|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
FULL PRESCRIBING INFORMATION
1 INDICATIONS AND USAGE
To reduce the development of drug-resistant bacteria and maintain the effectiveness of Cefepime Injection and other antibacterial drugs, Cefepime Injection should be used only to treat or prevent infections that are proven or strongly suspected to be caused by susceptible bacteria. When culture and susceptibility information are available, they should be considered in selecting or modifying antibacterial therapy. In the absence of such data, local epidemiology and susceptibility patterns may contribute to the empiric selection of therapy.
1.1 Pneumonia
Cefepime Injection is indicated for pneumonia (moderate to severe) caused by Streptococcus pneumoniae, including cases associated with concurrent bacteremia, Pseudomonas aeruginosa, Klebsiella pneumoniae, or Enterobacter species.
1.2 Empiric Therapy for Febrile Neutropenic Patients
Cefepime Injection as monotherapy is indicated for empiric treatment of febrile neutropenic patients. In patients at high risk for severe infection (including patients with a history of recent bone marrow transplantation, with hypotension at presentation, with an underlying hematologic malignancy, or with severe or prolonged neutropenia), antimicrobial monotherapy may not be appropriate. Insufficient data exist to support the efficacy of cefepime monotherapy in such patients [see Clinical Studies (14)].
1.3 Uncomplicated and Complicated Urinary Tract Infections (including pyelonephritis)
Cefepime Injection is indicated for uncomplicated and complicated urinary tract infections (including pyelonephritis) caused by Escherichia coli or Klebsiella pneumoniae, when the infection is severe, or caused by Escherichia coli, Klebsiella pneumoniae, or Proteus mirabilis, when the infection is mild to moderate, including cases associated with concurrent bacteremia with these microorganisms.
1.4 Uncomplicated Skin and Skin Structure Infections
Cefepime Injection is indicated for uncomplicated skin and skin structure infections caused by Staphylococcus aureus (methicillin-susceptible isolates only) or Streptococcus pyogenes.
1.5 Complicated Intra-abdominal Infections
Cefepime Injection is indicated for complicated intra-abdominal infections (used in combination with metronidazole) caused by Escherichia coli, viridans group streptococci, Pseudomonas aeruginosa, Klebsiella pneumoniae, Enterobacter species, or Bacteroides fragilis [see Clinical Studies (14)].
2 DOSAGE AND ADMINISTRATION
2.1 Adults and Pediatric Population
The recommended adult and pediatric dosages and routes of administration are outlined in Table 1. Cefepime Injection should be administered intravenously over approximately 30 minutes.
| Site and Type of Infection | Dose | Frequency | Duration (days) |
|---|---|---|---|
| Adults | |||
| Moderate to Severe Pneumonia due to S. pneumoniae*, P. aeruginosa, K. pneumoniae, or Enterobacter species | 1-2 g IV | Every 12 hours | 10 |
| Empiric therapy for febrile neutropenic patients [see Indications and Usage (1) and Clinical Studies (14)] | 2 g IV | Every 8 hours | 7† |
| Mild to Moderate Uncomplicated or Complicated Urinary Tract Infections, including pyelonephritis, due to E. coli, K. pneumoniae, or P. mirabilis* | 0.5-1 g IV | Every 12 hours | 7-10 |
| Severe Uncomplicated or Complicated Urinary Tract Infections, including pyelonephritis, due to E. coli or K. pneumoniae* | 2 g IV | Every 12 hours | 10 |
| Moderate to Severe Uncomplicated Skin and Skin Structure Infections due to S. aureus or S. pyogenes | 2 g IV | Every 12 hours | 10 |
| Complicated Intra-abdominal Infections (used in combination with metronidazole) caused by E. coli, viridans group streptococci, P. aeruginosa, K. pneumoniae, Enterobacter species, or B. fragilis. [see Clinical Studies (14)] | 2 g IV | Every 12 hours | 7-10 |
| Pediatric Patients (2 months up to 16 years) | |||
| The maximum dose for pediatric patients should not exceed the recommended adult dose. The usual recommended dosage in pediatric patients up to 40 kg in weight for uncomplicated and complicated urinary tract infections (including pyelonephritis), uncomplicated skin and skin structure infections, and pneumonia is 50 mg per kg per dose, administered every 12 hours (50 mg per kg per dose, every 8 hours for febrile neutropenic patients), for durations as given above. Cefepime Injection in GALAXY Container should be used only in pediatric patients who require the entire 1 or 2 g dose and not any fraction thereof. |
|||
2.2 Patients with Hepatic Impairment
No adjustment is necessary for patients with impaired hepatic function.
2.3 Patients with Renal Impairment
In patients with creatinine clearance less than or equal to 60 mL/min, the dose of Cefepime Injection should be adjusted to compensate for the slower rate of renal elimination. The recommended initial dose of Cefepime Injection should be the same as in patients with normal renal function except in patients undergoing hemodialysis. The recommended doses of Cefepime Injection in patients with renal impairment are presented in Table 2.
