LISINOPRIL
-
lisinopril tablet
REMEDYREPACK INC.
----------
BOXED WARNING
When used in pregnancy during the second and third trimesters, ACE inhibitors can cause injury and even death to the
developing fetus. When pregnancy is detected, lisinopril should be discontinued as soon as possible. See WARNINGS, Fetal/
Neonatal Morbidity and Mortality.
WARNINGS
WARNINGSAnaphylactoid and Possibly Related ReactionsPresumably because angiotensin-converting enzyme inhibitors affect the metabolism of eicosanoids and polypeptides, including endogenous bradykinin, patients receiving ACE inhibitors (including lisinopril) may be subject to a variety of adverse reactions, some of them serious.
Head and Neck Angioedema
Angioedema of the face, extremities, lips, tongue, glottis and/or larynx has been reported in patients treated with angiotensin converting enzyme inhibitors, including lisinopril. This may occur at any time during treatment. ACE inhibitors have been associated with a higher rate of angioedema in Black than in non-Black patients. Lisinopril should be promptly discontinued and appropriate therapy and monitoring should be provided until complete and sustained resolution of signs and symptoms has occurred. Even in those instances where swelling of only the tongue is involved, without respiratory distress, patients may require prolonged observation since treatment with antihistamines and corticosteroids may not be sufficient. Very rarely, fatalities have been reported due to angioedema associated with laryngeal edema or tongue edema. Patients with involvement of the tongue, glottis or larynx are likely to experience airway obstruction, especially those with a history of airway surgery. Where there is involvement of the tongue, glottis or larynx, likely to cause airway obstruction, appropriate therapy, e.g., subcutaneous epinephrine solution 1:1000 (0.3 mL to 0.5 mL) and/or measures necessary to ensure a patent airway should be promptly provided. (See ADVERSE REACTIONS.)
Intestinal Angioedema
Intestinal angioedema has been reported in patients treated with ACE inhibitors. These patients presented with abdominal pain (with or without nausea or vomiting); in some cases there was no prior history of facial angioedema and C-1 esterase levels were normal. The angioedema was diagnosed by procedures including abdominal CT scan or ultrasound, or at surgery, and symptoms resolved after stopping the ACE inhibitor. Intestinal angioedema should be included in the differential diagnosis of patients on ACE inhibitors presenting with abdominal pain.
Patients with a history of angioedema unrelated to ACE inhibitor therapy may be at increased risk of angioedema while receiving an ACE inhibitor (see also INDICATIONS AND USAGE and CONTRAINDICATIONS).
Anaphylactoid Reactions During Desensitization
Two patients undergoing desensitizing treatment with hymenoptera venom while receiving ACE inhibitors sustained life-threatening anaphylactoid reactions. In the same patients, these reactions were avoided when ACE inhibitors were temporarily withheld, but they reappeared upon inadvertent rechallenge.
Anaphylactoid Reactions During Membrane Exposure
Sudden and potentially life-threatening anaphylactoid reactions have been reported in some patients dialyzed with high-flux membranes (e.g., AN69¶) and treated concomitantly with an ACE inhibitor. In such patients, dialysis must be stopped immediately, and aggressive therapy for anaphylactoid reactions must be initiated. Symptoms have not been relieved by antihistamines in these situations. In these patients, consideration should be given to using a different type of dialysis membrane or a different class of antihypertensive agent. Anaphylactoid reactions have also been reported in patients undergoing low-density lipoprotein apheresis with dextran sulfate absorption.
DESCRIPTION
DESCRIPTIONLisinopril is an oral long-acting angiotensin converting enzyme inhibitor. Lisinopril, a synthetic peptide derivative, is chemically
described as (S)-1-[N2-(1-Carboxy-3-phenylpropyl)-L-lysyl]-L-proline dihydrate. Its empirical formula is C21H31N3O5•2H2O.
Lisinopril is a white to off-white, crystalline powder, with a molecular weight of 441.53. It is soluble in water and sparingly soluble in
methanol and practically insoluble in ethanol.
Lisinopril is supplied as 2.5 mg, 5 mg, 10 mg, 20 mg, 30 mg and 40 mg tablets for oral administration.
Each tablet for oral administration contains 2.5 mg, 5 mg, 10 mg, 20 mg, 30 mg, or 40 mg of lisinopril USP.
INACTIVE INGREDIENT
Inactive ingredients: colloidal silicon dioxide, dibasic calcium phosphate, FDandC Blue No 2 Aluminum Lake (10mg only), FDandC Yellow No 5 Aluminum Lake (20 mg, 30 mg, and 40 mg, only), magnesium stearate, mannitol, pregelatinized starch.
CLINICAL PHARMACOLOGY
CLINICAL PHARMACOLOGY
Mechanism of Action: Lisinopril inhibits angiotensin-converting enzyme (ACE) in human subjects and animals. ACE is a peptidyl
dipeptidase that catalyzes the conversion of angiotensin I to the vasoconstrictor substance, angiotensin II. Angiotensin II also
stimulates aldosterone secretion by the adrenal cortex. The beneficial effects of lisinopril in hypertension and heart failure appear
to result primarily from suppression of the renin-angiotensin-aldosterone system. Inhibition of ACE results in decreased plasma
angiotensin II which leads to decreased vasopressor activity and to decreased aldosterone secretion. The latter decrease may result in a
small increase of serum potassium. In hypertensive patients with normal renal function treated with lisinopril alone for up to 24 weeks,
the mean increase in serum potassium was approximately 0.1 mEq/L; however, approximately 15 percent of patients had increases greater
than 0.5 mEq/L and approximately 6% had a decrease greater than 0.5 mEq/L. In the same study, patients treated with lisinopril and
hydrochlorothiazide for up to 24 weeks had a mean decrease in serum potassium of 0.1 mEq/L; approximately 4percent of patients had
increases greater than 0.5 mEq/L and approximately 12% had a decrease greater than 0.5 mEq/L. (See PRECAUTIONS.) Removal of
angiotensin II negative feedback on renin secretion leads to increased plasma renin activity.
ACE is identical to kininase, an enzyme that degrades bradykinin. Whether increased levels of bradykinin, a potent vasodepressor
peptide, play a role in the therapeutic effects of lisinopril remains to be elucidated.
While the mechanism through which lisinopril lowers blood pressure is believed to be primarily suppression of the reninangiotensin-
aldosterone system, lisinopril is antihypertensive even in patients with low-renin hypertension. Although lisinopril was
antihypertensive in all races studied, Black hypertensive patients (usually a low-renin hypertensive population) had a smaller average
response to monotherapy than non-Black patients.
Concomitant administration of lisinopril and hydrochlorothiazide further reduced blood pressure in Black and non-Black patients and
any racial differences in blood pressure response were no longer evident.
