PEGASYS
-
peginterferon alfa-2a injection, solution
Hoffmann-La Roche Inc
----------
PEGASYS®(peginterferon alfa-2a)
Alpha interferons, including PEGASYS (peginterferon alfa-2a), may cause or aggravate fatal or life-threatening neuropsychiatric, autoimmune, ischemic, and infectious disorders. Patients should be monitored closely with periodic clinical and laboratory evaluations. Therapy should be withdrawn in patients with persistently severe or worsening signs or symptoms of these conditions. In many, but not all cases, these disorders resolve after stopping PEGASYS therapy (see WARNINGS and ADVERSE REACTIONS).
Use with Ribavirin. Ribavirin, including COPEGUS®, may cause birth defects and/or death of the fetus. Extreme care must be taken to avoid pregnancy in female patients and in female partners of male patients. Ribavirin causes hemolytic anemia. The anemia associated with ribavirin therapy may result in a worsening of cardiac disease. Ribavirin is genotoxic and mutagenic and should be considered a potential carcinogen (see COPEGUS Package Insert for additional information and other WARNINGS).
DESCRIPTION
PEGASYS, peginterferon alfa-2a, is a covalent conjugate of recombinant alfa-2a interferon (approximate molecular weight [MW] 20,000 daltons) with a single branched bis-monomethoxy polyethylene glycol (PEG) chain (approximate MW 40,000 daltons). The PEG moiety is linked at a single site to the interferon alfa moiety via a stable amide bond to lysine. Peginterferon alfa-2a has an approximate molecular weight of 60,000 daltons. Interferon alfa-2a is produced using recombinant DNA technology in which a cloned human leukocyte interferon gene is inserted into and expressed in Escherichia coli.
PEGASYS is supplied as an injectable solution in vials and prefilled syringes.
180 µg/1.0 mL Vial: A vial contains approximately 1.2 mL of solution to deliver 1.0 mL of drug product. Subcutaneous (sc) administration of 1.0 mL delivers 180 µg of drug product (expressed as the amount of interferon alfa-2a), 8.0 mg sodium chloride, 0.05 mg polysorbate 80, 10.0 mg benzyl alcohol, 2.62 mg sodium acetate trihydrate, and 0.05 mg acetic acid. The solution is colorless to light yellow and the pH is 6.0 ± 0.5.
180 µg/0.5 mL Prefilled Syringe: Each syringe contains 0.6 mL of solution to deliver 0.5 mL of drug product. Subcutaneous (sc) administration of 0.5 mL delivers 180 µg of drug product (expressed as the amount of interferon alfa-2a), 4.0 mg sodium chloride, 0.025 mg polysorbate 80, 5.0 mg benzyl alcohol, 1.3085 mg sodium acetate trihydrate, and 0.0231 mg acetic acid. The solution is colorless to light yellow and the pH is 6.0 ± 0.5.
CLINICAL PHARMACOLOGY
Pharmacodynamics
Interferons bind to specific receptors on the cell surface initiating intracellular signaling via a complex cascade of protein-protein interactions leading to rapid activation of gene transcription. Interferon-stimulated genes modulate many biological effects including the inhibition of viral replication in infected cells, inhibition of cell proliferation and immunomodulation. The clinical relevance of these in vitro activities is not known.
PEGASYS stimulates the production of effector proteins such as serum neopterin and 2', 5'-oligoadenylate synthetase.
Pharmacokinetics
Maximal serum concentrations (Cmax) and AUC increased in a nonlinear dose related manner following administration of 90 to 270 µg of PEGASYS. Maximal serum concentrations (Cmax) occur between 72 to 96 hours post-dose.
Week 48 mean trough concentrations (16 ng/mL; range 4 to 28) at 168 hours post-dose are approximately 2-fold higher than week 1 mean trough concentrations (9 ng/mL; range 0 to 15). Steady-state serum levels are reached within 5 to 8 weeks of once weekly dosing. The peak to trough ratio at week 48 is approximately 2. The mean systemic clearance in healthy subjects given PEGASYS was 94 mL/h, which is approximately 100-fold lower than that for interferon alfa-2a (ROFERON®-A). The mean terminal half-life after sc dosing in patients with chronic hepatitis C was 160 hours (range 84 to 353 hours) compared to 5 hours (range 3.7 to 8.5 hours) for ROFERON-A.
Special Populations
Gender and Age
PEGASYS administration yielded similar pharmacokinetics in male and female healthy subjects. The AUC was increased from 1295 to 1663 ng∙h/mL in subjects older than 62 years taking 180 µg PEGASYS, but peak concentrations were similar (9 vs. 10 ng/mL) in those older and younger than 62 years.
Pediatric Patients
In a population pharmacokinetics study, 14 children 2 to 8 years of age with CHC received PEGASYS based on their body surface area (BSA of the child × 180 µg/1.73m2). The clearance of PEGASYS in children was nearly 4-fold lower compared to the clearance reported in adults.
Steady-state trough levels in children with the BSA-adjusted dosing were similar to trough levels observed in adults with 180 µg fixed dosing. Time to reach the steady state in children is approximately 12 weeks, whereas in adults, steady state is reached within 5 to 8 weeks. In these children receiving the BSA adjusted dose, the mean exposure (AUC) during the dosing interval is predicted to be 25% to 70% higher than that observed in adults receiving 180 µg fixed dosing. The safety and effectiveness of PEGASYS in patients below the age of 18 years have not been established (see PRECAUTIONS: Pediatric Use).
Renal Dysfunction
In patients with end stage renal disease undergoing hemodialysis, there is a 25% to 45% reduction in PEGASYS clearance (see PRECAUTIONS: Renal Impairment).
The pharmacokinetics of ribavirin following administration of COPEGUS have not been studied in patients with renal impairment and there are limited data from clinical trials on administration of COPEGUS in patients with creatinine clearance <50 mL/min. Therefore, patients with creatinine clearance <50 mL/min should not be treated with COPEGUS (see WARNINGS and DOSAGE AND ADMINISTRATION).
Effect of Food on Absorption of Ribavirin
Bioavailability of a single oral dose of ribavirin was increased by co-administration with a high-fat meal. The absorption was slowed (Tmax was doubled) and the AUC0-192h and Cmax increased by 42% and 66%, respectively, when COPEGUS was taken with a high-fat meal compared with fasting conditions (see DOSAGE AND ADMINISTRATION).
Drug Interactions
Nucleoside Analogues
In vitro data indicate ribavirin reduces phosphorylation of lamivudine, stavudine, and zidovudine. However, no pharmacokinetic (e.g., plasma concentrations or intracellular triphosphorylated active metabolite concentrations) or pharmacodynamic (e.g., loss of HIV/HCV virologic suppression) interaction was observed when ribavirin and lamivudine (n=18), stavudine (n=10), or zidovudine (n=6) were co-administered as part of a multi-drug regimen to HCV/HIV coinfected patients (see PRECAUTIONS: Drug Interactions).
In vitro, didanosine or its active metabolite (dideoxyadenosine 5'-triphosphate) is increased when didanosine is co-administered with ribavirin (see PRECAUTIONS: Drug Interactions).
Drugs Metabolized by Cytochrome P450
There was no effect on the pharmacokinetics of representative drugs metabolized by CYP 2C9, CYP 2C19, CYP 2D6 or CYP 3A4.
Treatment with PEGASYS once weekly for 4 weeks in healthy subjects was associated with an inhibition of P450 1A2 and a 25% increase in theophylline AUC (see PRECAUTIONS: Drug Interactions).
Methadone
The pharmacokinetics of concomitant administration of methadone and PEGASYS were evaluated in 24 PEGASYS naive chronic hepatitis C (CHC) patients (15 male, 9 female) who received 180 µg PEGASYS subcutaneously weekly. All patients were on stable methadone maintenance therapy (median dose 95 mg, range 30 mg to 150 mg) prior to receiving PEGASYS. Mean methadone PK parameters were 10% to 15% higher after 4 weeks of PEGASYS treatment as compared to baseline (see PRECAUTIONS: Drug Interactions). Methadone did not significantly alter the PK of PEGASYS as compared to a PK study of 6 chronic hepatitis C patients not receiving methadone.
CLINICAL STUDIES
Chronic Hepatitis C Studies 1, 2, and 3: PEGASYS Monotherapy
The safety and effectiveness of PEGASYS for the treatment of hepatitis C virus infection were assessed in three randomized, open-label, active-controlled clinical studies. All patients were adults, had compensated liver disease, detectable hepatitis C virus (HCV), liver biopsy diagnosis of chronic hepatitis, and were previously untreated with interferon. All patients received therapy by sc injection for 48 weeks, and were followed for an additional 24 weeks to assess the durability of response. In studies 1 and 2, approximately 20% of subjects had cirrhosis or bridging fibrosis. Study 3 enrolled patients with a histological diagnosis of cirrhosis (78%) or bridging fibrosis (22%).
In Study 1 (n=630), patients received either ROFERON-A (interferon alfa-2a) 3 MIU three times/week (tiw), PEGASYS 135 µg once each week (qw) or PEGASYS 180 µg qw. In Study 2 (n=526), patients received either ROFERON-A 6 MIU tiw for 12 weeks followed by 3 MIU tiw for 36 weeks or PEGASYS 180 µg qw. In Study 3 (n=269), patients received ROFERON-A 3 MIU tiw, PEGASYS 90 µg qw or PEGASYS 180 µg once each week.
In all three studies, treatment with PEGASYS 180 µg resulted in significantly more patients who experienced a sustained response (defined as undetectable HCV RNA [<50 IU/mL] using the COBAS AMPLICOR® HCV Test, version 2.0 and normalization of ALT on or after study week 68) compared to treatment with ROFERON-A. In Study 1, response to PEGASYS 135 µg was not different from response to 180 µg. In Study 3, response to PEGASYS 90 µg was intermediate between PEGASYS 180 µg and ROFERON-A.
| Study 1 | Study 2 | Study 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| ROFERON-A 3 MIU (N=207) | PEGASYS 180 µg (N=208) | DIFF*
(95% CI) | ROFERON-A 6/3 MIU (N=261) | PEGASYS 180 µg (N=265) | DIFF*
(95% CI) | ROFERON-A 3 MIU (N=86) | PEGASYS 180 µg (N=87) | DIFF*
(95% CI) |
|
|
|||||||||
| Combined Virologic and Biologic Sustained Response | 11% | 24% | 13 (6, 20) | 17% | 35% | 18 (11, 25) | 7% | 23% | 16 (6, 26) |
| Sustained Virologic Response | 11% | 26% | 15 (8, 23) | 19% | 38% | 19 (11, 26) | 8% | 30% | 22 (11, 33) |
Matched pre- and post-treatment liver biopsies were obtained in approximately 70% of patients. Similar modest reductions in inflammation compared to baseline were observed in all treatment groups.
Of the patients who did not demonstrate either undetectable HCV RNA or at least a 2log10 drop in HCV RNA titer from baseline by 12 weeks of PEGASYS 180 µg therapy, 2% (3/156) achieved a sustained virologic response (see DOSAGE AND ADMINISTRATION).
Averaged over Study 1, Study 2, and Study 3, response rates to PEGASYS were 23% among patients with viral genotype 1 and 48% in patients with other viral genotypes. The treatment response rates were similar in men and women.
Chronic Hepatitis C Studies 4 and 5: PEGASYS/COPEGUS Combination Therapy
The safety and effectiveness of PEGASYS in combination with COPEGUS for the treatment of hepatitis C virus infection were assessed in two randomized controlled clinical trials. All patients were adults, had compensated liver disease, detectable hepatitis C virus, liver biopsy diagnosis of chronic hepatitis, and were previously untreated with interferon. Approximately 20% of patients in both studies had compensated cirrhosis (Child-Pugh class A). Patients coinfected with HIV were excluded from these studies.
In Study 4, patients were randomized to receive either PEGASYS 180 µg sc once weekly (qw) with an oral placebo, PEGASYS 180 µg qw with COPEGUS 1000 mg po (body weight <75 kg) or 1200 mg po (body weight ≥75 kg) or Rebetron® (interferon alfa-2b 3 MIU sc tiw plus ribavirin 1000 mg or 1200 mg po). All patients received 48 weeks of therapy followed by 24 weeks of treatment-free follow-up. COPEGUS or placebo treatment assignment was blinded. Sustained virological response was defined as undetectable (<50 IU/mL) HCV RNA on or after study week 68. PEGASYS in combination with COPEGUS resulted in a higher SVR compared to PEGASYS alone or interferon alfa-2b and ribavirin (Table 2). In all treatment arms, patients with viral genotype 1, regardless of viral load, had a lower response rate.
| Interferon alfa-2b + Ribavirin 1000 mg or 1200 mg | PEGASYS + Placebo | PEGASYS + COPEGUS 1000 mg or 1200 mg | |
|---|---|---|---|
|
|||
| All patients | 197/444 (44%)* | 65/224 (29%) | 241/453 (53%)* |
| Genotype 1 | 103/285 (36%) | 29/145 (20%) | 132/298 (44%) |
| Genotypes 2-6 | 94/159 (59%) | 36/79 (46%) | 109/155 (70%) |
In Study 5 (see Table 3), all patients received PEGASYS 180 µg sc qw and were randomized to treatment for either 24 or 48 weeks and to a COPEGUS dose of either 800 mg or 1000 mg/1200 mg (for body weight <75 kg / ≥75 kg). Assignment to the four treatment arms was stratified by viral genotype and baseline HCV viral titer. Patients with genotype 1 and high viral titer (defined as >2 × 106 HCV RNA copies/mL serum) were preferentially assigned to treatment for 48 weeks.
HCV Genotypes
HCV 1 and 4 – Irrespective of baseline viral titer, treatment for 48 weeks with PEGASYS and 1000 mg or 1200 mg of COPEGUS resulted in higher SVR (defined as undetectable HCV RNA at the end of the 24-week treatment-free follow-up period) compared to shorter treatment (24 weeks) and/or 800 mg COPEGUS.
