Figures 1 and 2).
| LVEF <50% and Absolute Decrease from Baseline | Absolute LVEF Decrease | ||||
|---|---|---|---|---|---|
| LVEF <50% | ≥10% decrease | ≥16% decrease | <20% and ≥10% | ≥20% | |
|
|||||
| Studies 1 & 2† | |||||
| AC→TH (n=1606) | 22.8% (366) | 18.3% (294) | 11.7% (188) | 33.4% (536) | 9.2% (148) |
| AC→T (n=1488) | 9.1% (136) | 5.4% (81) | 2.2% (33) | 18.3% (272) | 2.4% (36) |
| Study 3 | |||||
| Herceptin (n=1678) | 8.6 (144) | 7.0% (118) | 3.8% (64) | 22.4% (376) | 3.5% (59) |
| Observation (n=1708) | 2.7% (46) | 2.0% (35) | 1.2% (20) | 11.9% (204) | 1.2% (21) |
| Study 4 ‡ | |||||
| TCH (n=1056) | 8.5% (90) | 5.9% (62) | 3.3% (35) | 34.5% (364) | 6.3% (67) |
| AC→TH (n=1068) | 17% (182) | 13.3% (142) | 9.8% (105) | 44.3% (473) | 13.2% (141) |
| AC→T (n=1050) | 9.5% (100) | 6.6% (69) | 3.3% (35) | 34% (357) | 5.5% (58) |
| Figure 1:
Studies 1 and 2: Cumulative Incidence of Time to First LVEF Decline of ≥ 10 Percentage Points from Baseline and to Below 50% with Death as a Competing Risk Event |
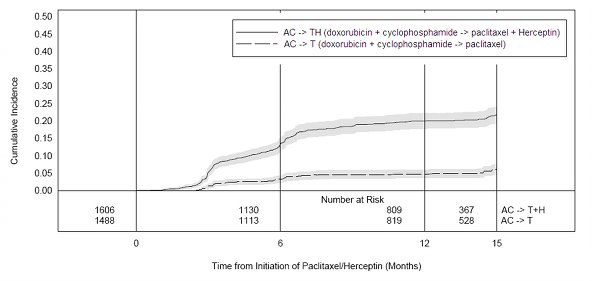 |
| Time 0 is initiation of paclitaxel or Herceptin + paclitaxel therapy. |
| Figure
2:
Study 3: Cumulative Incidence of Time to First LVEF Decline of ≥ 10 Percentage Points from Baseline and to Below 50% with Death as a Competing Risk Event |
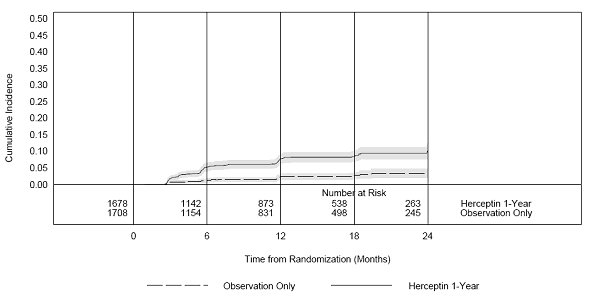 |
| Time 0 is the date of randomization. |
| Figure 3:
Study 4: Cumulative Incidence of Time to First LVEF Decline of ≥10 Percentage Points from Baseline and to Below 50% with Death as a Competing Risk Event |
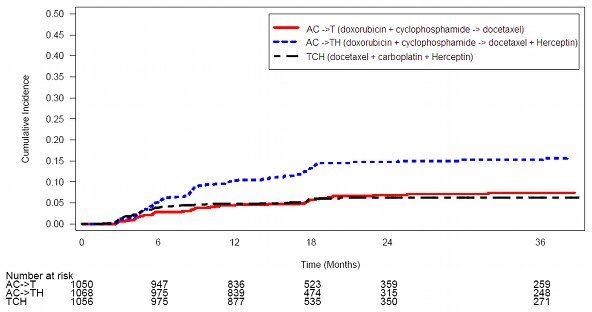 |
| Time 0 is the date of randomization. |
The incidence of treatment emergent congestive heart failure among patients in the metastatic breast cancer trials was classified for severity using the New York Heart Association classification system (I‑IV, where IV is the most severe level of cardiac failure) (see Table 2). In the metastatic breast cancer trials the probability of cardiac dysfunction was highest in patients who received Herceptin concurrently with anthracyclines.
Infusion Reactions
During the first infusion with Herceptin, the symptoms most commonly reported were chills and fever, occurring in approximately 40% of patients in clinical trials. Symptoms were treated with acetaminophen, diphenhydramine, and meperidine (with or without reduction in the rate of Herceptin infusion); permanent discontinuation of Herceptin for infusional toxicity was required in < 1% of patients. Other signs and/or symptoms may include nausea, vomiting, pain (in some cases at tumor sites), rigors, headache, dizziness, dyspnea, hypotension, elevated blood pressure, rash, and asthenia. Infusional toxicity occurred in 21% and 35% of patients, and was severe in 1.4% and 9% of patients, on second or subsequent Herceptin infusions administered as monotherapy or in combination with chemotherapy, respectively. In the post‑marketing setting, severe infusion reactions, including hypersensitivity, anaphylaxis, and angioedema have been reported.