MECHANISM OF ACTION
Mechanism of Action: Lisinopril inhibits angiotensin-converting enzyme (ACE) in human subjects and animals. ACE is a peptidyldipeptidase that catalyzes the conversion of angiotensin I to the vasoconstrictor substance, angiotensin II. Angiotensin II also
stimulates aldosterone secretion by the adrenal cortex. The beneficial effects of lisinopril in hypertension and heart failure appear
to result primarily from suppression of the renin-angiotensin-aldosterone system. Inhibition of ACE results in decreased plasma
angiotensin II which leads to decreased vasopressor activity and to decreased aldosterone secretion. The latter decrease may result in a
small increase of serum potassium. In hypertensive patients with normal renal function treated with lisinopril alone for up to 24 weeks,
the mean increase in serum potassium was approximately 0.1 mEq/L; however, approximately 15% of patients had increases greater
than 0.5 mEq/L and approximately 6percent had a decrease greater than 0.5 mEq/L. In the same study, patients treated with lisinopril and
hydrochlorothiazide for up to 24 weeks had a mean decrease in serum potassium of 0.1 mEq/L; approximately 4% of patients had
increases greater than 0.5 mEq/L and approximately 12percent had a decrease greater than 0.5 mEq/L. (See PRECAUTIONS.) Removal of
angiotensin II negative feedback on renin secretion leads to increased plasma renin activity.
ACE is identical to kininase, an enzyme that degrades bradykinin. Whether increased levels of bradykinin, a potent vasodepressor
peptide, play a role in the therapeutic effects of lisinopril remains to be elucidated.
While the mechanism through which lisinopril lowers blood pressure is believed to be primarily suppression of the reninangiotensin-
aldosterone system, lisinopril is antihypertensive even in patients with low-renin hypertension. Although lisinopril was
antihypertensive in all races studied, Black hypertensive patients (usually a low-renin hypertensive population) had a smaller average
response to monotherapy than non-Black patients.
Concomitant administration of lisinopril and hydrochlorothiazide further reduced blood pressure in Black and non-Black patients and
any racial differences in blood pressure response were no longer evident.
PRECAUTIONS
PRECAUTIONSGeneralAortic Stenosis/Hypertrophic Cardiomyopathy
As with all vasodilators, lisinopril should be given with caution to patients with obstruction in the outflow tract of the left ventricle.
Impaired Renal Function
As a consequence of inhibiting the renin-angiotensin-aldosterone system, changes in renal function may be anticipated in susceptible individuals. In patients with severe congestive heart failure whose renal function may depend on the activity of the renin-angiotensin-aldosterone system, treatment with angiotensin converting enzyme inhibitors, including lisinopril, may be associated with oliguria and/or progressive azotemia and rarely with acute renal failure and/or death.
In hypertensive patients with unilateral or bilateral renal artery stenosis, increases in blood urea nitrogen and serum creatinine may occur. Experience with another angiotensin-converting enzyme inhibitor suggests that these increases are usually reversible upon discontinuation of lisinopril and/or diuretic therapy. In such patients, renal function should be monitored during the first few weeks of therapy.
Some patients with hypertension or heart failure with no apparent pre-existing renal vascular disease have developed increases in blood urea nitrogen and serum creatinine, usually minor and transient, especially when lisinopril has been given concomitantly with a diuretic. This is more likely to occur in patients with pre-existing renal impairment. Dosage reduction and/or discontinuation of the diuretic and/or lisinopril may be required.
Patients with acute myocardial infarction in the GISSI-3 trial treated with lisinopril had a higher (2.4 percent versus 1.1 percent) incidence of renal dysfunction in-hospital and at six weeks (increasing creatinine concentration to over 3 mg/dL or a doubling or more of the baseline serum creatinine concentration). In acute myocardial infarction, treatment with lisinopril should be initiated with caution in patients with evidence of renal dysfunction, defined as serum creatinine concentration exceeding 2 mg/dL. If renal dysfunction develops during treatment with lisinopril (serum creatinine concentration exceeding 3 mg/dL or a doubling from the pre-treatment value) then the physician should consider withdrawal of lisinopril.
Evaluation of patients with hypertension, heart failure, or myocardial infarction should always include assessment of renal function. (See DOSAGE AND ADMINISTRATION.)
Hyperkalemia
In clinical trials hyperkalemia (serum potassium greater than 5.7 mEq/L) occurred in approximately 2.2 percent of hypertensive patients and 4.8 percent of patients with heart failure. In most cases these were isolated values which resolved despite continued therapy. Hyperkalemia was a cause of discontinuation of therapy in approximately 0.1 percent of hypertensive patients, 0.6 percent of patients with heart failure and 0.1 percent of patients with myocardial infarction. Risk factors for the development of hyperkalemia include renal insufficiency, diabetes mellitus, and the concomitant use of potassium-sparing diuretics, potassium supplements and/or potassium-containing salt substitutes. Hyperkalemia can cause serious, sometimes fatal, arrhythmias. Lisinopril should be used cautiously, if at all, with these agents and with frequent monitoring of serum potassium. (See Drug Interactions.)
Cough
Presumably due to the inhibition of the degradation of endogenous bradykinin, persistent nonproductive cough has been reported with all ACE inhibitors, almost always resolving after discontinuation of therapy. ACE inhibitor-induced cough should be considered in the differential diagnosis of cough.
Surgery/Anesthesia
In patients undergoing major surgery or during anesthesia with agents that produce hypotension, lisinopril may block angiotensin II formation secondary to compensatory renin release. If hypotension occurs and is considered to be due to this mechanism, it can be corrected by volume expansion.
PHARMACOKINETICS
PRECAUTIONSGeneral
Aortic Stenosis/Hypertrophic Cardiomyopathy:
As with all vasodilators, lisinopril should be given with caution to patients with obstruction in the outflow tract of the left ventricle.
Impaired Renal Function:
As a consequence of inhibiting the renin-angiotensin-aldosterone system, changes in renal function may be anticipated in susceptible
individuals. In patients with severe congestive heart failure whose renal function may depend on the activity of the renin-angiotensinaldosterone
system, treatment with angiotensin converting enzyme inhibitors, including lisinopril, may be associated with oliguria
and/or progressive azotemia and rarely with acute renal failure and/or death.
In hypertensive patients with unilateral or bilateral renal artery stenosis, increases in blood urea nitrogen and serum creatinine may
occur. Experience with another angiotensin-converting enzyme inhibitor suggests that these increases are usually reversible upon
discontinuation of lisinopril and/or diuretic therapy. In such patients, renal function should be monitored during the first few weeks of
therapy. Some patients with hypertension or heart failure with no apparent pre-existing renal vascular disease have developed increases in
blood urea nitrogen and serum creatinine, usually minor and transient, especially when lisinopril has been given concomitantly with
a diuretic. This is more likely to occur in patients with pre-existing renal impairment. Dosage reduction and/or discontinuation of the
diuretic and/or lisinopril may be required.
