HYPERTENIPINE
-
amlodipine besylate tablet
Physician Therapeutics LLC
----------
Hypertenipine-2.5DESCRIPTION
Amlodipine besylate, USP is a long-acting calcium channel blocker.
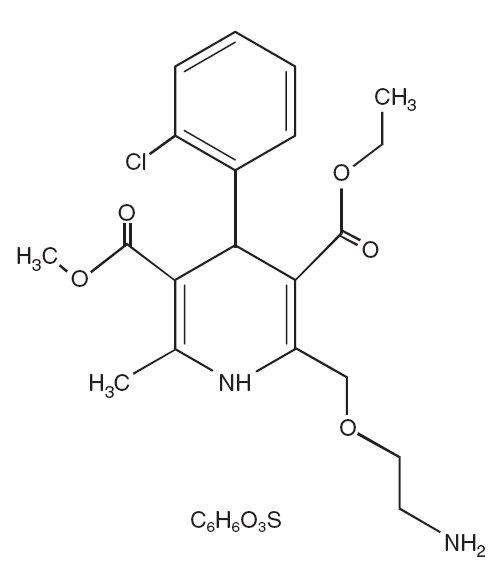
Amlodipine besylate, USP is chemically described as 3-Ethyl-5-methyl (±)-2-[(2-aminoethoxy) methy l ] - 4 - ( 2 - c h l o r o p h e ny l ) - 1 , 4 - d i hydro-6-methy l - 3 , 5 - py r i d i n e d i c a r b ox y l a t e, monobenzenesulphonate. Its molecular formula is C20H25CIN2O5•C6H6O3S, and its structural formula is:
Amlodipine besylate, USP is a white crystalline powder with a molecular weight of 567.1. It is slightly soluble in water and sparingly soluble in ethanol. Amlodipine besylate tablets are formulated as white tablets equivalent to 2.5, 5 and 10 mg of amlodipine for oral administration. In addition to the active ingredient, amlodipine besylate, USP, each tablet contains the following inactive ingredients: microcrystalline cellulose, dibasic calcium phosphate anhydrous, sodium starch glycolate, and magnesium stearate.
CLINICAL PHARMACOLOGY
Mechanism of Action
Amlodipine is a dihydropyridine calcium antagonist (calcium ion antagonist or slow-channel blocker)
that inhibits the transmembrane influx of calcium ions into vascular smooth muscle and cardiac
muscle. Experimental data suggest that amlodipine binds to both dihydropyridine and
nondihydropyridine binding sites. The contractile processes of cardiac muscle and vascular smooth
muscle are dependent upon the movement of extracellular calcium ions into these cells through
specific ion channels. Amlodipine inhibits calcium ion influx across cell membranes selectively, with
a greater effect on vascular smooth muscle cells than on cardiac muscle cells. Negative inotropic
effects can be detected in vitrobut such effects have not been seen in intact animals at therapeutic
doses. Serum calcium concentration is not affected by amlodipine. Within the physiologic pH range,
amlodipine is an ionized compound (pKa=8.6), and its kinetic interaction with the calcium channel
receptor is characterized by a gradual rate of association and dissociation with the receptor binding
site, resulting in a gradual onset of effect.
Amlodipine is a peripheral arterial vasodilator that acts directly on vascular smooth muscle to cause
a reduction in peripheral vascular resistance and reduction in blood pressure.
The precise mechanisms by which amlodipine relieves angina have not been fully delineated, but
are thought to include the following:
Exertional Angina: In patients with exertional angina, amlodipine besylate reduces the total
peripheral resistance (afterload) against which the heart works and reduces the rate pressure
product, and thus myocardial oxygen demand, at any given level of exercise.
Vasospastic Angina: Amlodipine besylate has been demonstrated to block constriction and restore
blood flow in coronary arteries and arterioles in response to calcium, potassium epinephrine,
serotonin, and thromboxane A2 analog in experimental animal models and in human coronary
vessels in vitro. This inhibition of coronary spasm is responsible for the effectiveness of amlodipine
besylate in vasospastic (Prinzmetal’s or variant) angina.
