FLEBOGAMMA DIF
-
human immunoglobulin g injection, solution
Instituto Grifols, S.A.
----------
|
||||||||||||||||||||||||||||||
FULL PRESCRIBING INFORMATION
Flebogamma® 10% DIF
Immune Globulin Intravenous (Human)
10% Liquid Preparation
WARNING: ACUTE RENAL DYSFUNCTION AND ACUTE RENAL FAILURE
- Use of immune globulin intravenous (IGIV) products, particularly those containing sucrose, has been reported to be associated with renal dysfunction, acute renal failure, osmotic nephropathy, and death (1). Patients at risk of acute renal failure include those with any degree of pre-existing renal insufficiency, diabetes mellitus, advanced age (above 65 years of age), volume depletion, sepsis, paraproteinemia, or those receiving known nephrotoxic drugs (see Warnings and Precautions [5.2]). Flebogamma 10% DIF does not contain sucrose.
- For patients at risk of renal dysfunction or failure, administer Flebogamma 10% DIF at the minimum infusion rate practicable (see Dosage and Administration [2.3], Warnings and Precautions [5.2]).
1 INDICATIONS AND USAGE
Flebogamma 10% DIF is a human immune globulin intravenous (IGIV) that is indicated for the treatment of primary immune deficiency (PI) including the humoral immune defect in common variable immunodeficiency, x-linked agammaglobulinemia, severe combined immunodeficiency, and Wiskott-Aldrich syndrome.
2. DOSAGE AND ADMINISTRATION
For Intravenous Use Only
2.1 Preparation and Handling
- Flebogamma 10% DIF is a clear or slightly opalescent, colorless solution. Inspect the drug product visually for particulate matter and discoloration prior to administration, whenever solution and container permit. Do not use if the solution is cloudy, turbid, or if it contains particulates.
- Do not shake.
- Do not freeze.
- Flebogamma 10% DIF should be administered at room temperature.
- The vial is for single use only.
- Flebogamma 10% DIF contains no preservative. Once the vial has been entered under aseptic conditions, its contents should be used promptly. Because the solution contains no preservative, Flebogamma 10% DIF should be infused as soon as possible.
- Do not mix Flebogamma 10% DIF with other IGIV products or other intravenous medications.
- Infuse Flebogamma 10% DIF using a separate infusion line.
- If larger doses of Flebogamma 10% DIF are to be administered, several vials may be pooled into sterile infusion bags using aseptic technique.
2.2 Dose
As there are significant differences in the half-life of IgG among patients with PI, the frequency and amount of immunoglobulin therapy may vary from patient to patient. Dosing should be adjusted according to the clinical response.
The recommended dose of Flebogamma 10% DIF for patients with PI is 300 to 600 mg/kg body weight (3.0 to 6.0 mL/kg), administered every 3 to 4 weeks. Adjust the dosage over time to achieve the desired serum trough levels and clinical responses. No randomized controlled trial data are available to determine an optimum target trough serum IgG level.
2.3 Administration
It has been reported that the frequency of adverse drug reactions to IGIV increases with the infusion rate. Initial infusion rates should be slow. If there are no adverse drug reactions, the infusion rate for subsequent infusions can be slowly increased to the maximum rate. For patients experiencing adverse drug reactions, it is advisable to reduce the infusion rate in subsequent infusions, or administer IGIV at a 5% concentration.
| Indication | Dose | Initial Infusion Rate | Maintenance Infusion Rate (if tolerated) |
| PI | 300-600 mg/kg every 3-4 weeks | 0.01 mL/kg/minute (1 mg/kg/min) | 0.08 mL/kg/minute (8 mg/kg/min) |
Monitor patient vital signs throughout the infusion. Slow or stop infusion if adverse reactions occur. If symptoms subside promptly, the infusion may be resumed at a lower rate that is comfortable for the patient.
Ensure that patients with pre-existing renal insufficiency are not volume depleted. For patients judged to be at risk for renal dysfunction or thrombotic events, administer Flebogamma 10% DIF at the minimum infusion rate practicable, and consider discontinuation of administration if renal function deteriorates (see Warnings and Precautions [5.2, 5.4]).
3. DOSAGE FORMS AND STRENGTHS
Flebogamma 10% DIF is a liquid solution containing 10% IgG (100 mg/mL).
4 CONTRAINDICATIONS
- Flebogamma 10% DIF is contraindicated in patients who have had a history of anaphylactic or severe systemic reactions to the administration of human immune globulin.
- Flebogamma 10% DIF is contraindicated in IgA deficient patients with antibodies to IgA and a history of hypersensitivity.
5 WARNINGS AND PRECAUTIONS
- Weigh the potential risks and benefits of Flebogamma 10% DIF against those of alternative therapies in all patients for whom Flebogamma 10% DIF is being considered.
- Before prescribing Flebogamma 10% DIF, the physician should discuss risks and benefits of its use with patients.
5.1 Hypersensitivity
Severe hypersensitivity reactions may occur (see Contraindications [4]). In case of hypersensitivity, discontinue Flebogamma 10% DIF infusion immediately and institute appropriate treatment. Medications such as epinephrine should be available for immediate treatment of acute hypersensitivity reactions.
Flebogamma 10% DIF contains trace amounts of IgA (less than 100 μg/mL) (see Description [11]). Patients with antibodies to IgA have a greater risk of developing potentially severe hypersensitivity and anaphylactic reactions. Flebogamma 10% DIF is contraindicated in patients with antibodies against IgA and a history of hypersensitivity reaction (see Contraindications [4]).