Patients with acute myocardial infarction in the GISSI-3 trial treated with lisinopril had a higher (2.4percent versus 1.1percent) incidence of renal
dysfunction in-hospital and at six weeks (increasing creatinine concentration to over 3 mg/dL or a doubling or more of the baseline
serum creatinine concentration). In acute myocardial infarction, treatment with lisinopril should be initiated with caution in patients
with evidence of renal dysfunction, defined as serum creatinine concentration exceeding 2 mg/dL. If renal dysfunction develops
during treatment with lisinopril (serum creatinine concentration exceeding 3 mg/dL or a doubling from the pre-treatment value) then
the physician should consider withdrawal of lisinopril.
Evaluation of patients with hypertension, heart failure, or myocardial infarction should always include assessment of renal
function. (See DOSAGE AND ADMINISTRATION.)
Hyperkalemia:
In clinical trials hyperkalemia (serum potassium greater than 5.7 mEq/L) occurred in approximately 2.2percent of hypertensive patients and
4.8percent of patients with heart failure. In most cases these were isolated values which resolved despite continued therapy. Hyperkalemia
was a cause of discontinuation of therapy in approximately 0.1percent of hypertensive patients; 0.6percent of patients with heart failure and
0.1 percent of patients with myocardial infarction. Risk factors for the development of hyperkalemia include renal insufficiency, diabetes
mellitus, and the concomitant use of potassium-sparing diuretics, potassium supplements and/or potassium-containing salt substitutes,
Hyperkalemia can cause serious, sometimes fatal, arrhythmias. Lisinopril should be used cautiously, if at all, with these agents and
with frequent monitoring of serum potassium. (See Drug Interactions.)
Cough:
Presumably due to the inhibition of the degradation of endogenous bradykinin, persistent nonproductive cough has been reported with
all ACE inhibitors, almost always resolving after discontinuation of therapy. ACE inhibitor-induced cough should be considered in the
differential diagnosis of cough.
Surgery/Anesthesia:
In patients undergoing major surgery or during anesthesia with agents that produce hypotension, lisinopril may block angiotensin II
formation secondary to compensatory renin release. If hypotension occurs and is considered to be due to this mechanism, it can be
corrected by volume expansion.
PHARMACODYNAMICS
Pharmacodynamics and Clinical Effects:Hypertension:
Adult Patients: Administration of lisinopril to patients with hypertension results in a reduction of both supine and standing blood
pressure to about the same extent with no compensatory tachycardia. Symptomatic postural hypotension is usually not observed
although it can occur and should be anticipated in volume and/or salt-depleted patients. (See WARNINGS.) When given together
with thiazide-type diuretics, the blood pressure lowering effects of the two drugs are approximately additive.
In most patients studied, onset of antihypertensive activity was seen at one hour after oral administration of an individual dose of
lisinopril, with peak reduction of blood pressure achieved by 6 hours. Although an antihypertensive effect was observed 24 hours
after dosing with recommended single daily doses, the effect was more consistent and the mean effect was considerably larger in
some studies with doses of 20 mg or more than with lower doses. However, at all doses studied, the mean antihypertensive effect was
substantially smaller 24 hours after dosing than it was 6 hours after dosing.
In some patients achievement of optimal blood pressure reduction may require two to four weeks of therapy.
The antihypertensive effects of lisinopril are maintained during long-term therapy. Abrupt withdrawal of lisinopril has not been
associated with a rapid increase in blood pressure, or a significant increase in blood pressure compared to pretreatment levels.
Two dose-response studies utilizing a once-daily regimen were conducted in 438 mild to moderate hypertensive patients not on a
diuretic. Blood pressure was measured 24 hours after dosing. An antihypertensive effect of lisinopril was seen with 5 mg in some
patients. However, in both studies blood pressure reduction occurred sooner and was greater in patients treated with 10, 20 or 80 mg
of lisinopril. In controlled clinical studies, lisinopril 20-80 mg has been compared in patients with mild to moderate hypertension to
hydrochlorothiazide 12.5-50 mg and with atenolol 50-200 mg; and in patients with moderate to severe hypertension to metoprolol
100-200 mg. It was superior to hydrochlorothiazide in effects on systolic and diastolic pressure in a population that was 3/4 Caucasian.
Lisinopril was approximately equivalent to atenolol and metoprolol in effects on diastolic blood pressure, and had somewhat greater
effects on systolic blood pressure.
Lisinopril had similar effectiveness and adverse effects in younger and older ( 65 years) patients. It was less effective in Blacks than
in Caucasians.
In hemodynamic studies in patients with essential hypertension, blood pressure reduction was accompanied by a reduction in
peripheral arterial resistance with little or no change in cardiac output and in heart rate. In a study in nine hypertensive patients,
following administration of lisinopril, there was an increase in mean renal blood flow that was not significant. Data from several small studies are inconsistent with respect to the effect of lisinopril on glomerular filtration rate in hypertensive patients with normal renal
function, but suggest that changes, if any, are not large.
In patients with renovascular hypertension lisinopril has been shown to be well tolerated and effective in controlling blood pressure.
(See PRECAUTIONS.)
Pediatric Patients: In a clinical study involving 115 hypertensive pediatric patients 6 to 16 years of age, patients who weighed
50 kg received either 0.625, 2.5 or 20 mg of lisinopril daily and patients who weighed ³ 50 kg received either 1.25, 5, or 40 mg of
lisinopril daily. At the end of 2 weeks, lisinopril administered once daily lowered trough blood pressure in a dose-dependent manner
with consistent antihypertensive efficacy demonstrated at doses 1.25 mg (0.02 mg/kg). This effect was confirmed in a withdrawal
phase, where the diastolic pressure rose by about 9 mmHg more in patients randomized to placebo than it did in patients who were
randomized to remain on the middle and high doses of lisinopril. The dose-dependent antihypertensive effect of lisinopril was
consistent across several demographic subgroups: age, Tanner stage, gender, and race. In this study, lisinopril was generally well
tolerated.In the above pediatric studies, lisinopril was given either as tablets or in a suspension for those children and infants who were unable
to swallow tablets or who required a lower dose than is available in tablet form (see DOSAGE AND ADMINISTRATION).
Heart Failure:
During baseline-controlled clinical trials, in patients receiving digitalis and diuretics, single doses of lisinopril resulted in decreases in
pulmonary capillary wedge pressure, systemic vascular resistance and blood pressure accompanied by an increase in cardiac output
and no change in heart rate.