Anemia
In randomized controlled clinical trials, the overall incidence of anemia (30% vs. 21% [Study 5]), of selected NCI‑CTC Grade 2—5 anemia (12.5% vs. 6.6% [Study 1]), and of anemia requiring transfusions (0.1% vs. 0 patients [Study 2]) were increased in patients receiving Herceptin and chemotherapy compared with those receiving chemotherapy alone. Following the administration of Herceptin as a single agent (Study 6), the incidence of NCI‑CTC Grade 3 anemia was < 1%.
Neutropenia
In randomized controlled clinical trials in the adjuvant setting, the incidence of selected NCI‑CTC Grade 4—5 neutropenia (2% vs. 0.7% [Study 2]) and of selected Grade 2—5 neutropenia (7.1% vs. 4.5% [Study 1]) were increased in patients receiving Herceptin and chemotherapy compared with those receiving chemotherapy alone. In a randomized, controlled trial in patients with metastatic breast cancer, the incidences of NCI‑CTC Grade 3/4 neutropenia (32% vs. 22%) and of febrile neutropenia (23% vs. 17%) were also increased in patients randomized to Herceptin in combination with myelosuppressive chemotherapy as compared to chemotherapy alone.
Infection
The overall incidences of infection (46% vs. 30% [Study 5]), of selected NCI‑CTC Grade 2—5 infection/febrile neutropenia (22% vs. 14% [Study 1]) and of selected Grade 3—5 infection/febrile neutropenia (3.3% vs. 1.4%) [Study 2]), were higher in patients receiving Herceptin and chemotherapy compared with those receiving chemotherapy alone. The most common site of infections in the adjuvant setting involved the upper respiratory tract, skin, and urinary tract.
In study 4, the overall incidence of infection was higher with the addition of Herceptin to AC‑T but not to TCH [44% (AC‑TH), 37% (TCH), 38% (AC‑T)]. The incidences of NCI‑CTC grade 3‑4 infection were similar [25% (AC‑TH), 21% (TCH), 23% (AC‑T)] across the three arms.
In a randomized, controlled trial in treatment of metastatic breast cancer, the reported incidence of febrile neutropenia was higher (23% vs. 17%) in patients receiving Herceptin in combination with myelosuppressive chemotherapy as compared to chemotherapy alone.
Pulmonary Toxicity
Adjuvant Breast Cancer
Among women receiving adjuvant therapy for breast cancer, the incidence of selected NCI‑CTC Grade 2—5 pulmonary toxicity (14% vs. 5% [Study 1]) and of selected NCI‑CTC Grade 3—5 pulmonary toxicity and spontaneous reported Grade 2 dyspnea (3.4% vs. 1% [Study 2]) was higher in patients receiving Herceptin and chemotherapy compared with chemotherapy alone. The most common pulmonary toxicity was dyspnea (NCI‑CTC Grade 2—5: 12% vs. 4% [Study 1]; NCI‑CTC Grade 2—5: 2.5% vs. 0.1% [Study 2]).
Pneumonitis/pulmonary infiltrates occurred in 0.7% of patients receiving Herceptin compared with 0.3% of those receiving chemotherapy alone. Fatal respiratory failure occurred in 3 patients receiving Herceptin, one as a component of multi‑organ system failure, as compared to 1 patient receiving chemotherapy alone.
In Study 3, there were 4 cases of interstitial pneumonitis in Herceptin‑treated patients compared to none in the control arm.
Metastatic Breast Cancer
Among women receiving Herceptin for treatment of metastatic breast cancer, the incidence of pulmonary toxicity was also increased. Pulmonary adverse events have been reported in the post‑marketing experience as part of the symptom complex of infusion reactions. Pulmonary events include bronchospasm, hypoxia, dyspnea, pulmonary infiltrates, pleural effusions, non‑cardiogenic pulmonary edema, and acute respiratory distress syndrome. For a detailed description, see Warnings and Precautions ( 5.4).
Thrombosis/Embolism
In 4 randomized, controlled clinical trials, the incidence of thrombotic adverse events was higher in patients receiving Herceptin and chemotherapy compared to chemotherapy alone in three studies (3.0% vs. 1.3% [Study 1], 2.5% and 3.7% vs. 2.2% [Study 4] and 2.1% vs. 0% [Study 5]).
Diarrhea
Among women receiving adjuvant therapy for breast cancer, the incidence of NCI‑CTC Grade 2–5 diarrhea (6.2% vs. 4.8% [Study 1]) and of NCI‑CTC Grade 3–5 diarrhea (1.6% vs. 0% [Study 2]), and of grade 1–4 diarrhea (7% vs. 1% [Study 3]) were higher in patients receiving Herceptin as compared to controls. In Study 4, the incidence of Grade 3–4 diarrhea was higher [5.7% AC-TH, 5.5% TCH vs. 3.0% AC-T] and of Grade 1–4 was higher [51% AC-TH, 63% TCH vs. 43% AC-T] among women receiving Herceptin. Of patients receiving Herceptin as a single agent for the treatment of metastatic breast cancer, 25% experienced diarrhea. An increased incidence of diarrhea was observed in patients receiving Herceptin in combination with chemotherapy for treatment of metastatic breast cancer.