Pharmacokinetics and Metabolism
After oral administration of therapeutic doses of amlodipine besylate, absorption produces peak
plasma concentrations between 6 and 12 hours. Absolute bioavailability has been estimated to be
between 64 and 90%. The bioavailability of amlodipine besylate is not altered by the presence of
food.
Amlodipine is extensively (about 90%) converted to inactive metabolites via hepatic metabolism with
10% of the parent compound and 60% of the metabolites excreted in the urine. Ex vivostudies have
shown that approximately 93% of the circulating drug is bound to plasma proteins in hypertensive
patients. Elimination from the plasma is biphasic with a terminal elimination half-life of about 30-50
hours. Steady-state plasma levels of amlodipine are reached after 7 to 8 days of consecutive daily
dosing.
The pharmacokinetics of amlodipine are not significantly influenced by renal impairment. Patients
with renal failure may therefore receive the usual initial dose.
Elderly patients and patients with hepatic insufficiency have decreased clearance of amlodipine with
a resulting increase in AUC of approximately 40-60%, and a lower initial dose may be required. A
similar increase in AUC was observed in patients with moderate to severe heart failure.
Pediatric Patients
Sixty-two hypertensive patients aged 6 to 17 years received doses of amlodipine besylate between
1.25 mg and 20 mg.Weight-adjusted clearance and volume of distribution were similar to values in
adults.
Pharmacodynamics
Hemodynamics Following administration of therapeutic doses to patients with hypertension,
amlodipine besylate produces vasodilation resulting in a reduction of supine and standing blood
pressures. These decreases in blood pressure are not accompanied by a significant change in heart
rate or plasma catecholamine levels with chronic dosing. Although the acute intravenous
administration of amlodipine decreases arterial blood pressure and increases heart rate in
hemodynamic studies of patients with chronic stable angina, chronic oral administration of
amlodipine in clinical trials did not lead to clinically significant changes in heart rate or blood
pressures in normotensive patients with angina.
With chronic once daily oral administration, antihypertensive effectiveness is maintained for at least
24 hours. Plasma concentrations correlate with effect in both young and elderly patients. The
magnitude of reduction in blood pressure with amlodipine besylate is also correlated with the height
of pretreatment elevation; thus, individuals with moderate hypertension (diastolic pressure 105-114
mmHg) had about a 50% greater response than patients with mild hypertension (diastolic pressure
90-104 mmHg). Normotensive subjects experienced no clinically significant change in blood
pressures (+1/–2 mmHg).
In hypertensive patients with normal renal function, therapeutic doses of amlodipine besylate
resulted in a decrease in renal vascular resistance and an increase in glomerular filtration rate and
effective renal plasma flow without change in filtration fraction or proteinuria.
As with other calcium channel blockers, hemodynamic measurements of cardiac function at rest and
during exercise (or pacing) in patients with normal ventricular function treated with amlodipine
besylate have generally demonstrated a small increase in cardiac index without significant influence
on dP/dt or on left ventricular end diastolic pressure or volume. In hemodynamic studies, amlodipine
besylate has not been associated with a negative inotropic effect when administered in the
therapeutic dose range to intact animals and man, even when co-administered with beta-blockers to
man. Similar findings, however, have been observed in normals or well-compensated patients with
heart failure with agents possessing significant negative inotropic effects.
Electrophysiologic Effects: Amlodipine besylate does not change sinoatrial nodal function or
atrioventricular conduction in intact animals or man. In patients with chronic stable angina,
intravenous administration of 10 mg did not significantly alter A-H and H-V conduction and sinus
node recovery time after pacing. Similar results were obtained in patients receiving amlodipine
besylate and concomitant beta blockers. In clinical studies in which amlodipine besylate was
administered in combination with beta-blockers to patients with either hypertension or angina, no
adverse effects on electrocardiographic parameters were observed. In clinical trials with angina
patients alone, amlodipine besylate therapy did not alter electrocardiographic intervals or produce
higher degrees of AV blocks.