HCV 2 and 3 – Irrespective of baseline viral titer, treatment for 24 weeks with PEGASYS and 800 mg of COPEGUS resulted in a similar SVR compared to longer treatment (48 weeks) and/or 1000 mg or 1200 mg of COPEGUS (see Table 3).
The numbers of patients with genotype 5 and 6 were too few to allow for meaningful assessment.
| 24 Weeks Treatment | 48 Weeks Treatment | |||
|---|---|---|---|---|
| PEGASYS + COPEGUS 800 mg (N=207) | PEGASYS + COPEGUS 1000 mg or 1200 mg* (N=280) | PEGASYS + COPEGUS 800 mg (N=361) | PEGASYS + COPEGUS 1000 mg or 1200 mg* (N=436) |
|
|
||||
| Genotype 1 | 29/101 (29%) | 48/118 (41%) | 99/250 (40%) | 138/271 (51%) |
| Genotypes 2, 3 | 79/96 (82%) | 116/144 (81%) | 75/99 (76%) | 117/153 (76%) |
| Genotype 4 | 0/5 (0%) | 7/12 (58%) | 5/8 (63%) | 9/11 (82%) |
Other Treatment Response Predictors
Treatment response rates are lower in patients with poor prognostic factors receiving pegylated interferon alpha therapy. In studies 4 and 5, treatment response rates were lower in patients older than 40 years (50% vs. 66%), in patients with cirrhosis (47% vs. 59%), in patients weighing over 85 kg (49% vs. 60%), and in patients with genotype 1 with high vs. low viral load (43% vs. 56%). African-American patients had lower response rates compared to Caucasians.
Paired liver biopsies were performed on approximately 20% of patients in studies 4 and 5. Modest reductions in inflammation compared to baseline were seen in all treatment groups.
In studies 4 and 5, lack of early virologic response by 12 weeks (defined as HCV RNA undetectable or >2log10 lower than baseline) was grounds for discontinuation of treatment. Of patients who lacked an early viral response by 12 weeks and completed a recommended course of therapy despite a protocol-defined option to discontinue therapy, 5/39 (13%) achieved an SVR. Of patients who lacked an early viral response by 24 weeks, 19 completed a full course of therapy and none achieved an SVR.
Chronic Hepatitis C and Coinfection with HIV (CHC/HIV) Study 6: PEGASYS Monotherapy and PEGASYS/COPEGUS Combination Therapy
In Study 6, patients with CHC/HIV were randomized to receive either PEGASYS 180 µg sc once weekly (qw) plus an oral placebo, PEGASYS 180 µg qw plus COPEGUS 800 mg po daily or ROFERON-A (interferon alfa-2a), 3 MIU sc tiw plus COPEGUS 800 mg po daily. All patients received 48 weeks of therapy and sustained virologic response (SVR) was assessed at 24 weeks of treatment-free follow-up. COPEGUS or placebo treatment assignment was blinded in the PEGASYS treatment arms. All patients were adults, had compensated liver disease, detectable hepatitis C virus, liver biopsy diagnosis of chronic hepatitis C, and were previously untreated with interferon. Patients also had CD4+ cell count ≥200 cells/µL or CD4+ cell count ≥100 cells/µL but <200 cells/µL and HIV-1 RNA <5000 copies/mL, and stable status of HIV. Approximately 15% of patients in the study had cirrhosis. Results are shown in Table 4.
| ROFERON-A + COPEGUS 800 mg (N=289) | PEGASYS + Placebo (N=289) | PEGASYS + COPEGUS 800 mg (N=290) |
|
|---|---|---|---|
|
|||
| All patients | 33 (11%)* | 58 (20%)* | 116 (40%) |
| Genotype 1 | 12/171 (7%) | 24/175 (14%) | 51/176 (29%) |
| Genotypes 2, 3 | 18/89 (20%) | 32/90 (36%) | 59/95 (62%) |
Treatment response rates are lower in CHC/HIV patients with poor prognostic factors (including HCV genotype 1, HCV RNA >800,000 IU/mL, and cirrhosis) receiving pegylated interferon alpha therapy. Geographic region is not a prognostic factor for response. However, poor prognostic factors occur more frequently in the US population than in the non-US population.
Of the patients who did not demonstrate either undetectable HCV RNA or at least a 2log10 reduction from baseline in HCV RNA titer by 12 weeks of PEGASYS and COPEGUS combination therapy, 2% (2/85) achieved an SVR.
In CHC patients with HIV coinfection who received 48 weeks of PEGASYS alone or in combination with COPEGUS treatment, mean and median HIV RNA titers did not increase above baseline during treatment or 24 weeks post-treatment.
Chronic Hepatitis B Studies 7 and 8: PEGASYS Monotherapy
The safety and effectiveness of PEGASYS for the treatment of chronic hepatitis B were assessed in controlled clinical trials in HBeAg positive (Study 7) and HBeAg negative (Study 8) patients with chronic hepatitis B.
Patients were randomized to PEGASYS 180 µg sc once weekly (qw), PEGASYS 180 µg sc qw combined with lamivudine 100 mg once daily po or lamivudine 100 mg once daily po. All patients received 48 weeks of their assigned therapy followed by 24 weeks of treatment-free follow-up. Assignment to receipt of PEGASYS or no PEGASYS was not masked.
All patients were adults with compensated liver disease, had chronic hepatitis B virus (HBV) infection, and evidence of HBV replication (serum HBV >500,000 copies/mL for Study 7 and >100,000 copies/mL for Study 8) as measured by PCR (COBAS AMPLICOR® HBV Assay). All patients had serum alanine aminotransferase (ALT) between 1 and 10 times the upper limit of normal (ULN) and liver biopsy findings compatible with the diagnosis of chronic hepatitis.
The results observed in the PEGASYS and lamivudine monotherapy groups are shown in Table 5.
| Study 7 HBeAg positive | Study 8 HBeAg negative |
|||||
|---|---|---|---|---|---|---|
|
||||||
| Lamivudine N = 272 | PEGASYS N = 271 | Lamivudine N = 181 | PEGASYS N = 177 |
|||
| EOT* | EOF† | EOF† | EOT* | EOF† | EOF† | |
| HBeAg Seroconversion (%) | 20 | 19‡ | 32‡ | NA | NA | NA |
| HBV DNA Response (%)§ | 62 | 22¶ | 32¶ | 85 | 29# | 43# |
| ALT Normalization (%) | 62 | 28 | 41 | 73 | 44# | 59# |
| HBsAg Seroconversion (%) | 0 | 0 | 3 | 1 | 0 | 3 |
| N = 184 | N = 207 | N = 125 | N = 143 | |||
| Histological Improvement (%)Þ | ND | 40 | 41 | ND | 41 | 48 |
| Changes in Ishak fibrosis score compared to baseline (%): | ||||||
| - Improvedß | ND | 32 | 25 | ND | 31 | 32 |
| - Unchanged | 20 | 25 | 23 | 30 | ||
| - Worsenedß | 16 | 26 | 15 | 19 | ||
PEGASYS co-administered with lamivudine did not result in any additional sustained response when compared to PEGASYS monotherapy.
Conclusions regarding comparative efficacy of PEGASYS and lamivudine treatment based upon the end of follow-up results are limited by the different mechanisms of action of the two compounds. Most treatment effects of lamivudine are unlikely to persist 24 weeks after therapy is withdrawn.
INDICATIONS AND USAGE
PEGASYS, peginterferon alfa-2a, alone or in combination with COPEGUS, is indicated for the treatment of adults with chronic hepatitis C virus infection who have compensated liver disease and have not been previously treated with interferon alpha. Patients in whom efficacy was demonstrated included patients with compensated liver disease and histological evidence of cirrhosis (Child-Pugh class A) and patients with HIV disease that is clinically stable (e.g., antiretroviral therapy not required or receiving stable antiretroviral therapy).
PEGASYS is indicated for the treatment of adult patients with HBeAg positive and HBeAg negative chronic hepatitis B who have compensated liver disease and evidence of viral replication and liver inflammation.
CONTRAINDICATIONS
PEGASYS is contraindicated in patients with:
- Hypersensitivity to PEGASYS or any of its components
- Autoimmune hepatitis
- Hepatic decompensation (Child-Pugh score greater than 6 [class B and C]) in cirrhotic patients before or during treatment
- Hepatic decompensation with Child-Pugh score greater than or equal to 6 in cirrhotic CHC patients coinfected with HIV before or during treatment
PEGASYS is contraindicated in neonates and infants because it contains benzyl alcohol. Benzyl alcohol is associated with an increased incidence of neurologic and other complications in neonates and infants, which are sometimes fatal.
PEGASYS and COPEGUS combination therapy is additionally contraindicated in:
- Patients with known hypersensitivity to COPEGUS or to any component of the tablet
- Women who are pregnant
- Men whose female partners are pregnant
- Patients with hemoglobinopathies (e.g., thalassemia major, sickle-cell anemia)
WARNINGS
General
Patients should be monitored for the following serious conditions, some of which may become life threatening. Patients with persistently severe or worsening signs or symptoms should have their therapy withdrawn (see BOXED WARNING).
Neuropsychiatric
Life-threatening or fatal neuropsychiatric reactions may manifest in patients receiving therapy with PEGASYS and include suicide, suicidal ideation, homicidal ideation, depression, relapse of drug addiction, and drug overdose. These reactions may occur in patients with and without previous psychiatric illness.
PEGASYS should be used with extreme caution in patients who report a history of depression. Neuropsychiatric adverse events observed with alpha interferon treatment include aggressive behavior, psychoses, hallucinations, bipolar disorders, and mania. Physicians should monitor all patients for evidence of depression and other psychiatric symptoms. Patients should be advised to report any sign or symptom of depression or suicidal ideation to their prescribing physicians. In severe cases, therapy should be stopped immediately and psychiatric intervention instituted (see ADVERSE REACTIONS and DOSAGE AND ADMINISTRATION).
Infections
While fever may be associated with the flu-like syndrome reported commonly during interferon therapy, other causes of high or persistent fever must be ruled out, particularly in patients with neutropenia. Serious and severe infections (bacterial, viral, fungal), some fatal, have been reported during treatment with alpha interferons including PEGASYS. Appropriate anti-infective therapy should be started immediately and discontinuation of therapy should be considered.
Bone Marrow Toxicity
PEGASYS suppresses bone marrow function and may result in severe cytopenias. Ribavirin may potentiate the neutropenia and lymphopenia induced by alpha interferons including PEGASYS. Very rarely alpha interferons may be associated with aplastic anemia. It is advised that complete blood counts (CBC) be obtained pre-treatment and monitored routinely during therapy (see PRECAUTIONS: Laboratory Tests).
PEGASYS and COPEGUS should be used with caution in patients with baseline neutrophil counts <1500 cells/mm3, with baseline platelet counts <90,000 cells/mm3 or baseline hemoglobin <10 g/dL. PEGASYS therapy should be discontinued, at least temporarily, in patients who develop severe decreases in neutrophil and/or platelet counts (see DOSAGE AND ADMINISTRATION: Dose Modifications).
Severe neutropenia and thrombocytopenia occur with a greater incidence in HIV coinfected patients than monoinfected patients and may result in serious infections or bleeding (see ADVERSE REACTIONS).
Cardiovascular Disorders
Hypertension, supraventricular arrhythmias, chest pain, and myocardial infarction have been observed in patients treated with PEGASYS.
PEGASYS should be administered with caution to patients with pre-existing cardiac disease. Because cardiac disease may be worsened by ribavirin-induced anemia, patients with a history of significant or unstable cardiac disease should not use COPEGUS (see WARNINGS: Anemia and COPEGUS Package Insert).
Cerebrovascular Disorders
Ischemic and hemorrhagic cerebrovascular events have been observed in patients treated with interferon alfa-based therapies, including PEGASYS. Events occurred in patients with few or no reported risk factors for stroke, including patients less than 45 years of age. Because these are spontaneous reports, estimates of frequency cannot be made and a causal relationship between interferon alfa-based therapies and these events is difficult to establish.
Hepatic Failure and Hepatitis Exacerbations
Chronic hepatitis C (CHC) patients with cirrhosis may be at risk of hepatic decompensation and death when treated with alpha interferons, including PEGASYS. Cirrhotic CHC patients coinfected with HIV receiving highly active antiretroviral therapy (HAART) and interferon alfa-2a with or without ribavirin appear to be at increased risk for the development of hepatic decompensation compared to patients not receiving HAART. In Study 6, among 129 CHC/HIV cirrhotic patients receiving HAART, 14 (11%) of these patients across all treatment arms developed hepatic decompensation resulting in 6 deaths. All 14 patients were on NRTIs, including stavudine, didanosine, abacavir, zidovudine, and lamivudine. These small numbers of patients do not permit discrimination between specific NRTIs for the associated risk. During treatment, patients' clinical status and hepatic function should be closely monitored, and PEGASYS treatment should be immediately discontinued if decompensation (Child-Pugh score ≥6) is observed (see CONTRAINDICATIONS).
Exacerbations of hepatitis during hepatitis B therapy are not uncommon and are characterized by transient and potentially severe increases in serum ALT. Chronic hepatitis B patients experienced transient acute exacerbations (flares) of hepatitis B (ALT elevation >10-fold higher than the upper limit of normal) during PEGASYS treatment (12% and 18%) and post-treatment (7% and 12%) in HBeAg negative and HBeAg positive patients, respectively. Marked transaminase flares while on PEGASYS therapy have been accompanied by other liver test abnormalities. Patients experiencing ALT flares should receive more frequent monitoring of liver function. PEGASYS dose reduction should be considered in patients experiencing transaminase flares. If ALT increases are progressive despite reduction of PEGASYS dose or are accompanied by increased bilirubin or evidence of hepatic decompensation, PEGASYS should be immediately discontinued (see ADVERSE REACTIONS: Chronic Hepatitis B and DOSAGE AND ADMINISTRATION: Dose Modifications).