Glomerulopathy
In the postmarketing setting, rare cases of nephrotic syndrome with pathologic evidence of glomerulopathy have been reported. The time to onset ranged from 4 months to approximately 18 months from initiation of Herceptin therapy. Pathologic findings included membranous glomerulonephritis, focal glomerulosclerosis, and fibrillary glomerulonephritis. Complications included volume overload and congestive heart failure.
6.2 Immunogenicity
As with all therapeutic proteins, there is a potential for immunogenicity. Among 903 women with metastatic breast cancer, human anti human antibody (HAHA) to Herceptin was detected in one patient using an enzyme‑linked immunosorbent assay (ELISA). This patient did not experience an allergic reaction. Samples for assessment of HAHA were not collected in studies of adjuvant breast cancer.
The incidence of antibody formation is highly dependent on the sensitivity and the specificity of the assay. Additionally, the observed incidence of antibody (including neutralizing antibody) positivity in an assay may be influenced by several factors including assay methodology, sample handling, timing of sample collection, concomitant medications, and underlying disease. For these reasons, comparison of the incidence of antibodies to Herceptin with the incidence of antibodies to other products may be misleading.
6.3 Post‑Marketing Experience
The following adverse reactions have been identified during post approval use of Herceptin. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
∙ Infusion reaction [see Warnings and Precautions ( 5.2)]
∙ Oligohydramnios [see Warnings and Precautions ( 5.6)]
∙ Glomerulopathy
7 DRUG INTERACTIONS
In clinical studies, administration of paclitaxel in combination with Herceptin resulted in a 1.5‑fold increase in trastuzumab serum levels [see Clinical Pharmacology ( 12)].
In drug interaction studies, the pharmacokinetics of docetaxel and paclitaxel were not altered when each was administered in combination with Herceptin.
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Teratogenic Effects: Category D [see Warnings and Precautions ( 5.6)]
Herceptin can cause fetal harm when administered to a pregnant woman. Post‑marketing case reports suggest that Herceptin use during pregnancy increases the risk for oligohydramnios during the second and third trimester. If Herceptin is used during pregnancy or if a woman becomes pregnant while taking Herceptin, she should be apprised of the potential hazard to a fetus.
In the postmarketing setting, oligohydramnios was reported in women who received Herceptin during pregnancy, either alone or in combination with chemotherapy. In half of these women, amniotic fluid index increased after Herceptin was stopped. In one case, Herceptin was resumed after the amniotic fluid index improved, and oligohydramnios recurred.
Women using Herceptin during pregnancy should be monitored for oligohydramnios. If oligohydramnios occurs, fetal testing should be done that is appropriate for gestational age and consistent with community standards of care. Additional intravenous (IV) hydration has been helpful when oligohydramnios has occurred following administration of other chemotherapy agents, however the effects of additional IV hydration with Herceptin treatment are not known.
Reproduction studies in cynomolgus monkeys at doses up to 25 times the recommended weekly human dose of 2 mg/kg trastuzumab and have revealed no evidence of harm to the fetus. However, HER2 protein expression is high in many embryonic tissues including cardiac and neural tissues; in mutant mice lacking HER2, embryos died in early gestation. Placental transfer of trastuzumab during the early (Days 20—50 of gestation) and late (Days 120—150 of gestation) fetal development period was observed in monkeys. [ See Nonclinical Toxicology ( 13.2)]
Because animal reproduction studies are not always predictive of human response, Herceptin should be used during pregnancy only if the potential benefit to the mother justifies the potential risk to the fetus.
Registry
Pregnant women with breast cancer who are using Herceptin are encouraged to enroll in the Cancer and Childbirth Registry: phone 1‑800‑690‑6720.
8.3 Nursing Mothers
It is not known whether Herceptin is excreted in human milk, but human IgG is excreted in human milk. Published data suggest that breast milk antibodies do not enter the neonatal and infant circulation in substantial amounts.
Trastuzumab was present in the breast milk of lactating cynomolgus monkeys given 12.5 times the recommended weekly human dose of 2 mg/kg of Herceptin. Infant monkeys with detectable serum levels of trastuzumab did not have any adverse effects on growth or development from birth to 3 months of age; however, trastuzumab levels in animal breast milk may not accurately reflect human breast milk levels.
Because many drugs are secreted in human milk and because of the potential for serious adverse reactions in nursing infants from Herceptin, a decision should be made whether to discontinue nursing, or discontinue drug, taking into account the elimination half‑life of trastuzumab and the importance of the drug to the mother.
8.4 Pediatric Use
The safety and effectiveness of Herceptin in pediatric patients has not been established.