Clinical Studies
Effects in Hypertension
Adult Patients: The antihypertensive efficacy of amlodipine besylate has been demonstrated in a
total of 15 double-blind, placebo-controlled, randomized studies involving 800 patients on amlodipine
besylate and 538 on placebo. Once daily administration produced statistically significant placebocorrected
reductions in supine and standing blood pressures at 24 hours postdose, averaging about
12/6 mmHg in the standing position and 13/7 mmHg in the supine position in patients with mild to
moderate hypertension. Maintenance of the blood pressure effect over the 24-hour dosing interval
was observed, with little difference in peak and trough effect. Tolerance was not demonstrated in
patients studied for up to 1 year. The 3 parallel, fixed dose, dose response studies showed that the
reduction in supine and standing blood pressures was dose-related within the recommended dosing
range. Effects on diastolic pressure were similar in young and older patients. The effect on systolic
pressure was greater in older patients, perhaps because of greater baseline systolic pressure.
Effects were similar in black patients and in white patients.
Pediatric Patients: Two-hundred sixty-eight hypertensive patients aged 6 to 17 years were
randomized first to amlodipine besylate 2.5 or 5 mg once daily for 4 weeks and then randomized
again to the same dose or to placebo for another 4 weeks. Patients receiving 5 mg at the end of 8
weeks had lower blood pressure than those secondarily randomized to placebo. The magnitude of
the treatment effect is difficult to interpret, but it is probably less than 5 mmHg systolic on the 5 mg
dose. Adverse events were similar to those seen in adults.
Effects in Chronic Stable Angina:
The effectiveness of 5 to 10 mg/day of amlodipine besylate in exercise-induced angina has been
evaluated in 8 placebo-controlled, double-blind clinical trials of up to 6 weeks duration involving 1038
patients (684 amlodipine besylate, 354 placebo) with chronic stable angina. In 5 of the 8 studies
significant increases in exercise time (bicycle or treadmill) were seen with the 10 mg dose. Increases
in symptom-limited exercise time averaged 12.8% (63 sec) for amlodipine besylate 10 mg, and
averaged 7.9% (38 sec) for amlodipine besylate 5 mg. Amlodipine besylate 10 mg also increased
time to 1 mm ST segment deviation in several studies and decreased angina attack rate. The
sustained efficacy of amlodipine besylate in angina patients has been demonstrated over long-term
dosing. In patients with angina there were no clinically significant reductions in blood pressures (4/1
mmHg) or changes in heart rate (+0.3 bpm).
Effects in Vasospastic Angina:
In a double-blind, placebo-controlled clinical trial of 4 weeks duration in 50 patients, amlodipine
besylate therapy decreased attacks by approximately 4/week compared with a placebo decrease of
approximately 1/week (p less than 0.01). Two of 23 amlodipine besylate and 7 of 27 placebo patients
discontinued from the study due to lack of clinical improvement.
Studies in Patients with Congestive Heart Failure:
Amlodipine besylate has been compared to placebo in four 8-12 week studies of patients with NYHA
class II/III heart failure, involving a total of 697 patients. In these studies, there was no evidence of
worsened heart failure based on measures of exercise tolerance, NYHA classification, symptoms,
or left ventricular ejection fraction. In a long-term (follow-up at least 6 months, mean 13.8 months)
placebo-controlled mortality/morbidity study of amlodipine besylate 5 to 10 mg in 1153 patients with
NYHA classes III (n=93 1) or IV (n=222) heart failure on stable doses of diuretics, digoxin, and ACE
inhibitors, amlodipine besylate had no effect on the primary endpoint of the study which was the
combined endpoint of all-cause mortality and cardiac morbidity (as defined by life-threatening
arrhythmia, acute myocardial infarction, or hospitalization for worsened heart failure), or on NYHA
classification, or symptoms of heart failure. Total combined all-cause mortality and cardiac morbidity
events were 222/571 (39%) for patients on amlodipine besylate and 246/583 (42%) for patients on
placebo; the cardiac morbid events represented about 25% of the endpoints in the study.
