CEFAZOLIN
-
cefazolin sodium injection, powder, for solution
Sagent Pharmaceuticals
----------
DESCRIPTION
To reduce the development of drug-resistant bacteria and maintain the effectiveness of cefazolin for injection and other antibacterial drugs, cefazolin for injection should be used only to treat or prevent infections that are proven or strongly suspected to be caused by bacteria.
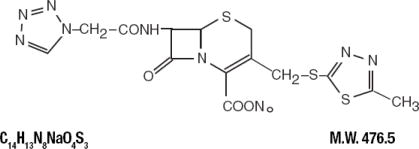
Cefazolin for Injection, USP is a semisynthetic cephalosporin, white to off white in color, for parenteral administration. It is 5-thia-1-azabicyclo [4.2.0] oct-2-ene-2-carboxylic acid, 3-{[(5-methyl-1, 3, 4-thiadiazol-2-yl) thio]-methyl}-8-oxo-7-[[(1H-tetrazol-1-yl) acetyl] amino]-, monosodium salt (6R-trans). The sodium content is 48 mg/g of cefazolin sodium.
The structural formula is as follows:
The pH of the constituted solution is between 4.5 and 6.
Cefazolin for Injection, USP is supplied in 10 or 20 grams Pharmacy Bulk Packages. Each Pharmacy Bulk Package contains, cefazolin sodium equivalent to 10 or 20 grams of cefazolin. The sodium content is approximately 48 mg (2.1 mEq sodium ion) per gram of cefazolin.
A pharmacy bulk package is a container of a sterile preparation for parenteral use that contains many single doses. The contents are intended for use in a pharmacy admixture service and are restricted to the preparation of admixtures for intravenous infusion. FURTHER DILUTION IS REQUIRED BEFORE USE.
CLINICAL PHARMACOLOGY
Human Pharmacology:
Studies have shown that following intravenous administration of cefazolin to normal volunteers, mean serum concentrations peaked at approximately 185 mcg/mL and were approximately 4 mcg/mL at 8 hours for a 1 gram dose.
The serum half-life for cefazolin is approximately 1.8 hours following IV administration. In a study (using normal volunteers) of constant intravenous infusion with dosages of 3.5 mg/kg for 1 hour (approximately 250 mg) and 1.5 mg/kg the next 2 hours (approximately 100 mg). Cefazolin produced a steady serum level at the third hour of approximately 28 mcg/mL.
Studies in patients hospitalized with infections indicate that cefazolin produces mean peak serum levels approximately equivalent to those seen in normal volunteers.
Bile levels in patients without obstructive biliary disease can reach or exceed serum levels by up to five times; however, in patients with obstructive biliary disease, bile levels of cefazolin for are considerably lower than serum levels (<1.0 mcg/mL).
In synovial fluid, the level of cefazolin becomes comparable to that reached in serum at about 4 hours after drug administration. Studies of cord blood show prompt transfer of cefazolin across the placenta. Cefazolin is present in very low concentrations in the milk of nursing mothers.
Cefazolin is excreted unchanged in the urine. In the first 6 hours approximately 60% of the drug is excreted in the urine and this increases to 70% to 80% within 24 hours.
In patients undergoing peritoneal dialysis (2 L/hr.), cefazolin produced mean serum levels of approximately 10 and 30 mcg/mL after 24 hours' instillation of a dialyzing solution containing 50 mg/L and 150 mg/L, respectively. Mean peak levels were 29 mcg/mL (range 13 to 44 mcg/mL) with 50 mg/L (three patients), and 72 mcg/mL (range 26 to 142 mcg/mL) with 150 mg/L (six patients). Intraperitoneal administration of cefazolin is usually well tolerated.
Controlled studies on adult normal volunteers, receiving 1 gram 4 times a day for 10 days, monitoring CBC, SGOT, SGPT, bilirubin, alkaline phosphatase, BUN, creatinine, and urinalysis, indicated no clinically significant changes attributed to cefazolin.
