ADACEL TDAP
-
clostridium tetani toxoid antigen (formaldehyde inactivated),
corynebacterium diphtheriae toxoid antigen (formaldehyde inactivated),
bordetella pertussis toxoid antigen (glutaraldehyde inactivated),
bordetella pertussis filamentous hemagglutinin antigen (formaldehyde inactivated),
bordetella pertussis pertactin antigen and
bordetella pertussis fimbriae 2/3 antigen injection, suspension
Sanofi Pasteur Limited
----------
Tetanus Toxoid, ReducedDiphtheria Toxoid and Acellular
Pertussis Vaccine Adsorbed
Adacel®
Tdap
Rx only
DESCRIPTION
Adacel®, Tetanus Toxoid, Reduced Diphtheria Toxoid and Acellular Pertussis Vaccine Adsorbed (Tdap), is a sterile liquid suspension of tetanus and diphtheria toxoids and acellular pertussis components adsorbed onto aluminum phosphate, for intramuscular administration. After shaking, the vaccine is a white, homogenous, cloudy suspension.
Each dose of Adacel vaccine (0.5 mL) contains the following active ingredients:
| Acellular Pertussis | |
| Detoxified Pertussis Toxin (PT) | 2.5 µg |
| Filamentous Hemagglutinin (FHA) | 5 µg |
| Pertactin (PRN) | 3 µg |
| Fimbriae Types 2 and 3 (FIM) | 5 µg |
| Tetanus Toxoid (T) | 5 Lf |
| Diphtheria Toxoid (d) | 2 Lf |
Other ingredients per dose include 1.5 mg aluminum phosphate (0.33 mg aluminum) as the adjuvant, ≤5 µg residual formaldehyde, <50 ng residual glutaraldehyde and 3.3 mg (0.6% v/v) 2-phenoxyethanol (not as a preservative). The antigens are the same as those in DAPTACEL®, Diphtheria and Tetanus Toxoids and Acellular Pertussis Vaccine Adsorbed (DTaP); however, Adacel vaccine is formulated with reduced quantities of d and detoxified PT.
The acellular pertussis vaccine components are obtained from Bordetella pertussis cultures grown in Stainer-Scholte medium (1) modified by the addition of casamino acids and dimethyl-beta-cyclodextrin. PT, FHA and PRN are isolated separately from the supernatant culture medium. FIM are extracted and co-purified from the bacterial cells. The pertussis antigens are purified by sequential filtration, salt-precipitation, ultrafiltration and chromatography. PT is detoxified with glutaraldehyde, FHA is treated with formaldehyde, and the residual aldehydes are removed by ultrafiltration. The individual antigens are adsorbed onto aluminum phosphate.
Corynebacterium diphtheriae is grown in modified Mueller's growth medium. (2) After purification by ammonium sulfate fractionation, diphtheria toxin is detoxified with formaldehyde and diafiltered. Clostridium tetani is grown in modified Mueller-Miller casamino acid medium without beef heart infusion. (3) Tetanus toxin is detoxified with formaldehyde and purified by ammonium sulfate fractionation and diafiltration. Diphtheria and tetanus toxoids are individually adsorbed onto aluminum phosphate.
The adsorbed diphtheria, tetanus and acellular pertussis components are combined with aluminum phosphate (as adjuvant), 2-phenoxyethanol (not as a preservative) and water for injection.
Tetanus and diphtheria toxoid potency is determined by measuring the amount of neutralizing antitoxin in previously immunized guinea pigs. The tetanus component induces at least 2 neutralizing units/mL of serum and the diphtheria component induces at least 0.5 neutralizing units/mL of serum. The potency of the acellular pertussis vaccine components is evaluated by the antibody response of immunized mice to detoxified PT, FHA, PRN and FIM as measured by enzyme-linked immunosorbent assay (ELISA).
CLINICAL PHARMACOLOGY
Background
Tetanus
Tetanus is an acute and often fatal disease caused by an extremely potent neurotoxin produced by C tetani. The toxin causes neuromuscular dysfunction, with rigidity and spasms of skeletal muscles. The muscle spasms usually involve the jaw (lockjaw) and neck and then become generalized.
Spores of C tetani are ubiquitous. Serological tests indicate that naturally acquired immunity to tetanus toxin does not occur in the US. Thus, universal primary immunization, with subsequent maintenance of adequate antitoxin levels by means of appropriately timed boosters, is necessary to protect all age groups. Following immunization, protection generally persists for at least 10 years. (4)
Diphtheria
C diphtheriae may cause both localized and generalized disease. The systemic intoxication is caused by diphtheria exotoxin, an extracellular protein metabolite of toxigenic strains of C diphtheriae. Both toxigenic and nontoxigenic strains of C diphtheriae can cause disease, but only strains that produce toxin can cause severe manifestations such as myocarditis and neuritis. Toxigenic strains are more often associated with severe or fatal respiratory infections than with cutaneous infections.
Complete immunization significantly reduces the risk of developing diphtheria and immunized persons who develop disease have milder illness.
Immunization with diphtheria toxoid does not, however, eliminate carriage of C diphtheriae in the pharynx, nose, or on the skin. Following immunization, protection lasts at least 10 years. (4)
Pertussis
Pertussis (whooping cough) is a disease of the respiratory tract, most often caused by B pertussis. This gram-negative coccobacillus produces a variety of biologically active components, though their role in pathogenesis is not clearly defined.
Mechanism of Action
Protection against disease attributable to C tetani is due to the development of neutralizing antiboides to tetanus toxin. A serum antitoxin level of ≥0.1 IU/mL is considered protective, although a level of at least 0.01 IU/mL, measured by neutralization assay is considered the minimum protective level. (5) Protection against disease attributable to C diphtheriae is due to the development of neutralizing antibodies to diphtheria toxin. A serum antitoxin level of 0.01 IU/mL is the lowest level giving some degree of protection. Antitoxin levels of at least 0.1 IU/mL are generally regarded as protective. (6) Levels of 1.0 IU/mL have been associated with long-term protection. (7)
The mechanism of protection from B pertussis disease is not well understood. However, the pertussis components in Adacel vaccine (i.e., detoxified PT, FHA, PRN and FIM) have been shown to prevent pertussis in infants in a clinical trial with DAPTACEL vaccine. (See Clinical Studies.)