Another study (PRAISE-2) randomized patients with NYHA class III (80%) or IV (20%) heart failure
without clinical symptoms or objective evidence of underlying ischemic disease, on stable doses of
ACE inhibitor (99%), digitalis (99%) and diuretics (99%), to placebo (n=827) or amlodipine besylate
(n=827) and followed them for a mean of 33 months. There was no statistically significant difference
between amlodipine besylate and placebo in the primary endpoint of all cause mortality (95%
confidence limits from 8% reduction to 29% increase on amlodipine besylate). With amlodipine
besylate there were more reports of pulmonary edema.
INDICATIONS AND USAGE
1. Hypertension
Amlodipine besylate is indicated for the treatment of hypertension. It may be used alone or in
combination with other antihypertensive agents.
2. Coronary Artery Disease
Cronic Stable Angina
Amlodipine besylate is indicated for the symptomatic treatment of chronic stable angina.
Amlodipine besylate may be used alone or in combination with other antianginal agents.
Vasospastic Angina (Prinzmetal’s or Variant Angina)
Amlodipine besylate is indicated for the treatment of confirmed or suspected vasospastic angina.
Amlodipine besylate may be used as monotherapy or in combination with other antianginal drugs.
CONTRAINDICATIONS
Amlodipine besylate is contraindicated in patients with known sensitivity to amlodipine.
WARNINGS
Increased Angina and/or Myocardial Infarction: Rarely, patients, particularly those with severe
obstructive coronary artery disease, have developed documented increased frequency, duration
and/or severity of angina or acute myocardial infarction on starting calcium channel blocker therapy
or at the time of dosage increase. The mechanism of this effect has not been elucidated.
PRECAUTIONS
General: Since the vasodilation induced by amlodipine besylate is gradual in onset, acute
hypotension has rarely been reported after oral administration. Nonetheless, caution as with any
other peripheral vasodilator, should be exercised when administering amlodipine besylate,
particularly in patients with severe aortic stenosis.
Use in Patients with Congestive Heart Failure: In general, calcium channel blockers should be
used with caution in patients with heart failure. Amlodipine besylate (5 to 10 mg per day) has been
studied in a placebo-controlled trial of 1153 patients with NYHA Class III or IV heart failure (see
CLINICAL PHARMACOLOGY) on stable doses of ACE inhibitor, digoxin, and diuretics. Follow-up
was at least 6 months, with a mean of about 14 months. There was no overall adverse effect on
survival or cardiac morbidity (as defined by life-threatening arrhythmia, acute myocardial infarction,
or hospitalization for worsened heart failure). Amlodipine besylate has been compared to placebo in
four 8-12 week studies of patients with NYHA class II/III heart failure, involving a total of 697 patients.
In these studies, there was no evidence of worsened heart failure based on measures of exercise
tolerance, NYHA classification, symptoms, or LVEF.
Beta-Blocker Withdrawal: Amlodipine besylate is not a beta-blocker and therefore gives no
protection against the dangers of abrupt beta-blocker withdrawal; any such withdrawal should be by
gradual reduction of the dose of beta-blocker.
Patients with Hepatic Failure: Since amlodipine besylate is extensively metabolized by the liver
and the plasma elimination half-life (t 1/2) is 56 hours in patients with impaired hepatic function,
caution should be exercised when administering amlodipine besylate to patients with severe hepatic
impairment.
Drug Interactions: In vitro data indicate that amlodipine besylate has no effect on the human
plasma protein binding of digoxin, phenytoin, warfarin, and indomethacin.
Effect of other agents on Amlodipine besylate.
CIMETIDINE: Co-administration of amlodipine besylate with cimetidine did not alter the
pharmacokinetics of amlodipine besylate.
GRAPEFRUIT JUICE: Co-administration of 240 mL of grapefruit juice with a single oral dose of
amlodipine 10 mg in 20 healthy volunteers had no significant effect on the C6H6O3S
pharmacokinetics of amlodipine.
MAALOX (antacid): Co-administration of the antacid Maalox with a single dose of amlodipine
besylate had no significant effect on the pharmacokinetics of amlodipine besylate.
SILDENAFIL: A single 100 mg dose of sildenafil (Viagra®) in subjects with essential hypertension
had no effect on the pharmacokinetic parameters of amlodipine besylate. When amlodipine besylate
and sildenafil were used in combination, each agent independently exerted its own blood pressure
lowering effect.