Microbiology:
In vitro tests demonstrate that the bactericidal action of cephalosporins results from inhibition of cell wall synthesis. Cefazolin is active against most strains of the following microorganisms both in vitro and in clinical infections as described in the INDICATIONS AND USAGE section:
Aerobic Gram-positive microorganisms:
- Staphylococcus aureus (including penicillinase-producing strains)
- Staphylococcus epidermidis
- Streptococcus pneumoniae
- Streptococcus pyogenes and other strains of Streptococci
Note: Methicillin-resistant staphylococci are uniformly resistant to cefazolin.
Group A beta-hemolytic streptococci and other strains of streptococci (many strains of enterococci are resistant)
- Escherichia coil
- Haemophilus influenzae
- Klebsiella species
- Proteus mirabilis
Note: Most strains of indole- positive Proteus (Proteus vulgaris), Enterobacter cloacae, Morganella morganii, and Providencia rettgeri are resistant. Serratia,
Pseudomonas, Mima, Herellea are almost uniformly resistant to cefazolin.
Disk Susceptibility Tests:
Dilution techniques
Quantitative methods are used to determine antimicrobial minimum inhibitory concentrations (MICs). These MICs provide estimates of the susceptibility of bacteria to antimicrobial compounds. The MICs should be determined using a standardized procedure. Standardized procedures are based on a dilution method1 (broth) or equivalent with standardized inoculum concentrations and standardized concentrations of cefazolin powder. The MIC values should be interpreted according to the following criteria:
For Enterbacteriaceae and Staphylococcus spp.
| MIC (mcg/mL) | Interpretation |
| < 8.0 | Susceptible (S) |
| 16.0 | Intermediate (I) |
| > 32 | Resistant ( R) |
A report of “Susceptible” indicates that the pathogen is likely to be inhibited if the antimicrobial compound in the blood reaches the concentrations usually achievable. A report of “Intermediate” indicates that the result should be considered equivocal, and, if the microorganism is not fully susceptible to alternative, clinically feasible drugs the test should be repeated. This category implies possible clinical applicability in body sties where the drug is physiologically concentrated or in situations where high dosage of drug can be used. This category also provides a buffer zone which prevents small uncontrolled technical factors from causing major discrepancies in interpretation. A report of “Resistant” indicates that the pathogen is not likely to be inhibited if the antimicrobial compound in the blood reaches the concentrations usually achievable; other therapy should be selected.
Standardized susceptibility test procedures require the use of laboratory control microorganisms to control the technical aspects of the laboratory procedures.
Standard cefazolin powder should provide the following MIC values:
| Microorganism | MIC (mcg/mL) |
| S. aureus ATCC 29213 | 0.25 to 1.0 |
| E. Coli ATCC25922 | 1.0 to 4.0 |
Diffusion Techniques
Quantitative methods that require measurement of zone diameters also provide reproducible estimates of the susceptibility of bacteria to antimicrobial compounds. One such standardized procedure2 requires the use of standardized inoculum concentrations. This procedure uses paper disks impregnated with 30 mcg cefazolin to test the susceptibility of microorganisms to cefazolin.
Reports from the laboratory providing results of the standard single disk susceptibility test with a 30 mcg cefazolin disk should be interpreted according to the following criteria:
For Enterobacteriaceae using the 30 mcg cefazolin disk
| Zone diameter (mm) | Interpretation |
| >18 | Susceptible (S) |
| 15 to 17 | Intermediate (I) |
| <14 | Resistant (R) |
For Staphylococcus spp. Using a 30 mcg cefazolin or the 30 mcg cephalothin disks
| Zone diameter (mm) | Interpretation |
| >18 | Susceptible (S) |
| 15 to 17 | Intermediate (I) |
| < 14 | Resistant (R) |
Interpretation should be as stated above for results using dilution techniques.
Interpretation involves correlation of the diameter obtained in the disk test with the MIC for cefazolin.