Clinical Studies
The efficacy of the tetanus toxoid and diphtheria toxoid used in Adacel vaccine was based on the immune response to these antigens compared to a US licensed Tetanus and Diphtheria Toxoids Adsorbed For Adult Use (Td) vaccine manufactured by Sanofi Pasteur Inc., Swiftwater, PA. The primary measures of immunogenicity were (a) the percentage of participants attaining an antibody level of at least 0.1 IU/mL and (b) the percentage of participants achieving a rise in antibody concentration after vaccination (booster response). The demonstration of a booster response depended on the antibody concentration to each antigen prior to immunization. Threshold or "cut-off" values for antibody concentrations to each antigen were established based on the 95th percentile of the pre-vaccination antibody concentrations observed in previous clinical trials. A booster response was defined as a four-fold rise in antibody concentration if the pre-vaccination concentration was equal to or below the cut-off value and a two-fold rise in antibody concentration if the pre-vaccination concentration was above the cut-off value.
The efficacy of the pertussis antigens used in Adacel vaccine was inferred based on a comparison of pertussis antibody levels achieved in recipients of a single booster dose of Adacel vaccine with those obtained in infants after three doses of DAPTACEL vaccine. In the Sweden I Efficacy Trial, three doses of DAPTACEL vaccine were shown to confer a protective efficacy of 84.9% (95% CI: 80.1%, 88.6%) against WHO defined pertussis (21 days of paroxysmal cough with laboratory-confirmed B pertussis infection or epidemiological link to a confirmed case). The protective efficacy against mild pertussis (defined as at least one day of cough with laboratory-confirmed B pertussis infection) was 77.9% (95% CI: 72.6%, 82.2%). (8) (9) In addition, the ability of Adacel vaccine to elicit a booster response to the pertussis antigens following vaccination was evaluated. The acellular pertussis formulations for Adacel and DAPTACEL vaccines differ only in the amount of detoxified PT (2.5 µg in Adacel vaccine versus 10 µg in DAPTACEL vaccine).
The principal immunogenicity study was a comparative, multi-center, randomized, observer-blind, controlled trial which enrolled 4,480 participants; 2,053 adolescents (11-17 years of age) and 2,427 adults (18-64 years of age). Enrollment was stratified by age to ensure adequate representation across the entire age range. Participants had not received a tetanus or diphtheria toxoid containing vaccine within the previous 5 years. After enrollment participants were randomized to receive one dose of either Adacel vaccine or Td vaccine. A total of 4,461 randomized participants were vaccinated. The per-protocol immunogenicity subset included 1,270 Adacel vaccine recipients and 1,026 Td vaccine recipients. Sera were obtained before and approximately 35 days after vaccination. (Blinding procedures for safety assessments are described in the ADVERSE REACTIONS section.)
Demographic characteristics were similar within age groups and between the vaccine groups. A total of 76% of the adolescents and 1.1% of the adults reported a history of receiving 5 previous doses of diphtheria-tetanus-pertussis containing vaccines. Anti-tetanus and anti-diphtheria seroprotection rates (≥0.1 IU/mL) and booster response rates were comparable between Adacel and Td vaccines. (See Table 1 and Table 2.) Adacel vaccine induced pertussis antibody levels that were non-inferior to those of Swedish infants who received three doses of DAPTACEL vaccine. (See Table 3.) Acceptable booster responses to each of the pertussis antigens were also demonstrated, i.e., the percentage of participants with a booster response exceeded the pre-defined lower limit. (9) (See Table 4.)
| Tetanus Antitoxin (IU/mL) | |||||||
|---|---|---|---|---|---|---|---|
| Pre-Vaccination | 1 Month Post-Vaccination | ||||||
| Age Group (years) | Vaccine | N* | % ≥0.10 (95% CI) | % ≥1.0 (95% CI) | % ≥0.10 (95% CI) | % ≥1.0 (95% CI) | % Booster†
(95% CI) |
|
|||||||
| 11-17 | Adacel | 527 | 99.6 (98.6, 100.0) | 44.6 (40.3, 49.0) | 100.0‡
(99.3, 100.0) | 99.6§
(98.6, 100.0) | 91.7‡
(89.0, 93.9) |
| Td¶ | 516 | 99.2 (98.0, 99.8) | 43.8 (39.5, 48.2) | 100.0 (99.3, 100.0) | 99.4 (98.3, 99.9) | 91.3 (88.5, 93.6) |
|
| 18-64 | Adacel | 742- 743 | 97.3 (95.9, 98.3) | 72.9 (69.6, 76.1) | 100.0‡
(99.5, 100.0) | 97.8§
(96.5, 98.8) | 63.1‡
(59.5, 66.6) |
| Td¶ | 509 | 95.9 (93.8, 97.4) | 70.3 (66.2, 74.3) | 99.8 (98.9, 100.0) | 98.2 (96.7, 99.2) | 66.8 (62.5, 70.9) |
|
| Diphtheria Antitoxin (IU/mL) | |||||||
|---|---|---|---|---|---|---|---|
| Pre-Vaccination | 1 Month Post-Vaccination | ||||||
| Age Group (years) | Vaccine | N* | % ≥0.10 (95% CI) | % ≥1.0 (95% CI) | % ≥0.10 (95% CI) | % ≥1.0 (95% CI) | % Booster†
(95% CI) |
|
|||||||
| 11-17 | Adacel | 527 | 72.5 (68.5, 76.3) | 15.7 (12.7, 19.1) | 99.8‡
(98.9, 100.0) | 98.7§
(97.3, 99.5) | 95.1‡
(92.9, 96.8) |
| Td¶ | 515- 516 | 70.7 (66.5, 74.6) | 17.3 (14.1, 20.8) | 99.8 (98.9, 100.0) | 98.4 (97.0, 99.3) | 95.0 (92.7, 96.7) |
|
| 18-64 | Adacel | 739- 741 | 62.6 (59.0, 66.1) | 14.3 (11.9, 17.0) | 94.1‡
(92.1, 95.7) | 78.0§
(74.8, 80.9) | 87.4‡
(84.8, 89.7) |
| Td¶ | 506- 507 | 63.3 (59.0, 67.5) | 16.0 (12.9, 19.5) | 95.1 (92.8, 96.8) | 79.9 (76.1, 83.3) | 83.4 (79.9, 86.5) |
|
| Adolescents | Adults | |
|---|---|---|
| Adacel†/DAPTACEL‡
GMC Ratio (95% CIs) | Adacel§/DAPTACEL‡
GMC Ratio (95% CIs) |
|
|
||
| Anti-PT | 3.6 (2.8, 4.5)¶ | 2.1 (1.6, 2.7)¶ |
| Anti-FHA | 5.4 (4.5, 6.5)¶ | 4.8 (3.9, 5.9)¶ |
