FLUMIST
-
influenza a virus a/california/7/2009 (h1n1) live(attenuated) antigen,
influenza a virus a/perth/16/2009 (h3n2) live(attenuated) antigen and
influenza b virus b/brisbane/60/2008 live(attenuated) antigen spray
MedImmune, LLC
----------
|
||||||||||||||||||||||||||||||||||||
FULL PRESCRIBING INFORMATION
1 INDICATIONS AND USAGE
FluMist is a vaccine indicated for the active immunization of individuals 2-49 years of age against influenza disease caused by influenza virus subtypes A and type B contained in the vaccine.
2 DOSAGE AND ADMINISTRATION
FOR INTRANASAL ADMINISTRATION BY A HEALTH CARE PROVIDER.
2.1 Dosing Information
FluMist should be administered according to the following schedule:
|
||
| Age Group | Vaccination Status | Dosage Schedule |
| Children age 2 years through 8 years | Not previously vaccinated with influenza vaccine | 2 doses (0.2 mL* each, at least 1 month apart) |
| Children age 2 years through 8 years | Previously vaccinated with influenza vaccine | 1 dose (0.2 mL*) |
| Children, adolescents, and adults age 9 through 49 years | Not applicable | 1 dose (0.2 mL*) |
For children age 2 years through 8 years who have not previously received influenza vaccine, the recommended dosage schedule for nasal administration is one 0.2 mL dose (0.1 mL per nostril), followed by a second 0.2 mL dose (0.1 mL per nostril) given at least 1 month later.
For all other individuals, including children age 2-8 years who have previously received influenza vaccine, the recommended schedule is one 0.2 mL dose (0.1 mL per nostril).
FluMist should be administered prior to exposure to influenza. Annual revaccination with influenza vaccine is recommended.
2.2 Administration Instructions
Each sprayer contains a single dose of FluMist; approximately one-half of the contents should be administered into each nostril. Refer to the administration diagram (Figure 1) for step-by-step administration instructions. Once FluMist has been administered, the sprayer should be disposed of according to the standard procedures for medical waste (e.g., sharps container or biohazard container).
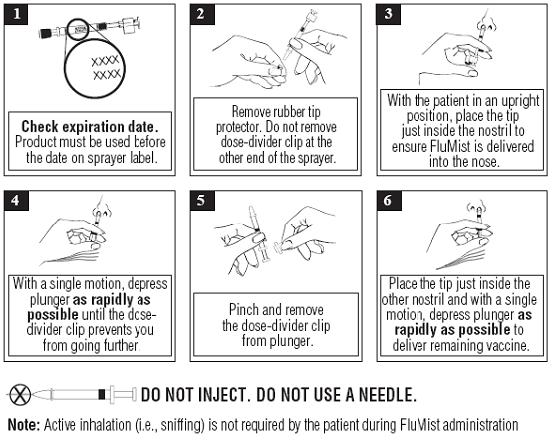
Figure 1
3 DOSAGE FORMS AND STRENGTHS
0.2 mL pre-filled, single-use intranasal spray.
Each 0.2 mL dose of FluMist is formulated to contain 106.5-7.5 FFU (fluorescent focus units) of each of three live attenuated influenza virus reassortants: A/California/7/2009 (H1N1), A/Perth/16/2009 (H3N2), and B/Brisbane/60/2008.
4 CONTRAINDICATIONS
4.1 Hypersensitivity
FluMist is contraindicated in individuals with a history of hypersensitivity, especially anaphylactic reactions, to eggs, egg proteins, gentamicin, gelatin, or arginine, or with life-threatening reactions to previous influenza vaccinations.
4.2 Concomitant Pediatric and Adolescent Aspirin Therapy and Reye’s Syndrome
FluMist is contraindicated in children and adolescents (2-17 years of age) receiving aspirin therapy or aspirin-containing therapy because of the association of Reye’s syndrome with aspirin and wild-type influenza infection.
5 WARNINGS AND PRECAUTIONS
5.1 Risks in Children <24 Months of Age
Do not administer FluMist to children <24 months of age. In clinical trials, an increased risk of wheezing post-vaccination was observed in FluMist recipients <24 months of age. An increase in hospitalizations was observed in children <24 months of age after vaccination with FluMist. [See Adverse Reactions (6.1).]
5.2 Asthma/Recurrent Wheezing
FluMist should not be administered to any individuals with asthma or children < 5 years of age with recurrent wheezing because of the potential for increased risk of wheezing post vaccination unless the potential benefit outweighs the potential risk.
Do not administer FluMist to individuals with severe asthma or active wheezing because these individuals have not been studied in clinical trials.
5.3 Guillain-Barré Syndrome
If Guillain-Barré syndrome has occurred within 6 weeks of any prior influenza vaccination, the decision to give FluMist should be based on careful consideration of the potential benefits and potential risks [see also Adverse Reactions (6.2)].
5.4 Altered Immunocompetence
Data supporting the safety and effectiveness of FluMist administration in immunocompromised individuals are limited to 174 individuals with HIV infection and 10 mild to moderately immunocompromised children and adolescents with cancer [see Clinical Studies (14.3)].
5.5 Medical Conditions Predisposing to Influenza Complications
The safety of FluMist in individuals with underlying medical conditions that may predispose them to complications following wild-type influenza infection has not been established. FluMist should not be administered unless the potential benefit outweighs the potential risk.
5.6 Management of Acute Allergic Reactions
Appropriate medical treatment and supervision must be available to manage possible anaphylactic reactions following administration of the vaccine [see Contraindications (4.1)].
