HEPARIN SODIUM AND SODIUM CHLORIDE
-
heparin sodium injection
Baxter Healthcare Corporation
----------
Heparin Sodium and 0.9% Sodium Chloride Injectionin Plastic Container
VIAFLEX Plus Container
DESCRIPTION
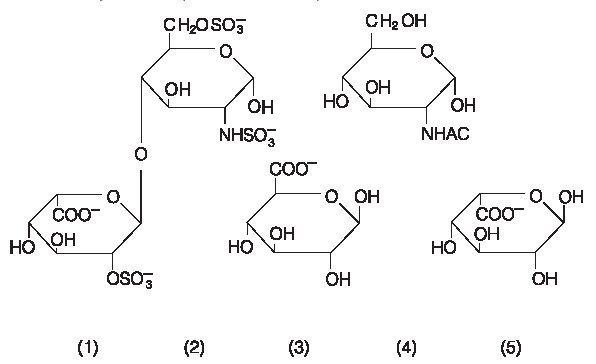
Heparin is a heterogenous group of straight-chain anionic mucopolysaccharides, called glycosaminoglycans having anticoagulant properties. Although others may be present, the main sugars occurring in heparin are: (1) α-L-iduronic acid 2-sulfate, (2) 2-deoxy-2-sulfamino-α-D-glucose 6-sulfate, (3) ß-D-glucuronic acid, (4) 2-acetamido-2-deoxy-α-D-glucose, and (5) α-L-iduronic acid. These sugars are present in decreasing amounts, usually in the order (2) > (1) > (4) > (3) > (5), and are joined by glycosidic linkages, forming polymers of varying sizes. Heparin is strongly acidic because of its content of covalently linked sulfate and carboxylic acid groups. In heparin sodium, the acidic protons of the sulfate units are partially replaced by sodium ions.
Structure of Heparin Sodium (representative subunits):
Heparin Sodium and 0.9% Sodium Chloride Injection is a buffered, sterile, nonpyrogenic solution of Heparin Sodium, USP derived from porcine intestinal mucosa, standardized for anticoagulant activity supplied in single dose containers for vascular administration. It contains no antimicrobial agents. The potency is determined by a biological assay using a USP reference standard based on units of heparin activity per milligram. Composition, osmolarity, pH and ionic concentration are shown in Table 1.
|
|||||||||||
| Size (mL) | Composition | *Osmolarity (mOsmol/L) (actual) | pH | Ionic Concentration (mEq/L) | |||||||
| Heparin Sodium, USP (units/mL) | Sodium Chloride, USP (NaCl) (g/L) | Dibasic Sodium Phosphate Heptahydrate, USP (Na2HPO4•7H2O) (g/L) | Citric Acid Hydrous, USP (C6H8O7•H2O) (g/L) | Sodium | Chloride | Phosphate (asHPO4=) | Citrate | ||||
| 1000 USP Heparin Units and 0.9% Sodium Chloride Injection | 500 | 2 | 9 | 4.34 | 0.4 | 322 | 7.0 (6.0to8.0) | 186 | 154 | 32 (16mmol/L) | 6 |
| 2000 USP Heparin Units and 0.9% Sodium Chloride Injection | 1000 | 2 | 9 | 4.34 | 0.4 | 322 | 7.0 (6.0to8.0) | 186 | 154 | 32 (16mmol/L) | 6 |
This VIAFLEX Plus plastic container is fabricated from a specially formulated polyvinyl chloride (PL 146 Plastic). VIAFLEX Plus on the container indicates the presence of a drug additive in a drug vehicle. The VIAFLEX Plus plastic container system utilizes the same container as the VIAFLEX plastic container system. The amount of water that can permeate from inside the container into the overwrap is insufficient to affect the solution significantly. Solutions in contact with the plastic container can leach out certain of its chemical components in very small amounts within the expiration period, e.g., di-2-ethylhexyl phthalate (DEHP), up to 5 parts per million. However, the safety of the plastic has been confirmed in tests in animals according to USP biological tests for plastic containers as well as by tissue culture toxicity studies.