Hypersensitivity
Severe acute hypersensitivity reactions (e.g., urticaria, angioedema, bronchoconstriction, and anaphylaxis) have been rarely observed during alpha interferon and ribavirin therapy. If such reaction occurs, therapy with PEGASYS and COPEGUS should be discontinued and appropriate medical therapy immediately instituted. Serious skin reactions including vesiculobullous eruptions, reactions in the spectrum of Stevens Johnson Syndrome (erythema multiforme major) with varying degrees of skin and mucosal involvement and exfoliative dermatitis (erythroderma) have been rarely reported in patients receiving PEGASYS with and without ribavirin. Patients developing signs or symptoms of severe skin reactions must discontinue therapy (see ADVERSE REACTIONS: Postmarketing Experience).
Endocrine Disorders
PEGASYS causes or aggravates hypothyroidism and hyperthyroidism. Hyperglycemia, hypoglycemia, and diabetes mellitus have been observed to develop in patients treated with PEGASYS. Patients with these conditions at baseline who cannot be effectively treated by medication should not begin PEGASYS therapy. Patients who develop these conditions during treatment and cannot be controlled with medication may require discontinuation of PEGASYS therapy.
Autoimmune Disorders
Development or exacerbation of autoimmune disorders including myositis, hepatitis, thrombotic thrombocytopenic purpura, idiopathic thrombocytopenic purpura, psoriasis, rheumatoid arthritis, interstitial nephritis, thyroiditis, and systemic lupus erythematosus have been reported in patients receiving alpha interferon. PEGASYS should be used with caution in patients with autoimmune disorders.
Pulmonary Disorders
Dyspnea, pulmonary infiltrates, pneumonia, bronchiolitis obliterans, interstitial pneumonitis, pulmonary hypertension and sarcoidosis, some resulting in respiratory failure and/or patient deaths, may be induced or aggravated by PEGASYS or alpha interferon therapy. Recurrence of respiratory failure has been observed with interferon rechallenge. PEGASYS combination treatment should be suspended in patients who develop pulmonary infiltrates or pulmonary function impairment. Patients who resume interferon treatment should be closely monitored.
Colitis
Ulcerative and hemorrhagic/ischemic colitis, sometimes fatal, have been observed within 12 weeks of starting alpha interferon treatment. Abdominal pain, bloody diarrhea, and fever are the typical manifestations of colitis. PEGASYS should be discontinued immediately if these symptoms develop. The colitis usually resolves within 1 to 3 weeks of discontinuation of alpha interferon.
Pancreatitis
Pancreatitis, sometimes fatal, has occurred during alpha interferon and ribavirin treatment. PEGASYS and COPEGUS should be suspended if symptoms or signs suggestive of pancreatitis are observed. PEGASYS and COPEGUS should be discontinued in patients diagnosed with pancreatitis.
Ophthalmologic Disorders
Decrease or loss of vision, retinopathy including macular edema, retinal artery or vein thrombosis, retinal hemorrhages and cotton wool spots, optic neuritis, papilledema and serous retinal detachment are induced or aggravated by treatment with PEGASYS or other alpha interferons. All patients should receive an eye examination at baseline. Patients with pre-existing ophthalmologic disorders (e.g., diabetic or hypertensive retinopathy) should receive periodic ophthalmologic exams during interferon alpha treatment. Any patient who develops ocular symptoms should receive a prompt and complete eye examination. PEGASYS treatment should be discontinued in patients who develop new or worsening ophthalmologic disorders.
Pregnancy: Use with Ribavirin (also, see COPEGUS Package Insert)
Ribavirin may cause birth defects and/or death of the exposed fetus. Extreme care must be taken to avoid pregnancy in female patients and in female partners of male patients taking PEGASYS and COPEGUS combination therapy. COPEGUS THERAPY SHOULD NOT BE STARTED UNLESS A REPORT OF A NEGATIVE PREGNANCY TEST HAS BEEN OBTAINED IMMEDIATELY PRIOR TO INITIATION OF THERAPY. Women of childbearing potential and men must use two forms of effective contraception during treatment and for at least 6 months after treatment has concluded. Routine monthly pregnancy tests must be performed during this time (see BOXED WARNING, CONTRAINDICATIONS, PRECAUTIONS: Information for Patients, and COPEGUS Package Insert).
Anemia
The primary toxicity of ribavirin is hemolytic anemia. Hemoglobin <10 g/dL was observed in approximately 13% of COPEGUS and PEGASYS treated patients in chronic hepatitis C clinical trials (see PRECAUTIONS: Laboratory Tests). The anemia associated with COPEGUS occurs within 1 to 2 weeks of initiation of therapy with maximum drop in hemoglobin observed during the first eight weeks. BECAUSE THE INITIAL DROP IN HEMOGLOBIN MAY BE SIGNIFICANT, IT IS ADVISED THAT HEMOGLOBIN OR HEMATOCRIT BE OBTAINED PRE-TREATMENT AND AT WEEK 2 AND WEEK 4 OF THERAPY OR MORE FREQUENTLY IF CLINICALLY INDICATED. Patients should then be followed as clinically appropriate.
Fatal and nonfatal myocardial infarctions have been reported in patients with anemia caused by ribavirin. Patients should be assessed for underlying cardiac disease before initiation of ribavirin therapy. Patients with pre-existing cardiac disease should have electrocardiograms administered before treatment, and should be appropriately monitored during therapy. If there is any deterioration of cardiovascular status, therapy should be suspended or discontinued (see DOSAGE AND ADMINISTRATION: COPEGUS Dosage Modification Guidelines). Because cardiac disease may be worsened by drug-induced anemia, patients with a history of significant or unstable cardiac disease should not use COPEGUS (see COPEGUS Package Insert).
Renal
It is recommended that renal function be evaluated in all patients started on COPEGUS. COPEGUS should not be administered to patients with creatinine clearance <50 mL/min (see CLINICAL PHARMACOLOGY: Special Populations).
Peripheral Neuropathy
Peripheral neuropathy has been reported when alpha interferons were given in combination with telbivudine. In one clinical trial, an increased risk and severity of peripheral neuropathy was observed with the combination use of telbivudine and pegylated interferon-alfa 2a as compared to telbivudine alone. The safety and efficacy of telbivudine in combination with interferons for the treatment of chronic hepatitis B has not been demonstrated.
PRECAUTIONS
General
The safety and efficacy of PEGASYS alone or in combination with COPEGUS have not been established in:
- Patients who have failed alpha interferon treatment with or without ribavirin
- Liver or other organ transplant recipients
- Hepatitis B patients coinfected with HCV or HIV
- Hepatitis C patients coinfected with HBV or coinfected with HIV with a CD4+ cell count <100 cells/µL
Caution should be exercised in initiating treatment in any patient with baseline risk of severe anemia (e.g., spherocytosis, history of GI bleeding).
Renal Impairment
A 25% to 45% higher exposure to PEGASYS is seen in subjects undergoing hemodialysis. In patients with impaired renal function, signs and symptoms of interferon toxicity should be closely monitored. Doses of PEGASYS should be adjusted accordingly. PEGASYS should be used with caution in patients with creatinine clearance <50 mL/min (see DOSAGE AND ADMINISTRATION: Dose Modifications).
COPEGUS should not be used in patients with creatinine clearance <50 mL/min (see COPEGUS Package Insert).
Information for Patients
Patients receiving PEGASYS alone or in combination with COPEGUS should be directed in its appropriate use, informed of the benefits and risks associated with treatment, and referred to the PEGASYS and, if applicable, COPEGUS (ribavirin) MEDICATION GUIDES.
PEGASYS and COPEGUS combination therapy must not be used by women who are pregnant or by men whose female partners are pregnant. COPEGUS therapy should not be initiated until a report of a negative pregnancy test has been obtained immediately before starting therapy. Female patients of childbearing potential and male patients with female partners of childbearing potential must be advised of the teratogenic/embryocidal risks and must be instructed to practice effective contraception during COPEGUS therapy and for 6 months post-therapy. Patients should be advised to notify the healthcare provider immediately in the event of a pregnancy (see CONTRAINDICATIONS and WARNINGS).
Women of childbearing potential and men must use two forms of effective contraception during treatment and during the 6 months after treatment has been stopped; routine monthly pregnancy tests must be performed during this time (see CONTRAINDICATIONS and COPEGUS Package Insert).
To monitor maternal and fetal outcomes of pregnant women exposed to COPEGUS, the Ribavirin Pregnancy Registry has been established. Patients should be encouraged to register by calling 1-800-593-2214.
Patients should be advised that laboratory evaluations are required before starting therapy and periodically thereafter (see Laboratory Tests). Patients should be instructed to remain well hydrated, especially during the initial stages of treatment. Patients should be advised to take COPEGUS with food.
Patients should be informed that it is not known if therapy with PEGASYS alone or in combination with COPEGUS will prevent transmission of HCV or HBV infection to others or prevent cirrhosis, liver failure or liver cancer that might result from HCV or HBV infection. Patients who develop dizziness, confusion, somnolence, and fatigue should be cautioned to avoid driving or operating machinery.
If home use is prescribed, a puncture-resistant container for the disposal of used needles and syringes should be supplied to the patients. Patients should be thoroughly instructed in the importance of proper disposal and cautioned against any reuse of any needles and syringes. The full container should be disposed of according to the directions provided by the physician (see MEDICATION GUIDE).
Laboratory Tests
Before beginning PEGASYS or PEGASYS and COPEGUS combination therapy, standard hematological and biochemical laboratory tests are recommended for all patients. Pregnancy screening for women of childbearing potential must be performed.
After initiation of therapy, hematological tests should be performed at 2 weeks and 4 weeks and biochemical tests should be performed at 4 weeks. Additional testing should be performed periodically during therapy. In the clinical studies, the CBC (including hemoglobin level and white blood cell and platelet counts) and chemistries (including liver function tests and uric acid) were measured at 1, 2, 4, 6, and 8 weeks, and then every 4 to 6 weeks or more frequently if abnormalities were found. Thyroid stimulating hormone (TSH) was measured every 12 weeks. Monthly pregnancy testing should be performed during combination therapy and for 6 months after discontinuing therapy.
The entrance criteria used for the clinical studies of PEGASYS may be considered as a guideline to acceptable baseline values for initiation of treatment:
- Platelet count ≥90,000 cells/mm3 (as low as 75,000 cells/mm3 in HCV patients with cirrhosis or 70,000 cells/mm3 in patients with CHC and HIV)
- Absolute neutrophil count (ANC) ≥1500 cells/mm3
- Serum creatinine concentration <1.5 × upper limit of normal
- TSH and T4 within normal limits or adequately controlled thyroid function
- CD4+ cell count ≥200 cells/µL or CD4+ cell count ≥100 cells/µL but <200 cells/µL and HIV-1 RNA <5000 copies/mL in patients coinfected with HIV
- Hemoglobin ≥12 g/dL for women and ≥13 g/dL for men in CHC monoinfected patients
- Hemoglobin ≥11 g/dL for women and ≥12 g/dL for men in patients with CHC and HIV
PEGASYS treatment was associated with decreases in WBC, ANC, lymphocytes, and platelet counts often starting within the first 2 weeks of treatment (see ADVERSE REACTIONS). Dose reduction is recommended in patients with hematologic abnormalities (see DOSAGE AND ADMINISTRATION: Dose Modifications).
While fever is commonly caused by PEGASYS therapy, other causes of persistent fever must be ruled out, particularly in patients with neutropenia (see WARNINGS: Infections).
In chronic hepatitis C, transient elevations in ALT (2-fold to 5-fold above baseline) were observed in some patients receiving PEGASYS, and were not associated with deterioration of other liver function tests. When the increase in ALT levels is progressive despite dose reduction or is accompanied by increased bilirubin, PEGASYS therapy should be discontinued (see DOSAGE AND ADMINISTRATION: Dose Modifications).
Unlike hepatitis C, during hepatitis B therapy and follow up, transient elevations in ALT of 5 to 10 × ULN were observed in 25% and 27% and of >10 × ULN were observed in 12% and 18%, of HBeAg negative and HBeAg positive patients, respectively. These ALT elevations have been accompanied by other liver test abnormalities (see WARNINGS: Hepatic Failure and Hepatitis Exacerbations and DOSAGE AND ADMINISTRATION: Dose Modifications).
Drug Interactions
Theophylline
Treatment with PEGASYS once weekly for 4 weeks in healthy subjects was associated with an inhibition of P450 1A2 and a 25% increase in theophylline AUC. Theophylline serum levels should be monitored and appropriate dose adjustments considered for patients given both theophylline and PEGASYS (see CLINICAL PHARMACOLOGY: Drug Interactions).
Methadone
In a PK study of HCV patients concomitantly receiving methadone, treatment with PEGASYS once weekly for 4 weeks was associated with methadone levels that were 10% to 15% higher than at baseline (see CLINICAL PHARMACOLOGY: Drug Interactions). The clinical significance of this finding is unknown; however, patients should be monitored for the signs and symptoms of methadone toxicity.
Nucleoside Analogues
NRTIs
In Study 6 among the CHC/HIV coinfected cirrhotic patients receiving NRTIs cases of hepatic decompensation (some fatal) were observed (see WARNINGS: Hepatic Failure and Hepatitis Exacerbations).
Patients receiving PEGASYS/COPEGUS and NRTIs should be closely monitored for treatment associated toxicities. Physicians should refer to prescribing information for the respective NRTIs for guidance regarding toxicity management. In addition, dose reduction or discontinuation of PEGASYS, COPEGUS or both should also be considered if worsening toxicities are observed (see WARNINGS, PRECAUTIONS, DOSAGE AND ADMINISTRATION: Dose Modifications).
Didanosine
Co-administration of COPEGUS and didanosine is not recommended. Reports of fatal hepatic failure, as well as peripheral neuropathy, pancreatitis, and symptomatic hyperlactatemia/lactic acidosis have been reported in clinical trials (see CLINICAL PHARMACOLOGY: Drug Interactions).