When only serum creatinine is available, the following formula (Cockcroft and Gault equation)1 may be used to estimate creatinine clearance. The serum creatinine should represent a steady state of renal function:
| Males: Creatinine Clearance (mL/min) = | Weight (kg) × (140 – age) | |
| 72 × serum creatinine (mg/dL) | ||
| Females: 0.85 × above value |
| Creatinine Clearance (mL/min) | Recommended Maintenance Schedule | |||
|---|---|---|---|---|
|
||||
| Greater than 60 (Normal recommended dosing schedule) | 500 mg every 12 hours | 1 g every 12 hours | 2 g every 12 hours | 2 g every 8 hours |
| 30–60 | 500 mg every 24 hours | 1 g every 24 hours | 2 g every 24 hours | 2 g every 12 hours |
| 11–29 | 500 mg every 24 hours | 500 mg every 24 hours | 1 g every 24 hours | 2 g every 24 hours |
| Less than 11 | 250 mg every 24 hours | 250 mg every 24 hours | 500 mg every 24 hours | 1 g every 24 hours |
| CAPD | 500 mg every 48 hours | 1 g every 48 hours | 2 g every 48 hours | 2 g every 48 hours |
| Hemodialysis* | 1 g on day 1, then 500 mg every 24 hours thereafter | 1 g every 24 hours | ||
In patients undergoing continuous ambulatory peritoneal dialysis, Cefepime Injection may be administered at normally recommended doses at a dosage interval of every 48 hours (see Table 2).
In patients undergoing hemodialysis, approximately 68% of the total amount of cefepime present in the body at the start of dialysis will be removed during a 3-hour dialysis period. The dosage of Cefepime Injection for hemodialysis patients is 1 g on Day 1 followed by 500 mg every 24 hours for the treatment of all infections except febrile neutropenia, which is 1 g every 24 hours. Cefepime Injection should be administered at the same time each day following the completion of hemodialysis on hemodialysis days (see Table 2).
Data in pediatric patients with impaired renal function are not available; however, since cefepime pharmacokinetics are similar in adults and pediatric patients [see Clinical Pharmacology (12)], changes in the dosing regimen proportional to those in adults (see Table 1 and Table 2) are recommended for pediatric patients.
2.4 Directions for Use of Cefepime Injection in GALAXY Container
Cefepime Injection in GALAXY Container (PL 2040 Plastic) is for intravenous administration using sterile equipment after thawing to room temperature.
Thawing of Plastic Container
Thaw frozen container at room temperature 25°C (77°F) or under refrigeration 5°C (41°F). Do not force thaw by immersion in water baths or by microwave irradiation. [See How Supplied/Storage and Handling (16).]
Check for minute leaks by squeezing container firmly. If leaks are detected, discard solution as sterility may be impaired.
Do not add supplementary medication.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
Components of the solution may precipitate in the frozen state and will dissolve upon reaching room temperature with little or no agitation. Potency is not affected. Agitate after solution has reached room temperature. If after visual inspection the solution remains cloudy or if an insoluble precipitate is noted or if any seals or the outlet port are not intact, the container should be discarded.
Caution: Do not use plastic containers in series connections. Such use could result in air embolism due to residual air being drawn from the primary container before administration of the fluid from the secondary container is complete.
Preparation for intravenous administration.
- Suspend container from eyelet support.
- Remove protector from outlet port at bottom of container.
- Attach administration set. Refer to complete directions accompanying set.
Cefepime Injection should be administered intravenously over approximately 30 minutes.
Intermittent intravenous infusion with a Y-type administration set can be accomplished with compatible solutions. However, during infusion of Cefepime Injection, it is desirable to discontinue the other solution.
Solutions of cefepime, like those of most beta-lactam antibiotics, should not be added to solutions of ampicillin at a concentration greater than 40 mg/mL, and should not be added to metronidazole, vancomycin, gentamicin, tobramycin, netilmicin sulfate or aminophylline because of potential interaction. However, if concurrent therapy with cefepime is indicated, each of these antibiotics can be administered separately.
3 DOSAGE FORMS AND STRENGTHS
Intravenous Injection:
- 1 g in 50 mL (contains 1 g of cefepime as Cefepime Hydrochloride, USP)
- 2 g in 100 mL (contains 2 g of cefepime as Cefepime Hydrochloride, USP)
4 CONTRAINDICATIONS
Cefepime Injection is contraindicated in patients who have shown immediate hypersensitivity reactions to cefepime or the cephalosporin class of antibiotics, penicillins or other beta-lactam antibiotics.
Solutions containing dextrose may be contraindicated in patients with known allergy to corn or corn products.
5 WARNINGS AND PRECAUTIONS
5.1 Hypersensitivity
Before therapy with Cefepime Injection is instituted, careful inquiry should be made to determine whether the patient has had previous immediate hypersensitivity reactions to cefepime, cephalosporins, penicillins, or other drugs. If this product is to be given to penicillin-sensitive patients, caution should be exercised because cross-hypersensitivity among beta-lactam antibiotics has been clearly documented and may occur in up to 10% of patients with a history of penicillin allergy. If an allergic reaction to Cefepime Injection occurs, discontinue the drug. Serious acute hypersensitivity reactions may require treatment with epinephrine and other emergency measures including oxygen, corticosteroids, intravenous fluids, intravenous antihistamines, pressor amines, and airway management, as clinically indicated.
5.2 Renal Impairment
In patients with creatinine clearance less than or equal to 60 mL/min, the dose of Cefepime Injection should be adjusted to compensate for the slower rate of renal elimination. Because high and prolonged serum antibiotic concentrations can occur from usual dosages in patients with renal impairment or other conditions that may compromise renal function, the maintenance dosage should be reduced when Cefepime Injection is administered to such patients. Continued dosage should be determined by degree of renal impairment, severity of infection, and susceptibility of the causative organisms. Refer to specific recommendations for dosing adjustment [See Dosage and Administration (2)]. During postmarketing surveillance, serious adverse events have been reported including life-threatening or fatal occurrences of the following: encephalopathy (disturbance of consciousness including confusion, hallucinations, stupor, and coma), myoclonus, and seizures [see Adverse Reactions (6.2)]. Most cases occurred in patients with renal impairment who received doses of cefepime that exceeded the recommended dosage schedules. However, some cases of encephalopathy occurred in patients receiving a dosage adjustment for their renal function. In the majority of cases, symptoms of neurotoxicity were reversible and resolved after discontinuation of cefepime and/or after hemodialysis.