CLINICAL PHARMACOLOGY
Heparin inhibits reactions that lead to the clotting of blood and the formation of fibrin clots both in vitro and in vivo. Heparin acts at multiple sites in the normal coagulation system. Small amounts of heparin in combination with antithrombin III (heparin cofactor) can inhibit thrombosis by inactivating activated Factor X and inhibiting the conversion of prothrombin to thrombin. Once active thrombosis has developed, larger amounts of heparin can inhibit further coagulation by inactivating thrombin and preventing the conversion of fibrinogen to fibrin. Heparin also prevents the formation of a stable fibrin clot by inhibiting the activation of the fibrin stabilizing factor.
Bleeding time is usually unaffected by heparin. Clotting time is prolonged by full therapeutic doses of heparin; in most cases, it is not measurably affected by low doses of heparin.
Patients over 60 years of age, following similar doses of heparin, may have higher plasma levels of heparin and longer activated partial thromboplastin times (APTTs) compared with patients under 60 years of age.
Heparin does not have fibrinolytic activity; therefore, it will not lyse existing clots.
INDICATIONS AND USAGE
Heparin Sodium and 0.9% Sodium Chloride Injection at a concentration of 2 units/mL is indicated as an aid in the maintenance of catheter patency.
CONTRAINDICATIONS
Heparin sodium should not be used in patients:
With severe thrombocytopenia;
In whom suitable blood coagulation tests - e.g., the whole-blood clotting time, partial thromboplastin time, etc. - cannot be performed at appropriate intervals (this contraindication refers to full-dose heparin; there is usually no need to monitor coagulation parameters in patients receiving low-dose heparin);
With an uncontrollable active bleeding state (see Warnings), except when this is due to disseminated intravascular coagulation.
WARNINGS
Hypersensitivity
Patients with documented hypersensitivity to heparin should be given the drug only in clearly life-threatening situations.
Hemorrhage
Hemorrhage can occur at virtually any site in patients receiving heparin. An unexplained fall in hematocrit, fall in blood pressure, or any other unexplained symptom should lead to serious consideration of hemorrhagic event.
Heparin sodium should be used with extreme caution in disease states in which there is increased danger of hemorrhage. Some of the conditions in which increased danger of hemorrhage exists are:
Cardiovascular - Subacute bacterial endocarditis. Severe hypertension.
Surgical - During and immediately following (a) spinal tap or spinal anesthesia or (b) major surgery, especially involving the brain, spinal cord, or eye.
Hematologic - Conditions associated with increased bleeding tendencies, such as hemophilia, thrombocytopenia, and some vascular purpuras.
Gastrointestinal - Ulcerative lesions and continuous tube drainage of the stomach or small intestine.
Other - Menstruation, liver disease with impaired hemostasis.
Coagulation Testing
When heparin sodium is administered in therapeutic amounts, its dosage should be regulated by frequent blood coagulation tests. If the coagulation test is unduly prolonged or if hemorrhage occurs, heparin sodium should be discontinued promptly (see Overdosage).
Thrombocytopenia
Thrombocytopenia has been reported to occur in patients receiving heparin with a reported incidence of up to 30%. Platelet counts should be obtained at baseline and periodically during heparin administration. Mild thrombocytopenia (count greater than 100,000/mm3) may remain stable or reverse even if heparin is continued. However, thrombocytopenia of any degree should be monitored closely. If the count falls below 100,000/mm3 or if recurrent thrombosis develops (see Heparin-induced Thrombocytopenia (HIT) With or Without Thrombosis), the heparin product should be discontinued and, if necessary, an alternative anticoagulant administered.
Heparin-induced Thrombocytopenia (HIT) (With or Without Thrombosis)
HIT is a serious immune-mediated reaction resulting from irreversible aggregation of platelets. HIT may progress to the development of venous and arterial thromboses, a condition referred to as HIT with thrombosis. Thrombotic events may also be the initial presentation for HIT. These serious thromboembolic events include deep vein thrombosis, pulmonary embolism, cerebral vein thrombosis, limb ischemia, stroke, myocardial infarction, mesenteric thrombosis, renal arterial thrombosis, skin necrosis, gangrene of the extremities that may lead to amputation, and fatal outcomes.
