DURAGESIC
-
fentanyl patch
Ortho-McNeil-Janssen Pharmaceuticals, Inc.
----------
DURAGESIC®(Fentanyl Transdermal System)
CII
Full Prescribing Information
FOR USE IN OPIOID-TOLERANT PATIENTS ONLY
DURAGESIC® contains a high concentration of a potent Schedule II opioid agonist, fentanyl. Schedule II opioid substances which include fentanyl, hydromorphone, methadone, morphine, oxycodone, and oxymorphone have the highest potential for abuse and associated risk of fatal overdose due to respiratory depression. Fentanyl can be abused and is subject to criminal diversion. The high content of fentanyl in the patches (DURAGESIC®) may be a particular target for abuse and diversion.
DURAGESIC® is indicated for management of persistent, moderate to severe chronic pain that:
- requires continuous, around-the-clock opioid administration for an extended period of time, and
- cannot be managed by other means such as non-steroidal analgesics, opioid combination products, or immediate-release opioids
DURAGESIC® should ONLY be used in patients who are already receiving opioid therapy, who have demonstrated opioid tolerance, and who require a total daily dose at least equivalent to DURAGESIC® 25 mcg/h. Patients who are considered opioid-tolerant are those who have been taking, for a week or longer, at least 60 mg of morphine daily, or at least 30 mg of oral oxycodone daily, or at least 8 mg of oral hydromorphone daily or an equianalgesic dose of another opioid.
Because serious or life-threatening hypoventilation could occur, DURAGESIC® (fentanyl transdermal system) is contraindicated:
- in patients who are not opioid-tolerant
- in the management of acute pain or in patients who require opioid analgesia for a short period of time
- in the management of post-operative pain, including use after out-patient or day surgeries (e.g., tonsillectomies)
- in the management of mild pain
- in the management of intermittent pain (e.g., use on an as needed basis [prn])
(See CONTRAINDICATIONS for further information.)
Since the peak fentanyl concentrations generally occur between 20 and 72 hours of treatment, prescribers should be aware that serious or life threatening hypoventilation may occur, even in opioid-tolerant patients, during the initial application period.
The concomitant use of DURAGESIC® with all cytochrome P450 3A4 inhibitors (such as ritonavir, ketoconazole, itraconazole, troleandomycin, clarithromycin, nelfinavir, nefazodone, amiodarone, amprenavir, aprepitant, diltiazem, erythromycin, fluconazole, fosamprenavir, grapefruit juice, and verapamil) may result in an increase in fentanyl plasma concentrations, which could increase or prolong adverse drug effects and may cause potentially fatal respiratory depression. Patients receiving DURAGESIC® and any CYP3A4 inhibitor should be carefully monitored for an extended period of time and dosage adjustments should be made if warranted (see CLINICAL PHARMACOLOGY – Drug Interactions, WARNINGS, PRECAUTIONS, and DOSAGE AND ADMINISTRATION for further information).
The safety of DURAGESIC® has not been established in children under 2 years of age. DURAGESIC® should be administered to children only if they are opioid-tolerant and 2 years of age or older (see PRECAUTIONS - Pediatric Use).
DURAGESIC® is ONLY for use in patients who are already tolerant to opioid therapy of comparable potency. Use in non-opioid tolerant patients may lead to fatal respiratory depression. Overestimating the DURAGESIC® dose when converting patients from another opioid medication can result in fatal overdose with the first dose (see DOSAGE AND ADMINISTRATON – Initial DURAGESIC® Dose Selection). Due to the mean half-life of approximately 20–27 hours, patients who are thought to have had a serious adverse event, including overdose, will require monitoring and treatment for at least 24 hours.
DURAGESIC® can be abused in a manner similar to other opioid agonists, legal or illicit. This risk should be considered when administering, prescribing, or dispensing DURAGESIC® in situations where the healthcare professional is concerned about increased risk of misuse, abuse, or diversion.
Persons at increased risk for opioid abuse include those with a personal or family history of substance abuse (including drug or alcohol abuse or addiction) or mental illness (e.g., major depression). Patients should be assessed for their clinical risks for opioid abuse or addiction prior to being prescribed opioids. All patients receiving opioids should be routinely monitored for signs of misuse, abuse, and addiction. Patients at increased risk of opioid abuse may still be appropriately treated with modified-release opioid formulations; however, these patients will require intensive monitoring for signs of misuse, abuse, or addiction.
DURAGESIC® patches are intended for transdermal use (on intact skin) only. Do not use a DURAGESIC® patch if the pouch seal is broken or the patch is cut, damaged, or changed in any way.