| Anti-PRN | 3.2 (2.5, 4.1)¶ | 3.2 (2.3, 4.4)¶ |
| Anti-FIM | 5.3 (3.9, 7.1)¶ | 2.5 (1.8, 3.5)¶ |
| Adolescents | Adults | Pre-defined Acceptable Rates* %† |
|||
|---|---|---|---|---|---|
| N‡ | % (95% CI) | N‡ | % (95% CI) | ||
|
|||||
| Anti-PT | 524 | 92.0 (89.3, 94.2) | 739 | 84.4 (81.6, 87.0) | 81.2 |
| Anti-FHA | 526 | 85.6 (82.3, 88.4) | 739 | 82.7 (79.8, 85.3) | 77.6 |
| Anti-PRN | 525 | 94.5 (92.2, 96.3) | 739 | 93.8 (91.8, 95.4) | 86.4 |
| Anti-FIM | 526 | 94.9 (92.6, 96.6) | 739 | 85.9 (83.2, 88.4) | 82.4 |
CONCURRENTLY ADMINISTERED VACCINES
Hepatitis B Vaccine
The concomitant use of Adacel vaccine and hepatitis B (Hep B) vaccine (Recombivax HB®, 10 μg per dose using a two-dose regimen, manufactured by Merck and Co., Inc) was evaluated in a multi-center, open-labeled, randomized, controlled study that enrolled 410 adolescents, 11-14 years of age inclusive. One group received Adacel and Hep B vaccines concurrently (N = 206). The other group (N = 204) received Adacel vaccine at the first visit, then 4-6 weeks later received Hep B vaccine. The second dose of Hep B vaccine was given 4-6 weeks after the first dose. Serum samples were obtained prior to and 4-6 weeks after Adacel vaccine administration, as well as 4-6 weeks after the 2nd dose of Hep B for all participants. No interference was observed in the immune responses to any of the vaccine antigens when Adacel and Hep B vaccines were given concurrently or separately. (9) (See DOSAGE AND ADMINISTRATION, Concomitant Vaccine Administration.)
Trivalent Inactivated Influenza Vaccine
The concomitant use of Adacel vaccine and trivalent inactivated influenza vaccine (TIV, Fluzone®, manufactured by Sanofi Pasteur Inc., Swiftwater, PA) was evaluated in a multi-center, open-labeled, randomized, controlled study conducted in 720 adults, 19-64 years of age inclusive. In one group, participants received Adacel and TIV vaccines concurrently (N = 359). The other group received TIV at the first visit, then 4-6 weeks later received Adacel vaccine (N = 361). Sera were obtained prior to and 4-6 weeks after Adacel vaccine, as well as 4-6 weeks after the TIV. The immune responses were comparable for concurrent and separate administration of Adacel and TIV vaccines for diphtheria (percent of participants with seroprotective concentration ≥0.10 IU/mL and booster responses), tetanus (percent of participants with seroprotective concentration ≥0.10 IU/mL), pertussis antigens (booster responses and GMCs except lower PRN GMC in the concomitant group, lower bound of the 90% CI was 0.61 and the pre-specified criterion was ≥0.67) and influenza antigens (percent of participants with hemagglutination-inhibition [HI] antibody titer ≥1:40 IU/mL and ≥4-fold rise in HI titer). Although tetanus booster response rates were significantly lower in the group receiving the vaccines concurrently versus separately, greater than 98% of participants in both groups achieved seroprotective levels of ≥0.1 IU/mL. (9) (See DOSAGE AND ADMINISTRATION, Concomitant Vaccine Administration.)
INDICATIONS AND USAGE
Adacel vaccine is indicated for active booster immunization for the prevention of tetanus, diphtheria and pertussis as a single dose in persons 11 through 64 years of age.
The use of Adacel vaccine as a primary series, or to complete the primary series, has not been studied.
Vaccination with Adacel vaccine may not protect all of vaccinated individuals.
CONTRAINDICATIONS
A severe allergic reaction (e.g., anaphylaxis) after a previous dose of Adacel vaccine or any other tetanus toxoid, diphtheria toxoid or pertussis containing vaccine or any other component of this vaccine is a contraindication to vaccination with Adacel vaccine. Because of uncertainty as to which component of the vaccine may be responsible, none of the components should be administered. Alternatively, such individuals may be referred to an allergist for evaluation if further immunizations are to be considered. (10) (11)
Encephalopathy within 7 days of a previous dose of a pertussis containing vaccine not attributable to another identifiable cause is a contraindication to vaccination with Adacel vaccine.(5) (10) (11)
WARNINGS
Persons who experienced Arthus-type hypersensitivity reactions (e.g., severe local reactions associated with systemic symptoms) (12) following a prior dose of tetanus toxoid usually have high serum tetanus antitoxin levels and should not be given emergency doses of tetanus toxoid containing vaccines more frequently than every 10 years, even if the wound is neither clean nor minor. (4) (10) (11) (13)
If Guillain-Barré syndrome occurred within 6 weeks of receipt of prior vaccine containing tetanus toxoid, the decision to give Adacel vaccine or any vaccine containing tetanus toxoid should be based on careful consideration of the potential benefits and possible risks. (5) (10) (11)
In the following situations, Adacel vaccine should generally be deferred:
- Moderate or severe acute illness with or without fever, until the acute illness resolves. (10) (11)
- In adolescents, progressive neurologic disorder, including progressive encephalopathy, or uncontrolled epilepsy, until the condition has stabilized. (11)
- In adults, unstable neurologic condition (e.g., cerebrovascular events and acute encephalopathic conditions), until the condition has resolved or is stabilized. (10)
PRECAUTIONS
General
Before administration of Adacel vaccine, the patient's current health status and medical history should be reviewed in order to determine whether any contraindications exist and to assess the benefits and risks of vaccination. (See CONTRAINDICATIONS and WARNINGS.)