In two placebo controlled, 12-week clinical studies using doses of lisinopril up to 20 mg, lisinopril as adjunctive therapy to digitalis
and diuretics improved the following signs and symptoms due to congestive heart failure: edema, rales, paroxysmal nocturnal dyspnea
and jugular venous distention. In one of the studies, beneficial response was also noted for: orthopnea, presence of third heart sound
and the number of patients classified as NYHA Class III and IV. Exercise tolerance was also improved in this study. The once-daily
dosing for the treatment of congestive heart failure was the only dosage regimen used during clinical trial development and was
determined by the measurement of hemodynamic response. A large (over 3000 patients) survival study, the ATLAS Trial, comparing
2.5 and 35 mg of lisinopril in patients with heart failure, showed that the higher dose of lisinopril had outcomes at least as favorable as
the lower dose.
Acute Myocardial Infarction:
The Gruppo Italiano per lo Studio della Sopravvienza nell’Infarto Miocardico (GISSI-3) study was a multicenter, controlled,
randomized, unblinded clinical trial conducted in 19,394 patients with acute myocardial infarction admitted to a coronary care unit.
It was designed to examine the effects of short-term (6 week) treatment with lisinopril, nitrates, their combination, or no therapy on
short-term (6 week) mortality and on long-term death and markedly impaired cardiac function. Patients presenting within 24 hours
of the onset of symptoms who were hemodynamically stable were randomized, in a 2 x 2 factorial design, to six weeks of either 1)
lisinopril alone (n=4841), 2) nitrates alone (n=4869), 3) lisinopril plus nitrates (n=4841), or 4) open control (n=4843). All patients
received routine therapies, including thrombolytics (72percent), aspirin (84percent), and a beta-blocker (31percent), as appropriate, normally utilized
in acute myocardial infarction (MI) patients.
The protocol excluded patients with hypotension (systolic blood pressure 100 mmHg), severe heart failure, cardiogenic shock, and
renal dysfunction (serum creatinine 2 mg/dL and/or proteinuria 500 mg/24 h). Doses of lisinopril were adjusted as necessary
according to protocol (see DOSAGE AND ADMINISTRATION).
Study treatment was withdrawn at six weeks except where clinical conditions indicated continuation of treatment.
The primary outcomes of the trial were the overall mortality at 6 weeks and a combined end point at 6 months after the myocardial
infarction, consisting of the number of patients who died, had late (day 4) clinical congestive heart failure, or had extensive left
ventricular damage defined as ejection fraction 35percent or an akinetic-dyskinetic [A-D] score 45 percent. Patients receiving lisinopril
(n=9646), alone or with nitrates, had an 11percent lower risk of death (2p [two-tailed] = 0.04) compared to patients receiving no lisinopril
(n=9672) (6.4percent vs. 7.2percent, respectively) at six weeks. Although patients randomized to receive lisinopril for up to six weeks also
fared numerically better on the combined end point at 6 months, the open nature of the assessment of heart failure, substantial loss
to follow-up echocardiography, and substantial excess use of lisinopril between 6 weeks and 6 months in the group randomized to 6
weeks of lisinopril, preclude any conclusion about this end point.
Patients with acute myocardial infarction, treated with lisinopril, had a higher (9.0percent versus 3.7percent) incidence of persistent hypotension
(systolic blood pressure 90 mmHg for more than 1 hour) and renal dysfunction (2.4percent versus 1.1percent) in-hospital and at six weeks
(increasing creatinine concentration to over 3 mg/dL or a doubling or more of the baseline serum creatinine concentration). See
ADVERSE REACTIONS - Acute Myocardial Infarction.
CLINICAL STUDIES
Clinical studies of lisinopril in patients with hypertension did not include sufficient numbers of subjects aged 65 and over to determine
whether they respond differently from younger subjects. Other clinical experience in this population has not identified differences
in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually
starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of
concomitant disease or other drug therapy.
In the ATLAS trial of lisinopril in patients with congestive heart failure, 1,596 (50percent) were 65 and over, while 437 (14percent) were
75 and over. In a clinical study of lisinopril in patients with myocardial infarctions 4,413 (47percent) were 65 and over, while 1,656
(18percent) were 75 and over. In these studies, no overall differences in safety or effectiveness were observed between elderly and
younger patients, and other reported clinical experiences has not identified differences in responses between the elderly and younger
patients (see CLINICAL PHARMACOLOGY – Pharmacodynamics and Clinical Effects –Heart Failure and CLINICAL
PHARMACOLOGY – Pharmacodynamics and Clinical Effects –Acute Myocardial Infarction).
Other reported clinical experience has not identified differences in responses between elderly and younger patients, but greater
sensitivity of some older individuals cannot be ruled out.
Pharmacokinetic studies indicate that maximum blood levels and area under the plasma concentration time curve (AUC) are doubled
in older patients (see CLINICAL PHARMACOLOGY – Pharmacokinetics and Metabolism).
This drug is known to be substantially excreted by the kidney, and the risk of toxic reactions to this drug may be greater in patients
with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in
dose selection. Evaluation of patients with hypertension, congestive heart failure, or myocardial infarction should always include
assessment of renal function (see DOSAGE AND ADMINISTRATION).
This product contains FD andC Yellow No.5 (tartrazine) which may cause allergic-type reactions (including bronchial asthma) in certain
susceptible persons. Although the overall incidence of FD andC Yellow No.5 (tartrazine) sensitivity in the general population is low, it is
frequently seen in patients who also have aspirin hypersensitivity.
ADVERSE REACTIONS
ADVERSE REACTIONSLisinopril has been found to be generally well tolerated in controlled clinical trials involving 1969 patients with hypertension or heart
failure. For the most part, adverse experiences were mild and transient.
Hypertension
In clinical trials in patients with hypertension treated with lisinopril, discontinuation of therapy due to clinical adverse experiences
occurred in 5.7percent of patients. The overall frequency of adverse experiences could not be related to total daily dosage within the
recommended therapeutic dosage range.
For adverse experiences occurring in greater than 1 percent of patients with hypertension treated with lisinopril or lisinopril plus
hydrochlorothiazide in controlled clinical trials, and more frequently with lisinopril and/or lisinopril plus hydrochlorothiazide than
placebo, comparative incidence data.
Heart Failure
In patients with heart failure treated with lisinopril for up to four years, discontinuation of therapy due to clinical adverse experiences
occurred in 11.0 percent of patients. In controlled studies in patients with heart failure, therapy was discontinued in 8.1 percent of patients treated
with lisinopril for 12 weeks, compared to 7.7 percent of patients treated with placebo for 12 weeks.
The following table lists those adverse experiences which occurred in greater than 1 percent of patients with heart failure treated with
lisinopril or placebo for up to 12 weeks in controlled clinical trials, and more frequently on lisinopril than placebo.
Also observed at less then 1 percent with lisinopril but more frequent or as frequent on placebo than lisinopril in controlled trials were asthenia,
angina pectoris, nausea, dyspnea, cough, and pruritus.