As with standardized dilution techniques, diffusion methods require the use of laboratory control microorganisms that are used to control the technical aspects of the laboratory procedures: For the diffusion technique, the 30- mcg cefazolin disk should provide the following zone diameters in this laboratory test quality control strain:
| Microorganism | Zone diameter (mm) |
| S. aureus ATCC 25923 | 29 to 35 |
| E. coli ATCC 25922 | 23 to 29 |
INDICATIONS AND USAGE
Cefazolin is indicated in the treatment of the following serious infections due to susceptible organisms:
Respiratory Tract Infections:
Due to Streptococcus pneumoniae, Klebsiella species, Haemophilus influenzae,
Staphylococcus aureus (penicillin-sensitive and penicillin-resistant), and group A
beta-hemolytic streptococci.
Injectable benzathine penicillin is considered to be the drug of choice in treatment and prevention of streptococcal infections, including the prophylaxis of rheumatic fever.
Cefazolin is effective in the eradication of streptococci from the nasopharynx; however, data establishing the efficacy of cefazolin in the subsequent prevention of rheumatic fever are not available at present.
Urinary Tract Infections:
Due to Escherichia coli, Proteus mirabilis, Kiebsiella species, and some strains of enterobacter and enterococci.
Skin and Skin Structure Infections:
Due to Staphylococcus aureus (penicillin-sensitive and penicillin- resistant), group A beta-hemolytic streptococci, and other strains of streptococci.
Biliary Tract Infections:
Due to Escherichia coli, various strains of streptococci, Proteus mirabilis, Klebsiella species and Staphylococcus aureus.
Bone and Joint Infections:
Due to Staphylococcus aureus.
Genital Infections:
(i.e., prostatitis, epididymitis) due to Escherichia coli, Proteus mirabilis, Klebsiella species, and some strains of enterococci.
Septicemia:
Due to Streptococcus pneumoniae, Staphylococcus aureus (penicillin-sensitive and penicillin-resistant), Proteus mirabilis, Escherichia coli and Klebsiella species.
Endocarditis:
Due to Staphylococcus aureus (penicillin-sensitive and penicillin-resistant) and group A beta-hemolytic streptococci.
Appropriate culture and susceptibility studies should be performed to determine the susceptibility of the causative organism to cefazolin.
Perioperative Prophylaxis:
The prophylactic administration of cefazolin preoperatively, intraoperatively, and postoperatively may reduce the incidence of certain postoperative infections in patients undergoing surgical procedures which are classified as contaminated or potentially contaminated (e.g., vaginal hysterectomy, and cholecystectomy in high-risk patients such as those older than 70 years of age, with acute cholecystitis, obstructive jaundice or common duct bile stones).
The perioperative use of cefazolin may also be effective in surgical patients in whom infection at the operative site would present a serious risk (e.g., during open-heart surgery and prosthetic arthroplasty).
The prophylactic administration of cefazolin should usually be discontinued within a 24 hour period after the surgical procedure. In surgery where the occurrence of infection may be particularly devastating (e.g., open-heart surgery and prosthetic arthroplasty), the prophylactic administration of cefazolin may be continued for 3 to 5 days following the completion of surgery.
If there are signs of infection, specimens for cultures should be obtained for the identification of the causative organism so that appropriate therapy may be instituted (see DOSAGE AND ADMINISTRATION).
To reduce the development of drug-resistant bacteria and maintain the effectiveness of cefazolin for injection, and other antibacterial drugs, cefazolin for injection, should be used only to treat or prevent infections that are proven or strongly suspected to be caused by susceptible bacteria. When culture and susceptibility information are available, they should be considered in selecting or modifying antibacterial therapy. In the absence of such data,local epidemiology and susceptibility patterns may contribute to the empiric selection of therapy.
CONTRAINDICATIONS
CEFAZOLIN IS CONTRAINDICATED IN PATIENTS WITH KNOWN ALLERGY TO THE CEPHALOSPORIN GROUP OF ANTIBIOTICS.