Avoid exposing the DURAGESIC® application site and surrounding area to direct external heat sources, such as heating pads or electric blankets, heat or tanning lamps, saunas, hot tubs, and heated water beds, while wearing the system. Avoid taking hot baths or sunbathing. There is a potential for temperature-dependent increases in fentanyl released from the system resulting in possible overdose and death. Patients wearing DURAGESIC® systems who develop fever or increased core body temperature due to strenuous exertion should be monitored for opioid side effects and the DURAGESIC® dose should be adjusted if necessary.
DESCRIPTION
DURAGESIC® (fentanyl transdermal system) is a transdermal system providing continuous systemic delivery of fentanyl, a potent opioid analgesic, for 72 hours. The chemical name is N-Phenyl-N-(1-(2-phenylethyl)-4-piperidinyl) propanamide. The structural formula is:
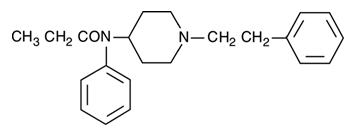
The molecular weight of fentanyl base is 336.5, and the empirical formula is C22H28N2O. The n-octanol:water partition coefficient is 860:1. The pKa is 8.4.
System Components and Structure
The amount of fentanyl released from each system per hour is proportional to the surface area (25 mcg/h per 10.5 cm2). The composition per unit area of all system sizes is identical.
| Dose*
(mcg/h) | Size (cm2) | Fentanyl Content (mg) |
|---|---|---|
| 12† | 5.25 | 2.1 |
| 25 | 10.5 | 4.2 |
| 50 | 21 | 8.4 |
| 75 | 31.5 | 12.6 |
| 100 | 42 | 16.8 |
DURAGESIC® is a rectangular transparent unit comprising a protective liner and two functional layers. Proceeding from the outer surface toward the surface adhering to skin, these layers are:
1) a backing layer of polyester/ethyl vinyl acetate film; 2) a drug-in-adhesive layer. Before use, a protective liner covering the adhesive layer is removed and discarded.
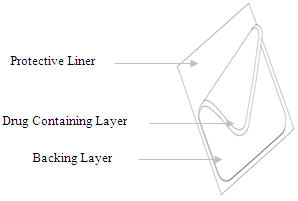
The active component of the system is fentanyl. The remaining components are pharmacologically inactive.
CLINICAL PHARMACOLOGY
Pharmacology
Fentanyl is an opioid analgesic. Fentanyl interacts predominately with the opioid mu-receptor. These mu-binding sites are discretely distributed in the human brain, spinal cord, and other tissues. In clinical settings, fentanyl exerts its principal pharmacologic effects on the central nervous system.
In addition to analgesia, alterations in mood, euphoria, dysphoria, and drowsiness commonly occur. Fentanyl depresses the respiratory centers, depresses the cough reflex, and constricts the pupils. Analgesic blood concentrations of fentanyl may cause nausea and vomiting directly by stimulating the chemoreceptor trigger zone, but nausea and vomiting are significantly more common in ambulatory than in recumbent patients, as is postural syncope.
Opioids increase the tone and decrease the propulsive contractions of the smooth muscle of the gastrointestinal tract. The resultant prolongation in gastrointestinal transit time may be responsible for the constipating effect of fentanyl. Because opioids may increase biliary tract pressure, some patients with biliary colic may experience worsening rather than relief of pain.
While opioids generally increase the tone of urinary tract smooth muscle, the net effect tends to be variable, in some cases producing urinary urgency, in others, difficulty in urination. At therapeutic dosages, fentanyl usually does not exert major effects on the cardiovascular system. However, some patients may exhibit orthostatic hypotension and fainting.
Histamine assays and skin wheal testing in clinical studies indicate that clinically significant histamine release rarely occurs with fentanyl administration. Clinical assays show no clinically significant histamine release in dosages up to 50 mcg/kg.
Pharmacokinetics
The DURAGESIC® (fentanyl transdermal system) is a drug-in-adhesive matrix designed formulation. Fentanyl is released from the matrix at a nearly constant amount per unit time. The concentration gradient existing between the matrix and the lower concentration in the skin drives drug release. Fentanyl moves in the direction of the lower concentration at a rate determined by the matrix and the diffusion of fentanyl through the skin layers. While the actual rate of fentanyl delivery to the skin varies over the 72-hour application period, each system is labeled with a nominal flux which represents the average amount of drug delivered to the systemic circulation per hour across average skin.
While there is variation in dose delivered among patients, the nominal flux of the systems (12.5, 25, 50, 75, and 100 mcg of fentanyl per hour) is sufficiently accurate as to allow individual titration of dosage for a given patient.