6 ADVERSE REACTIONS
FluMist is not indicated in children <24 months of age. In a clinical trial, among children 6-23 months of age, wheezing requiring bronchodilator therapy or with significant respiratory symptoms occurred in 5.9% of FluMist recipients compared to 3.8% of active control (injectable influenza vaccine made by Sanofi Pasteur Inc.) recipients (Relative Risk 1.5, 95% CI: 1.2, 2.1). Wheezing was not increased in children ≥24 months of age.
Hypersensitivity, including anaphylactic reaction, has been reported post-marketing.
[See Warnings and Precautions (5.1) and Adverse Reactions (6.1, 6.2).]
6.1 Adverse Reactions in Clinical Trials
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a vaccine cannot be directly compared to rates in the clinical trials of another vaccine and may not reflect the rates observed in practice.
A total of 9537 children and adolescents 1-17 years of age and 3041 adults 18-64 years of age received FluMist in randomized, placebo-controlled Studies D153-P501, AV006, D153-P526, AV019, and AV009 described below. In addition, 4179 children 6-59 months of age received FluMist in Study MI-CP111, a randomized, active-controlled trial. Among pediatric FluMist recipients 6 months-17 years of age, 50% were female; in the study of adults, 55% were female. In MI-CP111, AV006, D153-P526, AV019, and AV009, subjects were White (71%), Hispanic (11%), Asian (7%), Black (6%), and Other (5%), while in D153-P501, 99% of subjects were Asian.
Adverse Reactions in Children and Adolescents
In a placebo-controlled safety study (AV019) conducted in a large Health Maintenance Organization (HMO) in children 1-17 years of age (n = 9689), an increase in asthma events, captured by review of diagnostic codes, was observed in children <5 years of age (Relative Risk 3.53, 90% CI: 1.1, 15.7). This observation was prospectively evaluated in Study MI-CP111.
In MI-CP111, an active-controlled study, increases in wheezing and hospitalization (for any cause) were observed in children <24 months of age, as shown in Table 1.
| Adverse Reaction | Age Group | FluMist | Active Control* |
| Hospitalizations†
| 6-23 months (n = 3967) | 4.2 % | 3.2 % |
| 24-59 months (n = 4385) | 2.1 % | 2.5 % | |
| Wheezing‡ | 6-23 months (n = 3967) | 5.9 % | 3.8 % |
| 24-59 months (n = 4385) | 2.1 % | 2.5 % | |
Most hospitalizations observed were gastrointestinal and respiratory tract infections and occurred more than 6 weeks post vaccination. In post-hoc analysis, rates of hospitalization in children 6-11 months of age (n = 1376) were 6.1% in FluMist recipients and 2.6% in active control recipients.
Table 2 shows an analysis of pooled solicited events, occurring in at least 1% of FluMist recipients and at a higher rate compared to placebo, post Dose 1 for Study D153-P501 and AV006, and solicited events post Dose 1 for Study MI-CP111. Solicited events were those about which parents/guardians were specifically queried after vaccination with FluMist. In these studies, solicited events were documented for 10 days post vaccination. Solicited events post Dose 2 for FluMist were similar to those post Dose 1 and were generally observed at a lower frequency.
|
||||
| D153-P501 & AV006 | MI-CP111 | |||
| FluMist | Placebo | FluMist | Active Control† | |
| N=876-1759‡ | N=424-1034‡ | N=2170‡ | N=2165‡ | |
| Event | % | % | % | % |
| Runny Nose/ Nasal Congestion | 58 | 50 | 51 | 42 |
| Decreased Appetite | 21 | 17 | 13 | 12 |
| Irritability | 21 | 19 | 12 | 11 |
| Decreased Activity (Lethargy) | 14 | 11 | 7 | 6 |
| Sore Throat | 11 | 9 | 5 | 6 |
| Headache | 9 | 7 | 3 | 3 |
| Muscle Aches | 6 | 3 | 2 | 2 |
| Chills | 4 | 3 | 2 | 2 |
| Fever | ||||
| 100-101°F Oral | 9 | 6 | 6 | 4 |
| 101-102°F Oral | 4 | 3 | 4 | 3 |
In clinical studies D153-P501 and AV006, other adverse reactions in children occurring in at least 1% of FluMist recipients and at a higher rate compared to placebo were: abdominal pain (2% FluMist vs. 0% placebo) and otitis media (3% FluMist vs. 1% placebo).
An additional adverse reaction identified in the active-controlled trial MI-CP111, occurring in at least 1% of FluMist recipients and at a higher rate compared to active control, was sneezing (2% FluMist vs. 1% active control).
In a separate trial (MI-CP112) that compared the refrigerated and frozen formulations of FluMist in children and adults 5-49 years of age, the solicited events and other adverse events were consistent with observations from previous trials. Fever of >103°F was observed in 1 to 2% of children 5-8 years of age.
In a separate placebo-controlled trial (D153-P526) using the refrigerated formulation in a subset of older children and adolescents 9-17 years of age who received one dose of FluMist, the solicited events and other adverse events were generally consistent with observations from previous trials. Abdominal pain was reported in 12% of FluMist recipients compared to 4% of placebo recipients and decreased activity was reported in 6% of FluMist recipients compared to 0% of placebo recipients.
Adverse Reactions in Adults
In adults 18-49 years of age in Study AV009, summary of solicited adverse events occurring in at least 1% of FluMist recipients and at a higher rate compared to placebo include runny nose (44% FluMist vs. 27% placebo), headache (40% FluMist vs. 38% placebo), sore throat (28% FluMist vs. 17% placebo), tiredness/weakness (26% FluMist vs. 22% placebo), muscle aches (17% FluMist vs. 15% placebo), cough (14% FluMist vs. 11% placebo), and chills (9% FluMist vs. 6% placebo).