Effect of Amlodipine besylate on other agents.
ATORVASTATIN: Co-administration of multiple 10 mg doses of amlodipine besylate with 80 mg of
atorvastatin resulted in no significant change in the steady state pharmacokinetic parameters of
atorvastatin.
DIGOXIN: Co-administration of amlodipine besylate with digoxin did not change serum digoxin levels
or digoxin renal clearance in normal volunteers.
ETHANOL (alcohol): Single and multiple 10 mg doses of amlodipine besylate had no significant
effect on the pharmacokinetics of ethanol.
WARFARIN: Co-administration of amlodipine besylate with warfarin did not change the warfarin
prothrombin response time.
In clinical trials, amlodipine besylate has been safely administered with thiazide diuretics, betablockers,
angiotensin-converting enzyme inhibitors, long-acting nitrates, sublingual nitroglycerin,
digoxin, warfarin, non-steroidal anti-inflammatory drugs, antibiotics, and oral hypoglycemic drugs.
Drug/Laboratory Test Interactions: None known.
Carcinogenesis, Mutagenesis, Impairment of Fertility: Rats and mice treated with amlodipine
maleate in the diet for up to two years, at concentrations calculated to provide daily dosage levels of
0.5, 1.25, and 2.5 amlodipine mg/kg/day showed no evidence of a carcinogenic effect of the drug.
For the mouse, the highest dose was, on a mg/m2 basis, similar to the maximum recommended
human dose of 10 mg amlodipine/day*). For the rat, the highest dose, was on a mg/m2 basis, about
twice the maximum recommended human dose*.
Mutagenicity studies conducted with amlodipine maleate revealed no drug related effects at either
the gene or chromosome level.
There was no effect on the fertility of rats treated orally with amlodipine maleate (males for 64 days
and females for 14 days prior to mating) at doses up to 10 mg amlodipine/kg/day (8 times* the
maximum recommended human dose of 10 mg/day on a mg/m2 basis).
Pregnancy Category C: No evidence of teratogenicity or other embryo/fetal toxicity was found when
pregnant rats and rabbits were treated orally with amlodipine maleate at doses up to 10 mg
amlodipine/kg/day (respectively 8 times* and 23 times* the maximum recommended human dose of
10 mg on a mg/m2 basis) during their respective periods of major organogenesis. However, litter size
was significantly decreased (by about 50%) and the number of intrauterine deaths was significantly
increased (about 5-fold) in rats receiving amlodipine maleate at a dose equivalent to 10 mg
amlodipine/kg/day for 14 days before mating and throughout mating and gestation. Amlodipine
maleate has been shown to prolong both the gestation period and the duration of labor in rats at this
dose. There are no adequate and well-controlled studies in pregnant women. Amlodipine should be
used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
*Based on patient weight of 50 kg.
Nursing Mothers: It is not known whether amlodipine is excreted in human milk. In the absence of
this information, it is recommended that nursing be discontinued while amlodipine besylate is
administered.
Pediatric Use: The effect of amlodipine besylate on blood pressure in patients less than 6 years of
age is not known.
Geriatric Use: Clinical studies of amlodipine besylate did not include sufficient numbers of subjects
aged 65 and over to determine whether they respond differently from younger subjects. Other
reported clinical experience has not identified differences in responses between the elderly and
younger patients. In general, dose selection for an elderly patient should be cautious, usually starting
at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or
cardiac function, and of concomitant disease or other drug therapy. Elderly patients have decreased
clearance of amlodipine with a resulting increase of AUC of approximately 40-60%, and a lower
initial dose may be required (see DOSAGE AND ADMINISTRATION).