Following DURAGESIC® application, the skin under the system absorbs fentanyl, and a depot of fentanyl concentrates in the upper skin layers. Fentanyl then becomes available to the systemic circulation. Serum fentanyl concentrations increase gradually following initial DURAGESIC® application, generally leveling off between 12 and 24 hours and remaining relatively constant, with some fluctuation, for the remainder of the 72-hour application period. Peak serum concentrations of fentanyl generally occurred between 20 and 72 hours after initial application (see Table A). Serum fentanyl concentrations achieved are proportional to the DURAGESIC® delivery rate. With continuous use, serum fentanyl concentrations continue to rise for the first two system applications. By the end of the second 72-hour application, a steady-state serum concentration is reached and is maintained during subsequent applications of a patch of the same size. Patients reach and maintain a steady-state serum concentration that is determined by individual variation in skin permeability and body clearance of fentanyl.
After system removal, serum fentanyl concentrations decline gradually, falling about 50% in approximately 20–27 hours. Continued absorption of fentanyl from the skin accounts for a slower disappearance of the drug from the serum than is seen after an IV infusion, where the apparent half-life is approximately 7 (range 3–12) hours.
| Serum Fentanyl Concentrations Following Single and Multiple Applications of DURAGESIC® 100 mcg/h |
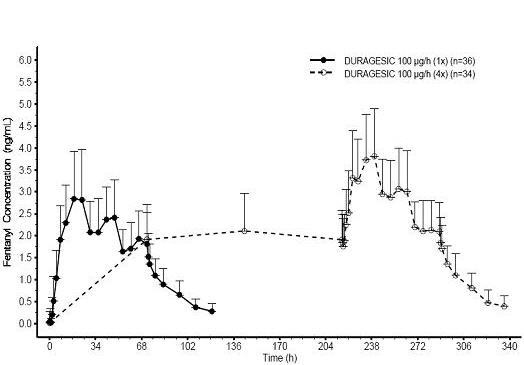 |
| Mean (SD) Time to Maximal Concentration Tmax (h) | Mean (SD) Maximal Concentration Cmax (ng/mL) |
|
|---|---|---|
| NOTE: After system removal there is continued systemic absorption from residual fentanyl in the skin so that serum concentrations fall 50%, on average, in approximately 20–27 hours. | ||
|
||
| DURAGESIC® 12 mcg/h | 28.8 (13.7) | 0.38 (0.13)* |
| DURAGESIC® 25 mcg/h | 31.7 (16.5) | 0.85 (0.26) |
| DURAGESIC® 50 mcg/h | 32.8 (15.6) | 1.72 (0.53) |
| DURAGESIC® 75 mcg/h | 35.8 (14.1) | 2.32 (0.86) |
| DURAGESIC® 100 mcg/h | 29.9 (13.3) | 3.36 (1.28) |
| Clearance (L/h) Range [70 kg] | Volume of Distribution VSS (L/kg) Range | Half-Life t1/2 (h) Range |
|
|---|---|---|---|
| NOTE: Information on volume of distribution and half-life not available for renally impaired patients. | |||
|
|||
| Surgical Patients | 27 – 75 | 3 – 8 | 3 – 12 |
| Hepatically Impaired Patients | 3 – 80* | 0.8 – 8* | 4 – 12* |
| Renally Impaired Patients | 30 – 78 | – | – |
Fentanyl plasma protein binding capacity decreases with increasing ionization of the drug. Alterations in pH may affect its distribution between plasma and the central nervous system. Fentanyl accumulates in the skeletal muscle and fat and is released slowly into the blood. The average volume of distribution for fentanyl is 6 L/kg (range 3–8; N=8).
Fentanyl is metabolized primarily via human cytochrome P450 3A4 isoenzyme system. In humans, the drug appears to be metabolized primarily by oxidative N-dealkylation to norfentanyl and other inactive metabolites that do not contribute materially to the observed activity of the drug. Within 72 hours of IV fentanyl administration, approximately 75% of the dose is excreted in urine, mostly as metabolites with less than 10% representing unchanged drug. Approximately 9% of the dose is recovered in the feces, primarily as metabolites. Mean values for unbound fractions of fentanyl in plasma are estimated to be between 13 and 21%.
Skin does not appear to metabolize fentanyl delivered transdermally. This was determined in a human keratinocyte cell assay and in clinical studies in which 92% of the dose delivered from the system was accounted for as unchanged fentanyl that appeared in the systemic circulation.