5.2 Renal Dysfunction/Failure
Acute renal dysfunction/failure, osmotic nephropathy, and death may occur upon use of Flebogamma 10% DIF. Ensure that patients are not volume-depleted before administering Flebogamma 10% DIF. In patients who are at risk of developing renal dysfunction because of pre-existing renal insufficiency or predisposition to acute renal failure (such as diabetes mellitus, age greater than 65 years, volume depletion, sepsis, paraproteinemia, use of concomitant nephrotoxic drugs, etc.), administer Flebogamma 10% DIF at the minimum rate of infusion practicable (2) (see Dosage and Administration [2.3]).
Periodic monitoring of renal function and urine output is particularly important in patients judged to be at increased risk of developing acute renal failure (1). Assess renal function, including measurement of blood urea nitrogen (BUN) and serum creatinine, before the initial infusion of Flebogamma 10% DIF and at appropriate intervals thereafter. If renal function deteriorates, consider discontinue use of Flebogamma 10% DIF.
5.3 Hyperproteinemia, Increased Serum Viscosity, and Hyponatremia
Hyperproteinemia, increased serum viscosity and hyponatremia may occur in patients receiving Flebogamma 10% DIF therapy. It is clinically critical to distinguish true hyponatremia from a pseudohyponatremia that is temporally or causally related to hyperproteinemia with concomitant decreased calculated serum osmolarity or elevated osmolar gap, because treatment aimed at decreasing serum free water in patients with pseudohyponatremia may lead to volume depletion, a further increase in serum viscosity and a higher risk of thrombotic events.
5.4 Thrombotic Events
Thrombotic events may occur during or following treatment with Flebogamma 10% DIF (8-10). Patients at risk include those with a history of atherosclerosis, multiple cardiovascular risk factors, advanced age, impaired cardiac output, coagulation disorders, prolonged periods of immobilization, and known or suspected hyperviscosity.
Consider baseline assessment of blood viscosity in patients at risk for hyperviscosity, including those with cryoglobulins, fasting chylomicronemia/markedly high triacylglycerols (triglycerides), or monoclonal gammopathies. For patients judged to be at risk of developing thrombotic events, administer Flebogamma 10% DIF at the minimum rate of infusion practicable (see Dosage and Administration [2.3]).
5.5 Aseptic Meningitis Syndrome (AMS)
AMS may occur infrequently with Flebogamma 10% DIF treatment. Discontinuation of IGIV treatment has resulted in remission of AMS within several days without sequelae (3-4).
AMS is characterized by the following signs and symptoms: severe headache, nuchal rigidity, drowsiness, fever, photophobia, painful eye movements, nausea, and vomiting (see Patient Counseling Information [17]). Cerebrospinal fluid (CSF) studies frequently reveal pleocytosis up to several thousand cells per cubic millimeter, predominantly from the granulocytic series and elevated protein levels up to several hundred mg/dL, but negative culture results. Conduct a thorough neurological examination to patients exhibiting such signs and symptoms, including CSF studies, to rule out other causes of meningitis.
AMS may occur more frequently following high doses (2 g/kg) and/or rapid infusion of IGIV.
5.6 Hemolysis
Flebogamma 10% DIF may contain blood group antibodies that can act as hemolysins and induce in vivo coating of red blood cells (RBCs) with immunoglobulin, causing a positive direct antiglobulin reaction and hemolysis (5-6). Delayed hemolytic anemia may develop subsequent to Flebogamma 10% DIF therapy due to enhanced RBC sequestration (7), and acute hemolysis, consistent with intravascular hemolysis, has been reported.
Monitor patients for clinical signs and symptoms of hemolysis. If signs and/or symptoms of hemolysis are present after Flebogamma 10% DIF infusion, perform appropriate confirmatory laboratory testing (see Patient Counseling Information [17]).
5.7 Transfusion-Related Acute Lung Injury (TRALI)
Non-cardiogenic pulmonary edema may occur in patients following Flebogamma 10% DIF treatment (11). TRALI is characterized by severe respiratory distress, pulmonary edema, hypoxemia, normal left ventricular function, and fever. Symptoms typically appear within 1 to 6 hours following treatment.
Monitor patients for pulmonary adverse reactions (see Patient Counseling Information [17]). If TRALI is suspected, perform appropriate tests for the presence of anti-neutrophil antibodies and anti-HLA antibodies in both the product and patient serum. TRALI may be managed using oxygen therapy with adequate ventilatory support.
5.8 Infusion Reactions
All patients, but especially individuals receiving Flebogamma 10% DIF for the first time or being restarted on the product after a treatment hiatus of more than 8 weeks, may be at a higher risk for the development of fever, chills, nausea, and vomiting. Careful monitoring of recipients and adherence to recommendations regarding dosage and administration may reduce the risk of these types of events (see Dosage and Administration [2.3]).
5.9 Transmissible Infectious Agents
Because Flebogamma 10% DIF is made from human plasma, it may carry a risk of transmitting infectious agents, e.g., viruses, and theoretically, the Creutzfeldt-Jakob (CJD) agent. No cases of transmission of viral diseases or CJD have ever been identified for Flebogamma 10% DIF. All infections suspected by a physician possibly to have been transmitted by this product should be reported by the physician or other healthcare provider to Grifols Biologicals at 1-888-474-3657. Before prescribing or administering Flebogamma 10% DIF, the physician should discuss the risks and benefits of its use with the patient (see Patient Counseling Information [17]).
5.10 Monitoring: Laboratory Tests
- Periodic monitoring of renal function and urine output is particularly important in patients judged to be at increased risk of developing acute renal failure. Assess renal function, including measurement of BUN and serum creatinine, before the initial infusion of Flebogamma 10% DIF and at appropriate intervals thereafter.
- Consider baseline assessment of blood viscosity in patients at risk for hyperviscosity, including those with cryoglobulins, fasting chylomicronemia/markedly high triacylglycerols (triglycerides), or monoclonal gammopathies, because of the potentially increased risk of thrombosis.