Once HIT (with or without thrombosis) is diagnosed or strongly suspected, all heparin sodium sources (including heparin flushes) should be discontinued and an alternative anticoagulant used. Future use of heparin sodium, especially within 3 to 6 months following the diagnosis of HIT (with or without thrombosis), and while patients test positive for HIT antibodies, should be avoided.
Immune-mediated HIT is diagnosed based on clinical findings supplemented by laboratory tests confirming the presence of antibodies to heparin sodium, or platelet activation induced by heparin sodium. A drop in platelet count greater than 50% from baseline is considered indicative of HIT. Platelet counts begin to fall 5 to 10 days after exposure to heparin sodium in heparin sodium–naïve individuals, and reach a threshold by days 7 to 14. In contrast, “rapid onset” HIT can occur very quickly (within 24 hours following heparin sodium initiation), especially in patients with a recent exposure to heparin sodium (i.e. previous 3 months). Thrombosis development shortly after documenting thrombocytopenia is a characteristic finding in almost half of all patients with HIT.
Thrombocytopenia of any degree should be monitored closely. If the platelet count falls below 100,000/mm3 or if recurrent thrombosis develops, the heparin product should be promptly discontinued and alternative anticoagulants considered if patients require continued anticoagulation.
Delayed Onset of HIT (With or Without Thrombosis)
Heparin-induced thrombocytopenia (with or without thrombosis) can occur up to several weeks after the discontinuation of heparin therapy. Patients presenting with thrombocytopenia or thrombosis after discontinuation of heparin sodium should be evaluated for HIT (with or without thrombosis).
Other
Solutions containing sodium ion should be used with great care in patients with congestive heart failure, severe renal insufficiency, and in clinical states in which there exists edema with sodium retention.
The intravenous administration of solutions can cause fluid and/or solute overloading resulting in dilution of serum electrolyte concentrations, overhydration, congested states or pulmonary edema. The risk of dilutional states is inversely proportional to the electrolyte concentrations of the injections. The risk of solute overload causing congested states with peripheral and pulmonary edema is directly proportional to the electrolyte concentrations of the injections.
Excessive administration of potassium free solutions may result in significant hypokalemia.
In patients with diminished renal function, administration may result in sodium retention.
PRECAUTIONS
General
Thrombocytopenia, Heparin-induced Thrombocytopenia (HIT) (With or Without Thrombosis) and Delayed Onset of HIT (With or Without Thrombosis).
See WARNINGS.
Heparin Resistance
Increased resistance to heparin is frequently encountered in fever, thrombosis, thrombophlebitis, infections with thrombosing tendencies, myocardial infarction, cancer and in postsurgical patients.
Increased Risk in Older Patients, Especially Women
A higher incidence of bleeding has been reported in patients, particularly women, over 60 years of age.
Solutions Containing Sodium
These solutions should be used with caution in patients receiving corticosteroids or corticotropin.
Laboratory Tests
Periodic platelet counts, hematocrits, and tests for occult blood in stool are recommended during the entire course of heparin therapy, regardless of the route of administration (see Dosage and Administration).
Drug Interactions
Oral anticoagulants: Heparin sodium may prolong the one-stage prothrombin time. Therefore, when heparin sodium is given with dicumarol or warfarin sodium, a period of at least 5 hours after the last intravenous dose or 24 hours after the last subcutaneous dose should elapse before blood is drawn if a valid prothrombin time is to be obtained.
Platelet inhibitors: Drugs such as acetylsalicylic acid, dextran, phenylbutazone, ibuprofen, indomethacin, dipyridamole, hydroxychloroquine and others that interfere with platelet-aggregation reactions (the main hemostatic defense of heparinized patients) may induce bleeding and should be used with caution in patients receiving heparin sodium.
Other interactions; Digitalis, tetracyclines, nicotine, or antihistamines may partially counteract the anticoagulant action of heparin sodium.
Drug/Laboratory Tests Interactions
Hyperaminotransferasemia
Significant elevations of aminotransferase (SGOT [S-AST] and SGPT [S-ALT]) levels have occurred in a high percentage of patients (and healthy subjects) who have received heparin. Since aminotransferase determinations are important in the differential diagnosis of myocardial infarction, liver disease, and pulmonary emboli, rises that might be caused by drugs (like heparin) should be interpreted with caution.