5.3 Clostridium difficile Associated Diarrhea
Clostridium difficile associated diarrhea (CDAD) has been reported with use of nearly all antibacterial agents, including Cefepime Injection, and may range in severity from mild diarrhea to fatal colitis. Treatment with antibacterial agents alters the normal flora of the colon leading to overgrowth of C. difficile.
C. difficile produces toxins A and B which contribute to the development of CDAD. Hypertoxin producing strains of C. difficile cause increased morbidity and mortality, as these infections can be refractory to antimicrobial therapy and may require colectomy. CDAD must be considered in all patients who present with diarrhea following antibiotic use. Careful medical history is necessary since CDAD has been reported to occur over two months after the administration of antibacterial agents.
If CDAD is suspected or confirmed, ongoing antibiotic use not directed against C. difficile may need to be discontinued. Appropriate fluid and electrolyte management, protein supplementation, antibiotic treatment of C. difficile, and surgical evaluation should be instituted as clinically indicated.
5.4 Risk of Development of Drug-Resistant Bacteria
Prescribing cefepime in the absence of a proven or strongly suspected bacterial infection or a prophylactic indication is unlikely to provide benefit to the patient and increases the risk of the development of drug-resistant bacteria.
As with other antimicrobials, prolonged use of cefepime may result in overgrowth of nonsusceptible microorganisms. Repeated evaluation of the patient’s condition is essential. Should superinfection occur during therapy, appropriate measures should be taken.
5.5 Patients with Meningeal Seeding/Meningitis
In those patients in whom meningeal seeding from a distant infection site or in whom meningitis is suspected or documented, an alternate agent with demonstrated clinical efficacy in this setting should be used.
5.6 Drug/Laboratory Test Interactions
Urinary Glucose
The administration of cefepime may result in a false-positive reaction for glucose in the urine when using CLINITEST tablets. It is recommended that glucose tests based on enzymatic glucose oxidase reactions (such as CLINISTIX) be used.
Coombs' Test
Positive direct Coombs’ tests have been reported during treatment with cefepime. In hematologic studies or in transfusion cross-matching procedures when antiglobulin tests are performed on the minor side or in Coombs’ testing of newborns whose mothers have received cephalosporin antibiotics before parturition, it should be recognized that a positive Coombs’ test may be due to the drug.
Prothrombin Time
Many cephalosporins, including cefepime, have been associated with a fall in prothrombin activity. Those at risk include patients with renal or hepatic impairment, or poor nutritional state, as well as patients receiving a protracted course of antimicrobial therapy. Prothrombin time should be monitored in patients at risk, and exogenous vitamin K administered as indicated.
5.7 Patients with a History of Gastrointestinal Disease
Cefepime Injection should be prescribed with caution in individuals with a history of gastrointestinal disease, particularly colitis.
5.8 Possible Effects of Arginine on Glucose Metabolism
Cefepime Injection contains arginine to adjust pH [see Description (11)]. Arginine has been shown to alter glucose metabolism and elevate serum potassium transiently when administered at 33 times the amount provided by the maximum recommended human dose of cefepime. The effect of lower doses is not presently known.
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
In clinical trials using multiple doses of cefepime, 4137 patients were treated with the recommended dosages of cefepime (500 mg to 2 g intravenously every 12 hours). Sixty-four (1.5%) patients discontinued medication due to adverse events thought by the investigators to be possibly, probably, or almost certainly related to drug toxicity. Thirty-three (51%) of these 64 patients who discontinued therapy did so because of rash. The percentage of cefepime-treated patients who discontinued study drug because of drug-related adverse events was very similar at daily doses of 500 mg, 1 g, and 2 g every 12 hours (0.8%, 1.1%, and 2.0%, respectively). However, the incidence of discontinuation due to rash increased with the higher recommended doses.
The following adverse events were thought to be probably related to cefepime during evaluation of the drug in clinical trials conducted in North America (n=3125 cefepime-treated patients).
|
|
| INCIDENCE EQUAL TO OR GREATER THAN 1% | Local reactions (3%), including phlebitis (1.3%), pain and/or inflammation (0.6%)*; rash (1.1%) |
| INCIDENCE LESS THAN 1% BUT GREATER THAN 0.1% | Colitis (including pseudomembranous colitis), diarrhea, fever, headache, nausea, oral moniliasis, pruritus, urticaria, vaginitis, vomiting |
At the higher dose of 2 g every 8 hours, the incidence of probably-related adverse events was higher among the 795 patients who received this dose of cefepime. They consisted of rash (4%), diarrhea (3%), nausea (2%), vomiting (1%), pruritus (1%), fever (1%), and headache (1%).
The following adverse laboratory changes, irrespective of relationship to therapy with cefepime, were seen during clinical trials conducted in North America.
|
|
| INCIDENCE EQUAL TO OR GREATER THAN 1% | Positive Coombs' test (without hemolysis) (16.2%); decreased phosphorus (2.8%); increased ALT/SGPT (2.8%), AST/SGOT (2.4%), eosinophils (1.7%); abnormal PTT (1.6%), PT (1.4%) |
| INCIDENCE LESS THAN 1% BUT GREATER THAN 0.1% | Increased alkaline phosphatase, BUN, calcium, creatinine, phosphorus, potassium, total bilirubin; decreased calcium*, hematocrit, neutrophils, platelets, WBC |
A similar safety profile was seen in clinical trials of pediatric patients [see Use in Specific Populations (8.4)].