Worsening of heart failure, anorexia, increased salivation, muscle cramps, back pain, myalgia, depression, chest sound abnormalities,
and pulmonary edema were also seen in controlled clinical trials, but were more common on placebo than lisinopril.
In the two-dose ATLAS trial in heart failure patients, withdrawals due to adverse events were not different between the low and high
groups, either in total number of discontinuation (17-18 percent) or in rare specific events (1 percent). The following adverse events, mostly
related to ACE inhibition, were reported more commonly in the high dose group:
Acute Myocardial Infarction
In the GISSI-3 trial, in patients treated with lisinopril for six weeks following acute myocardial infarction, discontinuation of therapy
occurred in 17.6 percent of patients.
Patients treated with lisinopril had a significantly higher incidence of hypotension and renal dysfunction compared with patients not
taking lisinopril.
In the GISSI-3 trial, hypotension (9.7 percent), renal dysfunction (2.0 percent), cough (0.5 percent), post infarction angina (0.3 percent), skin rash and generalized edema (0.01 percent), and angioedema (0.01 percent) resulted in withdrawal of treatment. In elderly patients treated with lisinopril,
discontinuation due to renal dysfunction was 4.2 percent.
Other clinical adverse experiences occurring in 0.3 percent to 1.0 percent of patients with hypertension or heart failure treated with lisinopril in
controlled clinical trials and rarer, serious, possibly drug-related events reported in uncontrolled studies or marketing experience are
listed below, and within each category are in order of decreasing severity:
Body as a Whole: Anaphylactoid reactions (see WARNINGS, Anaphylactoid Reactions and Possibly Related Reactions), syncope,
orthostatic effects, chest discomfort, pain, pelvic pain, flank pain, edema, facial edema, virus infection, fever, chills, malaise.
Cardiovascular: Cardiac arrest; myocardial infarction or cerebrovascular accident possibly secondary to excessive hypotension
in high risk patients (see WARNINGS, Hypotension); pulmonary embolism and infarction, arrhythmias (including ventricular
tachycardia, atrial tachycardia, atrial fibrillation, bradycardia and premature ventricular contractions), palpitations, transient ischemic
attacks, paroxysmal nocturnal dyspnea, orthostatic hypotension, decreased blood pressure, peripheral edema, vasculitis.
Digestive: Pancreatitis, hepatitis (hepatocellular or cholestatic jaundice) (see WARNINGS, Hepatic Failure), vomiting, gastritis,
dyspepsia, heartburn, gastrointestinal cramps, constipation, flatulence, dry mouth.
Hematologic: Rare cases of bone marrow depression, hemolytic anemia, leukopenia/neutropenia and thrombocytopenia.
Endocrine: Diabetes mellitus.
Metabolic: Weight loss, dehydration, fluid overload, gout, weight gain.
Cases of hypoglycemia in diabetic patients on oral antidiabetic agents or insulin have been reported in post-marketing experience (See
PRECAUTIONS, Drug Interactions).
Musculoskeletal: Arthritis, arthralgia, neck pain, hip pain, low back pain, joint pain, leg pain, knee pain, shoulder pain, arm pain,
lumbago.
CONTRAINDICATIONS
CONTRAINDICATIONSLisinopril tablets are contraindicated in patients who are hypersensitive to this product and in patients with a history of angioedema
related to previous treatment with an angiotensin converting enzyme inhibitor and in patients with hereditary or idiopathic
angioedema.
DRUG INTERACTIONS
Drug InteractionsHypotension - Patients on Diuretic Therapy: Patients on diuretics and especially those in whom diuretic therapy was recently
instituted, may occasionally experience an excessive reduction of blood pressure after initiation of therapy with lisinopril. The
possibility of hypotensive effects with lisinopril can be minimized by either discontinuing the diuretic or increasing the salt intake
prior to initiation of treatment with lisinopril. If it is necessary to continue the diuretic, initiate therapy with lisinopril at a dose of
5 mg daily, and provide close medical supervision after the initial dose until blood pressure has stabilized. (See WARNINGS and
DOSAGE AND ADMINISTRATION.) When a diuretic is added to the therapy of a patient receiving lisinopril an additional
antihypertensive effect is usually observed. Studies with ACE inhibitors in combination with diuretics indicate that the dose of the
ACE inhibitor can be reduced when it is given with a diuretic. (See DOSAGE AND ADMINISTRATION.)
Antidiabetics: Epidemiological studies have suggested that concomitant administration of ACE inhibitors and antidiabetic medicines
(insulins, oral hypoglycemic agents) may cause an increased blood-glucose-lowering effect with risk of hypoglycemia. This
phenomenon appeared to be more likely to occur during the first weeks of combined treatment and in patients with renal impairment.
In diabetic patients treated with oral antidiabetic agents or insulin, glycemic control should be closely monitored for hypoglycemia,
especially during the first month of treatment with an ACE inhibitor.
Non-steroidal Anti-inflammatory Agents: In some patients with compromised renal function who are being treated with non-steroidal
anti-inflammatory drugs, the co-administration of lisinopril may result in further deterioration of renal function. These effects are
usually reversible. In a study in 36 patients with mild to moderate hypertension where the antihypertensive effects of lisinopril alone
were compared to lisinopril given concomitantly with indomethacin, the use of indomethacin was associated with a reduced effect,
although the difference between the two regimens was not significant.
Other Agents: Lisinopril has been used concomitantly with nitrates and/or digoxin without evidence of clinically significant
adverse interactions. This included post myocardial infarction patients who were receiving intravenous or transdermal nitroglycerin.
No clinically important pharmacokinetic interactions occurred when lisinopril was used concomitantly with propranolol or
hydrochlorothiazide. The presence of food in the stomach does not alter the bioavailability of lisinopril.
Agents Increasing Serum Potassium: Lisinopril attenuates potassium loss caused by thiazide-type diuretics. Use of lisinopril with
potassium-sparing diuretics (e.g., spironolactone, triamterene or amiloride), potassium supplements, or potassium-containing salt
substitutes may lead to significant increases in serum potassium. Therefore, if concomitant use of these agents is indicated because of
demonstrated hypokalemia, they should be used with caution and with frequent monitoring of serum potassium. Potassium-sparing
agents should generally not be used in patients with heart failure who are receiving lisinopril.
Lithium: Lithium toxicity has been reported in patients receiving lithium concomitantly with drugs which cause elimination of
sodium, including ACE inhibitors. Lithium toxicity was usually reversible upon discontinuation of lithium and the ACE inhibitor. It is
recommended that serum lithium levels be monitored frequently if lisinopril is administered concomitantly with lithium.
Gold: Nitritoid reactions (symptoms include facial flushing, nausea, vomiting and hypotension) have been reported rarely in patients
on therapy with injectable gold (sodium aurothiomalate) and concomitant ACE inhibitor therapy including lisinopril.