Zidovudine
In Study 6, patients who were administered zidovudine in combination with PEGASYS/COPEGUS developed severe neutropenia (ANC <500) and severe anemia (hemoglobin <8 g/dL) more frequently than similar patients not receiving zidovudine (neutropenia 15% vs. 9%) (anemia 5% vs. 1%). Discontinuation of zidovudine should be considered as medically appropriate. Dose reduction or discontinuation of PEGASYS, COPEGUS or both should also be considered if worsening clinical toxicities are observed, including hepatic decompensation (e.g., Child-Pugh > 6).
Lamivudine, Stavudine, and Zidovudine
In vitro studies have shown ribavirin can reduce the phosphorylation of pyrimidine nucleoside analogs such as lamivudine, stavudine, and zidovudine. No evidence of a pharmacokinetic or pharmacodynamic interaction was seen when ribavirin was co-administered with lamivudine, stavudine, and/or zidovudine in HIV/HCV coinfected patients (see CLINICAL PHARMACOLOGY: Drug Interactions).
Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
PEGASYS has not been tested for its carcinogenic potential.
Mutagenesis
PEGASYS did not cause DNA damage when tested in the Ames bacterial mutagenicity assay and in the in vitro chromosomal aberration assay in human lymphocytes, either in the presence or absence of metabolic activation.
Use with Ribavirin
Ribavirin is genotoxic and mutagenic. The carcinogenic potential of ribavirin has not been fully determined. In a p53 (+/-) mouse carcinogenicity study at doses up to the maximum tolerated dose of 100 mg/kg/day ribavirin was not oncogenic. However, on a body surface area basis, this dose was 0.5 times maximum recommended human 24-hour dose of ribavirin. A study in rats to assess the carcinogenic potential of ribavirin is ongoing (see COPEGUS Package Insert).
Impairment of Fertility
PEGASYS may impair fertility in women. Prolonged menstrual cycles and/or amenorrhea were observed in female cynomolgus monkeys given sc injections of 600 µg/kg/dose (7200 µg/m2/dose) of PEGASYS every other day for one month, at approximately 180 times the recommended weekly human dose for a 60 kg person (based on body surface area). Menstrual cycle irregularities were accompanied by both a decrease and delay in the peak 17β-estradiol and progesterone levels following administration of PEGASYS to female monkeys. A return to normal menstrual rhythm followed cessation of treatment. Every other day dosing with 100 µg/kg (1200 µg/m2) PEGASYS (equivalent to approximately 30 times the recommended human dose) had no effects on cycle duration or reproductive hormone status.
The effects of PEGASYS on male fertility have not been studied. However, no adverse effects on fertility were observed in male Rhesus monkeys treated with non-pegylated interferon alfa-2a for 5 months at doses up to 25 × 106 IU/kg/day.
Use with Ribavirin
Ribavirin has shown reversible toxicity in animal studies of male fertility (see COPEGUS Package Insert).
Pregnancy
Pregnancy: Category C
PEGASYS has not been studied for its teratogenic effect. Non-pegylated interferon alfa-2a treatment of pregnant Rhesus monkeys at approximately 20 to 500 times the human weekly dose resulted in a statistically significant increase in abortions. No teratogenic effects were seen in the offspring delivered at term. PEGASYS should be assumed to have abortifacient potential. There are no adequate and well-controlled studies of PEGASYS in pregnant women. PEGASYS is to be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. PEGASYS is recommended for use in women of childbearing potential only when they are using effective contraception during therapy.
Pregnancy: Category X:
Use With Ribavirin (see CONTRAINDICATIONS)
Significant teratogenic and/or embryocidal effects have been demonstrated in all animal species exposed to ribavirin. COPEGUS therapy is contraindicated in women who are pregnant and in the male partners of women who are pregnant (see CONTRAINDICATIONS, WARNINGS, and COPEGUS Package Insert).
Ribavirin Pregnancy Registry
A Ribavirin Pregnancy Registry has been established to monitor maternal and fetal outcomes of pregnancies of female patients and female partners of male patients exposed to ribavirin during treatment and for 6 months following cessation of treatment. Healthcare providers and patients are encouraged to report such cases by calling 1-800-593-2214.
Nursing Mothers
It is not known whether peginterferon or ribavirin or its components are excreted in human milk. The effect of orally ingested peginterferon or ribavirin from breast milk on the nursing infant has not been evaluated. Because of the potential for adverse reactions from the drugs in nursing infants, a decision must be made whether to discontinue nursing or discontinue PEGASYS and COPEGUS treatment.
Pediatric Use
The safety and effectiveness of PEGASYS, alone or in combination with COPEGUS in patients below the age of 18 years have not been established.
PEGASYS contains benzyl alcohol. Benzyl alcohol has been reported to be associated with an increased incidence of neurological and other complications in neonates and infants, which are sometimes fatal (see CONTRAINDICATIONS).
Geriatric Use
Younger patients have higher virologic response rates than older patients. Clinical studies of PEGASYS alone or in combination with COPEGUS did not include sufficient numbers of subjects aged 65 or over to determine whether they respond differently from younger subjects. Adverse reactions related to alpha interferons, such as CNS, cardiac, and systemic (e.g., flu-like) effects may be more severe in the elderly and caution should be exercised in the use of PEGASYS in this population. PEGASYS and COPEGUS are excreted by the kidney, and the risk of toxic reactions to this therapy may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection and it may be useful to monitor renal function. PEGASYS should be used with caution in patients with creatinine clearance <50 mL/min and COPEGUS should not be administered to patients with creatinine clearance <50 mL/min.
ADVERSE REACTIONS
PEGASYS alone or in combination with COPEGUS causes a broad variety of serious adverse reactions (see BOXED WARNING and WARNINGS). The most common life-threatening or fatal events induced or aggravated by PEGASYS and COPEGUS were depression, suicide, relapse of drug abuse/overdose, and bacterial infections, each occurring at a frequency of <1%. Hepatic decompensation occurred in 2% (10/574) of CHC/HIV patients (see WARNINGS: Hepatic Failure and Hepatitis Exacerbations).
In all hepatitis C studies, one or more serious adverse reactions occurred in 10% of CHC monoinfected patients and in 19% of CHC/HIV patients receiving PEGASYS alone or in combination with COPEGUS. The most common serious adverse event (3% in CHC and 5% in CHC/HIV) was bacterial infection (e.g., sepsis, osteomyelitis, endocarditis, pyelonephritis, pneumonia). Other SAEs occurred at a frequency of <1% and included: suicide, suicidal ideation, psychosis, aggression, anxiety, drug abuse and drug overdose, angina, hepatic dysfunction, fatty liver, cholangitis, arrhythmia, diabetes mellitus, autoimmune phenomena (e.g., hyperthyroidism, hypothyroidism, sarcoidosis, systemic lupus erythematosus, rheumatoid arthritis), peripheral neuropathy, aplastic anemia, peptic ulcer, gastrointestinal bleeding, pancreatitis, colitis, corneal ulcer, pulmonary embolism, coma, myositis, cerebral hemorrhage, thrombotic thrombocytopenic purpura, psychotic disorder, and hallucination.
Nearly all patients in clinical trials experienced one or more adverse events. For hepatitis C patients, the most commonly reported adverse reactions were psychiatric reactions, including depression, insomnia, irritability, anxiety, and flu-like symptoms such as fatigue, pyrexia, myalgia, headache, and rigors. Other common reactions were anorexia, nausea and vomiting, diarrhea, arthralgias, injection site reactions, alopecia, and pruritus.
Overall 11% of CHC monoinfected patients receiving 48 weeks of therapy with PEGASYS either alone or in combination with COPEGUS discontinued therapy; 16% of CHC/HIV coinfected patients discontinued therapy. The most common reasons for discontinuation of therapy were psychiatric, flu-like syndrome (e.g., lethargy, fatigue, headache), dermatologic, and gastrointestinal disorders and laboratory abnormalities (thrombocytopenia, neutropenia, and anemia).
Overall 39% of patients with CHC or CHC/HIV required modification of PEGASYS and/or COPEGUS therapy. The most common reason for dose modification of PEGASYS in CHC and CHC/HIV patients was for laboratory abnormalities, neutropenia (20% and 27%, respectively) and thrombocytopenia (4% and 6%, respectively). The most common reason for dose modification of COPEGUS in CHC and CHC/HIV patients was anemia (22% and 16%, respectively).
PEGASYS dose was reduced in 12% of patients receiving 1000 mg to 1200 mg COPEGUS for 48 weeks and in 7% of patients receiving 800 mg COPEGUS for 24 weeks. COPEGUS dose was reduced in 21% of patients receiving 1000 mg to 1200 mg COPEGUS for 48 weeks and in 12% of patients receiving 800 mg COPEGUS for 24 weeks.
Chronic hepatitis C monoinfected patients treated for 24 weeks with PEGASYS and 800 mg COPEGUS were observed to have lower incidence of serious adverse events (3% vs. 10%), Hgb <10 g/dL (3% vs. 15%), dose modification of PEGASYS (30% vs. 36%) and COPEGUS (19% vs. 38%) and of withdrawal from treatment (5% vs. 15%) compared to patients treated for 48 weeks with PEGASYS and 1000 mg or 1200 mg COPEGUS. On the other hand the overall incidence of adverse events appeared to be similar in the two treatment groups.
Because clinical trials are conducted under widely varying and controlled conditions, adverse reaction rates observed in clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug. Also, the adverse event rates listed here may not predict the rates observed in a broader patient population in clinical practice.
| CHC Monotherapy (Pooled Studies 1-3) | CHC Combination Therapy Study 4 | |||
|---|---|---|---|---|
| Body System | PEGASYS 180 µg 48 week* | ROFERON-A†* | PEGASYS 180 µg + 1000 mg or 1200 mg COPEGUS 48 week‡ | Intron® A + 1000 mg or 1200 mg Rebetol® 48 week‡ |
| N=559 | N=554 | N=451 | N=443 | |
| % | % | % | % | |
| Application Site Disorders | ||||
| Injection site reaction | 22 | 18 | 23 | 16 |
| Endocrine Disorders | ||||
| Hypothyroidism | 3 | 2 | 4 | 5 |
| Flu-like Symptoms and Signs | ||||
| Fatigue/Asthenia | 56 | 57 | 65 | 68 |
| Pyrexia | 37 | 41 | 41 | 55 |
| Rigors | 35 | 44 | 25 | 37 |
| Pain | 11 | 12 | 10 | 9 |
| Gastrointestinal | ||||
| Nausea/Vomiting | 24 | 33 | 25 | 29 |
| Diarrhea | 16 | 16 | 11 | 10 |
| Abdominal pain | 15 | 15 | 8 | 9 |
| Dry mouth | 6 | 3 | 4 | 7 |
| Dyspepsia | <1 | 1 | 6 | 5 |
| Hematologic § | ||||
| Lymphopenia | 3 | 5 | 14 | 12 |
| Anemia | 2 | 1 | 11 | 11 |
| Neutropenia | 21 | 8 | 27 | 8 |
| Thrombocytopenia | 5 | 2 | 5 | <1 |
| Metabolic and Nutritional | ||||
| Anorexia | 17 | 17 | 24 | 26 |
| Weight decrease | 4 | 3 | 10 | 10 |
| Musculoskeletal, Connective Tissue and Bone | ||||
| Myalgia | 37 | 38 | 40 | 49 |
| Arthralgia | 28 | 29 | 22 | 23 |
| Back pain | 9 | 10 | 5 | 5 |
| Neurological | ||||
| Headache | 54 | 58 | 43 | 49 |
| Dizziness (excluding vertigo) | 16 | 12 | 14 | 14 |
| Memory impairment | 5 | 4 | 6 | 5 |
| Resistance Mechanism Disorders | ||||
| Overall | 10 | 6 | 12 | 10 |
| Psychiatric | ||||
| Irritability/Anxiety/ | 19 | 22 | 33 | 38 |
| Nervousness | ||||
| Insomnia | 19 | 23 | 30 | 37 |
| Depression | 18 | 19 | 20 | 28 |
| Concentration impairment | 8 | 10 | 10 | 13 |
| Mood alteration | 3 | 2 | 5 | 6 |
| Respiratory, Thoracic and Mediastinal | ||||
| Dyspnea | 4 | 2 | 13 | 14 |
| Cough | 4 | 3 | 10 | 7 |
| Dyspnea exertional | <1 | <1 | 4 | 7 |
| Skin and Subcutaneous Tissue | ||||
| Alopecia | 23 | 30 | 28 | 33 |
| Pruritus | 12 | 8 | 19 | 18 |
| Dermatitis | 8 | 3 | 16 | 13 |
| Dry skin | 4 | 3 | 10 | 13 |
| Rash | 5 | 4 | 8 | 5 |
| Sweating increased | 6 | 7 | 6 | 5 |
| Eczema | 1 | 1 | 5 | 4 |
| Visual Disorders | ||||
| Vision blurred | 4 | 2 | 5 | 2 |
CHC With HIV Coinfection
The adverse event profile of coinfected patients treated with PEGASYS and COPEGUS in Study 6 was generally similar to that shown for monoinfected patients in Study 4 (Table 6). Events occurring more frequently in coinfected patients were neutropenia (40%), anemia (14%), thrombocytopenia (8%), weight decrease (16%), and mood alteration (9%).
Chronic Hepatitis B
In clinical trials of 48 week treatment duration, the adverse event profile of PEGASYS in chronic hepatitis B was similar to that seen in chronic hepatitis C PEGASYS monotherapy use, except for exacerbations of hepatitis (see WARNINGS: Hepatic Failure and Hepatitis Exacerbations). Six percent of PEGASYS treated patients in the hepatitis B studies experienced one or more serious adverse events.
The most common or important serious adverse events in the hepatitis B studies were infections (sepsis, appendicitis, tuberculosis, influenza), hepatitis B flares, anaphylactic shock, thrombotic thrombocytopenic purpura.