ADVERSE REACTIONS
Amlodipine besylate has been evaluated for safety in more than 11,000 patients in U.S. and foreign
clinical trials. In general, treatment with amlodipine besylate was well-tolerated at doses up to 10 mg
daily. Most adverse reactions reported during therapy with amlodipine besylate were of mild or
moderate severity. In controlled clinical trials directly comparing amlodipine besylate (N=1730) in
doses up to 10 mg to placebo (N=1250), discontinuation of amlodipine besylate due to adverse
reactions was required in only about 1.5% of patients and was not significantly different from placebo
(about 1%). The most common side effects are headache and edema. The incidence (%) of side
effects which occurred in a dose related manner are as follows:
| Adverse Event | 2.5 mg N=275 | 5 mg N=296 | 10 mg N=268 | Placebo N=520 |
| Edema | 1.8 | 3 | 10.8 | 0.6 |
| Dizziness | 1.1 | 3.4 | 3.4 | 1.5 |
| Flushing | 0.7 | 1.4 | 2.6 | 0 |
| Palpitation | 0.7 | 1.4 | 4.5 | 0.6 |
incidence greater than 1% in placebo-controlled clinical trials include the following:
| Placebo-Controlled Studies | AMLODIPINE BESYLATE (%) (N=1730) | PLACEBO (%) (N=1250) |
| Headache | 7.3 | 7.8 |
| Fatigue | 4.5 | 2.8 |
| Nausea | 2.9 | 1.9 |
| Abdominal Pain | 1.6 | 0.3 |
| Somnolence | 1.4 | 0.6 |
incidence in women than men associated with amlodipine treatment as shown in the following table:
|
|
| AMLODIPINE BESYLATE |
| PLACEBO |
| Adverse Event | Male=% (N=1218) | Female=% (N=512) | Male=% (N=914) | Female=% (N=336) |
| Edema | 5.6 | 14.6 | 1.4 | 5.1 |
| Flushing | 1.5 | 4.5 | 0.3 | 0.9 |
| Palpitations | 1.4 | 3.3 | 0.9 | 0.9 |
| Somnolence | 1.3 | 1.6 | 0.8 | 0.3 |
conditions of open trials or marketing experience where a causal relationship is uncertain; they are
listed to alert the physician to a possible relationship:
Cardiovascular: arrhythmia (including ventricular tachycardia and atrial fibrillation), bradycardia,
chest pain, hypotension, peripheral ischemia, syncope, tachycardia, postural dizziness, postural
hypotension, vasculitis.
Central and Peripheral Nervous System: hypoesthesia, neuropathy peripheral, paresthesia,
tremor, vertigo.
Gastrointestinal: anorexia, constipation, dyspepsia,** dysphagia, diarrhea, flatulence, pancreatitis,
vomiting, gingival hyperplasia.
General: allergic reaction, asthenia,** back pain, hot flushes, malaise, pain, rigors, weight gain,
weight decrease.
Musculoskeletal System: arthralgia, arthrosis, muscle cramps,** myalgia.
Psychiatric: sexual dysfunction (male** and female), insomnia, nervousness, depression, abnormal
dreams, anxiety, depersonalization.
Respiratory System: dyspnea, * * epistaxis.
Skin and Appendages: angioedema, erythema multiforme, pruritus,** rash,** rash erythematous,
rash maculopapular.
* * These events occurred in less than 1% in placebo-controlled trials, but the incidence of these side
effects was between 1% and 2% in all multiple dose studies.
Special Senses: abnormal vision, conjunctivitis, diplopia, eye pain, tinnitus.
Urinary System: micturition frequency, micturition disorder, nocturia.
Autonomic Nervous System: dry mouth, sweating increased.
Metabolic and Nutritional: hyperglycemia, thirst.
Hemopoietic: leukopenia, purpura, thrombocytopenia.
The following events occurred in less than 0.1% of patients: cardiac failure, pulse irregularity, extrasystoles,
skin discoloration, urticaria, skin dryness, alopecia, dermatitis, muscle weakness, twitching, ataxia,
hypertonia, migraine, cold and clammy skin, apathy, agitation, amnesia, gastritis, increased appetite,
loose stools, coughing, rhinitis, dysuria, polyuria, parosmia, taste perversion, abnormal visual
accommodation, and xerophthalmia.
Other reactions occurred sporadically and cannot be distinguished from medications or concurrent
disease states such as myocardial infarction and angina.
Amlodipine besylate therapy has not been associated with clinically significant changes in routine
laboratory tests. No clinically relevant changes were noted in serum potassium, serum glucose, total
triglycerides, total cholesterol, HDL cholesterol, uric acid, blood urea nitrogen, or creatinine.