Carcinogenesis, Mutagenesis, Impairment of Fertility
No long-term studies in animals have been performed to evaluate carcinogenic potential of heparin. Also, no reproduction studies in animals have been performed concerning mutagenesis or impairment of fertility.
Pregnancy
Teratogenic Effects
Pregnancy Category C
Animal reproduction studies have not been conducted with heparin sodium. It is not known whether heparin sodium can cause fetal harm when administered to a pregnant woman or can affect reproduction capacity. Heparin sodium should be given to a pregnant woman only if clearly needed.
Nonteratogenic Effects: Heparin does not cross the placental barrier.
Nursing Mothers
Heparin is not excreted in human milk.
Pediatric Use
Safety and effectiveness in pediatric patients have not been established.
See Dosage and Administration.
Geriatric Use
A higher incidence of bleeding has been reported in patients over 60 years of age, especially women (see Precautions, General). Clinical studies indicate that lower doses of heparin may be indicated in these patients (see Precautions, General and Clinical Pharmacology).
Do not administer unless solution is clear and seal is intact.
ADVERSE REACTIONS
Hemorrhage
Hemorrhage is the chief complication that may result from heparin therapy (see Warnings). An overly prolonged clotting time or minor bleeding during therapy can usually be controlled by withdrawing the drug (see Overdosage). It should be appreciated that gastrointestinal or urinary tract bleeding during anticoagulant therapy may indicate the presence of an underlying occult lesion. Bleeding can occur at any site but certain specific hemorrhage complications may be difficult to detect:
Adrenal hemorrhage, with resultant acute adrenal insufficiency, has occurred during anticoagulant therapy. Therefore, such treatment should be discontinued in patients who develop signs and symptoms of acute adrenal hemorrhage and insufficiency. Initiation of corrective therapy should not depend on laboratory confirmation of the diagnosis, since any delay in an acute situation may result in the patient’s death.
Ovarian (corpus luteum) hemorrhage developed in a number of women of reproductive age receiving short or long-term anticoagulant therapy. This complication if unrecognized may be fatal.
Retroperitoneal hemorrhage.
Thrombocytopenia, Heparin-induced Thrombocytopenia (HIT) (With or Without Thrombosis) and Delayed Onset of HIT (With or Without Thrombosis).
See WARNINGS.
Local Irritation
Local irritation, erythema, mild pain, hematoma or ulceration may follow deep subcutaneous (intrafat) injection of heparin sodium. These complications are much more common after intramuscular use, and such use is not recommended.
Hypersensitivity
General hypersensitivity reactions have been reported, with chills, fever, and urticaria as the most usual manifestations, and asthma, rhinitis, lacrimation, headache, nausea and vomiting, and anaphylactoid reactions, including shock, occurring more rarely. Itching and burning, especially on the plantar site of the feet, may occur.
Thrombocytopenia has been reported to occur in patients receiving heparin with a reported incidence of up to 30%. While often mild and of no obvious clinical significance, such thrombocytopenia can be accompanied by severe thromboembolic complications such as skin necrosis, gangrene of the extremities that may lead to amputation, myocardial infarction, pulmonary embolism, stroke, and possibly death. (See Warnings, Precautions.)
Certain episodes of painful, ischemic, and cyanosed limbs have in the past been attributed to allergic vasospastic reactions. Whether these are in fact identical to the thrombocytopenia associated complications remains to be determined.
Miscellaneous
Osteoporosis following long-term administration of high-doses of heparin, cutaneous necrosis after systemic administration, suppression of aldosterone synthesis, delayed transient alopecia, priapism, and rebound hyperlipemia on discontinuation of heparin sodium have also been reported. Significant elevations of aminotransferase (SGOT [S-AST] and SGPT [S-ALT]) levels have occurred in a high percentage of patients (and healthy subjects) who have received heparin.
OVERDOSAGE
Symptoms
Bleeding is the chief sign of heparin overdosage. Nosebleeds, blood in urine or tarry stools may be noted as the first sign of bleeding. Easy bruising or petechial formations may precede frank bleeding.
Treatment
Neutralization of heparin effect.