WARNINGS
BEFORE THERAPY WITH CEFAZOLIN IS INSTITUTED, CAREFUL INQUIRY SHOULD BE MADE TO DETERMINE WHETHER THE PATIENT HAS HAD PREVIOUS HYPERSENSITIVITY REACTIONS TO CEFAZOLIN, CEPHALOSPORINS, PENICILLINS, OR OTHER DRUGS. IF THIS PRODUCT IS GIVEN TO PENICILLIN-SENSITIVE PATIENTS, CAUTION SHOULD BE EXERCISED BECAUSE CROSS-HYPERSENSITIVITY AMONG BETA-LACTAM ANTIBIOTICS HAS BEEN CLEARLY DOCUMENTED AND MAY OCCUR IN UP TO 10% OF PATIENTS WITH A HISTORY OF PENICILLIN ALLERGY. IF AN ALLERGIC REACTION TO CEFAZOLIN OCCURS, DISCONTINUE TREATMENT WITH THE DRUG. SERIOUS ACUTE HYPERSENSITIVITY REACTIONS MAY REQUIRE TREATMENT WITH EPINEPHRINE AND OTHER EMERGENCY MEASURES, INCLUDING OXYGEN, IV FLUIDS, IV ANTIHISTAMINES, CORTICOSTEROIDS, PRESSOR AMINES, AND AIRWAY MANAGEMENT, AS CLINICALLY INDICATED.
Clostridium difficile associated diarrhea (CDAD) has been reported with use of nearly all antibacterial agents, including cefazolin, and may range in severity from mild diarrhea to fatal colitis. Treatment with antibacterial agents alters the normal flora of the colon leading to overgrowth of C.difficile.
C.difficile produces toxins A and B which contribute to the development of CDAD.
Hypertoxin producing strains of C.difficile cause increase morbidity and mortality, as these infections can be refractory to antimicrobial therapy and may require colectomy. CDAD must be considered in all patients who present with diarrhea following antibiotic use. Careful medical history is necessary since CDAD has been reported to occur over two months after the administration of antibacterial agents.
If CDAD is suspected or confirmed, ongoing antibiotic use not directed against C.difficile may need to be discontinued. Appropriate fluid and electrolyte management, protein supplementation, antibiotic treatment of C.difficile, and surgical evaluation should be instituted as clinically indicated.
PRECAUTIONS
General:
Prolonged use of cefazolin may result in the overgrowth of nonsusceptible organisms. Careful clinical observation of the patient is essential.
When cefazolin is administered to patients with low urinary output because of impaired renal function, lower daily dosage is required (see DOSAGE AND ADMINISTRATION).
As with other beta-lactam antibiotics, seizures may occur if inappropriately high doses are administered to patients with impaired renal function (see DOSAGE AND ADMINISTRATION).
Cefazolin, as with all cephalosporins, should be prescribed with caution in individuals with a history of gastrointestinal disease, particularly colitis.
Cephalosporins may be associated with a fall in prothrombin activity. Those at risk include patients with renal or hepatic impairment or poor nutritional state, as well as patients receiving a protracted course of antimicrobial therapy, and patients previously stabilized on anticoagulant therapy. Prothrombin time should be monitored in patients at risk and exogenous vitamin K administered as indicated
Prescribing cefazolin in the absence of a proven or strongly suspected bacterial infection or a prophylactic indication is unlikely to provide benefit to the patient and increases the risk of the development of drug-resistant bacteria.
Drug Interactions:
Probenecid may decrease renal tubular secretion of cephalosporins when used concurrently, resulting in increased and more prolonged cephalosporin blood levels.
Drug/Laboratory Test Interactions:
A false positive reaction for glucose in the urine may occur with Benedict's solution, Fehling's solution or with Clinitest® tablets, but not with enzyme-based tests such as Clinistix® and Tes-Tape®
Positive direct and indirect antiglobulin (Coombs) tests have occurred; these may also occur in neonates whose mothers received cephalosporins before delivery.