The most commonly observed adverse reactions were pyrexia (54% vs. 4%), headache (27% vs. 9%), fatigue (24% vs. 10%), myalgia (26% vs. 4%), alopecia (18% vs. 2%), and anorexia (16% vs. 3%) in the PEGASYS and lamivudine groups respectively.
Overall 5% of hepatitis B patients discontinued PEGASYS therapy and 40% of patients required modification of PEGASYS dose. The most common reason for dose modification in patients receiving PEGASYS therapy was for laboratory abnormalities including neutropenia (20%), thrombocytopenia (13%), and ALT disorders (11%).
Laboratory Test Values
The laboratory test values observed in the hepatitis B trials (except where noted below) were similar to those seen in the PEGASYS monotherapy hepatitis C trials.
Neutrophils
In the hepatitis C studies, decreases in neutrophil count below normal were observed in 95% of all patients treated with PEGASYS either alone or in combination with COPEGUS. Severe potentially life-threatening neutropenia (ANC <0.5 × 109/L) occurred in 5% of CHC patients and 12% of CHC/HIV patients receiving PEGASYS either alone or in combination with COPEGUS. Modification of PEGASYS dose for neutropenia occurred in 17% of patients receiving PEGASYS monotherapy and 22% of patients receiving PEGASYS/COPEGUS combination therapy. In the CHC/HIV patients 27% required modification of interferon dosage for neutropenia. Two percent of patients with CHC and 10% of patients with CHC/HIV required permanent reductions of PEGASYS dosage and <1% required permanent discontinuation. Median neutrophil counts return to pre-treatment levels 4 weeks after cessation of therapy (see DOSAGE AND ADMINISTRATION: Dose Modifications).
Lymphocytes
Decreases in lymphocyte count are induced by interferon alpha therapy. PEGASYS plus COPEGUS combination therapy induced decreases in median total lymphocyte counts (56% in CHC and 40% in CHC/HIV, with median decrease of 1170 cells/mm3 in CHC and 800 cells/mm3 in CHC/HIV). In the hepatitis C studies, lymphopenia was observed during both monotherapy (81%) and combination therapy with PEGASYS and COPEGUS (91%). Severe lymphopenia (<0.5 × 109/L) occurred in approximately 5% of all monotherapy patients and 14% of all combination PEGASYS and COPEGUS therapy recipients. Dose adjustments were not required by protocol. The clinical significance of the lymphopenia is not known.
In CHC with HIV coinfection, CD4 counts decreased by 29% from baseline (median decrease of 137 cells/mm3) and CD8 counts decreased by 44% from baseline (median decrease of 389 cells/mm3) in the PEGASYS plus COPEGUS combination therapy arm. Median lymphocyte CD4 and CD8 counts return to pre-treatment levels after 4 to 12 weeks of the cessation of therapy. CD4% did not decrease during treatment.
Platelets
In the hepatitis C studies, platelet counts decreased in 52% of CHC patients and 51% of CHC/HIV patients treated with PEGASYS alone (respectively median decrease of 41% and 35% from baseline), and in 33% of CHC patients and 47% of CHC/HIV patients receiving combination therapy with COPEGUS (median decrease of 30% from baseline). Moderate to severe thrombocytopenia (<50,000/mm3) was observed in 4% of CHC and 8% of CHC/HIV patients. Median platelet counts return to pre-treatment levels 4 weeks after the cessation of therapy.
Hemoglobin
In the hepatitis C studies, the hemoglobin concentration decreased below 12 g/dL in 17% (median Hgb reduction of 2.2 g/dL) of monotherapy and 52% (median Hgb reduction of 3.7 g/dL) of combination therapy patients. Severe anemia (Hgb <10 g/dL) was encountered in 13% of all patients receiving combination therapy and in 2% of CHC patients and 8% of CHC/HIV patients receiving PEGASYS monotherapy. Dose modification for anemia in COPEGUS recipients treated for 48 weeks occurred in 22% of CHC patients and 16% of CHC/HIV patients (see DOSAGE AND ADMINISTRATION: Dose Modifications).
Triglycerides
Triglyceride levels are elevated in patients receiving alfa interferon therapy and were elevated in the majority of patients participating in clinical studies receiving either PEGASYS alone or in combination with COPEGUS. Random levels ≥400 mg/dL were observed in about 20% of CHC patients. Severe elevations of triglycerides (>1000 mg/dL) occurred in 2% of CHC monoinfected patients.
In HCV/HIV coinfected patients, fasting levels ≥400 mg/dL were observed in up to 36% of patients receiving either PEGASYS alone or in combination with COPEGUS. Severe elevations of triglycerides (>1000 mg/dL) occurred in 7% of coinfected patients.
ALT Elevations
Chronic Hepatitis C
One percent of patients in the hepatitis C trials experienced marked elevations (5- to 10-fold above the upper limit of normal) in ALT levels during treatment and follow-up. These transaminase elevations were on occasion associated with hyperbilirubinemia and were managed by dose reduction or discontinuation of study treatment. Liver function test abnormalities were generally transient. One case was attributed to autoimmune hepatitis, which persisted beyond study medication discontinuation (see DOSAGE AND ADMINISTRATION: Dose Modifications).
Chronic Hepatitis B
Transient ALT elevations are common during hepatitis B therapy with PEGASYS. Twenty-five percent and 27% of patients experienced elevations of 5 to 10 × ULN and 12% and 18% had elevations of >10 × ULN during treatment of HBeAg negative and HBeAg positive disease, respectively. Flares have been accompanied by elevations of total bilirubin and alkaline phosphatase and less commonly with prolongation of PT and reduced albumin levels. Eleven percent of patients had dose modifications due to ALT flares and <1% of patients were withdrawn from treatment (see WARNINGS: Hepatic Failure and Hepatitis Exacerbations and DOSAGE AND ADMINISTRATION: Dose Modifications).
ALT flares of 5 to 10 × ULN occurred in 13% and 16% of patients, while ALT flares of >10 × ULN occurred in 7% and 12% of patients in HBeAg negative and HBeAg positive disease, respectively, after discontinuation of PEGASYS therapy.
Thyroid Function
PEGASYS alone or in combination with COPEGUS was associated with the development of abnormalities in thyroid laboratory values, some with associated clinical manifestations. In the hepatitis C studies, hypothyroidism or hyperthyroidism requiring treatment, dose modification or discontinuation occurred in 4% and 1% of PEGASYS treated patients and 4% and 2% of PEGASYS and COPEGUS treated patients, respectively. Approximately half of the patients, who developed thyroid abnormalities during PEGASYS treatment, still had abnormalities during the follow-up period (see PRECAUTIONS: Laboratory Tests).
Immunogenicity
Chronic Hepatitis C
Nine percent (71/834) of patients treated with PEGASYS with or without COPEGUS developed binding antibodies to interferon alfa-2a, as assessed by an ELISA assay. Three percent of patients (25/835) receiving PEGASYS with or without COPEGUS, developed low-titer neutralizing antibodies (using an assay with a sensitivity of 100 INU/mL).
Chronic Hepatitis B
Twenty-nine percent (42/143) of hepatitis B patients treated with PEGASYS for 24 weeks developed binding antibodies to interferon alfa-2a, as assessed by an ELISA assay. Thirteen percent of patients (19/143) receiving PEGASYS developed low-titer neutralizing antibodies (using an assay with a sensitivity of 100 INU/mL).
The clinical and pathological significance of the appearance of serum neutralizing antibodies is unknown. No apparent correlation of antibody development to clinical response or adverse events was observed. The percentage of patients whose test results were considered positive for antibodies is highly dependent on the sensitivity and specificity of the assays.
Additionally, the observed incidence of antibody positivity in these assays may be influenced by several factors including sample timing and handling, concomitant medications, and underlying disease. For these reasons, comparison of the incidence of antibodies to PEGASYS with the incidence of antibodies to other products may be misleading.
Postmarketing Experience
The following adverse reactions have been identified and reported during post-approval use of PEGASYS therapy: dehydration, hearing impairment, hearing loss, and serious skin reactions (see WARNINGS: Hypersensitivity). Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. Decisions to include these reactions in labeling are typically based on one or more of the following factors: (1) seriousness of the reaction, (2) frequency of reporting or (3) strength of causal connection to PEGASYS.
OVERDOSAGE
There is limited experience with overdosage. The maximum dose received by any patient was 7 times the intended dose of PEGASYS (180 µg/day for 7 days). There were no serious reactions attributed to overdosages. Weekly doses of up to 630 µg have been administered to patients with cancer. Dose-limiting toxicities were fatigue, elevated liver enzymes, neutropenia, and thrombocytopenia. There is no specific antidote for PEGASYS. Hemodialysis and peritoneal dialysis are not effective.
DOSAGE AND ADMINISTRATION
There are no safety and efficacy data on treatment of chronic hepatitis C or hepatitis B for longer than 48 weeks. For patients with hepatitis C, consideration should be given to discontinuing therapy after 12 to 24 weeks of therapy if the patient has failed to demonstrate an early virologic response defined as undetectable HCV RNA or at least a 2log10 reduction from baseline in HCV RNA titer by 12 weeks of therapy (see CLINICAL STUDIES).
A patient should self-inject PEGASYS only if the physician determines that it is appropriate and the patient agrees to medical follow-up as necessary and training in proper injection technique has been provided to him/her (see illustrated PEGASYS MEDICATION GUIDE for directions on injection site preparation and injection instructions).
PEGASYS should be inspected visually for particulate matter and discoloration before administration, and not used if particulate matter is visible or product is discolored. Vials and prefilled syringes with particulate matter or discoloration should be returned to the pharmacist.
Chronic Hepatitis C
PEGASYS Monotherapy
The recommended dose of PEGASYS monotherapy for chronic hepatitis C is 180 µg (1.0 mL vial or 0.5 mL prefilled syringe) once weekly for 48 weeks by subcutaneous administration in the abdomen or thigh.
PEGASYS and COPEGUS Combination Therapy
The recommended dose of PEGASYS when used in combination with ribavirin for chronic hepatitis C is 180 µg (1.0 mL vial or 0.5 mL prefilled syringe) once weekly. The recommended dose of COPEGUS and duration for PEGASYS/COPEGUS therapy is based on viral genotype (see Table 7).
The daily dose of COPEGUS is 800 mg to 1200 mg administered orally in two divided doses. The dose should be individualized to the patient depending on baseline disease characteristics (e.g., genotype), response to therapy, and tolerability of the regimen.
Since COPEGUS absorption increases when administered with a meal, patients are advised to take COPEGUS with food.
| Genotype | PEGASYS Dose | COPEGUS Dose | Duration |
|---|---|---|---|
| Genotypes 2 and 3 showed no increased response to treatment beyond 24 weeks (see Table 3). | |||
| Data on genotypes 5 and 6 are insufficient for dosing recommendations. | |||
| Genotypes 1, 4 | 180 µg | <75 kg = 1000 mg ≥75 kg = 1200 mg | 48 weeks 48 weeks |
| Genotypes 2, 3 | 180 µg | 800 mg | 24 weeks |
CHC with HIV Coinfection
PEGASYS Monotherapy
The recommended dose of PEGASYS monotherapy for chronic hepatitis C in patients coinfected with HIV is 180 µg (1.0 mL vial or 0.5 mL prefilled syringe) once weekly for 48 weeks by subcutaneous administration in the abdomen or thigh.
PEGASYS/COPEGUS Combination Therapy
The recommended dose when used in combination with ribavirin is PEGASYS 180 µg sc once weekly and COPEGUS 800 mg po daily given in two divided doses for a total of 48 weeks, regardless of genotype.
Since COPEGUS absorption increases when administered with a meal, patients are advised to take COPEGUS with food.
Chronic Hepatitis B
PEGASYS Monotherapy
The recommended dose of PEGASYS monotherapy for hepatitis B is 180 µg (1.0 mL vial or 0.5 mL prefilled syringe) once weekly for 48 weeks by subcutaneous administration in the abdomen or thigh.
Dose Modifications
If severe adverse reactions or laboratory abnormalities develop during combination COPEGUS/PEGASYS therapy, the dose should be modified or discontinued, if appropriate, until the adverse reactions abate. If intolerance persists after dose adjustment, COPEGUS/PEGASYS therapy should be discontinued.
PEGASYS
General
When dose modification is required for moderate to severe adverse reactions (clinical and/or laboratory), initial dose reduction to 135 µg (which is 0.75 mL for the vials or adjustment to the corresponding graduation mark for the syringes) is generally adequate. However, in some cases, dose reduction to 90 µg (which is 0.5 mL for the vials or adjustment to the corresponding graduation mark for the syringes) may be needed. Following improvement of the adverse reaction, re-escalation of the dose may be considered (see WARNINGS, PRECAUTIONS, and ADVERSE REACTIONS).
Hematological
| Laboratory Values | Reduce PEGASYS Dose to: | Discontinue PEGASYS if: |
|---|---|---|
| ANC ≥750/mm3
ANC <750/mm3 | Maintain 180 µg Reduce to 135 µg | ANC <500/mm3, treatment should be suspended until ANC values return to more than 1000/mm3
Reinstitute at 90 µg and monitor ANC |
| Platelet ≥50,000/mm3
Platelet <50,000/mm3 | Maintain 180 µg Reduce to 90 µg | Platelet count <25,000/mm3 |
Psychiatric: Depression
| Depression Severity | Initial Management (4-8 weeks) | Depression | |||
|---|---|---|---|---|---|
| Dose modification | Visit schedule | Remains stable | Improves | Worsens | |
| Mild | No change | Evaluate once weekly by visit and/or phone | Continue weekly visit schedule | Resume normal visit schedule | (See moderate or severe depression) |
| Moderate | Decrease PEGASYS dose to 135 µg (in some cases dose reduction to 90 µg may be needed) | Evaluate once weekly (office visit at least every other week) | Consider psychiatric consultation. Continue reduced dosing | If symptoms improve and are stable for 4 weeks, may resume normal visit schedule. Continue reduced dosing or return to normal dose | (See severe depression) |
| Severe | Discontinue PEGASYS permanently | Obtain immediate psychiatric consultation | Psychiatric therapy necessary | ||
Renal Function
In patients with end-stage renal disease requiring hemodialysis, dose reduction to 135 µg PEGASYS is recommended. Signs and symptoms of interferon toxicity should be closely monitored.