Special Populations
Hepatic or Renal Disease
Insufficient information exists to make recommendations regarding the use of DURAGESIC® in patients with impaired renal or hepatic function. Fentanyl is metabolized primarily via human cytochrome P450 3A4 isoenzyme system and mostly eliminated in urine. If the drug is used in these patients, it should be used with caution because of the hepatic metabolism and renal excretion of fentanyl.
Pediatric Use
In 1.5 to 5 year old, non-opioid-tolerant pediatric patients, the fentanyl plasma concentrations were approximately twice as high as that of adult patients. In older pediatric patients, the pharmacokinetic parameters were similar to that of adults. However, these findings have been taken into consideration in determining the dosing recommendations for opioid-tolerant pediatric patients (2 years of age and older). For pediatric dosing information, refer to DOSAGE AND ADMINISTRATION section.
Geriatric Use
Data from intravenous studies with fentanyl suggest that the elderly patients may have reduced clearance and a prolonged half-life. Moreover elderly patients may be more sensitive to the active substance than younger patients. A study conducted with the DURAGESIC® fentanyl transdermal patch in elderly patients demonstrated that fentanyl pharmacokinetics did not differ significantly from young adult subjects, although peak serum concentrations tended to be lower and mean half-life values were prolonged to approximately 34 hours.
Respiratory depression is the chief hazard in elderly or debilitated patients, usually following large initial doses in non-tolerant patients or when opioids are given in conjunction with other agents that depress respiration.
DURAGESIC® should be used with caution in elderly, cachectic or debilitated patients as they may have altered pharmacokinetics due to poor fat stores, muscle wasting, or altered clearance (see DOSAGE AND ADMINISTRATION).
Drug Interactions
The interaction between ritonavir, a CPY3A4 inhibitor, and fentanyl was investigated in eleven healthy volunteers in a randomized crossover study. Subjects received oral ritonavir or placebo for 3 days. The ritonavir dose was 200 mg tid on Day 1 and 300 mg tid on Day 2 followed by one morning dose of 300 mg on Day 3. On Day 2, fentanyl was given as a single IV dose at 5 mcg/kg two hours after the afternoon dose of oral ritonavir or placebo. Naloxone was administered to counteract the side effects of fentanyl. The results suggested that ritonavir might decrease the clearance of fentanyl by 67%, resulting in a 174% (range 52%–420%) increase in fentanyl AUC0–∞. Coadministration of ritonavir in patients receiving DURAGESIC® has not been studied; however, an increase in fentanyl AUC is expected (see BOX WARNING, WARNINGS, PRECAUTIONS, and DOSAGE AND ADMINISTRATION).
Fentanyl is metabolized mainly via the human cytochrome P450 3A4 isoenzyme system (CYP3A4), therefore, potential interactions may occur when DURAGESIC® is given concurrently with agents that affect CYP3A4 activity. Coadminstration with agents that induce CYP3A4 activity may reduce the efficacy of DURAGESIC®. The concomitant use of transdermal fentanyl with all CYP3A4 inhibitors (such as ritonavir, ketoconazole, itraconazole, troleandomycin, clarithromycin, nelfinavir, nefazadone, amiodarone, amprenavir, aprepitant, diltiazem, erythromycin, fluconazole, fosamprenavir, grapefruit juice, and verapamil) may result in an increase in fentanyl plasma concentrations, which could increase or prolong adverse drug effects and may cause potentially fatal respiratory depression. Patients receiving DURAGESIC® and any CYP3A4 inhibitor should be carefully monitored for an extended period of time and dosage adjustments should be made if warranted (see BOX WARNING, WARNINGS, PRECAUTIONS, and DOSAGE AND ADMINISTRATION for further information).
PHARMACODYNAMICS
Ventilatory Effects
Because of the risk for serious or life-threatening hypoventilation, DURAGESIC® is CONTRAINDICATED in the treatment of post-operative and acute pain and in patients who are not opioid-tolerant. In clinical trials of 357 patients with acute pain treated with DURAGESIC®, 13 patients experienced hypoventilation. Hypoventilation was manifested by respiratory rates of less than 8 breaths/minute or a pCO2 greater than 55 mm Hg. In these studies, the incidence of hypoventilation was higher in nontolerant women (10) than in men (3) and in patients weighing less than 63 kg (9 of 13). Although patients with impaired respiration were not common in the trials, they had higher rates of hypoventilation. In addition, post-marketing reports have been received that describe opioid-naive post-operative patients who have experienced clinically significant hypoventilation and death with DURAGESIC®.
While most adult and pediatric patients using DURAGESIC® chronically develop tolerance to fentanyl induced hypoventilation, episodes of slowed respirations may occur at any time during therapy.