When clinical circumstances (bleeding) require reversal of heparinization, protamine sulfate (1% solution) by slow infusion will neutralize heparin sodium. No more than 50 mg should be administered, very slowly in any 10 minute period. Each mg of protamine sulfate neutralizes approximately 100 USP heparin units. The amount of protamine required decreases over time as heparin is metabolized. Although the metabolism of heparin is complex, it may, for the purpose of choosing a protamine dose, be assumed to have a half-life of about 1/2 hour after intravenous injection.
Administration of protamine sulfate can cause severe hypotensive and anaphylactoid reactions. Because fatal reactions often resembling anaphylaxis have been reported, the drug should be given only when resuscitation techniques and treatment of anaphylactoid shock are readily available.
For additional information the labeling of Protamine Sulfate Injection, USP products should be consulted.
DOSAGE AND ADMINISTRATION
Heparin sodium is not effective by oral administration and Heparin Sodium and 0.9% Sodium Chloride Injection should not be given orally.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration whenever solution and container permit. Use of a final filter is recommended during administration of all parenteral solutions, where possible.
Maintenance of Catheter Patency
Although the rate for infusion of the 2 units/mL formulation is dependent upon age, weight, clinical condition of the patient and the procedure being employed, an infusion rate of 3 mL/hour has been found to be satisfactory.
Periodic platelet counts, hematocrits, and tests for occult blood in stool are recommended during the entire course of heparin therapy, regardless of the route of administration.
All injections in VIAFLEX Plus plastic containers are intended for administration using sterile equipment.
Because dosages of this drug are titrated to response, no additives should be made to Heparin Sodium and 0.9% Sodium Chloride Injection.
HOW SUPPLIED
Heparin Sodium and 0.9% Sodium Chloride Injection in VIAFLEX Plus plastic container is supplied as follows:
| Code | Size (mL) | NDC | Product Name |
| 2B0953 | 500 | 0338-0431-03 | 1000 USP Heparin Units and 0.9% Sodium Chloride Injection |
| 2B0944 | 1000 | 0338-0433-04 | 2000 USP Heparin Units and 0.9% Sodium Chloride Injection |
Exposure of pharmaceutical products to heat should be minimized. Avoid excessive heat. It is recommended the product be stored at room temperature (25°C); brief exposure up to 40°C does not adversely affect the product.
DIRECTION FOR USE OF VIAFLEX PLUS PLASTIC CONTAINER
Warning: Do not use plastic containers in series connections. Such use could result in air embolism due to residual air being drawn from the primary container before administration of the fluid from the secondary container is completed.
To Open
Tear overwrap down side at slit and remove solution container. Some opacity of the plastic due to moisture absorption during the sterilization process may be observed. This is normal and does not affect the solution quality or safety. The opacity will diminish gradually. Check for minute leaks by squeezing inner bag firmly. If leaks are found discard solution as sterility may be impaired. Do not add supplementary medication.
Preparation for Administration
- Suspend container from eyelet support.
- Remove plastic protector from outlet port at bottom of container.
- Attach administration set. Refer to complete directions accompanying set.
Baxter Healthcare Corporation
Deerfield, IL 60015 USA
Printed in USA
©Copyright 1981, 1982, 1983, 1989, 1995,
Baxter Healthcare Corporation. All rights reserved.