Information for Patients:
Patients should be counseled that antibacterial drugs including cefazolin, should only be used to treat bacterial infections. They do not treat viral infections (e.g., the common cold). When cefazolin is prescribed to treat bacterial infection, patients should be told that although it is common to feel better early in the course of therapy, the medication should be taken exactly as directed. Skipping dosesor not completing the full course of therapy may: (1) decrease the effectiveness of the immediate treatment, and (2) increase the likelihood that bacteria will develop resistance and will not be treatable by cefazolin or other antibacterial drugs in the future.
Diarrhea is a common problem caused by antibiotics which usually ends when the antibiotic is discontinued. Sometimes after starting treatment with antibiotics, patients can develop watery and bloody stools (with or without stomach cramps and fever) even as late as two or more months after having taken the last dose of the antibiotic. If this occurs, patients should contact their physician as soon as possible.
Carcinogenesis/Mutagenesis:
Mutagenicity studies and long-term studies in animals to determine the carcinogenic potential of cefazolin have not been performed.
Pregnancy:
Teratogenic Effects-Pregnancy Category B. Reproduction studies have been performed in rats, mice, and rabbits at doses up to 25 times the human dose and have revealed no evidence of impaired fertility or harm to the fetus due to cefazolin. There are, however, no adequate and well-controlled studies in pregnant women. Because animal reproduction studies are not always predictive of human response, this drug should be used during pregnancy only if clearly needed.
Labor and Delivery:
When cefazolin has been administered prior to caesarean section, drug levels in cord blood have been approximately one quarter to one third of maternal drug levels. The drug appears to have no adverse effect on the fetus.
Nursing Mothers:
Cefazolin is present in very low concentrations in the milk of nursing mothers. Caution should be exercised when cefazolin is administered to a nursing woman.
Pediatric Use:
Safety and effectiveness for use in premature infants and neonates have not been established. See DOSAGE AND ADMINISTRATION for recommended dosage in pediatric patients over 1 month old.
Geriatric Use:
Of the 920 subjects who received cefazolin in clinical studies, 313 (34%) were 65 years and over, while 138 (15%) were 75 years and over. No overall differences in safety or effectiveness were observed between these subjects and younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out. This drug is known to be substantially excreted by the kidney, and the risk of toxic reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function (see PRECAUTIONS, General and DOSAGE AND ADMINISTRATION).
ADVERSE REACTIONS
The following reactions have been reported:
Gastrointestinal:
Diarrhea, oral candidiasis (oral thrush), vomiting, nausea, stomach cramps, anorexia, and pseudomembranous colitis. Onset of pseudomembranous colitis symptoms may occur during or after antibiotic treatment (see WARNINGS). Nausea and vomiting have been reported rarely.
Allergic:
Anaphylaxis, eosinophilia, itching, drug fever, skin rash, Stevens-Johnson syndrome.
Hematologic:
Neutropenia, leukopenia, thrombocytopenia, thrombocythermia.
Hepatic:
Transient rise in SGOT, SGPT, and alkaline phosphatase levels has been observed. As with other cephalosporins, reports of hepatitis have been received.
Renal:
As with other cephalosporins, reports of increased BUN and creatinine levels, as well as renal failure, have been received.
Local Reactions:
Rare instances of phlebitis have been reported at site of injection. Pain at the site of injection after intramuscular administration has occurred infrequently. Some induration has occurred.
Other Reactions:
Genital and anal pruritus (including vulvar pruritus, genital moniliasis, and vaginitis).
Cephalosporin-class Adverse Reactions: In addition to the adverse reactions listed above that have been observed in patients treated with cefazolin, the following adverse reactions and altered laboratory tests have been reported for cephalosporin-class antibiotics:
Adverse Reactions: Allergic reactions, urticaria, serum sickness-like reactions, erythema multiforme, toxic epidermal necrolysis, colitis, renal dysfunction, toxic nephropathy, abdominal pain, reversible hyperactivity, hypertonia, hepatic dysfunction including cholestasis, aplastic anemia, hemolytic anemia, hemorrhage, and superinfection.