Epinephrine Hydrochloride Solution (1:1,000) and other appropriate agents and equipment should be available for immediate use in case an anaphylactic or acute hypersensitivity reaction occurs.
If Adacel vaccine is administered to immunocompromised persons, including persons receiving immunosupressive therapy, the expected immune response may not be obtained.
Information for Vaccine Recipients and/or Parent or Guardian
Before administration of Adacel vaccine, health-care providers should inform the vaccine recipient and/or parent or guardian of the benefits and risks.
The health-care provider should inform the vaccine recipient and/or parent or guardian about the potential for adverse reactions that have been temporally associated with Adacel vaccine or other vaccines containing similar components. The health-care provider should provide the Vaccine Information Statements (VISs) that are required by the National Childhood Vaccine Injury Act of 1986 to be given with each immunization.
The vaccine recipient and/or parent or guardian should be instructed to report any serious adverse reactions to their health-care provider. Females of child-bearing potential should be informed that Sanofi Pasteur Inc. maintains a pregnancy surveillance system to collect data on pregnancy outcomes and newborn health status outcomes following vaccination with Adacel vaccine during pregnancy. If they are pregnant or become aware they were pregnant at the time of Adacel vaccine immunization, they are encouraged to contact directly or have their health-care professional contact Sanofi Pasteur Inc. at 1-800-822-2463 (1-800-VACCINE).
Reporting adverse events after vaccination to VAERS (Vaccine Adverse Event Reporting System) by recipients and/or parents/or guardian should be encouraged. The toll-free number for VAERS forms and information is 1-800-822-7967. Reporting forms may also be obtained at the VAERS website at www.vaers.hhs.gov
Drug Interactions
Immunosuppressive therapies, including irradiation, antimetabolites, alkylating agents, cytotoxic drugs and corticosteroids (used in greater than physiologic doses), may reduce the immune response to vaccines. (See PRECAUTIONS, General.)
For information regarding simultaneous administration with other vaccines refer to the CLINICAL PHARMACOLOGY, CONCURRENTLY ADMINISTERED VACCINES, ADVERSE REACTIONS and DOSAGE AND ADMINISTRATION sections.
Carcinogenesis, Mutagenesis, Impairment of Fertility
No studies have been performed with Adacel vaccine to evaluate carcinogenicity, mutagenic potential, or impairment of fertility.
Pregnancy Category C
Animal reproduction studies have not been conducted with Adacel vaccine. It is also not known whether Adacel vaccine can cause fetal harm when administered to a pregnant woman or can affect reproduction capacity. Adacel vaccine should be given to a pregnant woman only if clearly needed. Animal fertility studies have not been conducted with Adacel vaccine. The effect of Adacel vaccine on embryo-fetal and pre-weaning development was evaluated in two developmental toxicity studies using pregnant rabbits. Animals were administered Adacel vaccine twice prior to gestation, during the period of organogenesis (gestation day 6) and later during pregnancy on gestation day 29, 0.5 mL/rabbit/occasion (a 17-fold increase compared to the human dose of Adacel vaccine on a body weight basis), by intramuscular injection. No adverse effects on pregnancy, parturition, lactation, embryo-fetal or pre-weaning development were observed. There were no vaccine related fetal malformations or other evidence of teratogenesis noted in this study. (9)
Nursing Mothers
It is not known whether Adacel vaccine is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when Adacel vaccine is given to a nursing woman.
Pediatric Use
Adacel vaccine is not indicated for individuals less than 11 years of age. (See INDICATIONS AND USAGE.) For immunization of persons 6 weeks through 6 years of age against diphtheria, tetanus and pertussis refer to manufacturers' package inserts for DTaP vaccines.
Geriatric Use
Adacel vaccine is not indicated for individuals 65 years of age and older. No data are available regarding the safety and effectiveness of Adacel vaccine in individuals 65 years of age and older as clinical studies of Adacel vaccine did not include participants in the geriatric population.
ADVERSE REACTIONS
The safety of Adacel vaccine was evaluated in 4 clinical studies. A total of 5,841 individuals 11-64 years of age inclusive (3,393 adolescents 11-17 years of age and 2,448 adults 18-64 years) received a single dose of Adacel vaccine.
The principal safety study was a randomized, observer-blind, active controlled trial that enrolled participants 11-17 years of age (Adacel vaccine N = 1,184; Td vaccine N = 792) and 18-64 years of age (Adacel vaccine N = 1,752; Td vaccine N = 573). Study participants had not received tetanus or diphtheria containing vaccines within the previous 5 years. Solicited local and systemic reactions and unsolicited adverse events were monitored daily for 14 days post-vaccination using a diary card. From days 14-28 post-vaccination, information on adverse events necessitating a medical contact, such as a telephone call, visit to an emergency room, physician's office or hospitalization, was obtained via telephone interview or at an interim clinic visit. From days 28 to 6 months post-vaccination, participants were monitored for unexpected visits to a physician's office or to an emergency room, onset of serious illness and hospitalizations. Information regarding adverse events that occurred in the 6 month post-vaccination time period was obtained from the participant via telephone. Approximately 96% of participants completed the 6-month follow-up evaluation.