6.2 Postmarketing Experience
In addition to the events reported during North American clinical trials with cefepime, the following adverse experiences have been reported during worldwide postmarketing experience. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
As with some other drugs in this class, encephalopathy (disturbance of consciousness including confusion, hallucinations, stupor, and coma), myoclonus, and seizures have been reported. Although most cases occurred in patients with renal impairment who received doses of cefepime that exceeded the recommended dosage schedules, some cases of encephalopathy occurred in patients receiving a dosage adjustment for their renal function [see Warnings and Precautions (5)]. If seizures associated with drug therapy occur, the drug should be discontinued. Anticonvulsant therapy can be given if clinically indicated. Precautions should be taken to adjust daily dosage in patients with renal impairment or other conditions that may compromise renal function to reduce antibiotic concentrations that can lead or contribute to these and other serious adverse events, including renal failure.
As with other cephalosporins, anaphylaxis including anaphylactic shock, transient leukopenia, neutropenia, agranulocytosis, and thrombocytopenia have been reported.
6.3 Cephalosporin-class Adverse Reactions
In addition to the adverse reactions listed above that have been observed in patients treated with cefepime, the following adverse reactions have been reported for cephalosporin-class antibiotics:
Stevens-Johnson syndrome, erythema multiforme, toxic epidermal necrolysis, renal impairment, toxic nephropathy, aplastic anemia, hemolytic anemia, hemorrhage, hepatic impairment including cholestasis, and pancytopenia.
7 DRUG INTERACTIONS
7.1 Aminoglycosides
Renal function should be monitored carefully if high doses of aminoglycosides are to be administered with Cefepime Injection because of the increased potential of nephrotoxicity and ototoxicity of aminoglycoside antibiotics.
7.2 Diuretics
Nephrotoxicity has been reported following concomitant administration of other cephalosporins with potent diuretics such as furosemide.
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category B. Cefepime was not teratogenic or embryocidal when administered during the period of organogenesis to rats at doses up to 1000 mg/kg/day (1.6 times the recommended maximum human dose calculated on a mg/m2 basis) or to mice at doses up to 1200 mg/kg (approximately equal to the recommended maximum human dose calculated on a mg/m2 basis) or to rabbits at a dose level of 100 mg/kg (0.3 times the recommended maximum human dose calculated on a mg/m2 basis).
There are, however, no adequate and well-controlled studies of cefepime use in pregnant women. Because animal reproduction studies are not always predictive of human response, this drug should be used during pregnancy only if clearly needed.
8.2 Labor and Delivery
Cefepime has not been studied for use during labor and delivery. Treatment should only be given if clearly indicated.
8.3 Nursing Mothers
Cefepime is excreted in human breast milk in very low concentrations (0.5 mcg/mL). Caution should be exercised when Cefepime Injection is administered to a nursing woman.
8.4 Pediatric Use
The safety and effectiveness of cefepime in the treatment of uncomplicated and complicated urinary tract infections (including pyelonephritis), uncomplicated skin and skin structure infections, pneumonia, and as empiric therapy for febrile neutropenic patients have been established in the age groups 2 months up to 16 years. Use of Cefepime Injection in these age groups is supported by evidence from adequate and well-controlled studies of cefepime in adults with additional pharmacokinetic and safety data from pediatric trials [see Clinical Pharmacology (12)].
Safety and effectiveness in pediatric patients below the age of 2 months have not been established. There are insufficient clinical data to support the use of Cefepime Injection in pediatric patients under 2 months of age or for the treatment of serious infections in the pediatric population where the suspected or proven pathogen is Haemophilus influenzae type b.
Cefepime Injection in GALAXY Container should be used only in pediatric patients who require the entire 1 or 2 g dose and not any fraction thereof.
8.5 Geriatric Use
Of the more than 6400 adults treated with cefepime in clinical studies, 35% were 65 years or older while 16% were 75 years or older. When geriatric patients received the usual recommended adult dose, clinical efficacy and safety were comparable to clinical efficacy and safety in nongeriatric adult patients.
Serious adverse events have occurred in geriatric patients with renal impairment given unadjusted doses of cefepime, including life-threatening or fatal occurrences of the following: encephalopathy, myoclonus, and seizures [see Warnings and Precautions (5) and Adverse Reactions (6)].
This drug is known to be substantially excreted by the kidney, and the risk of toxic reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and renal function should be monitored [see Clinical Pharmacology (12), Warnings and Precautions (5), and Dosage and Administration (2)].
10 OVERDOSAGE
Patients who receive an overdose should be carefully observed and given supportive treatment. In the presence of renal impairment, hemodialysis, not peritoneal dialysis, is recommended to aid in the removal of cefepime from the body. Accidental overdosing has occurred when large doses were given to patients with impaired renal function. Symptoms of overdose include encephalopathy (disturbance of consciousness including confusion, hallucinations, stupor, and coma), myoclonus, seizures, and neuromuscular excitability [see Warnings and Precautions (5), Adverse Reactions (6), and Dosage and Administration (2)].
11 DESCRIPTION
Cefepime Injection in GALAXY Containers (PL 2040 Plastic) is a sterile, injectable product consisting of Cefepime Hydrochloride, USP, a semi-synthetic, broad spectrum, cephalosporin antibiotic for parenteral administration. The chemical name is 1-[[(6R,7R)-7-[2-(2-Amino-4-thiazolyl) glyoxylamido]-2-carboxy-8-oxo-5-thia-1-azabicyclo[4.2.0] oct-2-en-3-yl]methyl]-1-methylpyrrolidinium chloride, 72-(Z)-(O-methyloxime), monohydrochloride, monohydrate, which corresponds to the following structural formula:
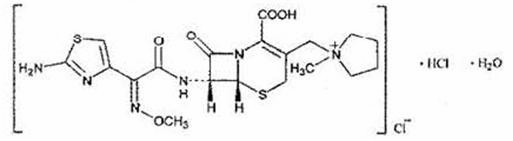
Cefepime hydrochloride (monohydrate) has a molecular mass of 571.50 and a molecular formula of C19H25ClN6O5S2•HCl•H2O.