In addition to the solicited events, other adverse reactions from Study AV009 occurring in at least 1% of FluMist recipients and at a higher rate compared to placebo were: nasal congestion (9% FluMist vs. 2% placebo) and sinusitis (4% FluMist vs. 2% placebo).
6.2 Postmarketing Experience
The following adverse reactions have been identified during postapproval use of FluMist. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to vaccine exposure.
Cardiac disorders: Pericarditis
Congenital, familial, and genetic disorders: Exacerbation of symptoms of mitochondrial encephalomyopathy (Leigh syndrome)
Gastrointestinal disorders: Nausea, vomiting, diarrhea
Immune system disorders: Hypersensitivity reactions (including anaphylactic reaction, facial edema, and urticaria)
Nervous system disorders: Guillain-Barré syndrome, Bell’s Palsy, meningitis, eosinophilic meningitis, vaccine-associated encephalitis
Respiratory, thoracic, and mediastinal disorders: Epistaxis
Skin and subcutaneous tissue disorders: Rash
7 DRUG INTERACTIONS
7.1 Aspirin Therapy
Do not administer FluMist to children or adolescents who are receiving aspirin therapy or aspirin-containing therapy [see Contraindications (4.2)]. Avoid aspirin-containing therapy in these age groups during the first 4 weeks after vaccination with FluMist unless medically indicated.
7.2 Antiviral Agents Against Influenza A and/or B
The concurrent use of FluMist with antiviral agents that are active against influenza A and/or B viruses has not been evaluated. However, based upon the potential for antiviral agents to reduce the effectiveness of FluMist, do not administer FluMist until 48 hours after the cessation of antiviral therapy, and antiviral agents should not be administered until two weeks after administration of FluMist unless medically indicated. If antiviral agents and FluMist are administered concomitantly, revaccination should be considered when appropriate.
7.3 Concomitant Inactivated Vaccines
The safety and immunogenicity of FluMist when administered concurrently with inactivated vaccines have not been determined. Studies of FluMist excluded subjects who received any inactivated or subunit vaccine within two weeks of enrollment. Therefore, healthcare providers should consider the risks and benefits of concurrent administration of FluMist with inactivated vaccines.
7.4 Concomitant Live Vaccines
Concurrent administration of FluMist with the measles, mumps, and rubella vaccine and the varicella vaccine was studied in 1245 children 12-15 months of age. Adverse events were similar to those seen in other clinical trials with FluMist [see Adverse Reactions (6.1)]. No evidence of interference with immune responses to measles, mumps, rubella, varicella, and FluMist vaccines was observed. Concurrent administration of FluMist with the measles, mumps, and rubella vaccine and the varicella vaccine in children >15 months of age has not been studied.
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category C
Animal reproduction studies have not been conducted with FluMist. It is not known whether FluMist can cause fetal harm when administered to a pregnant woman or can affect reproduction capacity. FluMist should be given to a pregnant woman only if clearly needed.
The effect of the vaccine on embryo-fetal and pre-weaning development was evaluated in a developmental toxicity study using pregnant rats receiving the frozen formulation. Groups of animals were administered the vaccine either once (during the period of organogenesis on gestation day 6) or twice (prior to gestation and during the period of organogenesis on gestation day 6), 250 microliter/rat/occasion (approximately 110-140 human dose equivalents), by intranasal instillation. No adverse effects on pregnancy, parturition, lactation, embryo-fetal or pre-weaning development were observed. There were no vaccine-related fetal malformations or other evidence of teratogenesis noted in this study.
8.3 Nursing Mothers
It is not known whether FluMist is excreted in human milk. Therefore, as some viruses are excreted in human milk, caution should be exercised if FluMist is administered to nursing mothers.
8.4 Pediatric Use
Safety and effectiveness of the vaccine has been demonstrated for children 2 years of age and older with reduction in culture-confirmed influenza rates compared to active control (injectable influenza vaccine made by Sanofi Pasteur Inc.) and placebo [see Clinical Studies (14.1)]. FluMist is not approved for use in children <24 months of age. FluMist use in children <24 months has been associated with increased risk of hospitalization and wheezing in clinical trials [see Warnings and Precautions (5.1) and Adverse Reactions (6.1)].
8.5 Geriatric Use
FluMist is not approved for use in individuals ≥65 years of age. Subjects with underlying high-risk medical conditions (n = 200) were studied for safety. Compared to controls, FluMist recipients had a higher rate of sore throat.
8.6 Use in Individuals 50-64 Years of Age
FluMist is not approved for use in individuals 50-64 years of age. In Study AV009, effectiveness was not demonstrated in individuals 50-64 years of age (n = 641). Solicited adverse events were similar in type and frequency to those reported in younger adults.
11 DESCRIPTION
FluMist (Influenza Vaccine Live, Intranasal) is a live trivalent vaccine for administration by intranasal spray. The influenza virus strains in FluMist are (a) cold-adapted (ca) (i.e., they replicate efficiently at 25°C, a temperature that is restrictive for replication of many wild-type influenza viruses); (b) temperature-sensitive (ts) (i.e., they are restricted in replication at 37°C (Type B strains) or 39°C (Type A strains), temperatures at which many wild-type influenza viruses grow efficiently); and (c) attenuated (att) (they do not produce classic influenza-like illness in the ferret model of human influenza infection). The cumulative effect of the antigenic properties and the ca, ts, and att phenotypes is that the attenuated vaccine viruses replicate in the nasopharynx to induce protective immunity.