In the concomitant vaccination study with Adacel and Hepatitis B vaccines (see Clinical Studies for description of study design and number of participants), local and systemic adverse events were monitored daily for 14 days post-vaccination using a diary card. Local adverse events were only monitored at site/arm of Adacel vaccine administration. Unsolicited reactions (including immediate reactions, serious adverse events and events that elicited seeking medical attention) were collected at a clinic visit or via telephone interview for the duration of the trial, i.e., up to six months post-vaccination.
In the concomitant vaccination study with Adacel vaccine and trivalent inactivated influenza vaccine (see Clinical Studies for description of study design and number of participants), local and systemic adverse events were monitored for 14 days post-vaccination using a diary card. All unsolicited reactions occurring through day 14 were collected. From day 14 to the end of the trial, i.e., up to 84 days, only events that elicited seeking medical attention were collected.
In all the studies, participants were monitored for serious adverse events throughout the duration of the study.
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a vaccine cannot be directly compared to rates in the clinical trials of another vaccine and may not reflect the rates observed in practice. The adverse reaction information from clinical trials does, however, provide a basis for identifying the adverse events that appear to be related to vaccine use and for approximating rates of those events.
Serious Adverse Events in All Safety Studies
Throughout the 6-month follow-up period in the principal safety study, serious adverse events were reported in 1.5% of Adacel vaccine recipients and 1.4% in Td vaccine recipients. Two serious adverse events in adults were neuropathic events that occurred within 28 days of Adacel vaccine administration; one severe migraine with unilateral facial paralysis and one diagnosis of nerve compression in neck and left arm. Similar or lower rates of serious adverse events were reported in the other trials and there were no additional neuropathic events reported.
Solicited Adverse Events in the Principal Safety Study
The frequency of selected solicited adverse events (erythema, swelling, pain and fever) occurring during Days 0-14 following one dose of Adacel vaccine or Td vaccine are presented in Table 5. Most of these events were reported at a similar frequency in recipients of both Adacel vaccine and Td vaccine. Few participants (<1%) sought medical attention for these reactions. Pain at the injection site was the most common adverse reaction occurring in 63 to 78% of all vaccinees. In addition, overall rates of pain were higher in adolescent recipients of Adacel vaccine compared to Td vaccine recipients. Rates of moderate and severe pain in adolescents did not significantly differ between the Adacel vaccine and Td vaccine groups. Among adults the rates of pain, after receipt of Adacel vaccine or Td vaccine, did not significantly differ. Fever of 38°C and higher was uncommon, although in the adolescent age group, it occurred significantly more frequently in Adacel vaccine recipients than Td vaccine recipients. (9)
| Adolescents 11-17 years | Adults 18-64 years |
||||
|---|---|---|---|---|---|
| Adverse Event* | Adacel N† = 1,170-1,175 (%) | Td‡
N† = 783-787 (%) | Adacel N† = 1,688-1,698 (%) | Td‡
N† = 551-561 (%) |
|
|
|||||
| Injection Site Pain | Any | 77.8§ | 71.0 | 65.7 | 62.9 |
| Moderate¶ | 18.0 | 15.6 | 15.1 | 10.2 | |
| Severe# | 1.5 | 0.6 | 1.1 | 0.9 | |
| Injection Site Swelling | Any | 20.9 | 18.3 | 21.0 | 17.3 |
| Moderate¶ | |||||
| 1.0 to 3.4 cm | 6.5 | 5.7 | 7.6 | 5.4 | |
| Severe# | |||||
| ≥3.5 cm | 6.4 | 5.5 | 5.8 | 5.5 | |
| ≥5 cm (2 inches) | 2.8 | 3.6 | 3.2 | 2.7 | |
| Injection Site Erythema | Any | 20.8 | 19.7 | 24.7 | 21.6 |
| Moderate¶ | |||||
| 1.0 to 3.4 cm | 5.9 | 4.6 | 8.0 | 8.4 | |
| Severe# | |||||
| ≥3.5 cm | 6.0 | 5.3 | 6.2 | 4.8 | |
| ≥5 cm (2 inches) | 2.7 | 2.9 | 4.0 | 3.0 | |
| Fever | ≥38.0°C (≥100.4°F) | 5.0§ | 2.7 | 1.4 | 1.1 |
| ≥38.8°C to ≤39.4°C (≥102.0°F to ≤103.0°F) | 0.9 | 0.6 | 0.4 | 0.2 | |
| ≥39.5°C (≥103.1°F) | 0.2 | 0.1 | 0.0 | 0.2 | |
The frequency of other solicited adverse events (Days 0-14) are presented in Table 6. The rates of these events following Adacel vaccine were comparable with those observed with Td vaccine. Headache was the most frequent systemic reaction and was usually of mild to moderate intensity.