- If signs and/or symptoms of hemolysis are present after an infusion of Flebogamma 10% DIF, perform appropriate laboratory testing for confirmation.
- If TRALI is suspected, perform appropriate tests for the presence of anti-neutrophil antibodies and anti-HLA antibodies in both the product and patient's serum.
5.11 Interference with Laboratory Tests
After infusion of IgG, the transitory rise of the various passively transferred antibodies in the patient's blood may yield positive serological testing results, with the potential for misleading interpretation. Passive transmission of antibodies to erythrocyte antigens (e.g., A, B, and D) may cause a positive direct or indirect antiglobulin (Coombs') test.
6 ADVERSE REACTIONS
Serious adverse reactions observed with Flebogamma 10% DIF were back pain, chest discomfort, headache, chest pain, maculopathy, rigors, tachycardia, bacterial pneumonia, and vasovagal syncope.
The most common adverse reactions (reported in ≥ 5% of clinical trial subjects) occurring during or within 72 hours of the end of an infusion were headache, chills, fever, shaking, fatigue, malaise, anxiety, back pain, muscle cramps, abdominal cramps, blood pressure changes, chest tightness, palpitations, tachycardia, nausea, vomiting, cutaneous reactions, wheezing, rash, arthralgia, and edema (see Tables 2 and 3).
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
In a multicenter, open-label, non-randomized, historically controlled clinical study, 46 individuals with primary humoral immunodeficiency received infusion doses of Flebogamma 10% DIF at 300 to 600 mg/kg body weight every 3 weeks (mean dose 469 mg/kg) or 4 weeks (mean dose 457 mg/kg) for up to 12 months (see Clinical Studies [14.1]). Routine pre-medication was not allowed. Of the 601 infusions administered, 130 infusions (22%) in 21 (47%) subjects were given pre-medications (antipyretic, antihistamine, or antiemetic agent) because of experience with consecutive infusion-related adverse reactions.
One subject experienced four serious adverse events (AEs, bacterial pneumonia, subcutaneous abscess and two episodes of cellulitis) and withdrew from the study. Two other subjects who participated in the study discontinued prematurely due to AEs (back pain/chest pain/headache; and chills/tachycardia). Three subjects experienced four serious non-related AEs (drug abuse/depression; hernia; and sinusitis).
Forty-five (98%) subjects experienced at least 1 AE irrespective of the relationship with the product, and these subjects reported a total of 723 AEs. Thirty-eight subjects (83%) had an adverse reaction at some time during the study that was considered product-related. Of the 21 subjects receiving pre-medications, 12 (57%) subjects reported adverse reactions during or within 72 hours after the infusion in 48 of the 130 pre-medicated infusions (37%).
|
Adverse Event | Subjects (%)
[N=46] | Infusions (%)
[N=601] |
|---|---|---|
| Headache | 24 (52%) | 67 (11%) |
| Rigors | 17 (37%) | 37 (6%) |
| Pyrexia | 15 (33%) | 27 (5%) |
| Tachycardia | 10 (22%) | 18 (3%) |
| Hypotension | 9 (20%) | 11 (2%) |
| Back pain | 8 (17%) | 27 (5%) |
| Myalgia | 8 (17%) | 17 (3%) |
| Body temperature increased | 4 (9%) | 6 (1%) |
| Nausea | 4 (9%) | 6 (1%) |
| Pain | 4 (9%) | 8 (1%) |
| Chest discomfort | 3 (7%) | 4 (1%) |
| Chest pain | 3 (7%) | 5 (1%) |
| Infusion site reaction | 3 (7%) | 4 (1%) |
| Pain in extremity | 3 (7%) | 3 (0.5%) |
The total number of adverse events occurring during or within 72 hours after the end of an infusion, irrespective of causality, was 359, excluding non-serious infections.
Table 3 lists the AEs that occurred in greater than 5% of subjects during a Flebogamma 10% DIF infusion or within 72 hours after the end of an infusion, irrespective of causality.
|
Adverse Event | Subjects (%)
[N=46] | Infusions (%) [N=601] |
|---|---|---|
| Headache | 28 (61%) | 71 (12%) |
| Pyrexia | 17 (37%) | 27 (5%) |
| Rigors | 17 (37%) | 37 (6%) |
| Back pain | 13 (28%) | 29 (5%) |
| Cough or Productive cough | 12 (26%) | 5 (1%) |
| Nausea | 12 (26%) | 8 (1%) |
| Hypotension | 10 (22%) | 13 (2%) |
| Tachycardia | 10 (22%) | 19 (3%) |
| Myalgia | 9 (20%) | 17 (3%) |
| Diarrhea | 8 (17%) | 2 (0.3%) |
| Infusion site reaction | 8 (17%) | 8 (1%) |
| Pharyngolaryngeal pain | 7 (15%) | 3 (1%) |
| Nasal congestion | 7 (15%) | 2 (0.3%) |
| Postnasal drip | 7 (15%) | 4 (1%) |
| Arthralgia | 6 (13%) | 2 (0.3%) |
| Conjunctivitis | 6 (13%) | 2 (0.3%) |
| Pain | 6 (13%) | 10 (2%) |
| Vomiting | 6 (13%) | 0 (0%) |
| Dizziness | 5 (11%) | 3 (1%) |
| Fatigue | 5 (11%) | 1 (0.2%) |
| Urinary tract infection | 5 (11%) | 4 (1%) |
| Chest pain | 5 (11%) | 4 (1%) |
| Ear pain | 5 (11%) | 1 (0.2%) |
| Pain in extremity | 5 (11%) | 2 (0.3%) |
| Dyspnea | 5 (11%) | 0 (0%) |
| Rhinorrhea | 4 (9%) | 1 (0.2%) |
| Wheezing | 4 (9%) | 4 (1%) |
| Body temperature increased | 4 (9%) | 6 (1%) |
| Neck pain | 4 (9%) | 2 (0.3%) |
| Sinus pain | 4 (9%) | 1 (0.2%) |
| Chest discomfort | 4 (9%) | 4 (1%) |
| Crackles lung | 4 (9%) | 2 (0.3%) |
| Abdominal pain | 3 (7%) | 2 (0.3%) |
| Dyspepsia | 3 (7%) | 1 (0.2%) |
| Toothache | 3 (7%) | 0 (0%) |
| Gastroesophageal reflux disease | 3 (7%) | 0 (0%) |
| Lymphadenopathy | 3 (7%) | 3 (1%) |
| Respiratory tract congestion | 3 (7%) | 0 (0%) |
| Fall | 3 (7%) | 1 (0.2%) |
| Hypertension | 3 (7%) | 4 (1%) |
In this study, the upper bound of the 1-sided 95% confidence interval for the proportion of Flebogamma 10% DIF infusions associated with one or more AEs was 37.8% (total infusions: 208; actual proportions: 34.6%). The average percent of infusions with AEs during or within 72 hours after the end of an infusion for each individual subject was 36.7% and the upper bound of the 1-sided 95% confidence interval was 43.9%.