Carcinogenesis, Mutagenesis, Impairment of Fertility
There was no evidence of a tumorigenic effect when lisinopril was administered for 105 weeks to male and female rats at doses up
to 90 mg/kg/day (about 56 or 9 times* the maximum recommended daily human dose, based on body weight and body surface area,
respectively). There was no evidence of carcinogenicity when lisinopril was administered for 92 weeks to (male and female) mice at doses up to 135 mg/kg/day (about 84 times the maximum recommended daily human dose). This dose was 6.8 times the maximum
human dose based on body surface area in mice.
Calculations assume a human weight of 50 kg and human body surface area of 1.62 m2.
Lisinopril was not mutagenic in the Ames microbial mutagen test with or without metabolic activation. It was also negative in a
forward mutation assay using Chinese hamster lung cells. Lisinopril did not produce single strand DNA breaks in an in vitro alkaline
elution rat hepatocyte assay. In addition, lisinopril did not produce increases in chromosomal aberrations in an in vitro test in Chinese
hamster ovary cells or in an in vivo study in mouse bone marrow.
There were no adverse effects on reproductive performance in male and female rats treated with up to 300 mg/kg/day of lisinopril.
This dose is 188 times and 30 times the maximum human dose when based on mg/kg and mg/m2, respectively.
TERATOGENIC EFFECTS
No teratogenic effects of lisinopril were seen in studies of pregnant rats, mice, and rabbits. On a mg/kg basis, the doses used were up
to 625 times (in mice), 188 times (in rats), and 0.6 times (in rabbits) the maximum recommended human dose.
INFORMATION FOR PATIENTS
Information for Patients
Angioedema: Angioedema, including laryngeal edema, may occur at any time during treatment with angiotensin-converting enzyme
inhibitors, including lisinopril. Patients should be so advised and told to report immediately any signs or symptoms suggesting
angioedema (swelling of face, extremities, eyes, lips, tongue, difficulty in swallowing or breathing) and to take no more drug until
they have consulted with the prescribing physician.
Symptomatic Hypotension: Patients should be cautioned to report lightheadedness especially during the first few days of therapy. If
actual syncope occurs, the patient should be told to discontinue the drug until they have consulted with the prescribing physician.
All patients should be cautioned that excessive perspiration and dehydration may lead to an excessive fall in blood pressure because
of reduction in fluid volume. Other causes of volume depletion such as vomiting or diarrhea may also lead to a fall in blood pressure;
patients should be advised to consult with their physician.
Hyperkalemia: Patients should be told not to use salt substitutes containing potassium without consulting their physician.
Hypoglycemia: Diabetic patients treated with oral antidiabetic agents or insulin starting an ACE inhibitor should be told to closely
monitor for hypoglycemia, especially during the first month of combined use. (See PRECAUTIONS, Drug Interactions.)
Leukopenia/Neutropenia: Patients should be told to report promptly any indication of infection (e.g., sore throat, fever) which may be
a sign of leukopenia/neutropenia.
Pregnancy: Female patients of childbearing age should be told about the consequences of second- and third-trimester exposure to
ACE inhibitors, and they should also be told that these consequences do not appear to have resulted from intrauterine ACE inhibitor
exposure that has been limited to the first trimester. These patients should be asked to report pregnancies to their physicians as soon as
possible.
NOTE: As with many other drugs, certain advice to patients being treated with lisinopril is warranted. This information is intended to
aid in the safe and effective use of this medication. It is not a disclosure of all possible adverse or intended effects.
Hypotension - Patients on Diuretic Therapy: Patients on diuretics and especially those in whom diuretic therapy was recently
instituted, may occasionally experience an excessive reduction of blood pressure after initiation of therapy with lisinopril. The
possibility of hypotensive effects with lisinopril can be minimized by either discontinuing the diuretic or increasing the salt intake
prior to initiation of treatment with lisinopril. If it is necessary to continue the diuretic, initiate therapy with lisinopril at a dose of
5 mg daily, and provide close medical supervision after the initial dose until blood pressure has stabilized. (See WARNINGS and
DOSAGE AND ADMINISTRATION.) When a diuretic is added to the therapy of a patient receiving lisinopril an additional
antihypertensive effect is usually observed. Studies with ACE inhibitors in combination with diuretics indicate that the dose of the
ACE inhibitor can be reduced when it is given with a diuretic. (See DOSAGE AND ADMINISTRATION.)
Antidiabetics: Epidemiological studies have suggested that concomitant administration of ACE inhibitors and antidiabetic medicines
(insulins, oral hypoglycemic agents) may cause an increased blood-glucose-lowering effect with risk of hypoglycemia. This
phenomenon appeared to be more likely to occur during the first weeks of combined treatment and in patients with renal impairment.
In diabetic patients treated with oral antidiabetic agents or insulin, glycemic control should be closely monitored for hypoglycemia,
especially during the first month of treatment with an ACE inhibitor.
Non-steroidal Anti-inflammatory Agents: In some patients with compromised renal function who are being treated with non-steroidal
anti-inflammatory drugs, the co-administration of lisinopril may result in further deterioration of renal function. These effects are
usually reversible. In a study in 36 patients with mild to moderate hypertension where the antihypertensive effects of lisinopril alone
were compared to lisinopril given concomitantly with indomethacin, the use of indomethacin was associated with a reduced effect,
although the difference between the two regimens was not significant.
Other Agents: Lisinopril has been used concomitantly with nitrates and/or digoxin without evidence of clinically significant
adverse interactions. This included post myocardial infarction patients who were receiving intravenous or transdermal nitroglycerin.
No clinically important pharmacokinetic interactions occurred when lisinopril was used concomitantly with propranolol or
hydrochlorothiazide. The presence of food in the stomach does not alter the bioavailability of lisinopril.
Agents Increasing Serum Potassium: Lisinopril attenuates potassium loss caused by thiazide-type diuretics. Use of lisinopril with
potassium-sparing diuretics (e.g., spironolactone, triamterene or amiloride), potassium supplements, or potassium-containing salt
substitutes may lead to significant increases in serum potassium. Therefore, if concomitant use of these agents is indicated because of
demonstrated hypokalemia, they should be used with caution and with frequent monitoring of serum potassium. Potassium-sparing
agents should generally not be used in patients with heart failure who are receiving lisinopril.
Lithium: Lithium toxicity has been reported in patients receiving lithium concomitantly with drugs which cause elimination of
sodium, including ACE inhibitors. Lithium toxicity was usually reversible upon discontinuation of lithium and the ACE inhibitor. It is
recommended that serum lithium levels be monitored frequently if lisinopril is administered concomitantly with lithium.
Gold: Nitritoid reactions (symptoms include facial flushing, nausea, vomiting and hypotension) have been reported rarely in patients
on therapy with injectable gold (sodium aurothiomalate) and concomitant ACE inhibitor therapy including lisinopril.