Cefepime Injection in GALAXY Container (PL 2040 Plastic) is a frozen, iso-osmotic, sterile, non-pyrogenic premixed solution supplied for intravenous administration in strengths equivalent to 1 g and 2 g of cefepime [see Dosage and Administration (2)]. It contains the equivalent of not less than 90 percent and not more than 115 percent of the labeled amount of cefepime (C19H24N6O5S2).
The solution is intended for intravenous use after thawing to room temperature. The components and dosage formulations are given in the table below:
| Component* | Function | Dosage Formulations | |
|---|---|---|---|
| 1 g in 50 mL | 2 g in 100 mL | ||
|
|||
| Cefepime | active ingredient | 1 g | 2 g |
| Dextrose Hydrous, USP | osmolality adjuster | 1.03 g | 2.06 g |
| L-Arginine, USP† | pH adjuster | 725 mg | 1.45 g |
| Hydrochloric Acid† | pH adjuster | As needed | As needed |
| Water for Injection, USP | vehicle | q.s.‡ 50 mL | q.s.‡ 100 mL |
Cefepime Injection will range in color from colorless to amber.
The plastic container is fabricated from a specially designed multilayer plastic (PL 2040). Solutions are in contact with the polyethylene layer of this container and can leach out certain chemical components of the plastic in very small amounts within the expiration period. The suitability of the plastic has been confirmed in tests in animals according to the USP biological tests for plastic containers, as well as by tissue culture toxicity studies.
12 CLINICAL PHARMACOLOGY
Cefepime is an antibacterial agent belonging to the cephalosporin class of antibacterials with in vitro antibacterial activity against facultative Gram-positive and Gram-negative bacteria.
12.1 Mechanism of Action
Cefepime is an antibacterial drug. [See Clinical Pharmacology (12.4)]
12.2 Pharmacodynamics
Similar to other beta-lactam antimicrobial agents, the time that the unbound plasma concentration of cefepime exceeds the MIC of the infecting organism has been shown to best correlate with efficacy in animal models of infection. However, the pharmacokinetic/pharmacodynamic relationship for cefepime has not been evaluated in patients.
12.3 Pharmacokinetics
The average plasma concentrations of cefepime observed in healthy adult male volunteers (n=9) at various times following single 30-minute intravenous infusions of cefepime 500 mg, 1 g, and 2 g are summarized in Table 6. Elimination of cefepime is principally via renal excretion with an average (±SD) half-life of 2 (±0.3) hours and total body clearance of 120 (±8) mL/min in healthy volunteers. Cefepime pharmacokinetics are linear over the range 250 mg to 2 g. There is no evidence of accumulation in healthy adult male volunteers (n=7) receiving clinically relevant doses for a period of 9 days.
| CEFEPIME | |||
|---|---|---|---|
| Parameter | 500 mg IV | 1 g IV | 2 g IV |
| 0.5 h | 38.2 | 78.7 | 163.1 |
| 1 h | 21.6 | 44.5 | 85.8 |
| 2 h | 11.6 | 24.3 | 44.8 |
| 4 h | 5 | 10.5 | 19.2 |
| 8 h | 1.4 | 2.4 | 3.9 |
| 12 h | 0.2 | 0.6 | 1.1 |
| Cmax, mcg/mL | 39.1 (3.5) | 81.7 (5.1) | 163.9 (25.3) |
| AUC, h∙mcg/mL | 70.8 (6.7) | 148.5 (15.1) | 284.8 (30.6) |
| Number of subjects (male) | 9 | 9 | 9 |
Distribution
The average steady-state volume of distribution of cefepime is 18.0 (±2.0) L. The serum protein binding of cefepime is approximately 20% and is independent of its concentration in serum.
Cefepime is excreted in human milk. A nursing infant consuming approximately 1000 mL of human milk per day would receive approximately 0.5 mg of cefepime per day [see Use in Specific Populations (8.3)].
Concentrations of cefepime achieved in specific tissues and body fluids are listed in Table 7.
| Tissue or Fluid | Dose/Route | # of Patients | Average Time of Sample Post-Dose (h) | Average Concentration |
|---|---|---|---|---|
| Blister Fluid | 2 g IV | 6 | 1.5 | 81.4 mcg/mL |
| Bronchial Mucosa | 2 g IV | 20 | 4.8 | 24.1 mcg/g |
| Sputum | 2 g IV | 5 | 4 | 7.4 mcg/mL |
| Urine | 500 mg IV | 8 | 0-4 | 292 mcg/mL |
| 1 g IV | 12 | 0-4 | 926 mcg/mL | |
| 2 g IV | 12 | 0-4 | 3120 mcg/mL | |
| Bile | 2 g IV | 26 | 9.4 | 17.8 mcg/mL |
| Peritoneal Fluid | 2 g IV | 19 | 4.4 | 18.3 mcg/mL |
| Appendix | 2 g IV | 31 | 5.7 | 5.2 mcg/g |
| Gall Bladder | 2 g IV | 38 | 8.9 | 11.9 mcg/g |
| Prostate | 2 g IV | 5 | 1 | 31.5 mcg/g |
Data suggest that cefepime does cross the inflamed blood-brain barrier. The clinical relevance of these data is uncertain at this time.