Altered Laboratory Tests: Prolonged prothrombin time, positive direct Coombs' test, false-positive test for urinary glucose, elevated bilirubin, elevated LDH, increased creatinine, pancytopenia, and agranulocytosis.
Several cephalosporins have been implicated in triggering seizures, particularly in patients with renal impairment when the dosage was not reduced (see DOSAGE AND ADMINISTRATION). If seizures associated with drug therapy occur, the drug should be discontinued. Anticonvulsant therapy can be given if clinically indicated.
DOSAGE AND ADMINISTRATION
After constitution, cefazolin can be administered by parenteral administration. However, the intent of this pharmacy bulk package is for the preparation of the solutions for intravenous infusion only.
|
*In rare instances, doses of up to 12 grams of cefazolin per day have been used. |
||
| Type of Infection | Dose | Frequency |
| Moderate to severe infections | 500 mg to 1 gram | every 6 to 8 hours |
| Mild infections caused by susceptible gram-positive cocci | 250 mg to 500mg | every 8 hours |
| Acute, uncomplicated urinary tract infections | 1gram | every 12 hours |
| Pneumococcal | 500 mg | every 12 hours |
| Severe, life-threatening infections (e.g., endocarditis, septicemia)* | 1 gram to 1.5 grams | every 6 hours |
Perioperative Prophylactic Use:
To prevent postoperative infection in contaminated or potentially contaminated surgery, recommended doses are:
- 1 gram IV administered one half to 1 hour prior to the start of surgery.
- For lengthy operative procedures (e.g., 2 hours or more), 500 mg to 1 gram IV during surgery (administration modified depending on the duration of the operative procedure).
- 500 mg to 1 gram IV every 6 to 8 hours for 24 hours postoperatively.
It is important that (1) the preoperative dose be given just (one half to 1 hour) prior to the start of surgery so that adequate antibiotic levels are present in the serum and tissues at the time of initial surgical incision and (2) cefazolin be administered, if necessary, at appropriate intervals during surgery to provide sufficient levels of the antibiotic at the anticipated moments of greatest exposure to infective organisms.
In surgery where the occurrence of infection may be particularly devastating (e.g., open-heart surgery and prosthetic arthroplasty), the prophylactic administration of cefazolin may be continued for 3 to 5 days following the completion of surgery.
Directions for Proper Use of Pharmacy Bulk Package:
Not for direct infusion. This Pharmacy Bulk Package is for use in a hospital pharmacy admixture service, only in a suitable work area, such as a laminar flow hood. Using aseptic technique, the container closure may be penetrated only one time using a suitable sterile dispensing set or transfer device that allows measured dispensing of the contents. Use of a syringe and needle is not recommended as it may cause leakage. The withdrawal of container contents should be accomplished without delay. However, should this not be possible, a maximum time of 4 HOURS from the initial closure entry is permitted to complete fluid transfer operations. This time limit should begin with the introduction of the solvent or diluent into the Pharmacy Bulk Package. DISCARD ANY UNUSED PORTION AFTER 4 HOURS. THIS PHARMACY BULK PACKAGE IS NOT INTENDED TO BE DISPENSED AS A UNIT.
Dosage Adjustment for Patients With Reduced Renal Function:
Cefazolin may be used in patients with reduced renal function with the following dosage adjustments. Patients with a creatinine clearance of 55 mL/min or greater or a serum creatinine of 1.5 mg% or less can be given full doses. Patients with creatinine clearance rates of 35 to 54 mL/min or serum creatinine of 1.6 to 3 mg% can also be given full doses but dosage should be restricted to at least 8 hour intervals. Patients with creatinine clearance rates of 11 to 34 mL/min or serum creatinine of 3.1 to 4.5 mg% should be given half the usual dose every 12 hours. Patients with creatinine clearance rates of 10 mL/min or less or serum creatinine of 4.6 mg% or greater should be given one half the usual dose every 18 to 24 hours. All reduced dosage recommendations apply after an initial loading dose appropriate to the severity of the infection. Patients undergoing peritoneal dialysis, see CLINICAL PHARMACOLOGY (Human Pharmacology).