Hypoventilation can occur throughout the therapeutic range of fentanyl serum concentrations, especially for patients who have an underlying pulmonary condition or who receive usual doses of opioids or other CNS drugs associated with hypoventilation in addition to DURAGESIC®. The use of DURAGESIC® is contraindicated in patients who are not tolerant to opioid therapy.
The use of DURAGESIC® should be monitored by clinical evaluation, especially within the initial 24–72 hours when serum concentrations from the initial patch will peak, and following increases in dosage. DURAGESIC® should be administered to children only if they are opioid-tolerant and 2 years of age or older.
See BOX WARNING, CONTRAINDICATIONS, WARNINGS, PRECAUTIONS, ADVERSE REACTIONS, and OVERDOSAGE for additional information on hypoventilation.
Cardiovascular Effects
Fentanyl may infrequently produce bradycardia. The incidence of bradycardia in clinical trials with DURAGESIC® was less than 1%.
CNS Effects
Central nervous system effects increase with increasing serum fentanyl concentrations.
INDICATIONS AND USAGE
DURAGESIC® is indicated for management of persistent, moderate to severe chronic pain that:
- requires continuous, around-the-clock opioid administration for an extended period of time, and
- cannot be managed by other means such as non-steroidal analgesics, opioid combination products, or immediate-release opioids.
DURAGESIC® should ONLY be used in patients who are already receiving opioid therapy, who have demonstrated opioid tolerance, and who require a total daily dose at least equivalent to DURAGESIC® 25 mcg/h (see DOSAGE AND ADMINISTRATION). Patients who are considered opioid-tolerant are those who have been taking, for a week or longer, at least 60 mg of morphine daily, or at least 30 mg of oral oxycodone daily, or at least 8 mg of oral hydromorphone daily, or an equianalgesic dose of another opioid.
Because serious or life-threatening hypoventilation could result, DURAGESIC® is contraindicated for use on an as needed basis (i.e., prn), for the management of post-operative or acute pain, or in patients who are not opioid-tolerant or who require opioid analgesia for a short period of time (see BOX WARNING and CONTRAINDICATIONS).
An evaluation of the appropriateness and adequacy of treating with immediate-release opioids is advisable prior to initiating therapy with any modified-release opioid. Prescribers should individualize treatment in every case, initiating therapy at the appropriate point along a progression from non-opioid analgesics, such as non-steroidal anti-inflammatory drugs and acetaminophen, to opioids, in a plan of pain management such as outlined by the World Health Organization, the Agency for Health Research and Quality, the Federation of State Medical Boards Model Policy, or the American Pain Society.
Patients should be assessed for their clinical risks for opioid abuse or addiction prior to being prescribed opioids. Patients receiving opioids should be routinely monitored for signs of misuse, abuse, and addiction. Persons at increased risk for opioid abuse include those with a personal or family history of substance abuse (including drug or alcohol abuse or addiction) or mental illness (e.g., major depression). Patients at increased risk may still be appropriately treated with modified-release opioid formulations; however these patients will require intensive monitoring for signs of misuse, abuse, or addiction.
CONTRAINDICATIONS
Because serious or life-threatening hypoventilation could occur, DURAGESIC® (fentanyl transdermal system) is contraindicated:
- in patients who are not opioid-tolerant
- in the management of acute pain or in patients who require opioid analgesia for a short period of time
- in the management of post-operative pain, including use after out-patient or day surgeries, (e.g., tonsillectomies)
- in the management of mild pain
- in the management of intermittent pain (e.g., use on an as needed basis [prn])
- in situations of significant respiratory depression, especially in unmonitored settings where there is a lack of resuscitative equipment
- in patients who have acute or severe bronchial asthma
DURAGESIC® (fentanyl transdermal system) is contraindicated in patients who have or are suspected of having paralytic ileus.
DURAGESIC® (fentanyl transdermal system) is contraindicated in patients with known hypersensitivity to fentanyl or any components of this product.
WARNINGS
DURAGESIC® patches are intended for transdermal use (on intact skin) only. Do not use a DURAGESIC® patch if the pouch seal is broken or the patch is cut, damaged, or changed in any way.
The safety of DURAGESIC® (fentanyl transdermal system) has not been established in children under 2 years of age. DURAGESIC® should be administered to children only if they are opioid-tolerant and 2 years of age or older (see PRECAUTIONS – Pediatric Use).
DURAGESIC® is ONLY for use in patients who are already tolerant to opioid therapy of comparable potency. Use in non-opioid tolerant patients may lead to fatal respiratory depression. Overestimating the DURAGESIC® dose when converting patients from another opioid medication can result in fatal overdose with the first dose. The mean half-life is approximately 20–27 hours. Therefore, patients who have experienced serious adverse events, including overdose, will require monitoring for at least 24 hours after DURAGESIC® removal since serum fentanyl concentrations decline gradually and reach an approximate 50% reduction in serum concentrations 20–27 hours after system removal.