8.5 Geriatric Use
Herceptin has been administered to 386 patients who were 65 years of age or over (253 in the adjuvant treatment and 133 in metastatic breast cancer treatment settings). The risk of cardiac dysfunction was increased in geriatric patients as compared to younger patients in both those receiving treatment for metastatic disease in Studies 5 and 6, or adjuvant therapy in Studies 1 and 2. Limitations in data collection and differences in study design of the 4 studies of Herceptin in adjuvant treatment of breast cancer preclude a determination of whether the toxicity profile of Herceptin in older patients is different from younger patients. The reported clinical experience is not adequate to determine whether the efficacy improvements (ORR, TTP, OS, DFS) of Herceptin treatment in older patients is different from that observed in patients <65 years of age for metastatic disease and adjuvant treatment.
10 OVERDOSAGE
There is no experience with overdosage in human clinical trials. Single doses higher than 8 mg/kg have not been tested.
11 DESCRIPTION
Herceptin (trastuzumab) is a humanized IgG1 kappa monoclonal antibody that selectively binds with high affinity to the extracellular domain of the human epidermal growth factor receptor 2 protein, HER2. Trastuzumab is produced by recombinant DNA technology in a mammalian cell (Chinese Hamster Ovary) culture containing the antibiotic gentamicin. Gentamicin is not detectable in the final product.
Herceptin is a sterile, white to pale yellow, preservative‑free lyophilized powder for intravenous administration. Each multi‑use vial of Herceptin contains 440 mg trastuzumab, 400 mg α,α‑trehalose dihydrate, 9.9 mg L‑histidine HCl, 6.4 mg L‑histidine, and 1.8 mg polysorbate 20, USP. Reconstitution with 20 mL of the appropriate diluent (BWFI or SWFI) yields a solution containing 21 mg/mL trastuzumab, at a pH of approximately 6.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
The HER2 (or c‑erbB2) proto‑oncogene encodes a transmembrane receptor protein of 185 kDa, which is structurally related to the epidermal growth factor receptor. Herceptin has been shown, in both in vitro assays and in animals, to inhibit the proliferation of human tumor cells that overexpress HER2.
Herceptin is a mediator of antibody‑dependent cellular cytotoxicity (ADCC). In vitro, Herceptin‑mediated ADCC has been shown to be preferentially exerted on HER2 overexpressing cancer cells compared with cancer cells that do not overexpress HER2.
12.2 Pharmacokinetics
The pharmacokinetics of trastuzumab were studied in women with metastatic breast cancer. Short duration intravenous infusions of 10 to 500 mg Herceptin once weekly demonstrated dose‑dependent pharmacokinetics. Mean half‑life increased and clearance decreased with increasing dose level. The half‑life averaged 2 and 12 days at the 10 and 500 mg dose levels, respectively. The volume of distribution of trastuzumab was approximately that of serum volume (44 mL/kg). At the highest weekly dose studied (500 mg), mean peak serum concentrations were 377 mcg/mL.
In studies using an initial dose of 4 mg/kg followed by a weekly dose of 2 mg/kg, a mean half‑life of 6 days (range 1—32 days) was observed. Between weeks 16 and 32, trastuzumab serum concentrations reached a steady state with mean trough and peak concentrations of approximately 79 mcg/mL and 123 mcg/mL, respectively.
In a study of women receiving adjuvant therapy for breast cancer, a mean half‑life of trastuzumab of 16 days (range: 11—23 days) was observed after an initial dose of 8 mg/kg followed by a dose of 6 mg/kg every three weeks. Between weeks 6 and 37, trastuzumab serum concentrations reached a steady‑state with mean trough and peak concentrations of 63 mcg/mL and 216 mcg/mL, respectively.
Sixty‑four percent (286/447) of women with metastatic breast cancer had detectable circulating extracellular domain of the HER2 receptor (shed antigen), which ranged as high as 1880 ng/mL (median 11 ng/mL). Patients with higher baseline shed antigen levels were more likely to have lower serum trough concentrations.
Data suggest that the disposition of trastuzumab is not altered based on age or serum creatinine (≤ 2.0 mg creatinine/dL).
Mean serum trough concentrations of trastuzumab, when administered in combination with paclitaxel, were consistently elevated approximately 1.5‑fold as compared with serum concentrations of trastuzumab when used in combination with anthracycline plus cyclophosphamide. In clinical studies in HER2+ metastatic breast cancer where Herceptin was administered in combination with paclitaxel, in combination with docetaxel, or in combination with paclitaxel and doxorubicin, Herceptin did not appear to alter the plasma concentrations of these chemotherapeutic agents, or the metabolites that were analyzed.
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Herceptin has not been tested for its carcinogenic potential.
No evidence of mutagenic activity was observed when trastuzumab was tested in the standard Ames bacterial and human peripheral blood lymphocyte mutagenicity assays, at concentrations of up to 5000 mcg/mL. In an in vivo micronucleus assay, no evidence of chromosomal damage to mouse bone marrow cells was observed following bolus intravenous doses of up to 118 mg/kg Herceptin.
A fertility study conducted in female cynomolgus monkeys at doses up to 25 times the weekly recommended human dose of 2 mg/kg trastuzumab and has revealed no evidence of impaired fertility, as measured by menstrual cycle duration and female sex hormone levels. Studies to evaluate the effects of trastuzumab on male fertility have not been conducted.