Liver Function
If ALT increases are progressive despite dose reduction or accompanied by increased bilirubin or evidence of hepatic decompensation, therapy should be immediately discontinued.
In chronic hepatitis C patients with progressive ALT increases above baseline values, the dose of PEGASYS should be reduced to 135 µg and more frequent monitoring of liver function should be performed. After PEGASYS dose reduction or withholding, therapy can be resumed after ALT flares subside.
In chronic hepatitis B patients with elevations in ALT (>5 × ULN), more frequent monitoring of liver function should be performed and consideration should be given to either reducing the dose of PEGASYS to 135 µg or temporarily discontinuing treatment. After PEGASYS dose reduction or withholding, therapy can be resumed after ALT flares subside.
In patients with persistent, severe (ALT >10 times above the upper limit of normal) hepatitis B flares, consideration should be given to discontinuation of treatment.
COPEGUS
| Laboratory Values | Reduce Only COPEGUS Dose to 600 mg/day* if: | Discontinue COPEGUS if: |
|---|---|---|
|
||
| Hemoglobin in patients with no cardiac disease | <10 g/dL | <8.5 g/dL |
| Hemoglobin in patients with history of stable cardiac disease | ≥2 g/dL decrease in hemoglobin during any 4 week period treatment | <12 g/dL despite 4 weeks at reduced dose |
Once COPEGUS has been withheld due to a laboratory abnormality or clinical manifestation, an attempt may be made to restart COPEGUS at 600 mg daily and further increase the dose to 800 mg daily depending upon the physician's judgment. However, it is not recommended that COPEGUS be increased to the original dose (1000 mg or 1200 mg).
Renal Impairment
COPEGUS should not be used in patients with creatinine clearance <50 mL/min (see CLINICAL PHARMACOLOGY, WARNINGS and COPEGUS Package Insert).
HOW SUPPLIED
Single Dose Vial
Each PEGASYS (peginterferon alfa-2a) 180 µg single use, clear glass vial provides 1.0 mL containing 180 µg peginterferon alfa-2a for sc injection. Each package contains 1 vial (NDC 0004-0350-09).
Prefilled Syringes Monthly Convenience Pack
Four prefilled syringes of PEGASYS (peginterferon alfa-2a), 180 µg single use, graduated, clear glass prefilled syringes, in a box with 4 needles and 4 alcohol swabs (NDC 0004-0352-39). Each syringe is a 0.5 mL (½ cc) volume syringe supplied with a 27-gauge, ½-inch needle with needle-stick protection device.
Storage
Store in the refrigerator at 2°C to 8°C (36°F to 46°F). Do not freeze or shake. Protect from light. Vials and prefilled syringes are for single use only. Discard any unused portion.
COPEGUS and PEGASYS are trademarks of Hoffmann-La Roche Inc.
PI Revised: January 2010
MEDICATION GUIDE
PEGASYS®
(peginterferon alfa-2a)
Before you start taking PEGASYS (PEG-ah-sis), alone or in combination with COPEGUS® (Co-PEG-UHS), please read this Medication Guide carefully. Read this Medication Guide each time you refill your prescription in case new information has been added and make sure the pharmacist has given you the medicine your healthcare provider prescribed for you. Reading the information in this Medication Guide does not take the place of talking with your healthcare provider.
If you are taking PEGASYS in combination with COPEGUS, you should also read the Medication Guide for COPEGUS (ribavirin, USP) Tablets.
What is the most important information I should know about PEGASYS therapy?
PEGASYS, taken alone or in combination with COPEGUS, is a treatment for some people who are infected with hepatitis C virus. PEGASYS taken alone is a treatment for some people who are infected with the hepatitis B virus. However, PEGASYS and COPEGUS can have serious side effects that may cause death in rare cases. Before starting PEGASYS therapy, you should talk with your healthcare provider about the possible benefits and the possible side effects of treatment, to decide if either of these treatments is right for you. If you begin treatment you will need to see your healthcare provider regularly for examinations and blood tests to make sure your treatment is working and to check for side effects.
The most serious possible side effects of PEGASYS taken alone or in combination with COPEGUS include:
Taking PEGASYS in combination with COPEGUS tablets can cause death, serious birth defects or other harm to your unborn child. Therefore, if you are pregnant or your partner is pregnant or plans to become pregnant, do not take PEGASYS/COPEGUS combination therapy. Female patients and female partners of male patients being treated with PEGASYS/COPEGUS combination therapy must not become pregnant during treatment and for 6 months after treatment has stopped. During this time, you must have pregnancy tests that show you are not pregnant. You must also use two effective forms of birth control during therapy and for 6 months after stopping therapy. Male patients should use a condom with spermicide as one of the two forms. You must use birth control even if you believe that you are not fertile or that your fertility is low. You should talk to your healthcare provider about birth control for you and your partner.
If you are pregnant, you or your male partner must not take PEGASYS/COPEGUS combination therapy. If you or your partner are being treated and you become pregnant either during treatment or within 6 months of stopping treatment, call your healthcare provider right away.
If you or a female sexual partner becomes pregnant, you should tell your healthcare provider. There is a Ribavirin Pregnancy Registry that collects information about pregnancy outcomes of female patients and female partners of male patients exposed to ribavirin. You or your healthcare provider are encouraged to contact the Registry at 1-800-593-2214.
Mental health problems and suicide:
PEGASYS and PEGASYS/COPEGUS combination therapy may cause some patients to develop mood or behavioral problems. Signs of these problems include irritability (getting easily upset), depression (feeling low, feeling bad about yourself or feeling hopeless), and anxiety. Some patients may have aggressive behavior. Former drug addicts may fall back into drug addiction or overdosage. Some patients think about hurting or killing themselves or other people and some have killed (suicide) or hurt themselves or hurt other people. You must tell your healthcare provider if you are being treated for a mental illness or have a history of mental illness, including depression and suicidal behavior or if you are or have ever been addicted to drugs or alcohol. Call your healthcare provider immediately if you develop any of these problems while on PEGASYS treatment.
Heart problems:
Some patients taking PEGASYS or PEGASYS/COPEGUS therapies may develop problems with their heart, including low blood pressure, fast heart rate, and very rarely, heart attacks. Tell your healthcare provider if you have had any heart problems in the past.
Blood problems:
Many patients taking PEGASYS have had a drop in the number of their white blood cells and their platelets. If the numbers of these blood cells are too low, you could be at risk for serious infections or bleeding.
COPEGUS causes a decrease in the number of your red blood cells (anemia). This can be dangerous, especially for patients who already have heart or circulatory (cardiovascular) problems. If you have or have ever had any cardiovascular problems, talk with your healthcare provider before taking the combination of PEGASYS and COPEGUS.
Liver problems:
Infrequently, some patients with hepatitis C and liver scarring can develop sudden severe worsening (failure) of their liver disease while taking PEGASYS. Patients infected with both the hepatitis C virus and HIV can have an increased chance of having liver failure during PEGASYS treatment.
Some patients taking PEGASYS for hepatitis B have had a rise in a blood test that measures liver inflammation. If you have a rise in this blood test, your liver may need to be watched more closely with additional blood tests.
Infections:
Some patients taking interferon have had serious infections. Sometimes these infections have been fatal. If you develop a fever that does not go away or gets higher, call your healthcare provider right away. Your healthcare provider will need to examine you to rule out your having a serious infection.
Eye problems:
Changes in vision such as a decrease or loss of vision (blindness) may happen in some patients. You should have an eye exam before you take PEGASYS. If you have eye problems or have had them in the past you may need eye exams while you are taking PEGASYS. Tell your healthcare provider or eye doctor right away if you have changes in your vision while taking PEGASYS.
Body organ problems:
PEGASYS may cause lung problems including: trouble breathing, pneumonia, inflammation of lung tissue, and new or worse high blood pressure in the lungs (pulmonary hypertension), which can be severe and may in some cases lead to death. Certain symptoms like severe stomach pain may mean that your internal organs are being damaged. Cases of weakness, loss of coordination and numbness due to stroke have been reported in patients taking PEGASYS/COPEGUS, including patients with few or no reported risk factors for stroke.
Call your healthcare provider immediately if you develop any of these conditions:
- You become very depressed, think about suicide or injuring/killing another person
- You have severe chest pain
- You have trouble breathing
- You have a change in your vision
- You become pregnant
- You notice unusual bleeding or bruising
- You have psoriasis (a skin disease) and it gets worse while taking PEGASYS
-
You have weakness, loss of coordination, numbness or difficulty speaking
- High fever or a fever that does not go away
- You have severe stomach pain or lower back pain
- Bloody diarrhea
- Skin rash can occur in patients taking PEGASYS. In some patients a rash can be serious. If you develop a rash with fever, blisters, or sores in your mouth, nose or eyes or conjunctivitis (red or inflamed eyes, like "pink eye"), stop using PEGASYS and call your doctor right away
For more information on possible side effects with PEGASYS therapy, alone or in combination with COPEGUS, please read the section on "What are the possible side effects of PEGASYS, and PEGASYS taken with COPEGUS?" in this Medication Guide. You should also read the Medication Guide for COPEGUS tablets if you are taking that medicine with PEGASYS.
What is PEGASYS?
PEGASYS is a drug used to treat adults who have a lasting (chronic) infection with hepatitis C virus or hepatitis B virus and who show signs that the virus is damaging the liver. Patients with hepatitis have the virus in their blood and in their liver. PEGASYS reduces the amount of hepatitis C virus in the body and helps the body's immune system fight the virus. The drug COPEGUS are tablets that may be taken with PEGASYS to help fight the virus infection. Do not take COPEGUS by itself.
In some patients that have received PEGASYS treatment for approximately one year to treat hepatitis C, the amount of the hepatitis virus in the body was decreased to a level so low that it could not be measured by blood tests. After 3 months of therapy, your healthcare provider may ask you to have a blood test to help determine how you are responding to your treatment.
It is not known if PEGASYS, used alone or in combination with COPEGUS, can cure hepatitis (permanently eliminate the virus) or if it can prevent liver failure or liver cancer that is caused by hepatitis infection.
It is also not known if PEGASYS, alone or in combination with COPEGUS, will prevent one infected person from infecting another person with hepatitis.
Who should not take PEGASYS, or PEGASYS with COPEGUS?
Do not take PEGASYS or PEGASYS/COPEGUS therapy if you:
- are pregnant, planning to get pregnant during treatment or during the 6 months after treatment or breast-feeding
- are a male patient with a female sexual partner who is pregnant or plans to become pregnant at any time while you are being treated with COPEGUS or during the 6 months after your treatment has ended
- have hepatitis caused by your immune system attacking your liver (autoimmune hepatitis)
- have unstable or severe liver disease
- had an allergic reaction to another alpha interferon or are allergic to any of the ingredients in PEGASYS or COPEGUS tablets
- Do not take PEGASYS, alone or in combination with COPEGUS, if you have abnormal red blood cells such as sickle-cell anemia or thalassemia major.
If you have ever had any of the following conditions or serious medical problems, tell your healthcare provider before you start taking PEGASYS:
- History of or current severe mental illness (such as depression or anxiety)
- History of drug or alcohol addiction or abuse
- History of heart disease or previous heart attack
- History of cancer
- Autoimmune disease (where the body's immune system attacks the body's own cells), such as psoriasis (a skin disease), systemic lupus erythematosus, rheumatoid arthritis
- Kidney problems
- Blood disorders (bleeding problems)
- Diabetes (high blood sugar)
- Problems with the thyroid gland
- Liver problems, other than hepatitis C or hepatitis B
- Colitis (an inflammation of the bowels)
-
Eye problems
-
Sleep problems
-
HIV infection
-
Organ transplant and are taking medicine that keeps your body from rejecting your transplant (suppresses your immune system)
Tell your healthcare provider about all the medicines you take, including prescription and non-prescription medicines, vitamins and herbal supplements. PEGASYS and certain other medicines may affect each other causing side effects.
Especially tell your healthcare provider if you take:
-
the anti-hepatitis B medicine telbivudine (Tyzeka). See "What are the possible side effects of PEGASYS?".
-
Theophylline: Your healthcare provider may need to monitor the amount of theophylline in your body and make changes to your theophylline dose.
-
HIV medications called nucleoside reverse transcriptase inhibitors (abacavir, didanosine, emtricitabine, lamivudine, tenofovir, stavudine or zidovudine). Some patients developed serious liver problems including death.
-
Didanosine: Do not take COPEGUS and didanosine.
If you have any questions about your health condition or about taking PEGASYS alone or in combination with COPEGUS, you should talk to your healthcare provider.
How should I take PEGASYS, or PEGASYS with COPEGUS?
PEGASYS is given by injection under the skin (subcutaneous injection). PEGASYS comes in two different forms (a liquid in a single use vial and a liquid in a prefilled syringe). Your healthcare provider will determine which is best for you. Your healthcare provider will also decide whether you will take PEGASYS alone or with COPEGUS. Your dose of PEGASYS is given as a single injection once per week. At some point, your healthcare provider may change your dose of PEGASYS or COPEGUS. Do not change your dose unless your healthcare provider tells you to change it. It is important that you take PEGASYS and COPEGUS exactly as your healthcare provider tells you. Once you start treatment with PEGASYS, do not switch to another brand of interferon without talking to your healthcare provider. Other interferons may not have the same effect on the treatment of your disease. Switching brands will also require a change in your dose.
Take your prescribed dose of PEGASYS once a week, on the same day of each week and at approximately the same time. Your total dose of COPEGUS tablets should be divided so you take it twice a day with food (breakfast and dinner). Taking half your dose of COPEGUS in the morning and the other half at night will keep the medicine in your body at a steady level. Do not take more than your prescribed dose of PEGASYS or COPEGUS. Be sure to read the Medication Guide for COPEGUS (ribavirin, USP) for complete instructions on how to take the COPEGUS tablets.