Pediatric Dosage:
In pediatric patients, a total daily dosage of 25 to 50 mg/kg (approximately 10 to 20 mg/lb) of body weight, divided into 3 or 4 equal doses, is effective for most mild to moderately severe infections. Total daily dosage may be increased to 100 mg/kg (45 mg/lb) of body weight for severe infections. Since safety for use in premature infants and in neonates has not been established, the use of cefazolin in these patients is not recommended.
| Weight | 25 mg/kg/Day Divided Into 3 Doses |
||
| Lbs | Kg | Approximate Single Dose mg/q8h | Vol. (mL) needed with dilution of 125 mg/mL |
| 10 | 4.5 | 40 mg | 0.35 mL |
| 20 | 9.0 | 75 mg | 0.6 mL |
| 30 | 13.6 | 115 mg | 0.9 mL |
| 40 | 18.1 | 150 mg | 1.2 mL |
| 50 | 22.7 | 190 mg | 1.5 mL |
| Weight | 25 mg/kg/Day Divided Into 4 Doses |
||
| Lbs | Kg | Approximate Single Dose mg/q6h | Vol. (mL) needed with dilution of 125 mg/mL |
| 10 | 4.5 | 30 mg | 0.25 mL |
| 20 | 9.0 | 55 mg | 0.45 mL |
| 30 | 13.6 | 85 mg | 0.7 mL |
| 40 | 18.1 | 115mg | 0.9 mL |
| 50 | 22.7 | 140 mg | 1.1 mL |
| Weight | 50 mg/kg/Day Divided Into 3 Doses |
||
| Lbs | Kg | Approximate Single Dose mg/q8h | Vol. (mL) needed with dilution of 225 mg/mL |
| 10 | 4.5 | 75 mg | 0.35 mL |
| 20 | 9.0 | 150 mg | 0.7 mL |
| 30 | 13.6 | 225 mg | 1.0 mL |
| 40 | 18.1 | 300 mg | 1.35 mL |
| 50 | 22.7 | 375 mg | 1.7 mL |
| Weight | 50 mg/kg/Day Divided Into 4 Doses |
||
| Lbs | Kg | Approximate Single Dose mg/q6h | Vol. (mL) needed with dilution of 225 mg/mL |
| 10 | 4.5 | 55 mg | 0.25 mL |
| 20 | 9.0 | 110 mg | 0.5 mL |
| 30 | 13.6 | 170 mg | 0.75 mL |
| 40 | 18.1 | 225 mg | 1.0 mL |
| 50 | 22.7 | 285 mg | 1.25 mL |
In pediatric patients with mild to moderate renal impairment (creatinine clearance of 70 to 40 mL/min.), 60% of the normal daily dosage given in equally divided doses every 12 hours should be sufficient. In patients with moderate impairment (creatinine clearance of 40 to 20 mL/min), 25% of the normal daily dose given in equally divided doses every 12 hours should be adequate. Pediatric patients with severe renal impairment (creatinine clearance of 20 to 5 mL/min.) may be given 10% of the normal daily dose every 24 hours. All dosage recommendations apply after an initial loading dose.
RECONSTITUTION
Preparation of Parenteral Solution:
Parenteral drug products should be SHAKEN WELL when reconstituted and inspected visually for particulate matter prior to administration. If particulate matter is evident in reconstituted fluids, the drug solutions should be discarded.
Reconstituted solutions may range in color from pale yellow to yellow without change in potency.