No evidence of reversion has been observed in the recovered vaccine strains that have been tested (135 of possible 250 recovered isolates) [see Clinical Studies (14.5)]. For each of the three reassortant strains in FluMist, the six internal gene segments responsible for ca, ts, and att phenotypes are derived from a master donor virus (MDV), and the two segments that encode the two surface glycoproteins, hemagglutinin (HA) and neuraminidase (NA), are derived from the corresponding antigenically relevant wild-type influenza viruses that have been recommended by the USPHS for inclusion in the annual vaccine formulation. Thus, the three viruses contained in FluMist maintain the replication characteristics and phenotypic properties of the MDV and express the HA and NA of wild-type viruses that are related to strains expected to circulate during the 2011-2012 influenza season. For the Type A MDV, at least five genetic loci in three different internal gene segments contribute to the ts and att phenotypes. For the Type B MDV, at least three genetic loci in two different internal gene segments contribute to both the ts and att properties; five genetic loci in three gene segments control the ca property.
Specific pathogen-free (SPF) eggs are inoculated with each of the reassortant strains and incubated to allow vaccine virus replication. The allantoic fluid of these eggs is harvested, pooled, and then clarified by filtration. The virus is concentrated by ultracentrifugation and diluted with stabilizing buffer to obtain the final sucrose and potassium phosphate concentrations. Ethylene diamine tetraacetic acid (EDTA) is added to the dilution buffer for H3N2 strains. The viral harvests are then sterile filtered to produce the monovalent bulks. Each lot is tested for ca, ts, and att phenotypes and is also tested extensively by in vitro and in vivo methods to detect adventitious agents. Monovalent bulks from the three strains are subsequently blended and diluted as required to attain the desired potency with stabilizing buffers to produce the trivalent bulk vaccine. The bulk vaccine is then filled directly into individual sprayers for nasal administration.
Each pre-filled refrigerated FluMist sprayer contains a single 0.2 mL dose. Each 0.2 mL dose contains 106.5-7.5 FFU of live attenuated influenza virus reassortants of each of the three strains: A/California/7/2009 (H1N1), A/Perth/16/2009 (H3N2), and B/Brisbane/60/2008. Each 0.2 mL dose also contains 0.188 mg/dose monosodium glutamate, 2.00 mg/dose hydrolyzed porcine gelatin, 2.42 mg/dose arginine, 13.68 mg/dose sucrose, 2.26 mg/dose dibasic potassium phosphate, 0.96 mg/dose monobasic potassium phosphate, and <0.015 mcg/mL gentamicin sulfate. FluMist contains no preservatives.
The tip attached to the sprayer is equipped with a nozzle that produces a fine mist that is primarily deposited in the nose and nasopharynx. FluMist is a colorless to pale yellow liquid and is clear to slightly cloudy.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Immune mechanisms conferring protection against influenza following receipt of FluMist vaccine are not fully understood. Likewise, naturally acquired immunity to wild-type influenza has not been completely elucidated. Serum antibodies, mucosal antibodies, and influenza-specific T cells may play a role in prevention and recovery from infection.
Influenza illness and its complications follow infection with influenza viruses. Global surveillance of influenza identifies yearly antigenic variants. For example, since 1977, antigenic variants of influenza A (H1N1 and H3N2) viruses and influenza B viruses have been in global circulation. Antibody against one influenza virus type or subtype confers limited or no protection against another. Furthermore, antibody to one antigenic variant of influenza virus might not protect against a new antigenic variant of the same type or subtype. Frequent development of antigenic variants through antigenic drift is the virologic basis for seasonal epidemics and the reason for the usual change of one or more new strains in each year’s influenza vaccine. Therefore, influenza vaccines are standardized to contain the strains (i.e., typically two type A and one type B), representing the influenza viruses likely to be circulating in the United States in the upcoming winter.
Annual revaccination with the current vaccine is recommended because immunity declines during the year after vaccination, and because circulating strains of influenza virus change from year to year [1].
12.3 Pharmacokinetics
Biodistribution
A biodistribution study of intranasally administered radiolabeled placebo was conducted in 7 healthy adult volunteers. The mean percentage of the delivered doses detected were as follows: nasal cavity 89.7%, stomach 2.6%, brain 2.4%, and lung 0.4%. The clinical significance of these findings is unknown.
14 CLINICAL STUDIES
FluMist, in refrigerated and frozen formulations, was administered to approximately 35,000 subjects in controlled clinical studies. FluMist has been studied in placebo-controlled trials over multiple years, using different vaccine strains. Safety and efficacy have been studied where FluMist was compared to an inactivated influenza vaccine made by Sanofi Pasteur Inc. among children as young as 6 months of age. FluMist is not approved for use in children < 24 months of age [see Adverse Reactions (6)].
14.1 Studies in Children and Adolescents
Study MI-CP111: Pediatric Comparative Study
A multinational, randomized, double-blind, active-controlled trial (MI-CP111) was performed to assess the efficacy and safety of FluMist compared to an injectable influenza vaccine made by Sanofi Pasteur Inc. (active control) in children <5 years of age, using the refrigerated formulation. During the 2004-2005 influenza season, a total number of 3916 children <5 years of age and without severe asthma, without use of bronchodilator or steroids, and without wheezing within the prior 6 weeks were randomized to FluMist and 3936 were randomized to active control. Participants were then followed through the influenza season to identify illness caused by influenza virus. As the primary endpoint, culture-confirmed modified CDC-ILI (CDC-defined influenza-like illness) was defined as a positive culture for a wild-type influenza virus associated within ±7 days of modified CDC-ILI. Modified CDC-ILI was defined as fever (temperature ≥100°F oral or equivalent) plus cough, sore throat, or runny nose/nasal congestion on the same or consecutive days.