The following postmarketing event has been reported infrequently where a causal relationship is
uncertain: gynecomastia. In postmarketing experience, jaundice and hepatic enzyme elevations
(mostly consistent with cholestasis or hepatitis) in some cases severe enough to require
hospitalization have been reported in association with use of amlodipine.
Amlodipine besylate has been used safely in patients with chronic obstructive pulmonary disease,
well-compensated congestive heart failure, coronary artery disease, peripheral vascular disease,
diabetes mellitus, and abnormal lipid profiles.
OVERDOSAGE
Single oral doses of amlodipine maleate equivalent to 40 mg amlodipine/kg and 100 mg
amlodipine/kg in mice and rats, respectively, caused deaths. Single oral amlodipine maleate doses
equivalent to 4 or more mg amlodipine/kg or higher in dogs (11 or more times the maximum
recommended human dose on a mg/m2 basis) caused a marked peripheral vasodilation and
hypotension.
Overdosage might be expected to cause excessive peripheral vasodilation with marked hypotension
and possibly a reflex tachycardia. In humans, experience with intentional overdosage of amlodipine
besylate is limited. Reports of intentional overdosage include a patient who ingested 250 mg and
was asymptomatic and was not hospitalized; another (120 mg) was hospitalized, underwent gastric
lavage and remained normotensive; the third (105 mg) was hospitalized and had hypotension (90/50
mmHg) which normalized following plasma expansion. A case of accidental drug overdose has been
documented in a 19-month-old male who ingested 30 mg amlodipine (about 2 mg/kg). During the
emergency room presentation, vital signs were stable with no evidence of hypotension, but a heart
rate of 180 bpm. Ipecac was administered 3.5 hours after ingestion and on subsequent observation
(overnight) no sequelae were noted.
If massive overdose should occur, active cardiac and respiratory monitoring should be instituted.
Frequent blood pressure measurements are essential. Should hypotension occur, cardiovascular
support including elevation of the extremities and the judicious administration of fluids should be
initiated. If hypotension remains unresponsive to these conservative measures, administration of
vasopressors (such as phenylephrine) should be considered with attention to circulating volume and
urine output.
Intravenous calcium gluconate may help to reverse the effects of calcium entry blockade. As
amlodipine besylate is highly protein bound, hemodialysis is not likely to be of benefit.
DOSAGE AND ADMINISTRATION
Adults: The usual initial antihypertensive oral dose of amlodipine besylate is 5 mg once daily with
a maximum dose of 10 mg once daily. Small, fragile, or elderly individuals, or patients with hepatic
insufficiency may be started on 2.5 mg once daily and this dose may be used when adding
amlodipine besylate to other antihypertensive therapy.
Dosage should be adjusted according to each patient’s need. In general, titration should proceed
over 7 to 14 days so that the physician can fully assess the patient’s response to each dose level.
Titration may proceed more rapidly, however, if clinically warranted, provided the patient is assessed
frequently.
The recommended dose for chronic stable or vasospastic angina is 5 to 10 mg, with the lower dose
suggested in the elderly and in patients with hepatic insufficiency. Most patients will require 10 mg
for adequate effect. See ADVERSE REACTIONS section for information related to dosage and side
effects.
The recommended dose range for patients with coronary artery disease is 5 to 10 mg once daily. In
clinical studies the majority of patients required 10 mg (see CLINICAL PHARMACOLOGY, Clinical
studies).
Children: The effective antihypertensive oral dose in pediatric patients ages 6-17 years is 2.5 mg to
5 mg once daily. Doses in excess of 5 mg daily have not been studied in pediatric patients. See
CLINICAL PHARMACOLOGY.
Co-administration with Other Antihypertensive and/or Antianginal Drugs: Amlodipine besylate
has been safely administered with thiazides, ACE inhibitors, beta-blockers, long-acting nitrates,
and/or sublingual nitroglycerin.