Metabolism and Excretion
Cefepime is metabolized to N-methylpyrrolidine (NMP), which is rapidly converted to the N-oxide (NMP-N-oxide). Urinary recovery of unchanged cefepime accounts for approximately 85% of the administered dose. Less than 1% of the administered dose is recovered from urine as NMP, 6.8% as NMP-N-oxide, and 2.5% as an epimer of cefepime. Because renal excretion is a significant pathway of elimination, patients with renal dysfunction and patients undergoing hemodialysis require dosage adjustment [see Dosage and Administration (2)].
Specific Populations
Patients with Renal Impairment
Cefepime pharmacokinetics have been investigated in patients with various degrees of renal impairment (n=30). The average half-life in patients requiring hemodialysis was 13.5 (±2.7) hours and in patients requiring continuous peritoneal dialysis was 19 (±2.0) hours. Cefepime total body clearance decreased proportionally with creatinine clearance in patients with abnormal renal function, which serves as the basis for dosage adjustment recommendations in this group of patients [see Dosage and Administration (2)].
Patients with Hepatic Impairment
The pharmacokinetics of cefepime were unaltered in patients with impaired hepatic function who received a single 1 g dose (n=11).
Geriatric Patients
Cefepime pharmacokinetics have been investigated in elderly (65 years of age and older) men (n=12) and women (n=12) whose mean (SD) creatinine clearance was 74.0 (±15.0) mL/min. There appeared to be a decrease in cefepime total body clearance as a function of creatinine clearance. Therefore, dosage administration of cefepime in the elderly should be adjusted as appropriate if the patient’s creatinine clearance is 60 mL/min or less [see Dosage and Administration (2)].
Pediatric Patients
Cefepime pharmacokinetics have been evaluated in pediatric patients from 2 months to 11 years of age following single and multiple doses on every 8 hours (n=29) and every 12 hours (n=13) schedules. Following a single intravenous dose, total body clearance and the steady-state volume of distribution averaged 3.3 (±1.0) mL/min/kg and 0.3 (±0.1) L/kg, respectively. The urinary recovery of unchanged cefepime was 60.4 (±30.4)% of the administered dose, and the average renal clearance was 2.0 (±1.1) mL/min/kg. There were no significant effects of age or gender (25 male vs. 17 female) on total body clearance or volume of distribution, corrected for body weight. No accumulation was seen when cefepime was given at 50 mg per kg every 12 hours (n=13), while Cmax, AUC, and t1/2 were increased about 15% at steady state after 50 mg per kg every 8 hours. The exposure to cefepime following a 50 mg per kg intravenous dose in a pediatric patient is comparable to that in an adult treated with a 2 g intravenous dose.
12.4 Microbiology
Cefepime is a bactericidal agent that acts by inhibition of bacterial cell wall synthesis. Cefepime has a broad spectrum of in vitro activity that encompasses a wide range of gram-positive and gram-negative bacteria. Cefepime has a low affinity for chromosomally-encoded beta-lactamases. Cefepime is highly resistant to hydrolysis by most beta-lactamases and exhibits rapid penetration into gram-negative bacterial cells. Within bacterial cells, the molecular targets of cefepime are the penicillin binding proteins (PBP).
Cefepime has been shown to be active against most isolates of the following microorganisms, both in vitro and in clinical infections [see Indications and Usage (1)].
-
Aerobic Gram-Negative Microorganisms:
Enterobacter
Escherichia coli
Klebsiella pneumoniae
Proteus mirabilis
Pseudomonas aeruginosa
-
Aerobic Gram-Positive Microorganisms:
Staphylococcus aureus (methicillin-susceptible isolates only)
Streptococcus pneumoniae
Streptococcus pyogenes (Lancefield's Group A streptococci)
Viridans group streptococci
The following in vitro data are available, but their clinical significance is unknown. Cefepime has been shown to have in vitro activity against most isolates of the following microorganisms; however, the safety and effectiveness of cefepime in treating clinical infections due to these microorganisms have not been established in adequate and well-controlled trials.
-
Aerobic Gram-Positive Microorganisms:
Staphylococcus epidermidis (methicillin-susceptible isolates only)
Staphylococcus saprophyticus
Streptococcus agalactiae (Lancefield's Group B streptococci)
NOTE: Most isolates of enterococci, e.g., Enterococcus faecalis, and methicillin-resistant staphylococci are resistant to cefepime.
-
Aerobic Gram-Negative Microorganisms:
Acinetobacter calcoaceticus subsp. lwoffii
Citrobacter diversus
Citrobacter freundii
Enterobacter agglomerans
Haemophilus influenzae (including beta-lactamase producing isolates)
Hafnia alvei
Klebsiella oxytoca
Moraxella catarrhalis (including beta-lactamase producing isolates)
Morganella morganii
Proteus vulgaris
Providencia rettgeri
Providencia stuartii
Serratia marcescens
NOTE: Cefepime is inactive against many isolates of Stenotrophomonas (formerly Xanthomonas maltophilia and Pseudomonas maltophilia).
- Anaerobic Microorganisms:
NOTE: Cefepime is inactive against most isolates of Clostridium difficile.