In the primary efficacy analysis, FluMist demonstrated a 44.5% (95% CI: 22.4, 60.6) reduction in influenza rate compared to active control as measured by culture-confirmed modified CDC-ILI caused by wild-type strains antigenically similar to those contained in the vaccine. See Table 3 for a description of the results by strain and antigenic similarity.
|
||||||||
| FluMist | Active Control† | % | ||||||
| N | # of Cases | Rate
(cases/N) | N | # of Cases | Rate
(cases/N) | Reduction in Rate for FluMist‡ | 95% CI | |
| Matched Strains | ||||||||
| All strains | 3916 | 53 | 1.4% | 3936 | 93 | 2.4% | 44.5% | 22.4, 60.6 |
| A/H1N1 | 3916 | 3 | 0.1% | 3936 | 27 | 0.7% | 89.2% | 67.7, 97.4 |
| A/H3N2 | 3916 | 0 | 0.0% | 3936 | 0 | 0.0% | -- | -- |
| B | 3916 | 50 | 1.3% | 3936 | 67 | 1.7% | 27.3% | -4.8, 49.9 |
| Mismatched Strains | ||||||||
| All strains | 3916 | 102 | 2.6% | 3936 | 245 | 6.2% | 58.2% | 47.4, 67.0 |
| A/H1N1 | 3916 | 0 | 0.0% | 3936 | 0 | 0.0% | -- | -- |
| A/H3N2 | 3916 | 37 | 0.9% | 3936 | 178 | 4.5% | 79.2% | 70.6, 85.7 |
| B | 3916 | 66 | 1.7% | 3936 | 71 | 1.8% | 6.3% | -31.6, 33.3 |
| Regardless of Match | ||||||||
| All strains | 3916 | 153 | 3.9% | 3936 | 338 | 8.6% | 54.9% | 45.4, 62.9 |
| A/H1N1 | 3916 | 3 | 0.1% | 3936 | 27 | 0.7% | 89.2% | 67.7, 97.4 |
| A/H3N2 | 3916 | 37 | 0.9% | 3936 | 178 | 4.5% | 79.2% | 70.6, 85.7 |
| B | 3916 | 115 | 2.9% | 3936 | 136 | 3.5% | 16.1% | -7.7, 34.7 |
| ATP Population. | ||||||||
Study D153-P501: Pediatric Study
A randomized, double-blind, placebo-controlled trial (D153-P501) was performed to evaluate the efficacy of FluMist in children 12 to 35 months of age without high-risk medical conditions against culture-confirmed influenza illness, using the refrigerated formulation. A total of 3174 children were randomized 3:2 (vaccine: placebo) to receive 2 doses of study vaccine or placebo at least 28 days apart in Year 1. See Table 4 for a description of the results.
Study AV006: Pediatric Study
AV006 was a multi-center, randomized, double-blind, placebo-controlled trial performed in U.S. children without high-risk medical conditions to evaluate the efficacy of FluMist against culture-confirmed influenza over two successive seasons using the frozen formulation. The primary endpoint of the trial was the prevention of culture-confirmed influenza illness due to antigenically matched wild-type influenza in children who received two doses of vaccine in the first year and a single revaccination dose in the second year. During the first year of the study, 1602 children 15-71 months of age were randomized 2:1 (vaccine: placebo). Approximately 85% of the participants in the first year returned for the second year of the study. In Year 2, children remained in the same treatment group as in year one and received a single dose of FluMist or placebo. See Table 4 for a description of the results.
|
||||||
| D153-P501 | AV006 | |||||
| FluMist
n† (%) | Placebo
n† (%) | % Efficacy
(95% CI) | FluMist
n† (%) | Placebo
n† (%) | % Efficacy
(95% CI) |
|
| N‡=1653 | N‡=1111 | N‡=849 | N‡=410 | |||
| Any strain | 56 (3.4%) | 139 (12.5%) | 72.9%§
(62.8, 80.5) | 10 (1%) | 73 (18%) | 93.4% (87.5, 96.5) |
| A/H1N1 | 23 (1.4%) | 81 (7.3%) | 80.9% (69.4, 88.5)¶ | 0 | 0 | -- |
| A/H3N2 | 4 (0.2%) | 27 (2.4%) | 90.0% (71.4, 97.5) | 4 (0.5%) | 48 (12%) | 96.0% (89.4, 98.5) |
| B | 29 (1.8%) | 35 (3.2%) | 44.3% (6.2, 67.2) | 6 (0.7%) | 31 (7%) | 90.5% (78.0, 95.9) |
During the second year of Study AV006, the primary circulating strain was the A/Sydney/05/97 H3N2 strain, which was antigenically dissimilar from the H3N2 strain represented in the vaccine, A/Wuhan/359/95; FluMist demonstrated 87.0% (95% CI: 77.0, 92.6) efficacy against culture-confirmed influenza illness.
14.2 Study in Adults
AV009 was a multi-center, randomized, double-blind, placebo-controlled trial to evaluate effectiveness in adults 18-64 years of age without high-risk medical conditions. Participants were randomized 2:1 (vaccine: placebo). Cultures for influenza virus were not obtained from subjects in the trial, so that the efficacy against culture-confirmed influenza was not assessed. The A/Wuhan/359/95 (H3N2) strain, which was contained in FluMist, was antigenically distinct from the predominant circulating strain of influenza virus during the trial period, A/Sydney/05/97 (H3N2). Type A/Wuhan (H3N2) and Type B strains also circulated in the U.S. during the study period. The primary endpoint of the trial was the reduction in the proportion of participants with one or more episodes of any febrile illness, and prospective secondary endpoints were severe febrile illness and febrile upper respiratory illness. Effectiveness for any of the three endpoints was not demonstrated in a subgroup of adults 50-64 years of age. Primary and secondary effectiveness endpoints from the age group 18-49 years of age are presented in Table 5. Effectiveness was not demonstrated for the primary endpoint in adults 18-49 years of age.
| Endpoint | FluMist
N=2411† n (%) | Placebo
N=1226† n (%) | Percent Reduction | (95% CI) | |
| Participants with one or more events of:‡ | |||||
| Primary Endpoint: | |||||
| Any febrile illness | 331 (13.73) | 189 (15.42) | 10.9 | (-5.1, 24.4) | |
| Secondary Endpoints: | |||||
| Severe febrile illness | 250 (10.37) | 158 (12.89) | 19.5 | (3.0, 33.2) | |
| Febrile upper respiratory illness | 213 (8.83) | 142 (11.58) | 23.7 | (6.7, 37.5) | |
Effectiveness was shown in a post-hoc analysis using CDC-ILI in the age group 18-49 years.