Your healthcare provider will train you and/or the person that will be giving you the PEGASYS injections on the proper way to give injections. Whether you give yourself the injection or another person gives the injection to you, it is important that you are comfortable with preparing and injecting a dose of PEGASYS, and you understand the instructions in "How do I inject PEGASYS?" At the end of this guide there are detailed instructions on how to prepare and give yourself an injection of PEGASYS using the form your healthcare provider has prescribed for you.
If you miss a dose and you remember within 2 days of when you should have taken PEGASYS, give yourself an injection of PEGASYS as soon as you remember. Take your next dose on the day you would usually take it. If more than 2 days have passed, ask your healthcare provider what you should do. If you miss a dose of COPEGUS, take the missed dose as soon as you remember during the same day. Do not take 2 doses too close together in time. If it is late in the day, wait until the next day and go back on schedule. Do not double the next dose.
If you take more than the prescribed amount of PEGASYS, call your healthcare provider right away. Your healthcare provider may want to examine you and take blood for testing.
You must get regular blood tests to help your healthcare provider check how the treatment is working and to check for side effects.
What should I avoid while taking PEGASYS, or PEGASYS with COPEGUS?
- If you are pregnant do not start taking or continue taking COPEGUS in combination with PEGASYS. (See "What is the most important information I should know about PEGASYS therapy? Problems with Pregnancy".)
- Avoid becoming pregnant while taking PEGASYS, alone or in combination with COPEGUS. PEGASYS, alone or in combination with COPEGUS, may harm your unborn child (death or serious birth defects) or cause you to lose your baby (miscarry). (See "What is the most important information I should know about PEGASYS therapy? Problems with Pregnancy".)
- Do not breast-feed your baby while on PEGASYS, alone or in combination with COPEGUS.
-
Drinking alcohol, including beer, wine and liquor. This may make your liver disease worse.
-
Taking other medicines. Take only medicines prescribed or approved by your healthcare provider. These include prescription and nonprescription medicines and herbal supplements.
What are the possible side effects of PEGASYS, and PEGASYS taken with COPEGUS?
Also see "What is the most important information I should know about PEGASYS therapy?" in this Medication Guide.
PEGASYS and PEGASYS/COPEGUS combination therapy can cause serious side effects including:
-
See "What is the most important information I should know about PEGASYS?".
-
Blood problems including anemia: Anemia is a reduction in the number of red blood cells you have, which can be dangerous, especially if you have heart or breathing problems. Tell your healthcare provider right away if you feel tired, have chest pain or shortness of breath. These may be signs of low red blood cell counts.
-
Serious infections.
-
Stroke: Some patients may experience weakness, loss of coordination, and numbness due to stroke.
-
Autoimmune problems: Some patients may develop a disease where the body's own immune system begins to attack itself (autoimmune disease) while on PEGASYS therapy. These diseases can include rheumatoid arthritis, systemic lupus erythematosus, psoriasis or thyroid problems. In some patients who already have an autoimmune disease, the disease may worsen while on PEGASYS therapy.
-
Heart problems: PEGASYS may cause some patients to experience chest pain, and very rarely a heart attack. Patients who already have heart disease could be at greatest risk. Tell your healthcare provider if you have or have had a heart problem in the past.
-
Liver problems: Some patients may develop worsening of liver function. Some of the symptoms may include stomach bloating, confusion, brown urine, and yellow eyes. Tell your healthcare provider immediately if any of these symptoms occur.
-
Nerve problems: People who take PEGASYS or other alpha interferon products with telbivudine (Tyzeka) can have nerve problems such as continuing numbness, tingling, or burning sensation in the arms or legs (peripheral neuropathy). Call your healthcare provider if you have any of these symptoms.
-
Harm to unborn children: PEGASYS and PEGASYS/COPEGUS may cause birth defects or death of an unborn child. For more details, see "What is the most important information I should know about PEGASYS therapy?" in this Medication Guide.
Common, but less serious, side effects include:
- Flu-like symptoms: Most patients who take PEGASYS have flu-like symptoms that usually lessen after the first few weeks of treatment. Flu-like symptoms may include fever, chills, muscle aches, joint pain, and headaches. Taking pain and fever reducers such as acetaminophen or ibuprofen before you take PEGASYS can help with these symptoms. You can also try taking PEGASYS at night. You may be able to sleep through the symptoms.
- Extreme fatigue (tiredness): Many patients may become extremely tired while on PEGASYS therapy.
- Upset stomach: Nausea, taste changes, diarrhea, and loss of appetite occur commonly.
- Blood sugar problems: Some patients may develop a problem with the way their body controls their blood sugar and may develop diabetes.
-
Thyroid problems: Some patients develop changes in the function of their thyroid. Symptoms of thyroid changes include the inability to concentrate, feeling cold or hot all the time, a change in your weight, and changes to your skin.
- Skin reactions: Some patients may develop redness, swelling, dry or itchy skin at the site of injection. If after several days these symptoms do not disappear, contact your healthcare provider. You may get a rash during therapy. If this occurs, your healthcare provider may recommend medicine to treat the rash.
- Hair thinning: Temporary hair loss is not uncommon during treatment with PEGASYS.
- Trouble sleeping
These are not all of the side effects of PEGASYS, and PEGASYS taken with COPEGUS. Your healthcare provider or pharmacist can give you a more complete list. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. You may also report side effects to Genentech at 1-888-835-2555.
Talk to your healthcare provider if you are worried about side effects or find them very bothersome.
General advice about prescription medicines
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. If you have any concerns or questions about PEGASYS, contact your healthcare provider. Do not use PEGASYS for a condition or person other than that for which it is prescribed. If you want to know more about PEGASYS, your healthcare provider or pharmacist will be able to provide you with detailed information that is written for healthcare providers.
If you are taking COPEGUS (ribavirin, USP) in combination with PEGASYS, also read the Medication Guide supplied with that medicine.
Keep this and all drugs out of the reach of children.
This Medication Guide has been approved by the US Food and Drug Administration.
MG Revised: January 2010
Medication Guide Appendix: Instructions for Preparing and Giving a Dose with a PEGASYS® Prefilled Syringe
How should I store PEGASYS Prefilled Syringes?
PEGASYS must be stored in the refrigerator at a temperature of 2°C to 8°C (36°F to 46°F). Do not leave PEGASYS outside of the refrigerator for more than 24 hours. Do not freeze PEGASYS. Keeping PEGASYS at temperatures outside the recommended range can destroy the medicine.
Each PEGASYS prefilled syringe can only be used once. Discard after use.
To avoid product foaming, do not shake the prefilled syringe of PEGASYS.
Protect PEGASYS from light during storage.
Keep this and all other medicines out of the reach of children.
How do I prepare and inject PEGASYS?
You should read through all of these directions and ask your healthcare provider for help if you have any questions before trying to give yourself an injection. It is important to follow these directions carefully. Talk to your healthcare provider if you have any questions about PEGASYS.
Your healthcare provider may not want you to take all the medicine that comes in the prefilled syringe. To appropriately administer the dose that your healthcare provider tells you to take, you may have to get rid of some of the medicine before injecting the medicine.
If you ever switch between using prefilled syringes and vials, talk to your healthcare provider about how much PEGASYS to use. Equal volumes of liquid from the prefilled syringes and the vials DO NOT contain the same amount of PEGASYS. If you switch between prefilled syringes and vials, you will have to adjust the volume of liquid that you use to give your injection. If you do not adjust this, you could accidentally take too much or too little of your medicine.
If you are giving this injection to someone else, a healthcare provider must teach you how to avoid needle sticks. Being stuck by a used needle can pass diseases on to you.
The prefilled syringes are used for injecting PEGASYS under the surface of the skin (subcutaneous).
-
Collect all the materials you will need before you start to give the injection:
- One PEGASYS prefilled syringe Monthly Convenience Pack containing an inner carton holding the PEGASYS prefilled syringe
- A puncture-resistant container for cleaning up when you are finished
-
Open the convenience pack and look at the contents.
- Each convenience pack has everything you need for the PEGASYS injection.
– 4 single use syringes filled with medicine (should be colorless to light yellow)
– four 27-gauge, ½-inch needles with needle-stick protection device
– 4 alcohol swabs
- Each convenience pack has everything you need for the PEGASYS injection.
-
Take the syringe out of the refrigerator. If there is foam in the solution, put it back in the refrigerator for use at a later time and use another syringe.
-
Lay the syringe on a flat clean surface and wait a few minutes until it reaches room temperature. If you notice condensation water on the outside of the syringe, wait another few minutes until it disappears.
-
Wash your hands with soap and warm water to prevent infection.
-
After the syringe has warmed up, pick it up by the glass barrel and look at it carefully.
- Do not use PEGASYS if:
– the medicine is cloudy
– the medicine has particles floating in it
– the medicine is any color besides colorless to light yellow
– the expiration date has passed
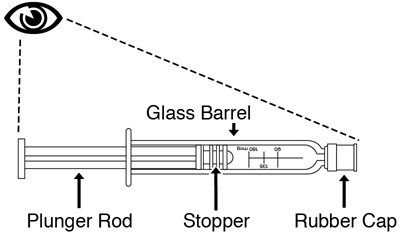
- Do not use PEGASYS if:
-
Attachment of the needle to the PEGASYS prefilled syringe:
-
Remove the needle from its package. Do not remove the needle shield yet. Keep the needle covered until just before you give the injection.
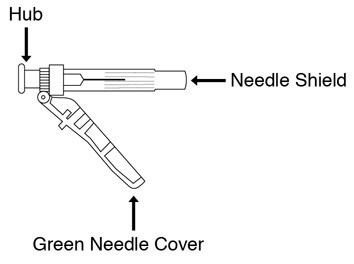
-
Remove and discard the rubber cap from the tip of the syringe barrel.
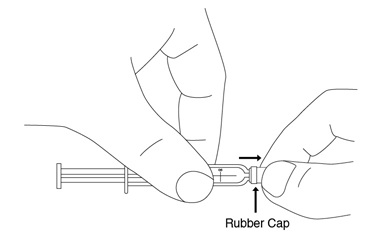
-
Hold the needle close to the hub where the green needle cover connects.
-
Put the needle onto the syringe by using an easy twisting motion to tighten the needle onto the syringe.
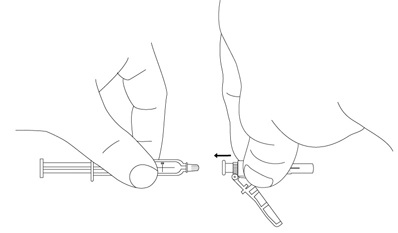
-
Here is a picture of the assembled syringe:
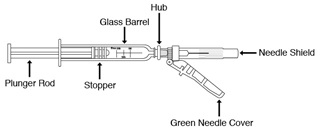
-
Keep the syringe in a horizontal position until ready for use.
-
If you need to set the syringe down, make sure the plastic needle shield covers the needle. Never let the needle touch any surface.
-
-
Decide where you will give the injection.
- Pick a place on your stomach or thigh (see the picture below). Avoid your navel and waistline. You should use a different place each time you give yourself an injection.
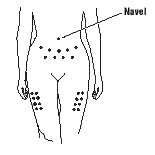
- Pick a place on your stomach or thigh (see the picture below). Avoid your navel and waistline. You should use a different place each time you give yourself an injection.
-
Prepare your skin for the injection.
- To minimize the discomfort from injections, you may want to gently tap the area where you plan to give yourself an injection.
- Clean the area using the alcohol pad. Let the skin dry for 10 seconds.
-
Prepare the syringe for injection.
- Pull the green needle cover back from the needle toward the syringe barrel. The green needle cover will remain in the position you set, do not remove it. This is the needle-stick protection device.
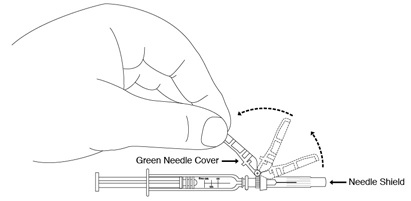
- Hold the syringe-needle assembly tightly at the hub.
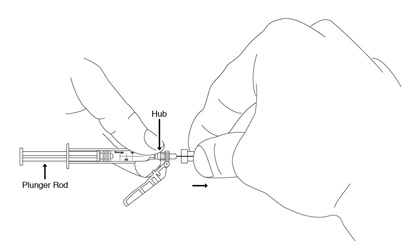
-
Remove the clear plastic needle shield covering the needle by pulling it straight off.
- Pull the green needle cover back from the needle toward the syringe barrel. The green needle cover will remain in the position you set, do not remove it. This is the needle-stick protection device.
-
Remove air bubbles from the syringe.
-
Hold the syringe with the needle pointing up to the ceiling.
-
If you see little bubbles, pull down slightly on the plunger rod.
-
Using your thumb and finger, gently tap the syringe to bring air bubbles to the top (small air bubbles may remain on the glass surface).
-
Press the plunger in slightly to push air bubbles out of the syringe.
-
If you find that there is still small air bubbles on glass surface after you push the air bubbles out, you can still give yourself the injection, the small air bubbles will not hurt you.
-
-
Dose adjustment.
-
Your healthcare provider may not want you to take all the medicine that comes in the prefilled syringe.
-
To appropriately administer the dose that your healthcare provider tells you to take, you may have to get rid of some of the medicine before injecting the medicine.
-
The syringe has markings for 180 mcg, 135 mcg, and 90 mcg. Your healthcare provider will tell you which mark to use.
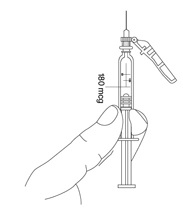
-
Once you know which mark to use, slowly and carefully press on the plunger rod of the syringe to push out medicine from the syringe. Keep pressing until the edge of the plunger stopper reaches the right mark on the side of the syringe.