AE reporting was based upon a clinical protocol precluding pre-medication against AEs. Pre-medication could be utilized only after the first 2 infusions only in those patients that exhibited adverse events.
Forty-three of the 46 subjects enrolled in this study had a negative Coombs test at baseline. Of these 43 subjects, 10 (23.3%) developed a positive Coombs test at some time during the study. However, no subjects showed evidence of hemolytic anemia.
6.2 Post-marketing Experience
Because adverse reactions are reported voluntarily post-approval from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to product exposure. The following adverse reactions have been identified during post approval use of intravenous immune globulins, including Flebogamma 5% (see References [15]).
| Infusion reactions | Hypersensitivity (e.g., anaphylaxis), headache, diarrhea, tachycardia, fever, fatigue, dizziness, malaise, chills, flushing, urticaria or other skin reactions, wheezing or other chest discomfort, nausea, vomiting, rigors, back pain, myalgia, arthralgia, and changes in blood pressure |
| Renal | Acute renal dysfunction/failure, osmotic nephropathy |
| Respiratory | Apnea, Acute Respiratory Distress Syndrome (ARDS), Transfusion-Related Acute Lung Injury (TRALI), cyanosis, hypoxemia, pulmonary edema, dyspnea, bronchospasm |
| Cardiovascular | Cardiac arrest, thromboembolism, vascular collapse, hypotension |
| Neurological | Coma, loss of consciousness, seizures, tremor, aseptic meningitis syndrome |
| Integumentary | Stevens-Johnson Syndrome, epidermolysis, erythema multiformae, dermatitis (e.g., bullous dermatitis) |
| Hematologic | Pancytopenia, leukopenia, hemolysis, positive direct antiglobulin (Coombs) test |
| Musculoskeletal | Back pain |
| Gastrointestinal | Hepatic dysfunction, abdominal pain |
| General/Body as a Whole | Pyrexia, rigors |
7 DRUG INTERACTIONS
Passive transfer of antibodies may transiently impair the immune response to live attenuated virus vaccines such as measles, mumps, and rubella. Inform the immunizing physician of recent therapy with Flebogamma 10% DIF so that appropriate measures may be taken (see Patient Counseling Information [17]).
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category C. Animal reproduction studies have not been performed with Flebogamma 10% DIF. It is also not known whether Flebogamma 10% DIF can cause fetal harm when administered to a pregnant woman or can affect reproduction capacity. Flebogamma 10% DIF should be given to a pregnant woman only if clearly needed. Immunoglobulins cross the placenta from maternal circulation increasingly after 30 weeks of gestation.
8.3 Nursing Mothers
Use of Flebogamma 10% DIF has not been evaluated in nursing mothers.
8.4 Pediatric Use
Three (3) pediatric patients with primary humoral immunodeficiency (two between the ages of 6 and 10, and one 16 year old) were included in the clinical evaluation of Flebogamma 10% DIF. This number of subjects is too small to establish safety and efficacy in the pediatric population (see Clinical Studies [14]).
8.5 Geriatric Use
Use caution when administering Flebogamma 10% DIF to patients over 65 years of age who are judged to be at increased risk for developing certain adverse reactions such as thromboembolic events and acute renal failure (see Boxed Warning, Warnings and Precautions [5.2]). Do not exceed the recommended dose, and infuse Flebogamma 10% DIF at the minimum infusion rate practicable.
One (1) patient with primary humoral immunodeficiency at or over the age of 65 was included within the clinical evaluation of Flebogamma 10% DIF. This number of geriatric patients was too small for separate evaluation from the younger patients for safety or efficacy (see Clinical Studies [14]).
11 DESCRIPTION
Flebogamma 10% DIF is a ready to use, sterile, clear or slightly opalescent and colorless to pale yellow, liquid preparation of highly purified immunoglobulin (IgG) obtained from human plasma pools. The purification process includes cold ethanol fractionation, polyethylene glycol precipitation, ion exchange chromatography, low pH treatment, pasteurization, solvent detergent treatment and Planova nanofiltration using 20 nanometer (nm) filters.
Flebogamma 10% DIF is a purified (≥ 97% IgG), unmodified, human IgG. The distribution of the four IgG subclasses is approximately 66.6% IgG1, 27.9% IgG2, 3.0% IgG3 and 2.5% IgG4. Flebogamma 10% DIF contains trace amounts of IgA (typically < 100 μg/mL) and trace amounts of sodium and IgM.