| Adverse Event | Adolescents 11-17 years | Adults 18-64 years |
|||
|---|---|---|---|---|---|
| Adacel N* = 1,174-1,175 (%) | Td†
N* = 787 (%) | Adacel N* = 1,697-1,698 (%) | Td†
N* = 560-561 (%) |
||
|
|||||
| Headache | Any | 43.7 | 40.4 | 33.9 | 34.1 |
| Moderate‡ | 14.2 | 11.1 | 11.4 | 10.5 | |
| Severe§ | 2.0 | 1.5 | 2.8 | 2.1 | |
| Body Ache or Muscle Weakness | Any | 30.4 | 29.9 | 21.9 | 18.8 |
| Moderate‡ | 8.5 | 6.9 | 6.1 | 5.7 | |
| Severe§ | 1.3 | 0.9 | 1.2 | 0.9 | |
| Tiredness | Any | 30.2 | 27.3 | 24.3 | 20.7 |
| Moderate‡ | 9.8 | 7.5 | 6.9 | 6.1 | |
| Severe§ | 1.2 | 1.0 | 1.3 | 0.5 | |
| Chills | Any | 15.1 | 12.6 | 8.1 | 6.6 |
| Moderate‡ | 3.2 | 2.5 | 1.3 | 1.6 | |
| Severe§ | 0.5 | 0.1 | 0.7 | 0.5 | |
| Sore and Swollen Joints | Any | 11.3 | 11.7 | 9.1 | 7.0 |
| Moderate‡ | 2.6 | 2.5 | 2.5 | 2.1 | |
| Severe§ | 0.3 | 0.1 | 0.5 | 0.5 | |
| Nausea | Any | 13.3 | 12.3 | 9.2 | 7.9 |
| Moderate‡ | 3.2 | 3.2 | 2.5 | 1.8 | |
| Severe§ | 1.0 | 0.6 | 0.8 | 0.5 | |
| Lymph Node Swelling | Any | 6.6 | 5.3 | 6.5 | 4.1 |
| Moderate‡ | 1.0 | 0.5 | 1.2 | 0.5 | |
| Severe§ | 0.1 | 0.0 | 0.1 | 0.0 | |
| Diarrhea | Any | 10.3 | 10.2 | 10.3 | 11.3 |
| Moderate‡ | 1.9 | 2.0 | 2.2 | 2.7 | |
| Severe§ | 0.3 | 0.0 | 0.5 | 0.5 | |
| Vomiting | Any | 4.6 | 2.8 | 3.0 | 1.8 |
| Moderate‡ | 1.2 | 1.1 | 1.0 | 0.9 | |
| Severe§ | 0.5 | 0.3 | 0.5 | 0.2 | |
| Rash | Any | 2.7 | 2.0 | 2.0 | 2.3 |
Local and systemic solicited reactions occurred at similar rates in Adacel vaccine and Td vaccine recipients in the 3 day post-vaccination period. Most local reactions occurred within the first 3 days after vaccination (with a mean duration of less than 3 days).
The rates of unsolicited adverse events reported from days 14-28 post-vaccination were comparable between the two groups, as were the rates of unsolicited adverse events from day 28 through 6 months.
There were no spontaneous reports of whole-arm swelling of the injected limb in this study, nor in the other three studies which contributed to the safety database for Adacel vaccine.
Adverse Events in the Concomitant Vaccine Studies
Local and Systemic Reactions when Given with Hepatitis B Vaccine
The rates reported for fever and injection site pain (at the Adacel vaccine administration site) were similar when Adacel and Hep B vaccines were given concurrently or separately. However, the rates of injection site erythema (23.4% for concomitant vaccination and 21.4% for separate administration) and swelling (23.9% for concomitant vaccination and 17.9% for separate administration) at the Adacel vaccine administration site were increased when co-administered. Swollen and/or sore joints were reported by 22.5% for concomitant vaccination and 17.9% for separate administration. The rates of generalized body aches in the individuals who reported swollen and/or sore joints were 86.7% for concomitant vaccination and 72.2% for separate administration. Most joint complaints were mild in intensity with a mean duration of 1.8 days. The incidence of other solicited and unsolicited adverse events were not different between the 2 study groups. (9)
Local and Systemic Reactions when Given with Trivalent Inactivated Influenza Vaccine
The rates of fever and injection site erythema and swelling were similar for recipients of concurrent and separate administration of Adacel vaccine and TIV. However, pain at the Adacel vaccine injection site occurred at statistically higher rates following concurrent administration (66.6%) versus separate administration (60.8%). The rates of sore and/or swollen joints were 13% for concurrent administration and 9% for separate administration. Most joint complaints were mild in intensity with a mean duration of 2.0 days. The incidence of other solicited and unsolicited adverse events were similar between the 2 study groups. (9)
Additional Studies
An additional 1,806 adolescents received Adacel vaccine as part of the lot consistency study used to support Adacel vaccine licensure. This study was a randomized, double-blind, multi-center trial designed to assess lot consistency as measured by the safety and immunogenicity of 3 lots of Adacel vaccine when given as a booster dose to adolescents 11-17 years of age inclusive. Local and systemic adverse events were monitored for 14 days post-vaccination using a diary card. Unsolicited adverse events and serious adverse events were collected for 28 days post-vaccination. Pain was the most frequently reported local adverse event occurring in approximately 80% of all participants. Headache was the most frequently reported systemic event occurring in approximately 44% of all participants. Sore and/or swollen joints were reported by approximately 14% of participants. Most joint complaints were mild in intensity with a mean duration of 2.0 days. (9)
An additional 962 adolescents and adults received Adacel vaccine in three supportive Canadian studies used as the basis for licensure in other countries. Within these clinical trials, the rates of local and systemic reactions following Adacel vaccine were similar to those reported in the four principal trials in the US with the exception of a higher rate (86%) of adults experiencing 'any' local injection site pain. The rate of severe pain (0.8%), however, was comparable to the rates reported in four principal trials conducted in the US. (9) There was one spontaneous report of whole-arm swelling of the injected limb among the 277 Td vaccine recipients, and two spontaneous reports among the 962 Adacel vaccine recipients in the supportive Canadian studies.
Postmarketing Reports
The following adverse events have been spontaneously reported during the post-marketing use of Adacel vaccine in the US and other countries. Because these events are reported voluntarily from a population of uncertain size, it is not possible to reliably estimate their frequency or establish a causal relationship to vaccine exposure.
The following adverse events were included based on severity, frequency of reporting or the strength of causal association to Adacel vaccine.
General disorders and administration site conditions:
- Large injection site reactions (>50 mm), extensive limb swelling from the injection site beyond one or both joints.
- Injection site bruising, sterile abscess
Nervous system disorders:
- Paraesthesia, hypoesthesia, Guillain-Barré syndrome, facial palsy, convulsion, syncope, myelitis
Immune system disorders:
- Anaphylactic reaction, hypersensitivity reaction (angioedema, edema, rash, hypotension)
Skin and subcutaneous tissue disorders:
- Pruritus, urticaria
Musculoskeletal and connective tissue disorders:
- Myositis, muscle spasm
Cardiac disorders:
- Myocarditis
Additional Adverse Events
Additional adverse events, included in this section, have been reported in conjunction with receipt of vaccines containing diphtheria, tetanus toxoids and/or pertussis antigens.