-
Do not decrease or increase your dose of PEGASYS unless your healthcare provider tells you to.
-
-
Give the injection of PEGASYS.
-
Position the point of the needle (the bevel) so it is facing up.
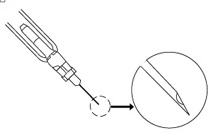
-
Pinch a fold of skin on your stomach or thigh firmly with your thumb and forefinger.

-
Hold the syringe like a pencil at a 45° to 90° angle to your skin. In one quick motion, insert the needle as far as it will go into the pinched area of skin. Pull the plunger of the syringe back very slightly. If blood comes into the syringe, the needle has entered a blood vessel. Do not inject. Withdraw the needle and discard the syringe as outlined in step 14. Repeat the above steps with a new prefilled syringe and prepare a new site.
-
If no blood appears, release your skin and slowly push the plunger all the way down so that you get all of your medicine.

-
Pull out the needle at same angle you put it in.
-
Wipe the area with an alcohol swab.
-
-
For safety reasons, before you dispose of the syringe and needle, push the green needle cover toward the needle. Then place the free end of the green cap on a flat surface and push down on it until it clicks and covers over the needle. Always place used syringes and needles in a puncture-resistant container immediately after use and never reuse them. Keep your disposal container out of the reach of children.
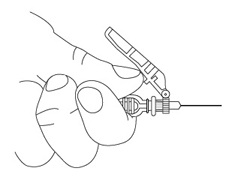
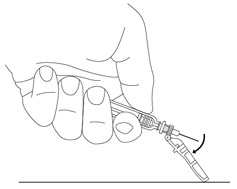
How should I dispose of materials used to inject PEGASYS?
There may be special state and local laws for disposal of used needles and syringes. Your healthcare provider or pharmacist should provide you with instructions on how to properly dispose of your used syringes and needles. Always follow these instructions.
The instructions below should be used as a general guide for proper disposal:
- The needles and syringes should never be reused.
- Place all used needles and syringes in a puncture-proof disposable container that is available through your pharmacy or healthcare provider (Sharp's container).
- DO NOT use glass or clear plastic containers for disposal of needles and syringes.
- Dispose of the full container as instructed by your healthcare provider or pharmacist.
DO NOT throw the container in your household trash. DO NOT recycle. Keep the container out of the reach of children.
MG Appendix: Prefilled Syringe revision date: April 2009
Medication Guide Appendix: Instructions for Preparing and Giving a Dose with a PEGASYS® Vial
How should I store PEGASYS vials?
PEGASYS must be stored in the refrigerator at a temperature of 2°C to 8°C (36°F to 46°F). Do not leave PEGASYS outside of the refrigerator for more than 24 hours. Do not freeze PEGASYS. Keeping PEGASYS at temperatures outside the recommended range can destroy the medicine.
Each PEGASYS vial can only be used once. Discard after use.
Do not shake the vial of PEGASYS. If PEGASYS is shaken too hard, it will not work properly.
Protect PEGASYS from light during storage.
Keep this and all other medicines out of the reach of children.
The following instructions will help you learn how to measure your dose and give yourself an injection of PEGASYS. You should read through all of these directions and ask your healthcare provider for help if you have any questions before trying to give yourself an injection. It is important to follow these directions carefully. Talk to your healthcare provider if you have any questions about PEGASYS.
If you are giving an injection to someone else, a healthcare provider must teach you how to avoid needle sticks. Being stuck by a used needle can pass diseases on to you.
- 1.
- Collect all the materials you will need before you start to give the injection:
- One vial of PEGASYS
- One syringe and needle
- Several alcohol pads
- A puncture-resistant container to dispose of the needle and syringe when you are finished
- 2.
- Check the date on the carton the PEGASYS comes in and make sure the expiration date has not passed, then remove a vial from the package and look at the medicine.
- Do not use PEGASYS if:
– the medicine is cloudy
– the medicine has particles floating in it
– the medicine is any color besides colorless to light yellow
– the expiration date has passed
- Do not use PEGASYS if:
- 3.
- Warm the refrigerated medicine by gently rolling it in the palms of your hands for about one minute. Do not shake.
- 4.
- Wash your hands with soap and warm water to prevent infection.
- 5.
- Take the vial of PEGASYS and flip off the plastic top covering the vial opening, and clean the rubber stopper on the top of the vial with a different alcohol pad.

If you are not sure how much medicine to use or which mark to use, STOP and call your healthcare provider right away. - 6.
- Remove the needle and syringe from their packaging and attach the needle to the end of the syringe.
- Pull the plunger back so the end of it is to the mark on the syringe barrel that matches the dose prescribed for you by your healthcare provider. This will pull air into the syringe barrel.
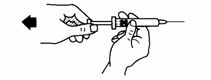
- Push the needle through the center of the stopper on the vial.
- Slowly inject all the air from the syringe into the air space above the solution. Do not inject air into the fluid.

- Keep the needle inside the vial and turn both upside down. Hold the vial and syringe straight up. Slowly pull back on the plunger until the medicine is in the syringe up to the mark that matches your dose. Make sure the needle tip always stays in the medicine (not in the air space above it).

- When the medicine is up to the right mark on the syringe barrel, take the syringe and needle out of the rubber stopper on the vial.
- Keep the syringe pointing up until you are ready to use it.
- If you need to set the syringe down, make sure that you never let the needle touch any surface.
- Pull the plunger back so the end of it is to the mark on the syringe barrel that matches the dose prescribed for you by your healthcare provider. This will pull air into the syringe barrel.
- 7.
- Remove air bubbles from the syringe.
- Hold the syringe with the needle pointing up to the ceiling.
- Using your thumb and finger, tap the syringe to bring air bubbles to the top.
- Press the plunger in slightly to push air bubbles out of the syringe.
- 8.
- Decide where you will give the injection.
- Pick a place on your stomach or thigh (see the picture below). Avoid your navel and waistline. You should use a different place each time you give yourself an injection.
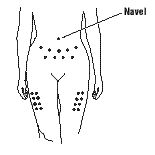
- Pick a place on your stomach or thigh (see the picture below). Avoid your navel and waistline. You should use a different place each time you give yourself an injection.
- 9.
- Prepare your skin for the injection.
- To minimize the discomfort from injections, you may want to gently tap the area where you plan to give yourself an injection.
- Clean the area using an alcohol pad. Let the skin dry for 10 seconds.
- 10.
- Give the injection of PEGASYS.
- Position the point of the needle (the bevel) so it is facing up.
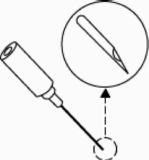
- Pinch a fold of skin on your stomach or thigh firmly between your thumb and forefinger.

- Hold the syringe like a pencil at a 45° to 90° angle to your skin. In one quick motion, insert the needle as far as it will go into the pinched area of skin. Pull the plunger of the syringe back very slightly. If blood comes into the syringe, the needle has entered a blood vessel. Do not inject. Withdraw the needle and discard the syringe as outlined in step 11. Repeat the above steps with a new vial and syringe and prepare a new site.
- If no blood appears, release your skin and slowly push the plunger all the way down so that you get all of your medicine.

- Pull out the needle at same angle you put it in. Wipe the area with an alcohol pad.
- Position the point of the needle (the bevel) so it is facing up.
- 11.
- For safety reasons, always place used syringes and needles in a puncture-resistant container immediately after use and never reuse them.
- If you are using a syringe with a needle-stick protection device, before you dispose of the syringe and needle, place the free end of the green cap on a flat surface and push down on it until it clicks and covers over the needle.
How should I dispose of materials used to inject PEGASYS?
There may be special state and local laws for disposal of used needles and syringes. Your healthcare provider or pharmacist should provide you with instructions on how to properly dispose of your used syringes and needles. Always follow these instructions.
The instructions below should be used as a general guide for proper disposal:
- The needles and syringes should never be reused.
- Place all used needles and syringes in a puncture-proof disposable container that is available through your pharmacy or healthcare provider (Sharp's container).
- DO NOT use glass or clear plastic containers for disposal of needles and syringes.
- Dispose of the full container as instructed by your healthcare provider or pharmacist.
DO NOT throw the container in your household trash. DO NOT recycle. Keep the container out of the reach of children.
MG Appendix: Vial revision date: October 2008
COPEGUS and PEGASYS are trademarks of Hoffmann-La Roche Inc.
Manufactured by:
Hoffmann-La Roche Inc.
340 Kingsland Street
Nutley, NJ 07110-1199
(US Govt. Lic. No. 0136)
Distributed by:
Genentech USA, Inc.
A Member of the Roche Group
1 DNA Way
South San Francisco, CA 94080-4990
PSVS_258310_PI_AR2010_N
PSVS_258310_PI_AR2010_K
© 2010 Genentech, Inc. All rights reserved.
Representative sample of labeling (see the HOW SUPPLIED section for complete listing):
PRINCIPAL DISPLAY PANEL - 0.5 mL 4 Syringe Carton
NDC 0004-0352-30
Pegasys®
(peginterferon alfa-2a)
180 µg/0.5 mL
For Subcutaneous Injection Only
Sterile
Each Carton Contains:
4 Single-Use Prefilled Syringes
Each Prefilled Syringe Contains:
180 µg/0.5 mL
NOT FOR INDIVIDUAL SALE
ATTENTION PHARMACISTS: Each patient is required
to receive the enclosed Medication Guide.
Refrigerate Immediately
Rx only
Genentech
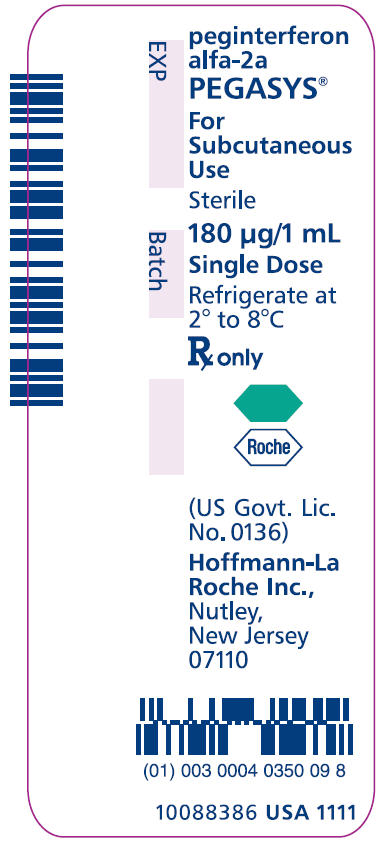
PRINCIPAL DISPLAY PANEL - 0.5 mL 4 Syringe Monthly Convenience Pack
NDC 0004-0352-39
Pegasys®
(peginterferon alfa-2a)
180 µg/0.5 mL
For Subcutaneous Injection Only
Sterile
Prefilled Syringes Monthly Convenience Pack Package Contains:
4 Singel-Use Prefilled Syringes Pegasys® 180 µg/0.5 mL, NDC 0004-0352-30
4 Needles (27-gauge, 1/2-inch)
4 Alcohol Swabs
Each Prefilled Syringe Contains:
180 µg/0.5 mL
ATTENTION PHARMACIST: Each patient is required
to receive the enclosed Medication Guide.
Refrigerate Immediately
Rx only
Genentech
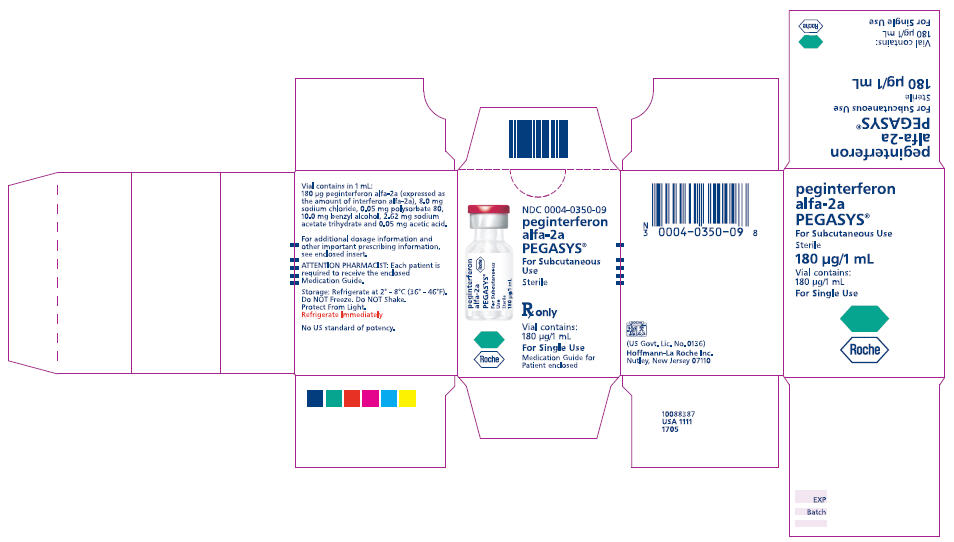
| PEGASYS
peginterferon alfa-2a injection, solution |
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
| Marketing Information | |||
| Marketing Category | Application Number or Monograph Citation | Marketing Start Date | Marketing End Date |
| BLA | BLA103964 | 10/16/2002 | |
| PEGASYS
peginterferon alfa-2a injection, solution |
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
| Marketing Information | |||
| Marketing Category | Application Number or Monograph Citation | Marketing Start Date | Marketing End Date |
| BLA | BLA103964 | 10/16/2002 | |
| Labeler - Hoffmann-La Roche Inc (002191211) |
| Establishment | |||
| Name | Address | ID/FEI | Operations |
| F. Hoffmann-La Roche Ltd | 482242971 | ANALYSIS, MANUFACTURE | |
| Establishment | |||
| Name | Address | ID/FEI | Operations |
| Hoffmann-La Roche Inc | 002191211 | MANUFACTURE | |
| Establishment | |||
| Name | Address | ID/FEI | Operations |
| Roche Diagnostics GmbH | 323105205 | API MANUFACTURE | |