HOW SUPPLIED
Amlodipine besylate 2.5 mg Tablets (amlodipine besylate, USP equivalent to 2.5 mg of amlodipine
per tablet) are supplied as white, round, flat-faced, beveled edged tablets debossed with IG on one
side and 237 on the other and supplied as follows:
NDC 31722-237-90 Bottle of 90
NDC 31722-237-10 Bottle of 1000
Amlodipine besylate 5 mg Tablets (amlodipine besylate, USP equivalent to 5 mg of amlodipine per
tablet) are supplied as white, round, flat-faced, beveled edged tablets debossed with IG on one side
and 238 on the other and supplied as follows:
NDC 31722-238-90 Bottle of 90
NDC 31722-238-10 Bottle of 1000
Amlodipine besylate 10 mg Tablets (amlodipine besylate, USP equivalent to 10 mg of amlodipine per
tablet) are supplied as white, round, flat-faced, beveled edged tablets debossed with IG on one side
and 239 on the other and supplied as follows:
NDC 31722-239-90 Bottle of 90
NDC 31722-239-10 Bottle of 1000
Manufactured by:
InvaGen Pharmaceuticals, Inc
Hauppauge, NY 11788
Manufactured for:
Camber Pharmaceuticals, Inc.
Piscataway, NJ 08854
Rev : 09/07
Store at 20°-25°C (68°-77°F). [See USP Controlled Room Temperature].
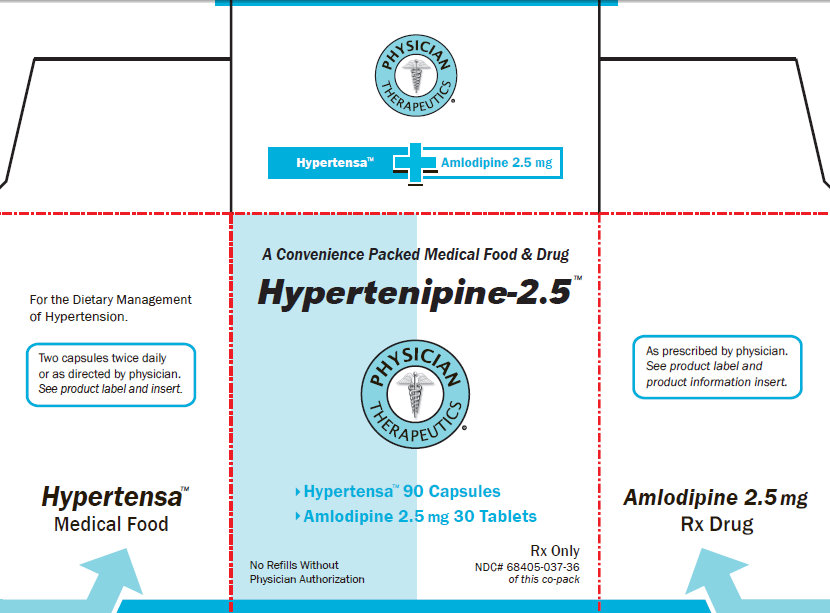
For the Dietary Management of Hypertension.
Two capsules twice daily or as directed by physician. See product label and insert.
Hypertensa Medical Food
PHYSICIAN THERAPEUTICS
Hypertensa + Amlodipine 2.5 mg
A Convenience Packed Medical Food and Drug
Hypertenipine-2.5
PHYSICIAN THERAPEUTICS
> Hypertensa 90 Capsuled
> Amlodipine 2.5 mg 30 Tablets
Rx Only
No Refills Without NDC# 68405-037-36
Physician Authorization of this co-pack
As prescribed by physician. See product label and product information insert.
Amlodipine 2.5 mg
Rx Drug
| HYPERTENIPINE
amlodipine besylate tablet |
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
| Marketing Information | |||
| Marketing Category | Application Number or Monograph Citation | Marketing Start Date | Marketing End Date |
| unapproved drug other | 12/29/2010 | ||
| Labeler - Physician Therapeutics LLC (931940964) |
| Establishment | |||
| Name | Address | ID/FEI | Operations |
| InvaGen Pharmaceuticals, Inc | 165104469 | manufacture | |
| Establishment | |||
| Name | Address | ID/FEI | Operations |
| Pharma Pac | 147681894 | repack | |