DURAGESIC® should be prescribed only by persons knowledgeable in the continuous administration of potent opioids, in the management of patients receiving potent opioids for treatment of pain, and in the detection and management of hypoventilation including the use of opioid antagonists.
All patients and their caregivers should be advised to avoid exposing the DURAGESIC® application site and surrounding area to direct external heat sources, such as heating pads or electric blankets, heat or tanning lamps, saunas, hot tubs, and heated water beds, etc., while wearing the system. Patients should be advised against taking hot baths or sunbathing. There is a potential for temperature-dependent increases in fentanyl released from the system resulting in possible overdose and death. A clinical pharmacology trial conducted in healthy adult subjects has shown that the application of heat over the DURAGESIC® system increased mean fentanyl AUC values by 120% and mean Cmax values by 61%.
Based on a pharmacokinetic model, serum fentanyl concentrations could theoretically increase by approximately one-third for patients with a body temperature of 40°C (104°F) due to temperature-dependent increases in fentanyl released from the system and increased skin permeability. Patients wearing DURAGESIC® systems who develop fever or increased core body temperature due to strenuous exertion should be monitored for opioid side effects and the DURAGESIC® dose should be adjusted if necessary.
Death and other serious medical problems have occurred when people were accidentally exposed to DURAGESIC®. Examples of accidental exposure include transfer of a DURAGESIC® patch from an adult's body to a child while hugging, accidental sitting on a patch and possible accidental exposure of a caregiver's skin to the medication in the patch while the caregiver was applying or removing the patch.
Placing DURAGESIC® in the mouth, chewing it, swallowing it, or using it in ways other than indicated may cause choking or overdose that could result in death.
Misuse, Abuse and Diversion of Opioids
Fentanyl is an opioid agonist of the morphine-type. Such drugs are sought by drug abusers and people with addiction disorders and are subject to criminal diversion.
Fentanyl can be abused in a manner similar to other opioids, legal or illicit. This should be considered when prescribing or dispensing DURAGESIC® in situations where the physician or pharmacist is concerned about an increased risk of misuse, abuse, or diversion.
DURAGESIC® has been reported as being abused by other methods and routes of administration. These practices will result in uncontrolled delivery of the opioid and pose a significant risk to the abuser that could result in overdose and death (see WARNINGS and DRUG ABUSE AND ADDICTION).
Concerns about abuse, addiction, and diversion should not prevent the proper management of pain. However, all patients treated with opioids require careful monitoring for signs of abuse and addiction, since use of opioid analgesic products carries the risk of addiction even under appropriate medical use.
Healthcare professionals should contact their state professional licensing board or state controlled substances authority for information on how to prevent and detect abuse or diversion of this product.
Hypoventilation (Respiratory Depression)
Serious or life-threatening hypoventilation may occur at any time during the use of DURAGESIC® especially during the initial 24–72 hours following initiation of therapy and following increases in dose.
Because significant amounts of fentanyl continue to be absorbed from the skin for 20–27 hours or more after the patch is removed, hypoventilation may persist beyond the removal of DURAGESIC®. Consequently, patients with hypoventilation should be carefully observed for degree of sedation and their respiratory rate monitored until respiration has stabilized.
The use of concomitant CNS active drugs requires special patient care and observation.
Respiratory depression is the chief hazard of opioid agonists, including fentanyl the active ingredient in DURAGESIC®. Respiratory depression is more likely to occur in elderly or debilitated patients, usually following large initial doses in non-tolerant patients, or when opioids are given in conjunction with other drugs that depress respiration.
Respiratory depression from opioids is manifested by a reduced urge to breathe and a decreased rate of respiration, often associated with the "sighing" pattern of breathing (deep breaths separated by abnormally long pauses). Carbon dioxide retention from opioid-induced respiratory depression can exacerbate the sedating effects of opioids. This makes overdoses involving drugs with sedative properties and opioids especially dangerous.
DURAGESIC® should be used with extreme caution in patients with significant chronic obstructive pulmonary disease or cor pulmonale, and in patients having a substantially decreased respiratory reserve, hypoxia, hypercapnia, or pre-existing respiratory depression. In such patients, even usual therapeutic doses of DURAGESIC® may decrease respiratory drive to the point of apnea. In these patients, alternative non-opioid analgesics should be considered, and opioids should be employed only under careful medical supervision at the lowest effective dose.