Arthus-type hypersensitivity reactions, characterized by severe local reactions (generally starting 2-8 hours after an injection), may follow receipt of tetanus toxoid. Such reactions may be associated with high levels of circulating antitoxin in persons who have had overly frequent injections of tetanus toxoid. (14) (See WARNINGS.)
Persistent nodules at the site of injection have been reported following the use of adsorbed products. (12)
Certain neurological conditions have been reported in temporal association with some tetanus toxoid containing vaccines or tetanus and diphtheria toxoid containing vaccines. A review by the Institute of Medicine (IOM) concluded that the evidence favors acceptance of a causal relation between tetanus toxoid and both brachial neuritis and Guillain-Barré syndrome. Other neurological conditions that have been reported include: demyelinating diseases of the central nervous system, peripheral mononeuropathies, and cranial mononeuropathies. The IOM has concluded that the evidence is inadequate to accept or reject a causal relation between these conditions and vaccines containing tetanus and/or diphtheria toxoids.
Reporting of Adverse Events
The National Vaccine Injury Compensation Program, established by the National Childhood Vaccine Injury Act of 1986, requires physicians and other health-care providers who administer vaccines to maintain permanent vaccination records of the manufacturer and lot number of the vaccine administered in the vaccine recipient's permanent medical record along with the date of administration of the vaccine and the name, address and title of the person administering the vaccine. The Act further requires the health-care professional to report to the US Department of Health and Human Services the occurrence following immunization of any event set forth in the Vaccine Injury Table. These include anaphylaxis or anaphylactic shock within 7 days; brachial neuritis within 28 days; an acute complication or sequelae (including death) of an illness, disability, injury, or condition referred to above, or any events that would contraindicate further doses of vaccine, according to this Adacel vaccine package insert. (15) (16) (17)
The US Department of Health and Human Services has established the Vaccine Adverse Event Reporting System (VAERS) to accept all reports of suspected adverse events after the administration of any vaccine. Reporting of all adverse events occurring after vaccine administration is encouraged from vaccine recipients, parents/guardians and the health-care provider. Adverse events following immunization should be reported to VAERS. Reporting forms and information about reporting requirements or completion of the form can be obtained from VAERS through a toll-free number 1-800-822-7967 or visit the VAERS website at www.vaers.hhs.gov (15) (16) (17)
Health-care providers should also report these events to Sanofi Pasteur Inc., Discovery Drive, Swiftwater, PA 18370 or call 1-800-822-2463 (1-800-VACCINE).
DOSAGE AND ADMINISTRATION
Adacel vaccine should be administered as a single injection of one dose (0.5 mL) by the intramuscular route. Adacel vaccine should not be combined through reconstitution or mixed with any other vaccine.
Just before use, shake the vial well until a uniform, white, cloudy suspension results.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit. (See DESCRIPTION.) If these conditions exist, the vaccine should not be administered.
When administering a dose from a rubber-stoppered vial, do not remove either the stopper or the metal seal holding it in place.
The preferred site is into the deltoid muscle. The vaccine should not be injected into the gluteal area or areas where there is a major nerve trunk.
Do NOT administer this product intravenously or subcutaneously.
Five years should have elapsed since the recipient's last dose of tetanus toxoid, diphtheria toxoid and/or pertussis containing vaccine.
There are no data to support repeat administration of Adacel vaccine.
The use of Adacel vaccine as a primary series or to complete the primary series for tetanus, diphtheria, or pertussis has not been studied.
Diphtheria Prophylaxis for Case Contacts
The ACIP has published recommendations on vaccination for diphtheria prophylaxis in individuals who have had contact with a person with confirmed or suspected diphtheria. (4)
Tetanus Prophylaxis in Wound Management
Clinicians should refer to guidelines for tetanus prophylaxis in routine wound management. (4) (13)
A thorough attempt must be made to determine whether a patient has completed primary immunization. Individuals who have completed primary immunization against tetanus and who sustain wounds that are minor and uncontaminated, should receive a booster dose of a tetanus toxoid containing preparation if they have not received tetanus toxoid within the preceding 10 years. For tetanus prone wounds (e.g., wounds contaminated with dirt, feces, soil and saliva, puncture wounds, avulsions and wounds resulting from missiles, crushing, burns or frostbite), a booster is appropriate if the patient has not received a tetanus toxoid containing preparation within the preceding 5 years. (4)
Adacel vaccine can be used as a one-time alternative to Tetanus and Diphtheria Toxoids Adsorbed for Adult Use (Td) vaccine in patients for whom the pertussis component is also indicated. (See INDICATIONS AND USAGE.)
If passive protection against tetanus is required, Tetanus Immune Globulin (Human) (TIG) may be administered at a separate site with a separate needle and syringe.
Concomitant Vaccine Administration
Safety and immunogenicity data are available on concomitant administration of Adacel vaccine with Hepatitis B (10 µg, two dose regimen) and trivalent inactivated influenza vaccines (TIV). (See CLINICAL PHARMACOLOGY and ADVERSE REACTIONS sections.)
Concomitant immunization of Adacel vaccine with Hepatitis B vaccine did not result in reduced antibody responses to any of the antigens from either vaccine. (9)
No interference in tetanus and diphtheria seroprotection rates and responses to influenza vaccine, detoxified PT, FIM or FHA were observed when Adacel vaccine was administered concomitantly with TIV compared to separate administration. A lower PRN GMC was observed when Adacel vaccine was administered concomitantly with TIV compared to separate administration. (9)
The safety and effectiveness of concomitant administration of Adacel vaccine with other vaccines has not been evaluated.
Separate injection sites and separate syringes must be used in case of concomitant administration.
STORAGE
Adacel vaccine should be stored at 2° to 8°C (35° to 46°F). DO NOT FREEZE. Product which has been exposed to freezing should not be used.
Do not use after expiration date shown on the label.
HOW SUPPLIED
Syringe, without needle, 1 dose (5 per package) – Product No. 49281-400-15
Vial, 1 dose (5 per package) – Product No. 49281-400-05
Vial, 1 dose (10 per package) – Product No. 49281-400-10
Neither the vial nor the syringe for this product contain latex.