When reconstituted or diluted according to the instructions below, cefazolin is stable for 24 hours at room temperature or for 10 days if stored under refrigeration (5˚C or 41˚F). Reconstituted solutions may range in color from pale yellow to yellow without a change in potency.
Pharmacy Bulk Packages:
Add Sterile Water for Injection, Bacteriostatic Water for Injection, 0.9% Sodium Chloride Injection, or 5% Dextrose Injection according to the table below. SHAKE WELL. Use promptly. Discard vial within 4 hours after initial entry.
| Bottle Size | Amount of Diluent | Approximate Concentration | Approximate Available Volume |
| 20 grams | 87 mL | 1 gram/5 mL | 99 mL |
ADMINISTRATION
Intravenous Administration:
Intermittent or continuous infusion - Dilute reconstituted cefazolin in 50 to 100 mL of one of the following solutions:
- Sodium Chloride Injection, USP
- 5% or 10% Dextrose Injection, USP
- 5% Dextrose in Lactated Ringer's Injection, USP
- 5% Dextrose and 0.9% Sodium Chloride Injection, USP
- 5% Dextrose and 0.45% Sodium Chloride Injection, USP
- 5% Dextrose and 0.2% Sodium Chloride Injection, USP
- Lactated Ringer's Injection, USP
- Invert Sugar 5% or 10% in Sterile Water for Injection
- Ringer's Injection, USP
- 5% Sodium Bicarbonate Injection, USP
When diluted according to the instructions above, cefazolin is stable for 24 hours at room temperature or for 10 days if stored under refrigeration (5°C or 41°F).
Prior to administration parenteral drug products should be inspected visually for particulate matter and discoloration whenever solution and container permit.
HOW SUPPLIED
Each Pharmacy Bulk Package contains cefazolin sodium equivalent to 20 grams of cefazolin.
| NDC | Cefazolin for Injection, USP | Package Factor |
| 25021-103-99 | Cefazolin sodium equivalent to 20 grams of cefazolin in a 100 mL vial | 10 Pharmacy Bulk Package vials per Carton |
As with other cephalosporins, reconstituted Cefazolin for Injection, USP tends to darken depending on storage conditions, within the stated recommendations, however, product potency is not adversely affected.
REFERENCE
- National Committee for Clinical Laboratory Standards, Method for Dilution Antimicrobial Susceptibility Tests for Bacteria that Grow Aerobically – Fifth Edition. Approved Standard NCCLS Document M7-A4, Vol. 20, No. 2, NCCLS, Wayne, PA, January 2000.
- National Committee for Clinical Laboratory Standards, Performance Standards for Antimicrobial Disk Susceptibility Tests – Seventh Edition. Approved Standard NCCLS Document M2-A7, Vol. 20, No. 1, NCCLS, Wayne, PA, January 2000.
SAGENT®
Mfd. for SAGENT Pharmaceuticals
Schaumburg, IL 60195
Made in USA
©2009 Sagent Pharmaceuticals, Inc.
May 2009
IN-0002
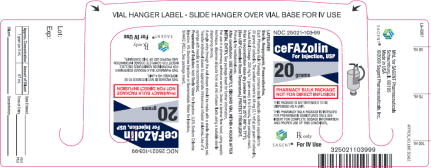
PACKAGE LABEL – PRINCIPAL DISPLAY PANEL – VIAL LABEL
NDC 25021-103-99
PROFESSIONAL SAMPLE – NOT FOR SALE
Rx only
Cefazolin for Injection, USP 20 gram Pharmacy Bulk Package
| CEFAZOLIN
cefazolin sodium injection, powder, for solution |
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
| Marketing Information | |||
| Marketing Category | Application Number or Monograph Citation | Marketing Start Date | Marketing End Date |
| ANDA | ANDA065296 | 07/15/2009 | 04/13/2012 |
| Labeler - Sagent Pharmaceuticals (796852890) |
Revised: 04/2012 Sagent Pharmaceuticals