Carcinogenesis, Mutagenesis, Impairment of Fertility
There was no evidence of a tumorigenic effect when lisinopril was administered for 105 weeks to male and female rats at doses up
to 90 mg/kg/day (about 56 or 9 times* the maximum recommended daily human dose, based on body weight and body surface area,
respectively). There was no evidence of carcinogenicity when lisinopril was administered for 92 weeks to (male and female) mice at doses up to 135 mg/kg/day (about 84 times the maximum recommended daily human dose). This dose was 6.8 times the maximum
human dose based on body surface area in mice.
Calculations assume a human weight of 50 kg and human body surface area of 1.62 m2.
Lisinopril was not mutagenic in the Ames microbial mutagen test with or without metabolic activation. It was also negative in a
forward mutation assay using Chinese hamster lung cells. Lisinopril did not produce single strand DNA breaks in an in vitro alkaline
elution rat hepatocyte assay. In addition, lisinopril did not produce increases in chromosomal aberrations in an in vitro test in Chinese
hamster ovary cells or in an in vivo study in mouse bone marrow.
There were no adverse effects on reproductive performance in male and female rats treated with up to 300 mg/kg/day of lisinopril.
This dose is 188 times and 30 times the maximum human dose when based on mg/kg and mg/m2, respectively.
NURSING MOTHERS
Nursing Mothers:Milk of lactating rats contains radioactivity following administration of 14C lisinopril. It is not known whether this drug is excretedin human milk. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in nursinginfants from ACE inhibitors, a decision should be made whether to discontinue nursing or discontinue lisinopril, taking into accountthe importance of the drug to the mother.
PEDIATRIC USE
Pediatric Use:Antihypertensive effects of lisinopril have been established in hypertensive pediatric patients aged 6 to 16 years.There are no data on the effect of lisinopril on blood pressure in pediatric patients under the age 6 or in pediatric patients withglomerular filtration rate < 30 mL/min/1.73 m2. (See CLINICAL PHARMACOLOGY, Pharmacokinetics and Metabolism andPharmacodynamics and Clinical Effects, and DOSAGE AND ADMINISTRATION.)
GERIATRIC USE
Geriatric Use:Clinical studies of lisinopril in patients with hypertension did not include sufficient numbers of subjects aged 65 and over to determine
whether they respond differently from younger subjects. Other clinical experience in this population has not identified differences
in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually
starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of
concomitant disease or other drug therapy.
In the ATLAS trial of lisinopril in patients with congestive heart failure, 1,596 (50 percent) were 65 and over, while 437 (14 percent) were
75 and over. In a clinical study of lisinopril in patients with myocardial infarctions 4,413 (47 percent) were 65 and over, while 1,656
(18 percent) were 75 and over. In these studies, no overall differences in safety or effectiveness were observed between elderly and
younger patients, and other reported clinical experiences has not identified differences in responses between the elderly and younger
patients (see CLINICAL PHARMACOLOGY – Pharmacodynamics and Clinical Effects –Heart Failure and CLINICAL
PHARMACOLOGY – Pharmacodynamics and Clinical Effects –Acute Myocardial Infarction).
Other reported clinical experience has not identified differences in responses between elderly and younger patients, but greater
sensitivity of some older individuals cannot be ruled out.
Pharmacokinetic studies indicate that maximum blood levels and area under the plasma concentration time curve (AUC) are doubled
in older patients (see CLINICAL PHARMACOLOGY – Pharmacokinetics and Metabolism).
This drug is known to be substantially excreted by the kidney, and the risk of toxic reactions to this drug may be greater in patients
with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in
dose selection. Evaluation of patients with hypertension, congestive heart failure, or myocardial infarction should always include
assessment of renal function (see DOSAGE AND ADMINISTRATION).
This product contains FD and C Yellow No.5 (tartrazine) which may cause allergic-type reactions (including bronchial asthma) in certain
susceptible persons. Although the overall incidence of FD and C Yellow No.5 (tartrazine) sensitivity in the general population is low, it is
frequently seen in patients who also have aspirin hypersensitivity.
OVERDOSAGE
OVERDOSAGEFollowing a single oral dose of 20 g/kg no lethality occurred in rats, and death occurred in one of 20 mice receiving the same dose.The most likely manifestation of overdosage would be hypotension, for which the usual treatment would be intravenous infusion ofnormal saline solution.Lisinopril can be removed by hemodialysis. (See WARNINGS, Anaphylactoid Reactions During Membrane Exposure.) page 12 of 13 DOSAGE AND ADMINISTRATIONHypertensionInitial Therapy: In patients with uncomplicated essential hypertension not on diuretic therapy, the recommended initial dose is 10mg once a day. Dosage should be adjusted according to blood pressure response. The usual dosage range is 20 to 40 mg per dayadministered in a single daily dose. The antihypertensive effect may diminish toward the end of the dosing interval regardless ofthe administered dose, but most commonly with a dose of 10 mg daily. This can be evaluated by measuring blood pressure justprior to dosing to determine whether satisfactory control is being maintained for 24 hours. If it is not, an increase in dose shouldbe considered. Doses up to 80 mg have been used but do not appear to give greater effect. If blood pressure is not controlled withlisinopril alone, a low dose of a diuretic may be added. Hydrochlorothiazide, 12.5 mg has been shown to provide an additive effect.After the addition of a diuretic, it may be possible to reduce the dose of lisinopril.Diuretic Treated Patients: In hypertensive patients who are currently being treated with a diuretic, symptomatic hypotension mayoccur occasionally following the initial dose of lisinopril. The diuretic should be discontinued, if possible, for two to three days beforebeginning therapy with lisinopril tablet to reduce the likelihood of hypotension. (See WARNINGS.) The dosage of lisinopril shouldbe adjusted according to blood pressure response. If the patient's blood pressure is not controlled with lisinopril alone, diuretic therapymay be resumed as described above.If the diuretic cannot be discontinued, an initial dose of 5 mg should be used under medical supervision for at least two hours and untilblood pressure has stabilized for at least an additional hour.
WARNINGS AND PRECAUTIONS
(See WARNINGS snd PRECAUTIONS.)HOW SUPPLIED
HOW SUPPLIED2.5 mg Tablets – White to off-white, round shaped, biconvex, uncoated tablets, debossed with ‘A’ on one side and ‘20’ on the other side.
Bottles of 30 NDC 65862-037-30 (Child Resistant Closure)
Bottles of 100 NDC 65862-037-01 (Child Resistant Closure)
Bottles of 100 NDC 65862-037-00 (Non Child Resistant Closure)
Bottles of 500 NDC 65862-037-05 (Non Child Resistant Closure)
5 mg Tablets – Light red colored, round shaped, biconvex, uncoated tablets, debossed with ‘A’ on one side and on other side with ‘2 and 1’ on either side of score line.