14.3 Studies in Immunocompromised Individuals
Safety and shedding of vaccine virus following FluMist administration (frozen formulation) were evaluated in 28 HIV-infected adults [median CD4 cell count of 541 cells/mm3] and 27 HIV-negative adults 18-58 years of age. No serious adverse events were reported during the one-month follow-up period. Vaccine strain (type B) virus was detected in 1 of 28 HIV-infected subjects on Day 5 only, and in none of the HIV-negative FluMist recipients.
Safety and shedding of vaccine virus following FluMist administration (frozen formulation) were also evaluated in children in a randomized (1:1), cross-over, double-blind, placebo-controlled trial in 24 HIV-infected children [median CD4 cell count of 1013 cells/mm3] and 25 HIV-negative children 1-7 years of age, and in a randomized (1:1), open-label, inactivated influenza vaccine-controlled trial in 243 HIV-infected children and adolescents 5-17 years of age receiving stable anti-retroviral therapy. Frequency and duration of vaccine virus shedding in HIV-infected individuals were comparable to that seen in healthy individuals. No adverse effects on HIV viral load or CD4 counts were identified following FluMist administration. In the 5-17 year old age group, one inactivated influenza vaccine recipient and one FluMist recipient experienced pneumonia within 28 days of vaccination (days 17 and 13, respectively). The effectiveness of FluMist in preventing influenza illness in HIV-infected individuals has not been evaluated.
Twenty mild to moderately immunocompromised children and adolescents 5-17 years of age (receiving chemotherapy and/or radiation therapy or who had received chemotherapy in the 12 weeks prior to enrollment) were randomized 1:1 to receive FluMist (frozen formulation) or placebo. Frequency and duration of vaccine virus shedding in these immunocompromised children and adolescents were comparable to that seen in healthy children and adolescents. The effectiveness of FluMist in preventing influenza illness in immunocompromised individuals has not been evaluated.
14.4 Refrigerated Formulation Study
A double-blind, randomized, multi-center trial was conducted to evaluate the comparative immunogenicity and safety of refrigerated and frozen formulations of FluMist in individuals 5 to 49 years of age without high-risk medical conditions. Nine hundred and eighty-one subjects were randomized at a 1:1 ratio to receive either vaccine formulation. Subjects 5-8 years of age received two doses of study vaccine 46-60 days apart; subjects 9-49 years of age received one dose of study vaccine. The study met its primary endpoint. The GMT ratios of refrigerated and frozen formulations (adjusted for baseline serostatus) for H1N1, H3N2, and B strains, respectively, were 1.24, 1.02, and 1.00 in the two dose group and 1.14, 1.12, and 0.96 in the one dose group.
14.5 Shedding Studies
FluMist contains live attenuated influenza viruses that must infect and replicate in cells lining the nasopharynx of the recipient to induce immunity. Vaccine viruses capable of infection and replication can be cultured from nasal secretions obtained from vaccine recipients (shedding).
Shedding of vaccine viruses within 28 days of vaccination was evaluated in 1) multi-center study MI-CP129 which enrolled healthy individuals 6-59 months of age (N = 200); and 2) multi-center study FM026 which enrolled healthy individuals 5-49 years of age (N = 344). In each study, nasal secretions were obtained daily for the first 7 days and every other day through either Day 25 and on Day 28 or through Day 28. In study MI-CP129, individuals with a positive shedding sample at Day 25 or Day 28 were to have additional shedding samples collected every 7 days until culture negative on 2 consecutive samples. Results of these studies are presented in Table 6.
|
|||||
| Age | Number of Subjects | % Shedding* | Peak Titer (TCID50/mL)† | % Shedding After
Day 11 | Day of Last Positive Culture |
| 6 - 23 months‡ | 99 | 89 | < 5 log10 | 7.0 | Day 23§ |
| 24 - 59 months | 100 | 69 | < 5 log10 | 1.0 | Day 25¶ |
| 5 - 8 years | 102 | 50 | < 5 log10 | 2.9 | Day 23# |
| 9 - 17 years | 126 | 29 | < 4 log10 | 1.6 | Day 28# |
| 18 - 49 years | 115 | 20 | < 3 log10 | 0.9 | Day 17# |
The highest proportion of subjects in each group shed one or more vaccine strains on Days 2-3 post-vaccination. After Day 11 among individuals 2-49 years of age (n = 443), virus titers did not exceed 1.5 log10 TCID50/mL.
14.6 Transmission Study
Using the frozen formulation, a prospective, randomized, double-blind, placebo-controlled trial was performed in a daycare setting in children <3 years of age to assess the transmission of vaccine viruses from a vaccinated individual to a non-vaccinated individual. A total of 197 children 8-36 months of age were randomized to receive one dose of FluMist (n = 98) or placebo (n = 99). Virus shedding was evaluated for 21 days by culture of nasal swab specimens. Wild-type A (H3N2) influenza virus was documented to have circulated in the community and in the study population during the trial, whereas Type A (H1N1) and Type B strains did not.