07-19-51-816
Rev. October 2009
PRINCIPAL DISPLAY PANEL - PACKAGE LABEL
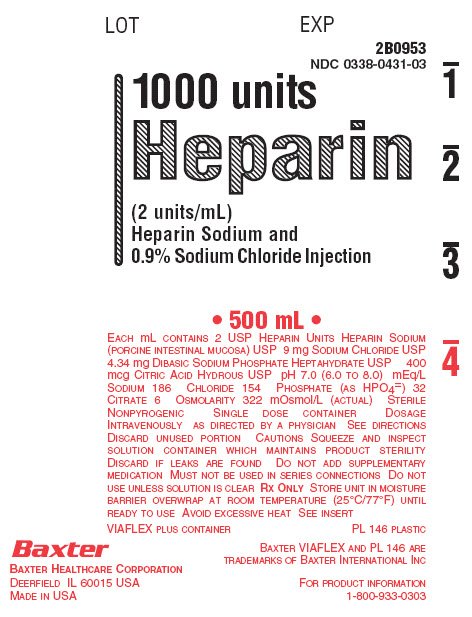
Container Label
LOT
EXP
2B0953
NDC 0338-0431-03
1000 units
Heparin
(2 units/mL)
Heparin Sodium and
0.9%Sodium Chloride Injection
• 500 mL •
EACH mL CONTAINS 2 USP HEPARIN UNITS HEPARIN SODIUM
(PORCINE INTESTINAL MUCOSA) USP 9 mg SODIUM CHLORIDE USP
4.34 mg DIBASIC SODIUM PHOSPHATE HEPTAHYDRATE USP 400
mcg CITRIC ACID HYDROUS USP pH 7.0 (6.0 TO 8.0) mEq/L
SODIUM 186 CHLORIDE 154 PHOSPHATE (AS HPO4=) 32
CITRATE 6 OSMOLARITY 322 mOsmol/L (ACTUAL) STERILE
NONPYROGENIC SINGLE DOSE CONTAINER DOSAGE
INTRAVENOUSLY AS DIRECTED BY A PHYSICIAN SEE DIRECTIONS
DISCARD UNUSED PORTION CAUTIONS SQUEEZE AND INSPECT
SOLUTION CONTAINER WHICH MAINTAINS PRODUCT STERILITY
DISCARD IF LEAKS ARE FOUND DO NOT ADD SUPPLEMENTARY
MEDICATION MUST NOT BE USED IN SERIES CONNECTIONS DO NOT
USE UNLESS SOLUTION IS CLEAR Rx ONLY STORE UNIT IN MOISTURE
BARRIER OVERWRAP AT ROOM TEMPERATURE (25°C/77°F) UNTIL
READY TO USE AVOID EXCESSIVE HEAT SEE INSERT
VIAFLEX PLUS CONTAINER
PL 146 PLASTIC
BAXTER VIAFLEX AND PL 146 ARE
TRADEMARKS OF BAXTER INTERNATIONAL INC
FOR PRODUCT INFORMATION
1-800-933-0303
Baxter
BAXTER HEALTHCARE CORPORATION
DEERFIELD IL 60015 USA
MADE IN USA
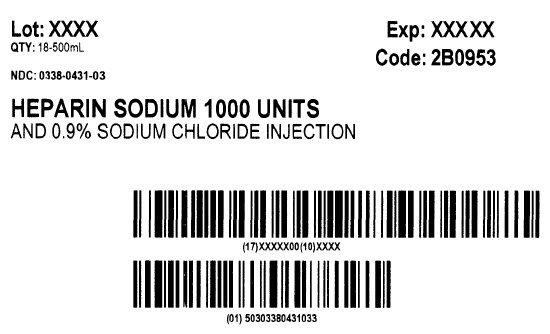
Carton Label
Lot: XXXX
QTY: 18-500mL
Exp: XXXX
Code: 2B0953
NDC: 0338-0431-03
HEPARIN SODIUM 1000 UNITS
AND 0.9% SODIUM CHLORIDE INJECTION
(17)XXXXX00(10)XXXX
(01)50303380431033
| HEPARIN SODIUM AND SODIUM CHLORIDE
heparin sodium injection |
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
| Marketing Information | |||
| Marketing Category | Application Number or Monograph Citation | Marketing Start Date | Marketing End Date |
| NDA | NDA018609 | 06/18/2010 | |
| HEPARIN SODIUM AND SODIUM CHLORIDE
heparin sodium injection |
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
| Marketing Information | |||
| Marketing Category | Application Number or Monograph Citation | Marketing Start Date | Marketing End Date |
| NDA | NDA018609 | 06/18/2010 | |
| Labeler - Baxter Healthcare Corporation (005083209) |
| Establishment | |||
| Name | Address | ID/FEI | Operations |
| Baxter Healthcare SA dba Baxter Healthcare of Puerto Rico | 189326168 | MANUFACTURE | |
| Establishment | |||
| Name | Address | ID/FEI | Operations |
| Baxter Healthcare Corporation | 059140764 | MANUFACTURE | |