13.2 Animal Toxicology and/or Pharmacology
Reproductive Toxicology Studies
Reproductive toxicology studies have been conducted in cynomolgus monkeys at doses up to 25 times the weekly recommended human dose of 2 mg/kg Herceptin and have revealed no evidence of impaired fertility or harm to the fetus. However, HER2 protein expression is high in many embryonic tissues including cardiac and neural tissues; in mutant mice lacking HER2, embryos died in early gestation. Placental transfer of Herceptin during the early (Days 20—50 of gestation) and late (Days 120—150 of gestation) fetal development period was observed in monkeys.
14 CLINICAL STUDIES
14.1 Adjuvant Breast Cancer
The safety and efficacy of Herceptin in women receiving adjuvant chemotherapy for HER2 overexpressing breast cancer, were evaluated in an integrated analysis of two randomized, open‑label, clinical trials (Studies 1 and 2) with a total of 3752 women, a third randomized, open‑label, clinical trial (Study 3) with a total of 3386 women, and a fourth randomized, open‑label clinical trial with a total of 3222 patients (Study 4).
Studies 1 and 2
In Studies 1 and 2, breast tumor specimens were required to show HER2 overexpression (3+ by IHC) or gene amplification (by FISH). HER2 testing was verified by a central laboratory prior to randomization (Study 2) or was required to be performed at a reference laboratory (Study 1). Patients with a history of active cardiac disease based on symptoms, abnormal electrocardiographic, radiologic, or left ventricular ejection fraction findings or uncontrolled hypertension (diastolic > 100 mmHg or systolic > 200 mmHg) were not eligible.
Patients were randomized (1:1) to receive doxorubicin and cyclophosphamide followed by paclitaxel (AC→paclitaxel) alone or paclitaxel plus Herceptin (AC→paclitaxel + Herceptin). In both trials, patients received four 21‑day cycles of doxorubicin 60 mg/m2 and cyclophosphamide 600 mg/m2. Paclitaxel was administered either weekly (80 mg/m2) or every 3 weeks (175 mg/m2) for a total of 12 weeks in Study 1; paclitaxel was administered only by the weekly schedule in Study 2. Herceptin was administered at 4 mg/kg on the day of initiation of paclitaxel and then at a dose of 2 mg/kg weekly for a total of 52 weeks. Herceptin treatment was permanently discontinued in patients who developed congestive heart failure, or persistent/recurrent LVEF decline [ see Dosage and Administration ( 2.2)]. Radiation therapy, if administered, was initiated after the completion of chemotherapy. Patients with ER+ and/or PR+ tumors received hormonal therapy. Disease‑free survival (DFS), defined as the time from randomization to recurrence, occurrence of contralateral breast cancer, other second primary cancer, or death, was the main outcome measure of the combined efficacy analysis.
A total of 3752 patients were included in the efficacy analyses. The data from both arms in Study 1 and two of the three study arms in Study 2 were pooled for efficacy analyses. Of these patients, the median age was 49 years (range, 22–80 years; 6% > 65 years), 84% were white, 7% black, 4% Hispanic, and 4% Asian/Pacific Islander. Disease characteristics included 90% infiltrating ductal histology, 38% T1, 91% nodal involvement, 27% intermediate and 66% high grade pathology, and 53% ER+ and/or PR+ tumors. At the time of randomization 53% of the population were to receive paclitaxel on a weekly regimen, and the remainder were to receive a q3 week schedule of paclitaxel.
Study 3
In Study 3, breast tumor specimens were required to show HER2 overexpression (3+ by IHC) or gene amplification (by FISH) as determined at a central laboratory. Patients with node‑negative disease were required to have pathological tumor size ≥ T1c primary tumor. Patients with a history of congestive heart failure or LVEF <55%, uncontrolled arrhythmias, angina requiring medication, clinically significant valvular heart disease, evidence of transmural infarction on ECG, poorly controlled hypertension (systolic > 180 mm Hg or diastolic > 100 mm Hg) were not eligible.
Patients were randomized (1:1) upon completion of definitive surgery, and at least four cycles of chemotherapy; to receive no additional treatment (n = 1693) or 1 year of Herceptin treatment (n = 1693). Patients undergoing a lumpectomy had also completed standard radiotherapy. Patients with ER+ and/or PgR+ disease received systemic adjuvant hormonal therapy at investigator discretion. Herceptin was administered with an initial dose of 8 mg/kg followed by subsequent doses of 6 mg/kg once every three weeks for a total of 52 weeks. The main outcome measure was disease‑free survival (DFS), defined as in Studies 1 and 2.
Among the 3386 patients randomized to the two treatment arms, the median age was 49 years (range 21—80), 83% were Caucasian, and 13% were Asian. Disease characteristics: 94% infiltrating ductal carcinoma, 50% ER+ and/or PgR+, 57% node positive, 32% node negative, and in 11% of patients, nodal status was not assessable due to prior neo‑adjuvant chemotherapy. Ninety‑six percent (1055/1098) of patients with node‑negative disease had high risk features: among the 1098 patients with node‑negative disease, 49% (543) were ER− and PgR−, and 47% (512) were ER and/or PgR + and had at least one of the following high risk features: pathological tumor size greater than 2 cm, Grade 2—3, or age < 35 years. Prior to randomization, 94% of patients had received anthracycline‑based chemotherapy regimens.