At least one vaccine strain was isolated from 80% of FluMist recipients; strains were recovered from 1-21 days post vaccination (mean duration of 7.6 days ± 3.4 days). The cold-adapted (ca) and temperature-sensitive (ts) phenotypes were preserved in 135 tested of 250 strains isolated at the local laboratory. Ten influenza isolates (9 influenza A, 1 influenza B) were cultured from a total of seven placebo subjects. One placebo subject had mild symptomatic Type B virus infection confirmed as a transmitted vaccine virus by a FluMist recipient in the same playgroup. This Type B isolate retained the ca, ts, and att phenotypes of the vaccine strain and had the same genetic sequence when compared to a Type B virus cultured from a vaccine recipient within the same playgroup. Four of the influenza Type A isolates were confirmed as wild-type A/Panama (H3N2). The remaining isolates could not be further characterized.
Assuming a single transmission event (isolation of the Type B vaccine strain), the probability of a young child acquiring vaccine virus following close contact with a single FluMist vaccinee in this daycare setting was 0.58% (95% CI: 0, 1.7) based on the Reed-Frost model. With documented transmission of one Type B in one placebo subject and possible transmission of Type A viruses in four placebo subjects, the probability of acquiring a transmitted vaccine virus was estimated to be 2.4% (95% CI: 0.13, 4.6) using the Reed-Frost model.
15 REFERENCES
- Centers for Disease Control and Prevention. Prevention and Control of Influenza: Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR 2010; 59(RR-8): 1-62.
16 HOW SUPPLIED/STORAGE AND HANDLING
FluMist is supplied for intranasal delivery in a package of 10 pre-filled, single-use sprayers. The single-use intranasal sprayer contains no latex.
NDC 66019-109-10
Storage and Handling
Once FluMist has been administered, the sprayer should be disposed of according to the standard procedures for medical waste (e.g., sharps container or biohazard container).
FLUMIST SHOULD BE STORED IN A REFRIGERATOR BETWEEN 2-8°C (35-46°F) UPON RECEIPT AND UNTIL USE. THE PRODUCT MUST BE USED BEFORE THE EXPIRATION DATE ON THE SPRAYER LABEL.
DO NOT FREEZE.
The cold chain (2 to 8°C) must be maintained when transporting FluMist.
17 PATIENT COUNSELING INFORMATION
See FDA-approved patient labeling (Information for Patients and Their Caregivers).
Vaccine recipients or their parents/guardians should be informed by the health care provider of the potential benefits and risks of FluMist, and the need for two doses at least 1 month apart in children 2-8 years old who have not previously received influenza vaccine.
17.1 Asthma and Recurrent Wheezing
Ask the vaccinee or their parent/guardian if the vaccinee has asthma. For children <5 years of age, also ask if the vaccinee has recurrent wheezing since this may be an asthma equivalent in this age group.
17.2 Vaccination with a Live Virus Vaccine
Vaccine recipients or their parents/guardians should be informed by the health care provider that FluMist is an attenuated live virus vaccine and has the potential for transmission to immunocompromised household contacts.
17.3 Adverse Event Reporting
The vaccine recipient or the parent/guardian accompanying the vaccine recipient should be told to report any suspected adverse events to the physician or clinic where the vaccine was administered.
FluMist® is a registered trademark of MedImmune, LLC.
Manufactured by:
MedImmune, LLC
Gaithersburg, MD 20878
1-877-633-4411
U.S. Government License No. 1799
Issue Date: May 2011 RAL-FLUV11
INFORMATION FOR PATIENTS AND THEIR CAREGIVERS
FluMist® (pronounced FLEW-mĭst)
(Influenza Vaccine Live, Intranasal)
Please read this Patient Information carefully before you or your child is vaccinated with FluMist.
This is a summary of information about FluMist. It does not take the place of talking with your healthcare provider about influenza vaccination. If you have questions or would like more information, please talk with your healthcare provider.
What is FluMist?
FluMist is a vaccine that is sprayed into the nose to help protect against influenza. It can be used in children, adolescents, and adults ages 2 through 49. FluMist may not prevent influenza in everyone who gets vaccinated.
Who should not get FluMist?
You should not get FluMist if you:
- are allergic to eggs, gentamicin, gelatin, or arginine
- have ever had a life-threatening reaction to influenza vaccinations
- are 2 through 17 years old and take aspirin or medicines containing aspirin. Children or adolescents should not be given aspirin for 4 weeks after getting FluMist unless your healthcare provider tells you otherwise.
Please talk to your healthcare provider if you are not sure if the items listed above apply to you or your child.
Children under 2 years old should not get FluMist because there is a chance they may wheeze (have difficulty with breathing) after getting FluMist.
Who may not be able to get FluMist?
Tell your healthcare provider if you:
- are currently wheezing
- have a history of wheezing if under 5 years old
- have had Guillain-Barré syndrome
- have a weakened immune system or live with someone who has a severely weakened immune system
- have problems with your heart, kidneys, or lungs
- have diabetes
- are pregnant or nursing
- are taking Tamiflu®, Relenza®, amantadine, or rimantadine
If you or your child cannot take FluMist, you may still be able to get an influenza shot. Talk to your healthcare provider about this.
How is FluMist given?
- FluMist is a liquid that is sprayed into the nose.
- You can breathe normally while getting FluMist. There is no need to inhale or “sniff” it.
- People over 8 years old need one dose of FluMist each year.
- Children 2 through 8 years old may need 2 doses of FluMist if they have not been vaccinated against influenza before. Your healthcare provider will decide if your child needs to come back for a second dose.
What are the possible side effects of FluMist?