Flebogamma 10% DIF contains 10 g human normal immunoglobulin and 5 g D-sorbitol (as stabilizer) in 100 mL of water for injection, and ≤ 6 mg/mL polyethylene glycol. There is no preservative in the formulation. The pH of the solution ranges from 5 to 6 and the osmolality from 240 to 370 mOsm/kg, which is within the normal physiological range. The Fc and Fab functionality is maintained in Flebogamma 10% DIF.
All Source Plasma used in the manufacture of Flebogamma 10% DIF was collected only at FDA approved plasmapheresis centers in the United States and tested by FDA-licensed serological tests and found to be non-reactive (negative) for Hepatitis B Surface Antigen (HBsAg), antibodies to Hepatitis C Virus (HCV) and Human Immunodeficiency Virus (HIV) and negative on Nucleic Acid Test (NAT) for HCV and HIV. An investigational NAT for HBV is also performed on all Source Plasma and found to be negative; however, the significance of a negative result has not been established. Additionally, plasma is tested by in-process NAT testing for hepatitis A virus (HAV) and parvovirus B19 (B19) on minipools and the viral load limit for B19 in the manufacturing pool is set not to exceed 104 IU/ml. NAT testing for the presence of HCV and HIV in the manufacturing plasma pool is also performed and found to be negative.
In addition, several manufacturing steps can contribute towards viral safety of the final product. The effectiveness of these steps to remove or inactivate viruses from the product was evaluated through virus spiking experiments using a scaled down version of the manufacturing process. Virus elimination experiments have been performed on 7 steps of the production process.
Flebogamma 10% DIF production process includes the following specific virus inactivation/ removal steps:
- Pasteurization at 60 ºC, 10 hours
- Solvent-Detergent treatment for 6 hours
- Nanofiltration down to 20 nm Planova filters
The following purification processes can also reduce the risk of viral transmission:
- Fraction I precipitation
- Fraction II+III precipitation
- 4% PEG precipitation
- pH 4 treatment for 4 hours at 37 ºC
The viral reduction data (in log10) from these experiments are summarized in Table 4.
|
*When the RF is <1 log10, it is not taken into account for the calculation of the overall reduction capacity. |
||||||||
|
≥: No residual infectivity detected / nd: not done / na: non-applicable, since the virus is theoretically resistant to this treatment. |
||||||||
|
a) During the nanofiltration validation, 9 different viruses (HIV, PRV, BVDV, WNV, EMC, SV40, BEV, Echo 11 and PPV) were evaluated. Eight of these viruses were inactivated by the process conditions and/or removed by prefiltration. Only PPV was affected neither by the filtration conditions nor by the prefiltration and could be assayed and efficiently removed in these experiments. |
||||||||
|
Abbreviations: HIV; Human Immunodeficiency Virus, PRV; Pseudorabies Virus, IBR; Infectious Bovine Rhinotracheitis Virus, BVDV; Bovine Viral Diarrhoea Virus, SINDBIS; Sindbis Virus, WNV; West Nile Virus, EMC; Encephalomyocarditis Virus, PPV; Porcine Parvovirus. |
||||||||
| Target virus | HIV-1, HIV-2
(env. RNA) | HBV Herpesvirus
(env. DNA) | HCV
(env. RNA) | WNV
(env. RNA) | HAV
(non-env. RNA) | B19
Virus (non-env. DNA) |
||
| Model virus | HIV-1 | PRV | IBR | BVDV | SINDBIS | WNV | EMC | PPV |
| Fraction I precipitation | < 1.00* | nd | nd | nd | nd | 2.78 | nd | < 1.00* |
| Ethanol incubation (Fraction II+III) | 1.48 | nd | nd | nd | nd | < 1.00* | nd | nd |
| PEG precipitation | ≥ 6.10 | ≥ 5.92 | nd | ≥ 5.78 | nd | nd | ≥ 6.41 | 6.35 |
| Acid pH treatment | 2.47 | ≥ 5.32 | nd | < 1.00* | nd | nd | 1.36 | na |
| Pasteurization | ≥ 5.64 | ≥ 4.96 | ≥ 6.33 | ≥ 4.69 | ≥ 6.49 | ≥ 5.42 | ≥ 5.56 | 4.08 |
| Solvent Detergent | ≥ 4.61 | ≥ 6.95 | nd | ≥ 6.14 | nd | ≥ 5.59 | na | na |
| Nanofiltration
20 nanometer | a | a | a | a | a | a | a | 4.61 |
| Overall Reduction Capacity | ≥ 20.30 | ≥ 23.15 | ≥ 6.33 | ≥ 16.61 | ≥ 6.49 | ≥ 13.79 | ≥ 13.33 | 15.04 |
Additionally, the manufacturing process was investigated for its capacity to decrease infectivity of an experimental agent of transmissible spongiform encephalopathy (TSE), considered as a model for the vCJD and CJD agents.
Several individual production steps in the Flebogamma 10% DIF manufacturing process have been shown to decrease TSE infectivity of an experimental model agent. TSE reduction steps include: 4% Polyethylene glycol precipitation [≥ 6.19 log10] and Planova nanofiltration using a 20 nanometer filter [≥ 5.45 log10]. These studies provide reasonable assurance that low levels of CJD/vCJD agent infectivity, if present in the starting material, would be removed.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Flebogamma 10% DIF is a replacement therapy for PI. It supplies a broad spectrum of opsonizing and neutralizing antibodies against a wide variety of bacterial and viral agents. However, the mechanism of action in PI has not been fully elucidated.