Study 4
In Study 4, breast tumor specimens were required to show HER2 gene amplification (FISH+ only) as determined at a central laboratory. Patients were required to have either node-positive disease, or node-negative disease with at least one of the following high-risk features: ER/PR-negative, tumor size > 2 cm, age < 35 years, or histologic and/or nuclear Grade 2 or 3. Patients with a history of CHF, myocardial infarction, Grade 3 or 4 cardiac arrhythmia, angina requiring medication, clinically significant valvular heart disease, poorly controlled hypertension (diastolic > 100 mmHg), any T4 or N2 or known N3 or M1 breast cancer were not eligible.
Patients were randomized (1:1:1) to receive doxorubicin and cyclophosphamide followed by docetaxel (AC‑T), doxorubicin and cyclophosphamide followed by docetaxel plus Herceptin (AC‑TH), or docetaxel and carboplatin plus Herceptin (TCH). In both the AC‑T and AC‑TH arms, doxorubicin 60 mg/m2 and cyclophosphamide 600 mg/m2 were administered every 3 weeks for four cycles; docetaxel 100 mg/m 2 was administered every 3 weeks for four cycles. In the TCH arm, docetaxel 75 mg/m2 and carboplatin (at a target AUC of 6 mg/mL/min as a 30‑ to 60‑minute infusion) were administered every 3 weeks for six cycles. Herceptin was administered weekly (initial dose of 4 mg/kg followed by weekly dose of 2 mg/kg) concurrently with either T or TC, and then every 3 weeks (6 mg/kg) as monotherapy for a total of 52 weeks. Radiation therapy, if administered, was initiated after completion of chemotherapy. Patients with ER+ and/or PR+ tumors received hormonal therapy. Disease free survival (DFS) was the main outcome measure.
Among the 3222 patients randomized, the median age was 49 (range 22 to 74 years; 6% ≥ 65 years). Disease characteristics included 54% ER+ and/or PR+ and 71% node positive. Prior to randomization, all patients underwent primary surgery for breast cancer.
|
DFS events | Hazard ratio (95% CI) p value |
Deaths | Hazard ratio p value |
|
|---|---|---|---|---|
| CI=confidence interval. | ||||
|
||||
| Studies 1 + 2* | ||||
| AC→TH (n=1872) | 133 | 0.48†
(0.39, 0.59) p=<0.0001‡ | 62 | 0.67 p=NS§ |
| AC→T (n=1880) | 261 | 92 | ||
|
Study 3 |
||||
| Chemo→Herceptin (n=1693) | 127 | 0.54 (0.44, 0.67) p=<0.0001¶ | 31 | 0.75 p=NS§ |
| Chemo→Observation (n=1693) | 219 | 40 | ||
|
Study 4 # |
||||
| TCH (n=1075) | 134 | 0.67 (0.54 – 0.84) p=0.0006‡,Þ | 56 | |
| AC→TH (n=1074) | 121 | 0.60 (0.48 – 0.76) p=<0.0001‡,Þ | 49 | |
| AC→T (n=1073) | 180 | 80 | ||
The results for DFS for the integrated analysis of Studies 1 and 2, Study 3, and Study 4 are presented in Table 7. The duration of DFS for Studies 1 and 2 is presented in Figure 4, and the duration of DFS for Study 4 is presented in Figure 5. Across all four studies, there were insufficient numbers of patients within each of the following subgroups to determine if the treatment effect was different from that of the overall patient population: patients with low tumor grade, patients within specific ethnic/racial subgroups (Black, Hispanic, Asian/Pacific Islander patients), and patients > 65 years of age.
| Figure
4
Duration of Disease‑Free Survival in Patients with Adjuvant Treatment of Breast Cancer (Studies 1 and 2) |
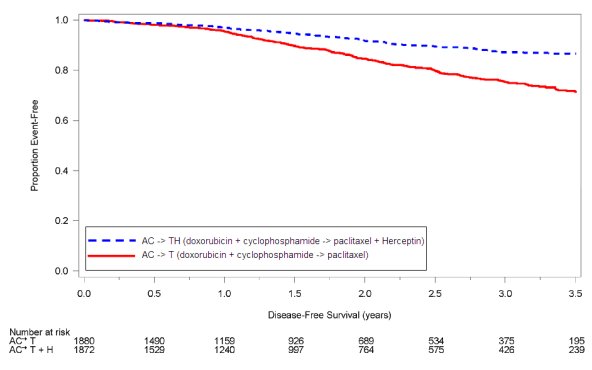 |
| Figure
5
Duration of Disease‑Free Survival in Patient with Adjuvant Treatment of Breast Cancer (Study 4) |
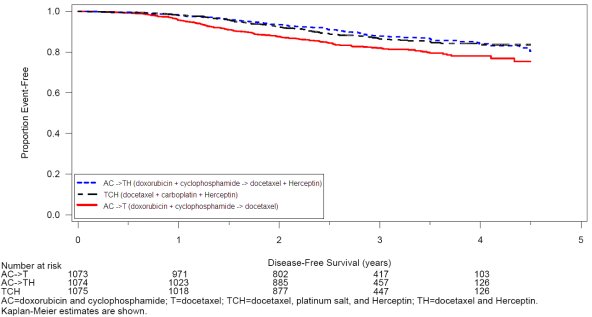 |
Exploratory analyses of DFS as a function of HER2 overexpression or gene amplification were conducted for patients in Studies 2 and 3, where central laboratory testing data were available. The results are shown in Table 8. The number of events in Study 2 was small with the exception of the IHC 3+/FISH+ subgroup, which constituted 81% of those with data. Definitive conclusions cannot be drawn regarding efficacy within other subgroups due to the small number of events. The number of events in Study 3 was adequate to demonstrate significant effects on DFS in the IHC 3+/FISH unknown and the FISH +/IHC unknown subgroups.