REFERENCES
- 1
- Stainer DW, et al. A simple chemically defined medium for the production of phase I Bordetella pertussis. J Gen Microbiol 1970;63:211-20.
- 2
- Stainer DW. Production of diphtheria toxin. In: Manclark CR, editor. Proceedings of an informal consultation on the World Health Organization requirements for diphtheria, tetanus, pertussis and combined vaccines. United States Public Health Service, Bethesda, MD. DHHS 91-1174. 1991. p. 7-11.
- 3
- Mueller JH, et al. Variable factors influencing the production of tetanus toxin. J Bacteriol 1954;67(3):271-7.
- 4
- CDC. Diphtheria, tetanus and pertussis: recommendations for vaccine use and other preventive measures. Recommendations of the Immunization Practices Advisory Committee (ACIP). MMWR 1991;40(RR-10):1-28.
- 5
- CDC. General recommendations on immunization. Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR 2006;55(RR-15):1-48.
- 6
- FDA. Department of Health and Human Services (DHHS). Biological products bacterial vaccines and toxoids; implementation of efficacy review; proposed rule. Fed Reg 1985;50(240):51002-117.
- 7
- Diphtheria toxoid. Tetanus toxoid. In: Plotkin SA, Orenstein WA, editors. Vaccines. 4th ed. Philadelphia, PA: WB Saunders; 2004. p. 211-28, 745-81.
- 8
- Gustafsson L, et al. A controlled trial of a two-component acellular, a five-component acellular and a whole-cell pertussis vaccine. N Engl J Med 1996;334(6):349-55.
- 9
- Data on file at Sanofi Pasteur Limited.
- 10
- CDC. Preventing tetanus, diphtheria and pertussis among adults: use of tetanus toxoid, reduced diphtheria toxoid and acellular pertussis vaccine. MMWR 2006;55(RR-17):1-36.
- 11
- CDC. Preventing tetanus, diphtheria and pertussis among adolescents: use of tetanus toxoid, reduced diphtheria toxoid and acellular pertussis vaccines. MMWR 2006;55(RR-3):1-35.
- 12
- CDC. Update: vaccine side effects, adverse reactions, contraindications and precautions. Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR 1996;45(RR-12):1-35.
- 13
- CDC. Update on adult immunization. Recommendations of the Immunization Practices Advisory Committee (ACIP). MMWR 1991;40(RR-12):1-52.
- 14
- Stratton KR, et al, editors. Adverse events associated with childhood vaccines; evidence bearing on causality. Washington: National Academy Press; 1994. p. 67-117.
- 15
- CDC. Current trends - Vaccine Adverse Event Reporting System (VAERS) United States. MMWR 1990;39(41):730-3.
- 16
- CDC. Current trends - national vaccine injury act: requirements for permanent vaccination records and for reporting of selected events after vaccination. MMWR 1988;37(13):197-200.
- 17
- FDA. New reporting requirements for vaccine adverse events. FDA Drug Bull 1988;18(2):16-8.
Product Information as of January 2009.
Printed in USA.
Manufactured by:
Sanofi Pasteur Limited
Toronto Ontario Canada
Distributed by:
Sanofi Pasteur Inc.
Swiftwater PA 18370 USA
R5-0109 USA
5751
PRINCIPAL DISPLAY PANEL - Syringe Label
NDC 49281-400-15
Adolescent/Adult
Tdap
Tetanus Toxoid, Reduced
Diphtheria Toxoid and Acellular
Pertussis Vaccine Adsorbed
Adacel®
Rx only
0.5 mL Dose
IM only
Sanofi Pasteur Limited
5433
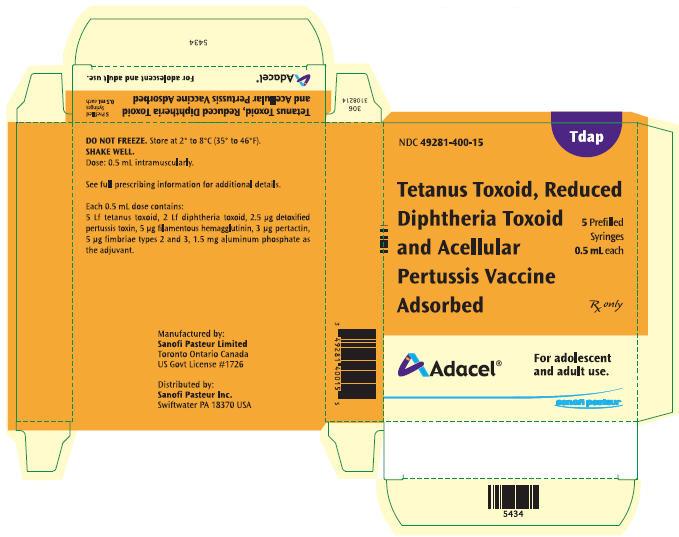
PRINCIPAL DISPLAY PANEL - Syringe Container
NDC 49281-400-15
Tdap
Tetanus Toxoid, Reduced
Diphtheria Toxoid
and Acellular
Pertussis Vaccine
Adsorbed
5 Prefilled
Syringes
0.5 mL each
Rx only
Adacel®
For adolescent
and adult use.
sanofi pasteur
| ADACEL
TDAP
clostridium tetani toxoid antigen (formaldehyde inactivated), corynebacterium diphtheriae toxoid antigen (formaldehyde inactivated), bordetella pertussis toxoid antigen (glutaraldehyde inactivated), bordetella pertussis filamentous hemagglutinin antigen (formaldehyde inactivated), bordetella pertussis pertactin antigen, and bordetella pertussis fimbriae 2/3 antigen injection, suspension |
|||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||
| Marketing Information | |||
| Marketing Category | Application Number or Monograph Citation | Marketing Start Date | Marketing End Date |
| BLA | BLA125111 | 06/10/2005 | |
| Labeler - Sanofi Pasteur Limited (086723285) |
| Establishment | |||
| Name | Address | ID/FEI | Operations |
| Sanofi Pasteur Limited | 208206623 | MANUFACTURE | |