Bottles of 30 NDC 65862-038-30 (Child Resistant Closure)
Bottles of 100 NDC 65862-038-01 (Child Resistant Closure)
Bottles of 100 NDC 65862-038-00 (Non Child Resistant Closure)
Bottles of 500 NDC 65862-038-05 (Non Child Resistant Closure)
10 mg Tablets – Light yellow colored, round shaped, biconvex, uncoated tablets, debossed with ‘A’ on one side and on other side with ‘22’.
Bottles of 30 NDC 65862-039-30 (Child Resistant Closure)
Bottles of 100 NDC 65862-039-01 (Child Resistant Closure)
Bottles of 100 NDC 65862-039-00 (Non Child Resistant Closure)
Bottles of 500 NDC 65862-039-05 (Non Child Resistant Closure)
20 mg Tablets – Light yellow colored, capsule shaped, biconvex, uncoated tablets, debossed with ‘A’ on one side and on other side with ‘23’.
Bottles of 30 NDC 65862-040-30 (Child Resistant Closure)
Bottles of 100 NDC 65862-040-01 (Child Resistant Closure)
Bottles of 100 NDC 65862-040-00 (Non Child Resistant Closure)
30 mg Tablets – Light yellow colored, round shaped, uncoated tablets, debossed with ‘A’ on one side and on other side with ‘24’.
Bottles of 30 NDC 65862-041-30 (Child Resistant Closure)
Bottles of 100 NDC 65862-041-01 (Child Resistant Closure)
Bottles of 100 NDC 65862-041-00 (Non Child Resistant Closure)
40 mg Tablets – Light yellow colored, capsule shaped, biconvex, uncoated tablets, debossed with ‘A’ on one side and on other side with ‘25’.
Bottles of 30 NDC 65862-042-30 (Child Resistant Closure)
Bottles of 100 NDC 65862-042-01 (Child Resistant Closure)
Bottles of 100 NDC 65862-042-00 (Non Child Resistant Closure)
Storage
Store at controlled room temperature, 20°-25°C (68°-77°F) [see USP ]. Protect from moisture, freezing and excessive heat.
Dispense in a tight, light-resistant container as defined in the USP, with a child-resistant closure (as required).
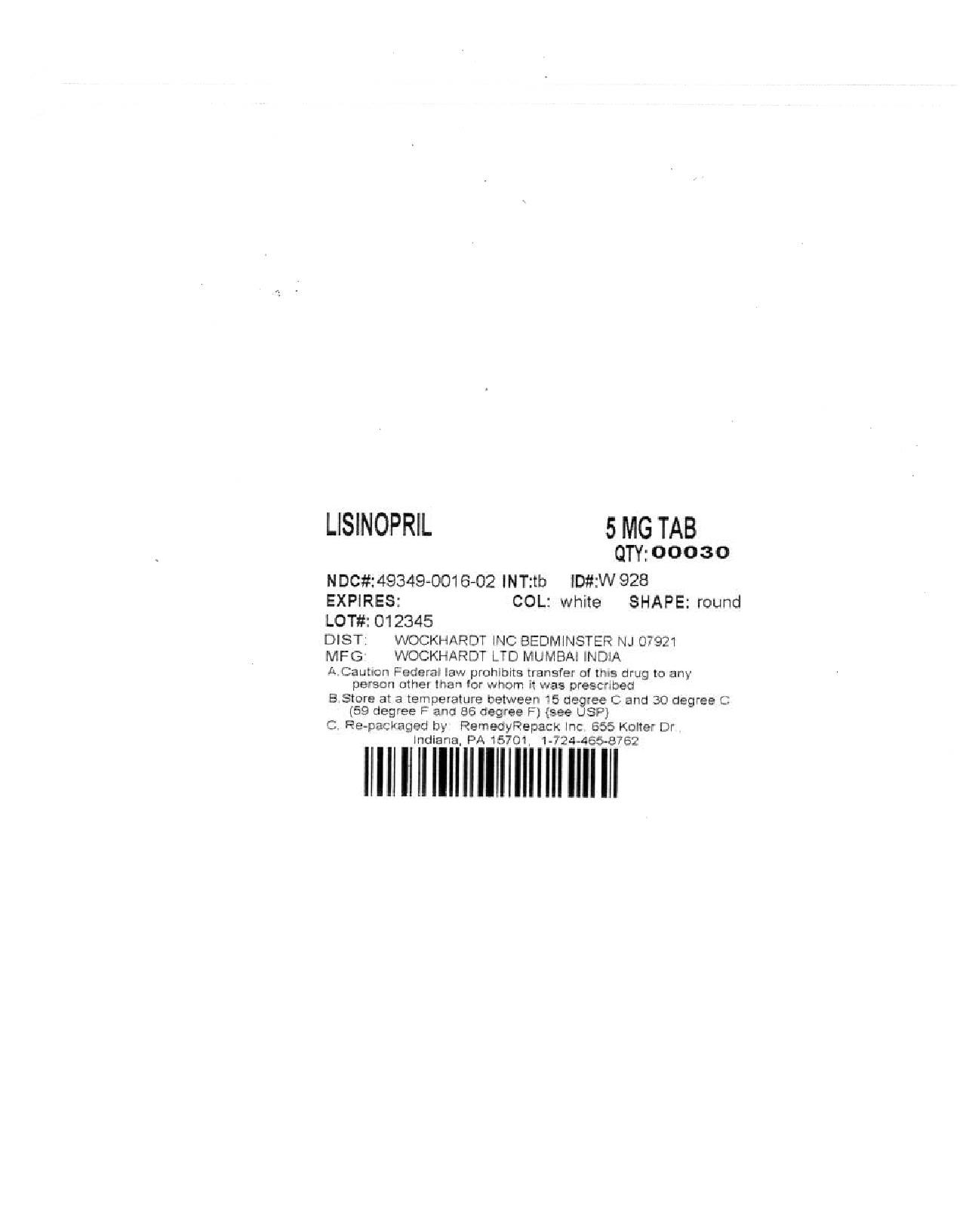
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
DRUG: LisinoprilGENERIC: Lisinopril
DOSAGE: TABLET
ADMINSTRATION: ORAL
NDC: 49349-016-02
STRENGTH:5 mg
COLOR: white
SHAPE: ROUND
SCORE: Two even pieces
SIZE: 5 mm
IMPRINT: 30
QTY: 30
| LISINOPRIL
lisinopril tablet |
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
| Marketing Information | |||
| Marketing Category | Application Number or Monograph Citation | Marketing Start Date | Marketing End Date |
| ANDA | ANDA075659 | 09/16/2010 | |
| Labeler - REMEDYREPACK INC. (829572556) |