| Study 2 | Study 3 | |||
|---|---|---|---|---|
| HER2 Assay Result* | Number of Patients | Hazard Ratio DFS (95% CI) | Number of Patients | Hazard Ratio DFS (95% CI) |
| IHC 3+ | ||||
| FISH (+) | 1170 | 0.42 (0.27, 0.64) | 91 | 0.56 (0.13, 2.50) |
| FISH (−) | 51 | 0.71 (0.04, 11.79) | 8 | — |
| FISH Unknown | 51 | 0.69 (0.09, 5.14) | 2258 | 0.53 (0.41, 0.69) |
| IHC < 3+ /
FISH (+) | 174 | 1.01 (0.18, 5.65) | 299† | 0.53 (0.20, 1.42) |
| IHC unknown / FISH (+) | — | — | 724 | 0.59 (0.38, 0.93) |
14.2 Metastatic Breast Cancer
The safety and efficacy of Herceptin in treatment of women with metastatic breast cancer were studied in a randomized, controlled clinical trial in combination with chemotherapy (Study 5, n=469 patients) and an open label single agent clinical trial (Study 6, n=222 patients). Both trials studied patients with metastatic breast cancer whose tumors overexpress the HER2 protein. Patients were eligible if they had 2 or 3 levels of overexpression (based on a 0 to 3 scale) by immunohistochemical assessment of tumor tissue performed by a central testing lab.
Previously Untreated Metastatic Breast Cancer (Study 5)
Study 5 was a multicenter, randomized, open‑label clinical trial conducted in 469 women with metastatic breast cancer who had not been previously treated with chemotherapy for metastatic disease. Tumor specimens were tested by IHC (Clinical Trial Assay, CTA) and scored as 0, 1+, 2+, or 3+, with 3+ indicating the strongest positivity. Only patients with 2+ or 3+ positive tumors were eligible (about 33% of those screened). Patients were randomized to receive chemotherapy alone or in combination with Herceptin given intravenously as a 4 mg/kg loading dose followed by weekly doses of Herceptin at 2 mg/kg. For those who had received prior anthracycline therapy in the adjuvant setting, chemotherapy consisted of paclitaxel (175 mg/m2 over 3 hours every 21 days for at least six cycles); for all other patients, chemotherapy consisted of anthracycline plus cyclophosphamide (AC: doxorubicin 60 mg/m2 or epirubicin 75 mg/m2 plus 600 mg/m2 cyclophosphamide every 21 days for six cycles). Sixty five percent of patients randomized to receive chemotherapy alone in this study received Herceptin at the time of disease progression as part of a separate extension study.
Based upon the determination by an independent response evaluation committee the patients randomized to Herceptin and chemotherapy experienced a significantly longer median time to disease progression, a higher overall response rate (ORR), and a longer median duration of response, as compared with patients randomized to chemotherapy alone. Patients randomized to Herceptin and chemotherapy also had a longer median survival (see Table 8). These treatment effects were observed both in patients who received Herceptin plus paclitaxel and in those who received Herceptin plus AC; however the magnitude of the effects was greater in the paclitaxel subgroup.
| Combined Results | Paclitaxel Subgroup | AC Subgroup | ||||
|---|---|---|---|---|---|---|
| Herceptin + All
Chemotherapy (n = 235) | All
Chemotherapy (n = 234) | Herceptin +
Paclitaxel (n = 92) | Paclitaxel (n = 96) | Herceptin + AC
*
(n = 143) | AC (n = 138) |
|
| Primary Endpoint | ||||||
| Median TTP(mos)†, ‡ | 7.2 | 4.5 | 6.7 | 2.5 | 7.6 | 5.7 |
| 95% CI | 7, 8 | 4, 5 | 5, 10 | 2, 4 | 7, 9 | 5, 7 |
| p‑value§ | < 0.0001 | < 0.0001 | 0.002 | |||
| Secondary Endpoints | ||||||
| Overall Response Rate† | 45 | 29 | 38 | 15 | 50 | 38 |
| 95% CI | 39, 51 | 23, 35 | 28, 48 | 8, 22 | 42, 58 | 30, 46 |
| p‑value¶ | < 0.001 | < 0.001 | 0.10 | |||
| Median Resp Duration (mos)†,‡ | 8.3 | 5.8 | 8.3 | 4.3 | 8.4 | 6.4 |
| 25%, 75% quartile | 6, 15 | 4, 8 | 5 ,11 | 4, 7 | 6, 15 | 4, 8 |
| Med Survival (mos)‡ | 25.1 | 20.3 | 22.1 | 18.4 | 26.8 | 21.4 |
| 95% CI | 22, 30 | 17, 24 | 17, 29 | 13, 24 | 23, 33 | 18, 27 |
| p‑value§ | 0.05 | 0.17 | 0.16 | |||
Data from Study 5 suggest that the beneficial treatment effects were largely limited to patients with the highest level of HER2 protein overexpression (3+) (see Table 9).