Chronic Pulmonary Disease
Because potent opioids can cause serious or life-threatening hypoventilation, DURAGESIC® should be administered with caution to patients with pre-existing medical conditions predisposing them to hypoventilation. In such patients, normal analgesic doses of opioids may further decrease respiratory drive to the point of respiratory failure.
Head Injuries and Increased Intracranial Pressure
DURAGESIC® should not be used in patients who may be particularly susceptible to the intracranial effects of CO2 retention such as those with evidence of increased intracranial pressure, impaired consciousness, or coma. Opioids may obscure the clinical course of patients with head injury. DURAGESIC® should be used with caution in patients with brain tumors.
Interactions with Other CNS Depressants
The concomitant use of DURAGESIC® (fentanyl transdermal system) with other central nervous system depressants, including but not limited to other opioids, sedatives, hypnotics, tranquilizers (e.g., benzodiazepines), general anesthetics, phenothiazines, skeletal muscle relaxants, and alcohol, may cause respiratory depression, hypotension, and profound sedation or potentially result in coma. When such combined therapy is contemplated, the dose of one or both agents should be significantly reduced.
Interactions with Alcohol and Drugs of Abuse
Fentanyl may be expected to have additive CNS depressant effects when used in conjunction with alcohol, other opioids, or illicit drugs that cause central nervous system depression.
Interactions with CYP3A4 Inhibitors
The concomitant use of transdermal fentanyl with all CYP3A4 inhibitors (such as ritonavir, ketoconazole, itraconazole, troleandomycin, clarithromycin, nelfinavir, nefazadone, amiodarone, amprenavir, aprepitant, diltiazem, erythromycin, fluconazole, fosamprenavir, grapefruit juice, and verapamil) may result in an increase in fentanyl plasma concentrations, which could increase or prolong adverse drug effects and may cause potentially fatal respiratory depression. Patients receiving DURAGESIC® and any CYP3A4 inhibitor should be carefully monitored for an extended period of time, and dosage adjustments should be made if warranted (see BOX WARNING, CLINICAL PHARMACOLOGY – Drug Interactions, PRECAUTIONS, and DOSAGE AND ADMINISTRATION for further information).
PRECAUTIONS
General
DURAGESIC® (fentanyl transdermal system) should not be used to initiate opioid therapy in patients who are not opioid-tolerant. Children converting to DURAGESIC® should be opioid-tolerant and 2 years of age or older (see BOX WARNING).
Patients, family members, and caregivers should be instructed to keep patches (new and used) out of the reach of children and others for whom DURAGESIC® was not prescribed. A considerable amount of active fentanyl remains in DURAGESIC® even after use as directed. Accidental or deliberate application or ingestion by a child or adolescent will cause respiratory depression that could result in death.
Cardiac Disease
Fentanyl may produce bradycardia. Fentanyl should be administered with caution to patients with bradyarrhythmias.
Hepatic or Renal Disease
Insufficient information exists to make recommendations regarding the use of DURAGESIC® in patients with impaired renal or hepatic function. If the drug is used in these patients, it should be used with caution because of the hepatic metabolism and renal excretion of fentanyl.
Use in Pancreatic/Biliary Tract Disease
DURAGESIC® may cause spasm of the sphincter of Oddi and should be used with caution in patients with biliary tract disease, including acute pancreatitis. Opioids like DURAGESIC® may cause increases in the serum amylase concentration.
Tolerance
Tolerance is a state of adaptation in which exposure to a drug induces changes that result in a diminution of one or more of the drug's effects over time. Tolerance may occur to both the desired and undesired effects of drugs, and may develop at different rates for different effects.
Physical Dependence
Physical dependence is a state of adaptation that is manifested by an opioid specific withdrawal syndrome that can be produced by abrupt cessation, rapid dose reduction, decreasing blood concentration of the drug, and/or administration of an antagonist. The opioid abstinence or withdrawal syndrome is characterized by some or all of the following: restlessness, lacrimation, rhinorrhea, yawning, perspiration, chills, piloerection, myalgia, mydriasis, irritability, anxiety, backache, joint pain, weakness, abdominal cramps, insomnia, nausea, anorexia, vomiting, diarrhea, or increased blood pressure, respiratory rate, or heart rate. In general, opioids should not be abruptly discontinued (see DOSAGE AND ADMINISTRATION – Discontinuation of DURAGESIC®).
Ambulatory Patients
Strong opioid analgesics impair the mental or physical abilities required for the performance of potentially dangerous tasks, such as driving a car or operating machinery. Patients who have been given DURAGESIC® should not drive or operate dangerous machinery unless they are tolerant to the effects of the drug.