12.3 Pharmacokinetics
In the clinical study assessing safety and efficacy in primary immunodeficiency disease (PI), the pharmacokinetics of Flebogamma 10% DIF was assessed for 21 or 28 days after administration in 19 subjects. PK analysis was performed for 10 subjects receiving Flebogamma 10% DIF on a 21-day schedule and for 9 subjects receiving treatment on a 28-day schedule. The mean dose (range) for those on the 21-day schedule was 476 mg/kg (range: 339-597), and it was 496 mg/kg (range: 434-588) for those on the 28-day schedule. Blood samples for PK analysis were obtained after Infusion 7 for subjects on a 28-day schedule and after Infusion 9 for subjects on a 21-day schedule. Table 5 summarizes the pharmacokinetic parameters of Flebogamma 10% DIF, measured as serum concentrations of total IgG.
|
a. This half-life is an apparent value derived from a period of measurement of 28 days |
||||
|
b. For subjects on the 3-week schedule, the average of the trough levels from Infusion 9 to the end of the study was calculated; for those on a 4-week schedule, the average of the trough levels from Infusion 7 to the end of the study was calculated. The means of the subject means are presented in this table. |
||||
| Variable | 3-Week Dosing Interval (n=10) | 4-Week Dosing Interval (n=9) | ||
| Mean ± SD | Range | Mean ± SD | Range | |
| Cmax (mg/dL) | 1,950 ± 283 | 1,510 – 2,440 | 2,092 ± 366 | 1,680 – 2,920 |
| AUC0 - last (day·mg/dL) | 33,951 ± 4,527 | 24,112 – 38,021 | 34,237 ± 3,972 | 27,683 – 40,825 |
| Clearance (mL/day) | 115 ± 31 | 81 – 186 | 144 ± 47 | 77 – 237 |
| Half-life (days)a | 34 ± 10 | 21 – 58 | 37 ± 13 | 24 – 59 |
| Trough IgG level (mg/dL)b | 976 ± 165 | 645 – 1,140 | 877 ± 126 | 759 – 1,170 |
The half-life of IgG can vary considerably among patients.
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenity, Mutagenesis, Impairment of Fertility
No animal studies were conducted to evaluate the carcinogenic or mutagenic effect of Flebogamma 10% DIF or its effects on fertility
13.2 Animal Toxicology and/or Pharmacology
Acute toxicity studies were performed in mice and rats at doses up to 2.5 g/kg body weight with infusion rates 6 to 37 times higher than the maximum rates recommended for humans. The most common clinical observations in mice studies were piloerection, ptosis, ataxia and increase in respiration all lasting 90 minutes or less. No relevant adverse effects could be confirmed affecting respiratory, circulatory, renal, autonomic and central nervous systems, somatomotor activity, and behavior of the treated mice and rats.
Five out of the 25 rats treated with the highest dose at approximately 8 times the maximum infusion rate recommended for humans, showed a transient “reddish urine” sign which was not confirmed as a relevant toxicity causing phenomenon after renal macro and microscopic analysis. This phenomenon was ascribed to hemolysis when serum was analyzed, suggesting a possible relation to cross-reactivity of rodent red cells with human antibodies. No “reddish urine” was detected in any mouse, a much smaller animal where the rate of infusion was comparatively much higher than in rats. The macroscopic inspection of all treated mice did not show any renal alteration.
14 CLINICAL STUDIES
A phase 3, multicenter, open-label, historically controlled study to assess the efficacy, safety and pharmacokinetics of Flebogamma 10% DIF in subjects with PI was conducted in the United States. Forty-six subjects were treated with Flebogamma 10% DIF for 12 months at a 3-week or 4-week dosing interval. Subjects ranged in age from 6 to 65 years; 65% were male and 35% were female; 96% were Caucasian and 4% were Hispanic.
The study included 46 subjects, 16 on a 3-week dosing interval and 30 on a 4-week dosing interval. Doses ranged from 307 mg/kg to 597 mg/kg. The median dose for the 3-week interval was 462.8 mg/kg; the median dose for the 4-week interval was 444 mg/kg. Subjects received a total of 601 infusions of Flebogamma 10% DIF. The maximum infusion rate allowed during the study was 0.08 mL/kg/min.
During the study period, the annual rate of acute serious bacterial infection, defined as bacterial pneumonia, bacteremia or sepsis, osteomyelitis/septic arthritis, visceral abscesses and bacterial meningitis per subject per year, was 0.025 (with an upper 1-sided 98% confidence interval of 0.001 to 0.133). One subject had one episode of bacterial pneumonia. There were no other episodes of serious bacterial infections (Table 6).
| Infections | Patients (N=46) N (%) | Episodes | Estimates [1] | 98% CI [2] | |
|---|---|---|---|---|---|
|
[1] Estimate = Total episodes/Total patient years. |
|||||
|
[2] The confidence interval is obtained by using a generalized linear model procedure for Poisson distribution |
|||||
| Bacterial pneumonia | 1 (2.2) | 1 | |||
| Bacteremia or sepsis | 0 (0.0) | 0 | |||
| Osteomyelitis/septic arthritis | 0 (0.0) | 0 | |||
| Visceral abscess | 0 (0.0) | 0 | |||
| Bacterial meningitis | 0 (0.0) | 0 | |||
| Patients with at least 1 serious bacterial infection | 1 (2.2) | 1 | 0.025 | (0.001, 0.133) | |
The other efficacy variables were the number of days of work/school missed, the number of hospitalizations and the number of days of each hospitalization, the number of visits to physicians or emergency rooms, the number of other infections documented by positive radiographic findings, fever, and the number of days of therapeutic and prophylactic oral and parenteral antibiotic use. These additional efficacy variables were annualized by using the subject-years exposure data only of those subjects experiencing the endpoints, not the entire study cohort. With regard to the number of other validated infections, the mean rate was less than 2 days/subject/year (The calculation uses all subjects, including those who had no infections, see Table 7).