| HER2 Assay Result | Number of Patients (N) | Relative Risk* for Time
to Disease Progression (95% CI) | Relative Risk * for Mortality (95% CI) |
|---|---|---|---|
| CTA 2+ or 3+ | 469 | 0.49 (0.40, 0.61) | 0.80 (0.64, 1.00) |
| FISH (+) † | 325 | 0.44 (0.34, 0.57) | 0.70 (0.53, 0.91) |
| FISH (−)† | 126 | 0.62 (0.42, 0.94) | 1.06 (0.70, 1.63) |
| CTA 2+ | 120 | 0.76 (0.50, 1.15) | 1.26 (0.82, 1.94) |
| FISH (+) | 32 | 0.54 (0.21, 1.35) | 1.31 (0.53, 3.27) |
| FISH (–) | 83 | 0.77 (0.48, 1.25) | 1.11 (0.68, 1.82) |
| CTA 3+ | 349 | 0.42 (0.33, 0.54) | 0.70 (0.51, 0.90) |
| FISH (+) | 293 | 0.42 (0.32, 0.55) | 0.67 (0.51, 0.89) |
| FISH (–) | 43 | 0.43 (0.20, 0.94) | 0.88 (0.39, 1.98) |
Previously Treated Metastatic Breast Cancer (Study 6)
Herceptin was studied as a single agent in a multicenter, open‑label, single‑arm clinical trial (Study 6) in patients with HER2 overexpressing metastatic breast cancer who had relapsed following one or two prior chemotherapy regimens for metastatic disease. Of 222 patients enrolled, 66% had received prior adjuvant chemotherapy, 68% had received two prior chemotherapy regimens for metastatic disease, and 25% had received prior myeloablative treatment with hematopoietic rescue. Patients were treated with a loading dose of 4 mg/kg IV followed by weekly doses of Herceptin at 2 mg/kg IV.
The ORR (complete response+partial response), as determined by an independent Response Evaluation Committee, was 14%, with a 2% complete response rate and a 12% partial response rate. Complete responses were observed only in patients with disease limited to skin and lymph nodes. The overall response rate in patients whose tumors tested as CTA 3+ was 18% while in those that tested as CTA 2+, it was 6%.
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
Herceptin is supplied in a multi‑use vial containing 440 mg trastuzumab as a lyophilized sterile powder, under vacuum. Each carton contains one vial Herceptin® and one vial (20 mL) of Bacteriostatic Water for Injection (BWFI), USP, containing 1.1% benzyl alcohol as a preservative. NDC 50242‑134‑68.
16.2 Stability and Storage
Vials of Herceptin are stable at 2–8°C (36–46°F) prior to reconstitution.
Do not use beyond the expiration date stamped on the vial. A vial of Herceptin reconstituted with BWFI, as supplied, is stable for 28 days after reconstitution when stored refrigerated at 2–8°C (36–46°F). Discard any remaining multi‑dose reconstituted solution after 28 days. A vial of Herceptin reconstituted with unpreserved SWFI (not supplied) should be used immediately and any unused portion discarded. Do Not Freeze Herceptin following reconstitution or dilution.
The solution of Herceptin for infusion diluted in polyvinylchloride or polyethylene bags containing 0.9% Sodium Chloride Injection, USP, should be stored at 2–8°C (36–46°F) for no more than 24 hours prior to use.
17 PATIENT COUNSELING INFORMATION
∙ Advise patients to contact a health care professional immediately for any of the following: new onset or worsening shortness of breath, cough, swelling of the ankles/legs, swelling of the face, palpitations, weight gain of more than 5 pounds in 24 hours, dizziness or loss of consciousness [ see Boxed Warning: Cardiomyopathy].
∙ Advise women with reproductive potential to use effective contraceptive methods during treatment and for a minimum of six months following Herceptin [ see Pregnancy ( 8.1)].
∙ Encourage pregnant women who are using Herceptin to enroll in the Cancer and Childbirth Registry [ see Pregnancy ( 8.1)].
Herceptin® [trastuzumab]
Manufactured by:
Genentech,
Inc.
1 DNA Way
South San Francisco, CA
94080‑4990
4839800
©2006 Genentech, Inc.
| Herceptin (Trastuzumab) | ||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
Revised: 06/2008Genentech