The most common side effects of FluMist are:
- runny or stuffy nose
- sore throat
- fever over 100 degrees F
Other possible side effects include:
- decreased appetite
- irritability
- tiredness
- cough
- headache
- muscle ache
- chills
Call your healthcare provider or go to the emergency department right away if you or your child experience:
- hives or a bad rash
- trouble breathing
- swelling of the face, tongue, or throat
These are not all the possible side effects of FluMist. You can ask your healthcare provider for a complete list of side effects that is available to healthcare professionals.
Call your healthcare provider for medical advice about side effects. You may report side effects to VAERS at 1-800-822-7967 or http://vaers.hhs.gov.
What are the ingredients in FluMist?
Active Ingredient: FluMist contains 3 influenza virus strains that are weakened (A(H1N1), A(H3N2), and B).
Inactive Ingredients: monosodium glutamate, gelatin, arginine, sucrose, dibasic potassium phosphate, monobasic potassium phosphate, and gentamicin.
FluMist does not contain preservatives.
If you would like more information, talk to your healthcare provider or visit www.FluMist.com or call 1-877-633-4411.
FluMist® is a registered trademark of MedImmune, LLC.
Other brands listed are registered trademarks of their respective owners and are not trademarks of MedImmune, LLC.
Manufactured by:
MedImmune, LLC
Gaithersburg, MD 20878
Issue date: May 2011 RAL-FLUV11
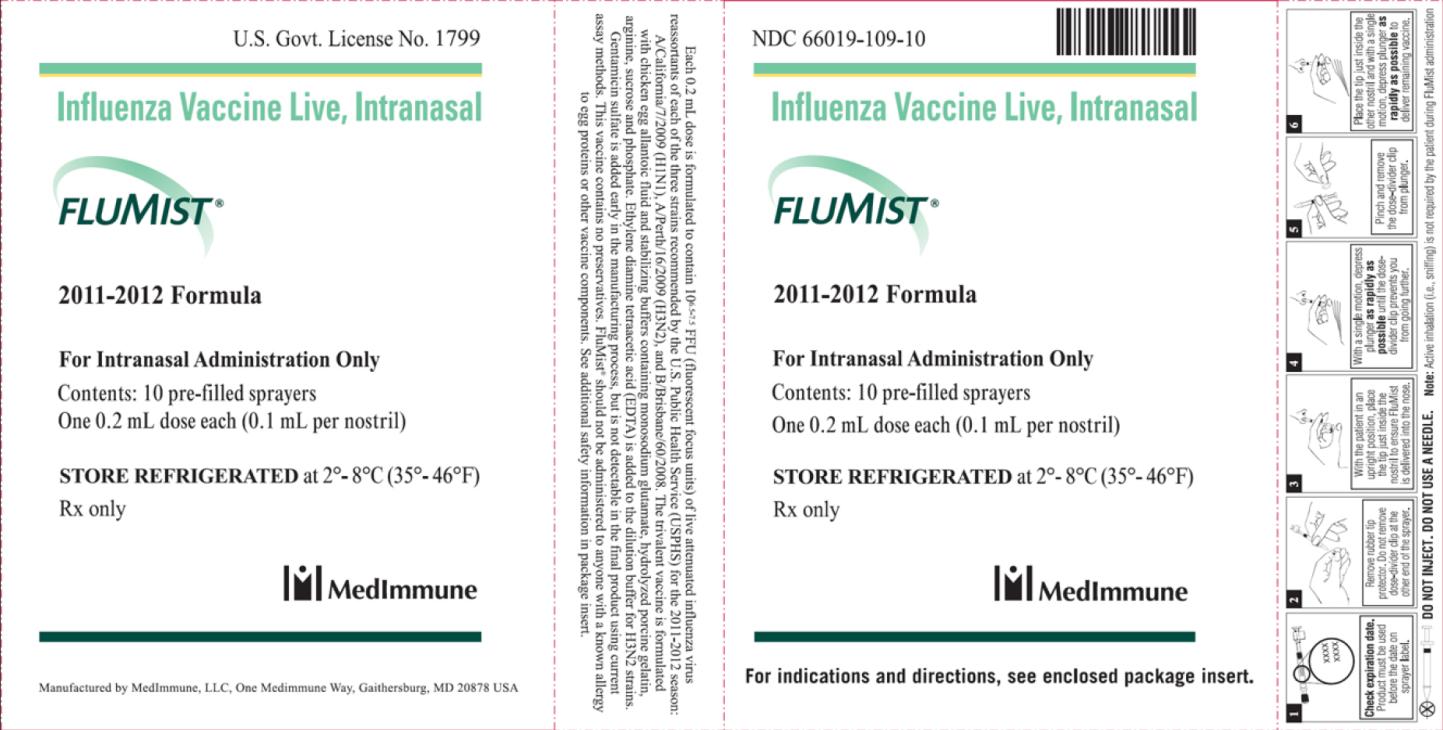
PRINCIPAL DISPLAY PANEL
Influenza Vaccine Live, Intranasal
FLUMIST®
2011-2012 Formula
For Intranasal Administration Only
Contents: 10 pre-filled sprayers
One 0.2 mL dose each (0.1 mL per nostril)
STORE REFRIGERATED at 2°-8°C (35°-46°F)
Rx Only
| FLUMIST
influenza vaccine live intranasal spray |
|||||||||||||||||||||
|
|||||||||||||||||||||
|
|||||||||||||||||||||
|
|||||||||||||||||||||
|
|||||||||||||||||||||
|
|||||||||||||||||||||
| Marketing Information | |||
| Marketing Category | Application Number or Monograph Citation | Marketing Start Date | Marketing End Date |
| BLA | BLA125020 | 06/30/2011 | 07/19/2012 |
| Labeler - MedImmune, LLC (489176682) |
Revised: 05/2011 MedImmune, LLC