Susceptibility Tests
Dilution Techniques
Quantitative methods are used to determine antimicrobial minimum inhibitory concentrations (MICs). These MICs provide estimates of the susceptibility of bacteria to antimicrobial compounds. The MICs should be determined using a standardized procedure. Standardized procedures are based on a dilution method2 (broth or agar) or equivalent with standardized inoculum concentrations and standardized concentrations of cefepime powder. The MIC values should be interpreted according to the following criteria:
| MIC (mcg/mL) | |||
|---|---|---|---|
| Microorganism | Susceptible (S) | Intermediate (I) | Resistant (R) |
|
|||
| Microorganisms other than Haemophilus spp.* and S. pneumoniae* | ≤8 | 16 | ≥32 |
| Haemophilus spp.* | ≤2 | –* | –* |
| Streptococcus pneumoniae* | ≤0.5 | 1 | ≥2 |
A report of "Susceptible" indicates that the pathogen is likely to be inhibited if the antimicrobial compound in the blood reaches the concentrations usually achievable. A report of "Intermediate" indicates that the result should be considered equivocal, and, if the microorganism is not fully susceptible to alternative, clinically feasible drugs, the test should be repeated. This category implies possible clinical applicability in body sites where the drug is physiologically concentrated or in situations where high dosage of drug can be used. This category also provides a buffer zone which prevents small uncontrolled technical factors from causing major discrepancies in interpretation. A report of "Resistant" indicates that the pathogen is not likely to be inhibited if the antimicrobial compound in the blood reaches the concentrations usually achievable; other therapy should be selected.
Standardized susceptibility test procedures require the use of laboratory control microorganisms to control the technical aspects of the laboratory procedures. Laboratory control microorganisms are specific strains of microbiological assay organisms with intrinsic biological properties relating to resistance mechanisms and their genetic expression within bacteria; the specific strains are not clinically significant in their current microbiological status. Standard cefepime powder should provide the following MIC values (Table 9) when tested against the designated quality control strains:
| Microorganism | ATCC | MIC (mcg/mL) |
|---|---|---|
| Escherichia coli | 25922 | 0.016–0.12 |
| Staphylococcus aureus | 29213 | 1–4 |
| Pseudomonas aeruginosa | 27853 | 1–4 |
| Haemophilus influenzae | 49247 | 0.5–2 |
| Streptococcus pneumoniae | 49619 | 0.06–0.25 |
Diffusion Techniques
Quantitative methods that require measurement of zone diameters also provide reproducible estimates of the susceptibility of bacteria to antimicrobial compounds. One such standardized procedure3 requires the use of standardized inoculum concentrations. This procedure uses paper disks impregnated with 30 mcg of cefepime to test the susceptibility of microorganisms to cefepime. Interpretation is identical to that stated above for results using dilution techniques.
Reports from the laboratory providing results of the standard single-disk susceptibility test with a 30-mcg cefepime disk should be interpreted according to the following criteria:
| Zone Diameter (mm) | |||
|---|---|---|---|
| Microorganism | Susceptible (S) | Intermediate (I) | Resistant (R) |
|
|||
| Microorganisms other than Haemophilus spp.* and S. pneumoniae* | ≥18 | 15–17 | ≤14 |
| Haemophilus spp.* | ≥26 | –* | –* |
As with standardized dilution techniques, diffusion methods require the use of laboratory control microorganisms to control the technical aspects of the laboratory procedures. Laboratory control microorganisms are specific strains of microbiological assay organisms with intrinsic biological properties relating to resistance mechanisms and their genetic expression within bacteria; the specific strains are not clinically significant in their current microbiological status. For the diffusion technique, the 30-mcg cefepime disk should provide the following zone diameters in these laboratory test quality control strains (Table 11):
| Microorganism | ATCC | Zone Size Range (mm) |
|---|---|---|
| Escherichia coli | 25922 | 29–35 |
| Staphylococcus aureus | 25923 | 23–29 |
| Pseudomonas aeruginosa | 27853 | 24–30 |
| Haemophilus influenzae | 49247 | 25–31 |
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
No long-term animal carcinogenicity studies have been conducted with cefepime. A battery of in vivo and in vitro genetic toxicity tests, including the Ames Salmonella reverse mutation assay, CHO/HGPRT mammalian cell forward gene mutation assay, chromosomal aberration and sister chromatid exchange assays in human lymphocytes, CHO fibroblast clastogenesis assay, and cytogenetic and micronucleus assays in mice were conducted. The overall conclusion of these tests indicated no definitive evidence of genotoxic potential. No untoward effects on fertility were observed in rats when cefepime was administered subcutaneously at doses up to 1000 mg/kg/day (1.6 times the recommended maximum human dose calculated on a mg/m2 basis).
14 CLINICAL STUDIES
14.1 Febrile Neutropenic Patients
The safety and efficacy of empiric cefepime monotherapy of febrile neutropenic patients have been assessed in two multicenter, randomized trials, comparing cefepime monotherapy (at a dose of 2 g intravenously every 8 hours) to ceftazidime monotherapy (at a dose of 2 g intravenously every 8 hours). These studies comprised 317 evaluable patients. Table 12 describes the characteristics of the evaluable patient population.
| Cefepime | Ceftazidime | |
|---|---|---|
| Total | 164 | 153 |
| ANC = absolute neutrophil count; SBP = systolic blood pressure. | ||
| Median age (yr) | 56 (range, 18-82) | 55 (range, 16-84) |
| Male | 86 (52%) | 85 (56%) |
| Female | 78 (48%) | 68 (44%) |
| Leukemia | 65 (40%) | 52 (34%) |
| Other hematologic malignancies | 43 (26%) | 36 (24%) |
| Solid tumor | 54 (33%) | 56 (37%) |
| Median ANC nadir (cells per microliter) | 20 (range, 0-500) | 20 (range, 0-500) |
| Median duration of neutropenia (days) | 6 (range, 0-39) | 6 (range, 0-32) |
| Indwelling venous catheter | 97 (59%) | 86 (56%) |
| Prophylactic antibiotics | 62 (38%) | 64 (42%) |
| Bone marrow graft | 9 (5%) | 7 (5%) |
| SBP less than 90 mm Hg at entry | 7 (4%) | 2 (1%) |
Table 13 describes the clinical response rates observed. For all outcome measures, cefepime was therapeutically equivalent to ceftazidime.