|
[1] Days of work/school missed per patient year are derived as total days of work/school missed divided by total days in study multiplied by 365. If data are missing for a period (e.g., between Infusion 2 and Infusion 3), then number of days in this period is not counted in the denominator. All other endpoints are derived similarly. |
|||
|
Variable |
Subjects | Mean number of events, days or visits/subject/year
[1] |
|
| N | % | ||
| Work/school days missed | 20 | 43.5 | 3.0 |
| Days in hospital | 5 | 11.0 | 0.6 |
| Visits to physician/ER | 24 | 52.2 | 2.1 |
| Number of other documented infectious episodes | 7 | 15.2 | 0.2 |
| Days of therapeutic oral antibiotic use | 36 | 78.3 | 56.4 |
| Days of therapeutic parenteral antibiotic use | 2 | 4.3 | 1.3 |
| Days of other therapeutic antibiotic use | 14 | 30.4 | 60.5 |
| Days of prophylactic oral antibiotic use | 19 | 41.3 | 45.8 |
| Days of prophylactic parenteral antibiotic use | 1 | 2.2 | 0.02 |
| Days of other prophylactic antibiotic use | 1 | 2.2 | 3.3 |
15 REFERENCES
- Cayco AV, Perazella MA, Hayslett JP. Renal insufficiency after intravenous immune globulin therapy: a report of two cases and an analysis of the literature. J Am Soc Nephrol 1997; 8:1788-94.
- Tan E, Hajinazarian M, Bay W, et al. Acute renal failure resulting from intravenous immunoglobulin therapy. Arch Neurol 1993; 50:137-9.
- Sekul EA, Cupler EJ, Dalakas MC. Aseptic meningitis associated with high-dose intravenous immunoglobulin therapy: frequency and risk factors. Ann Intern Med 1994; 121:259-62.
- Scribner CL, Kapit RM, Phillips ET, et al. Aseptic meningitis and intravenous immunoglobulin therapy. Ann Intern Med 1994; 121:305-6.
- Thomas MJ, Misbah SA, Chapel HM, et al. Hemolysis after high-dose intravenous Ig. Blood 1993; 15:3789.
- Reinhart WH, Berchtold PE. Effect of high-dose intravenous immunoglobulin therapy on blood rheology. Lancet 1992; 339:662-4.
- Kessary-Shoham H, Levy Y, Shoenfeld Y, et al. In vivo administration of intravenous immunoglobulin (IVIG) can lead to enhanced erythrocyte sequestration. J Autoimmun 1999; 13:129-35.
- Dalakas MC. High-dose intravenous immunoglobulin and serum viscosity: risk of precipitating thromboembolic events. Neurology 1994; 44:223-6.
- Woodruff RK, Grigg AP, Firkin FC, et al. Fatal thrombotic events during treatment of autoimmune thrombocytopenia with intravenous immunoglobulin in elderly patients. Lancet 1986; ii:217-8.
- Wolberg AS, Kon RH, Monroe DM, et al. Coagulation factor XI is a contaminant in intravenous immunoglobulin preparations. Am J Hematol 2000; 65:30-4.
- Rizk A, Gorson KC, Kenney L, et al. Transfusion-related acute lung injury after the infusion of IVIG. Transfusion 2001; 41:264-8.
16 HOW SUPPLIED/STORAGE AND HANDLING
Flebogamma 10% DIF is supplied in single-use, individually laser etched vials containing the labeled amount of functionally active IgG.
The following presentations of Flebogamma 10% DIF are available:
| NDC Number | Fill Size | Grams Protein |
|---|---|---|
| 61953-0005-1 | 50 mL | 5 g |
| 61953-0005-2 | 100 mL | 10 g |
| 61953-0005-3 | 200 mL | 20 g |
Each vial has an integral suspension band and a label with two peel-off strips showing the product name and lot number.
DO NOT FREEZE.
When stored at room temperature (up to 25 ºC [77 ºF]), Flebogamma 10% DIF is stable for up to 24 months, as indicated by the expiration date printed on the outer carton and container label.
Keep Flebogamma 10% DIF in its original carton to protect it from light.
17 PATIENT COUNSELING INFORMATION
Inform patients to immediately report the following signs and symptoms to their physician:
- Decreased urine output, sudden weight gain, fluid retention/edema, and/or shortness of breath (see Warnings and Precautions [5.2])
- Acute chest pain, shortness of breath, leg pain, and swelling of the legs/feet (see Warnings and Precautions [5.4])
- Severe headache, neck stiffness, drowsiness, fever, sensitivity to light, painful eye movements, nausea and vomiting (see Warnings and Precautions [5.5])
- Increased heart rate, fatigue, yellowing of skin or eyes, dark-colored urine (see Warnings and Precautions [5.6])
- Trouble breathing, chest pain, blue lips or extremities, fever (see Warnings and Precautions [5.7])
Inform patients that Flebogamma 10% DIF is made from human plasma and may contain infectious agents that can cause disease (e.g., viruses, and, theoretically, the CJD agent). While the risk that Flebogamma 10% DIF may transmit an infection has been reduced by screening plasma donors for prior exposure, testing donated plasma, and inactivating and/or removing certain viruses during manufacturing, patients should report any symptoms that concern them (see Warnings and Precautions [5.8]).
Inform patients that Flebogamma 10% DIF can interfere with the response to live viral vaccines such as measles, mumps and rubella, and instruct patients to notify their healthcare professional of this potential interaction when they are receiving vaccinations (see Drug Interactions [7]).
Manufactured by:
INSTITUTO GRIFOLS, S.A.
BARCELONA – SPAIN
U.S. License No. 1181
U.S. Distributor
GRIFOLS BIOLOGICALS Inc.