| % Response | ||
|---|---|---|
| Cefepime | Ceftazidime | |
| Outcome Measures | (n = 164) | (n = 153) |
| Primary episode resolved with no treatment modification, no new febrile episodes or infection, and oral antibiotics allowed for completion of treatment | 51 | 55 |
| Primary episode resolved with no treatment modification, no new febrile episodes or infection, and no post-treatment oral antibiotics | 34 | 39 |
| Survival, any treatment modification allowed | 93 | 97 |
| Primary episode resolved with no treatment modification and oral antibiotics allowed for completion of treatment | 62 | 67 |
| Primary episode resolved with no treatment modification and no post-treatment oral antibiotics | 46 | 51 |
Insufficient data exist to support the efficacy of cefepime monotherapy in patients at high risk for severe infection (including patients with a history of recent bone marrow transplantation, with hypotension at presentation, with an underlying hematologic malignancy, or with severe or prolonged neutropenia). No data are available in patients with septic shock.
14.2 Complicated Intra-abdominal Infections
Patients hospitalized with complicated intra-abdominal infections participated in a randomized, double-blind, multicenter trial comparing the combination of cefepime (2 g every 12 hours) plus intravenous metronidazole (500 mg every 6 hours) versus imipenem/cilastatin (500 mg every 6 hours) for a maximum duration of 14 days of therapy. The study was designed to demonstrate equivalence of the two therapies. The primary analyses were conducted on the protocol-valid population, which consisted of those with a surgically confirmed complicated infection, at least one pathogen isolated pretreatment, at least 5 days of treatment, and a 4-6 week follow-up assessment for cured patients. Subjects in the imipenem/cilastatin arm had higher APACHE II scores at baseline. The treatment groups were otherwise generally comparable with regard to their pretreatment characteristics. The overall clinical cure rate among the protocol-valid patients was 81% (51 cured/63 evaluable patients) in the cefepime plus metronidazole group and 66% (62/94) in the imipenem/cilastatin group. The observed differences in efficacy may have been due to a greater proportion of patients with high APACHE II scores in the imipenem/cilastatin group.
15 REFERENCES
- (1)
- Cockcroft DW, Gault MH. Prediction of creatinine clearance from serum creatinine. Nephron. 1976; 16:31-41.
- (2)
- National Committee for Clinical Laboratory Standards. Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria that Grow Aerobically—Third Edition. Approved Standard NCCLS Document M7-A3, Vol. 13, No. 25, NCCLS, Villanova, PA, December 1993.
- (3)
- National Committee for Clinical Laboratory Standards. Performance Standards for Antimicrobial Disk Susceptibility Tests—Fifth Edition. Approved Standard NCCLS Document M2-A5, Vol. 13, No. 24, NCCLS, Villanova, PA, December 1993.
16 HOW SUPPLIED/STORAGE AND HANDLING
Cefepime Injection is supplied as a frozen, iso-osmotic, sterile, nonpyrogenic solution in 50 mL and 100 mL single-dose GALAXY containers (PL 2040 Plastic) as follows:
|
|||
| 2G3578 | NDC 0338-1301-41 | 1 g* in 50 mL | Supplied 24/box |
| 2G3579 | NDC 0338-1301-48 | 2 g* in 100 mL | Supplied 12/box |
Store at or below –20°C (-4°F).
Thaw frozen container at room temperature 25°C (77°F) or under refrigeration 5°C (41°F). Do not force thaw by immersion in water baths or by microwave irradiation.
The thawed solution remains stable for 7 days under refrigeration 5°C (41°F) or 24 hours at room temperature 25°C (77°F). Do not refreeze.
[See Dosage and Administration (2.4)].
17 PATIENT COUNSELING INFORMATION
- Patients should be counseled that antibacterial drugs including Cefepime Injection should only be used to treat bacterial infections. They do not treat viral infections (e.g., the common cold). When Cefepime Injection is prescribed to treat a bacterial infection, patients should be told that although it is common to feel better early in the course of therapy, the medication should be taken exactly as directed. Skipping doses or not completing the full course of therapy may (1) decrease the effectiveness of the immediate treatment and (2) increase the likelihood that bacteria will develop resistance and will not be treatable by Cefepime Injection or other antibacterial drugs in the future.
- Patients should be advised of neurological adverse events that could occur with Cefepime Injection use. Patients should be instructed to inform their healthcare provider at once of any neurological signs and symptoms including encephalopathy (disturbance of consciousness including confusion, hallucinations, stupor, and coma), myoclonus and seizures for immediate treatment, dosage adjustment, or discontinuation of Cefepime Injection.
- Diarrhea is a common problem caused by antibiotics which usually ends when the antibiotic is discontinued. Sometimes after starting treatment with antibiotics, patients can develop watery and bloody stools (with or without stomach cramps and fever) even as late as two or more months after having taken the last dose of the antibiotic. If this occurs, patients should be instructed to contact their physician as soon as possible.
Manufactured by:
Baxter Healthcare Corporation
Deerfield, IL 60015
Baxter and Galaxy are trademarks of Baxter International Inc.
CLINITEST is a registered trademark of Miles, Inc.
CLINISTIX is a registered trademark of Bayer Corporation.
| Cefepime (cefepime hydrochloride) | ||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
| Cefepime (cefepime hydrochloride) | ||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
Revised: 08/2008Baxter