LOS ANGELES - CA 90032, U.S.A.
U.S. License No. 1694
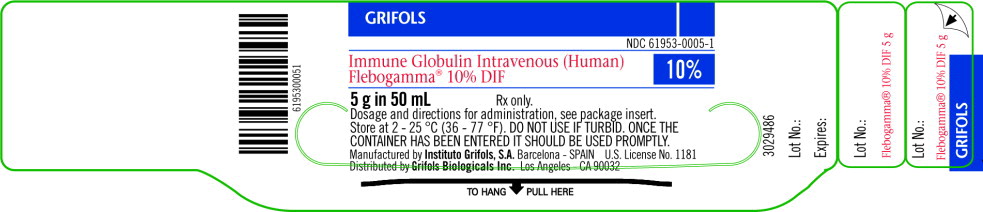
Principal Display Panel – 5g Vial Label
GRIFOLS
NDC 61953-0005-1
Immune Globulin Intravenous (Human)
Flebogamma® 10% DIF
10%
5 g in 50 mL Rx only.
Dosage and directions for administration, see package insert.
Store at 2 - 25 °C (36 - 77 °F). DO NOT USE IF TURBID. ONCE THE CONTAINER HAS BEEN ENTERED IT SHOULD BE USED PROMPTLY.
Manufactured by Instituto Grifols, S.A. Barcelona – SPAIN
U.S. License No. 1181
Distributed by Grifols Biologicals Inc. Los Angeles - CA 90032
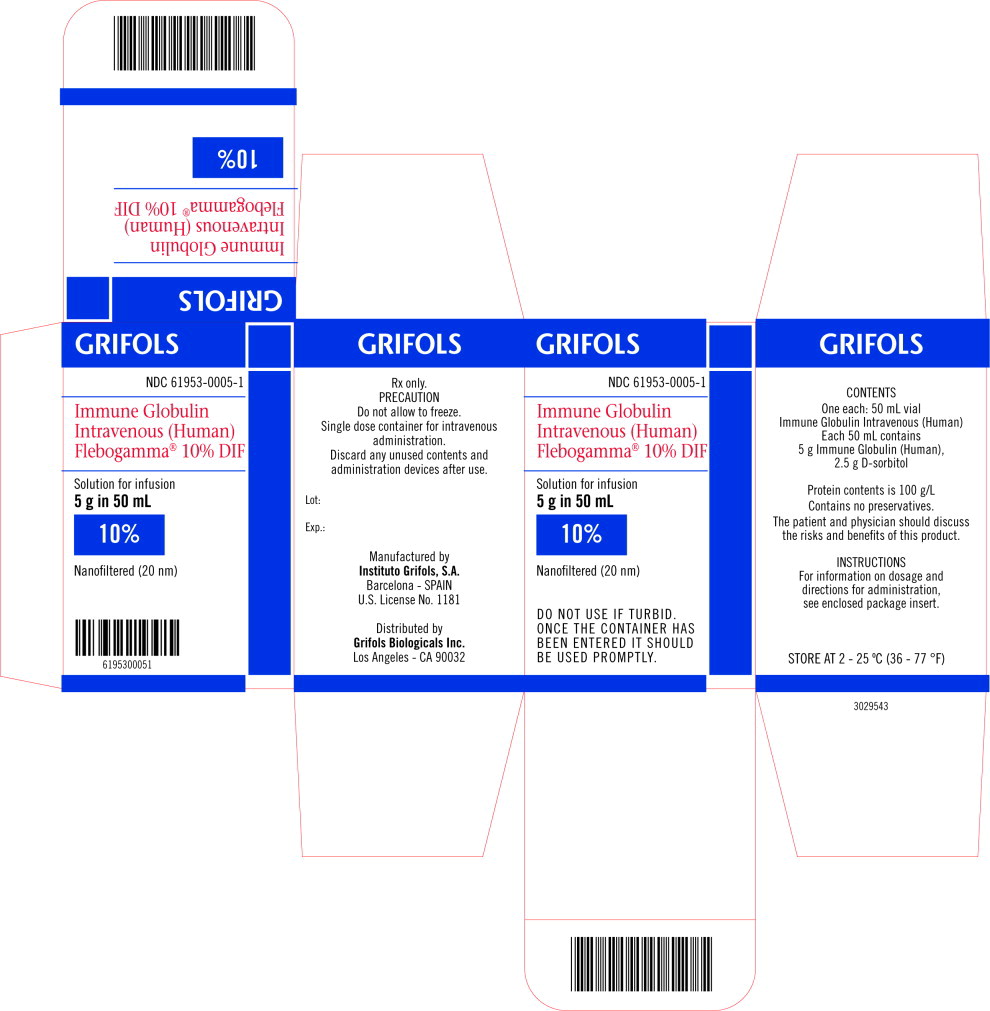
Principal Display Panel – 5g Carton Label
GRIFOLS
NDC 61953-0005-1
Immune Globulin Intravenous (Human)
Flebogamma® 10% DIF
Solution for infusion
5 g in 50 mL
10%
Nanofiltered (20 nm)
DO NOT USE IF TURBID.
ONCE THE CONTAINER HAS BEEN ENTERED IT SHOULD BE USED PROMPTLY.
| FLEBOGAMMA DIF
human immunoglobulin g injection, solution |
|||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||
| Marketing Information | |||
| Marketing Category | Application Number or Monograph Citation | Marketing Start Date | Marketing End Date |
| BLA | BLA125077 | 07/27/2010 | |
| Labeler - Instituto Grifols, S.A. (465562213) |
| Establishment | |||
| Name | Address | ID/FEI | Operations |
| Instituto Grifols, S.A. | 475610684 | MANUFACTURE | |