Information for Patients
Patients and their caregivers should be provided with a Medication Guide each time DURAGESIC® is dispensed because new information may be available.
Patients receiving DURAGESIC® patches should be given the following instructions by the physician:
- Patients should be advised that DURAGESIC® patches contain fentanyl, an opioid pain medicine similar to morphine, hydromorphone, methadone, oxycodone, and oxymorphone.
- Patients should be advised that each DURAGESIC® patch may be worn continuously for 72 hours, and that each patch should be applied to a different skin site after removal of the previous transdermal patch.
- Patients should be advised that DURAGESIC® patches should be applied to intact, non-irritated, and non-irradiated skin on a flat surface such as the chest, back, flank, or upper arm. Additionally, patients should be advised of the following:
- In young children or persons with cognitive impairment, the patch should be put on the upper back to lower the chances that the patch will be removed and placed in the mouth.
- Hair at the application site should be clipped (not shaved) prior to patch application.
- If the site of DURAGESIC® application must be cleansed prior to application of the patch, do so with clear water.
- Do not use soaps, oils, lotions, alcohol, or any other agents that might irritate the skin or alter its characteristics.
- Allow the skin to dry completely prior to patch application.
- Patients should be advised that DURAGESIC® should be applied immediately upon removal from the sealed pouch and after removal of the protective liner. Additionally the patient should be advised of the following:
- The DURAGESIC® patch should not be used if the pouch seal is broken, or if the patch is cut, damaged, or changed in any way.
- The transdermal patch should be pressed firmly in place with the palm of the hand for 30 seconds, making sure the contact is complete, especially around the edges.
- The patch should not be folded so that only part of the patch is exposed.
- Patients should be advised that the dose of DURAGESIC® or the number of patches applied to the skin should NEVER be adjusted without the prescribing healthcare professional's instruction.
- Patients should be advised that while wearing the patch, they should avoid exposing the DURAGESIC® application site and surrounding area to direct external heat sources, such as:
- heating pads,
- electric blankets,
- sunbathing,
- heat or tanning lamps,
- saunas,
- hot tubs or hot baths, and
- heated water beds, etc.
- Patients should also be advised of a potential for temperature-dependent increases in fentanyl release from the patch that could result in an overdose of fentanyl; therefore, patients who develop a high fever or increased body temperature due to strenuous exertion while wearing the patch should contact their physician.
- Patients should be advised that if they experience problems with adhesion of the DURAGESIC® patch, they may tape the edges of the patch with first aid tape. If problems with adhesion persist, patients may overlay the patch with a transparent adhesive film dressing (e.g., Bioclusive™ or Tegaderm™).
- Patients should be advised that if the patch falls off before 72 hours a new patch may be applied to a different skin site.
- Patients should be advised to fold (so that the adhesive side adheres to itself) and immediately flush down the toilet used DURAGESIC® patches after removal from the skin.
- Patients should be advised that DURAGESIC® may impair mental and/or physical ability required for the performance of potentially hazardous tasks (e.g., driving, operating machinery).
- Patients should be advised to refrain from any potentially dangerous activity when starting on DURAGESIC® or when their dose is being adjusted, until it is established that they have not been adversely affected.
- Patients should be advised that DURAGESIC® should not be combined with alcohol or other CNS depressants (e.g. sleep medications, tranquilizers) because dangerous additive effects may occur, resulting in serious injury or death.
- Patients should be advised to consult their physician or pharmacist if other medications are being or will be used with DURAGESIC®.
- Patients should be advised of the potential for severe constipation.
- Patients should be advised that if they have been receiving treatment with DURAGESIC® and cessation of therapy is indicated, it may be appropriate to taper the DURAGESIC® dose, rather than abruptly discontinue it, due to the risk of precipitating withdrawal symptoms.
- Patients should be advised that DURAGESIC® contains fentanyl, a drug with high potential for abuse.
- Patients, family members, and caregivers should be advised to protect DURAGESIC® from theft or misuse in the work or home environment.
- Patients should be instructed to keep DURAGESIC® in a secure place out of the reach of children due to the high risk of fatal respiratory depression.
- Patients should be advised that DURAGESIC® should never be given to anyone other than the individual for whom it was prescribed because of the risk of death or other serious medical problems to that person for whom it was not intended.
- Patients should be informed that, if the patch dislodges and accidentally sticks to the skin of another person, they should immediately take the patch off, wash the exposed area with water and seek medical attention for the accidentally exposed individual.
- When DURAGESIC® is no longer needed, the unused patches should be removed from their pouches, folded so that the adhesive side of the patch adheres to itself, and flushed down the toilet.
- Women of childbearing potential who become, or are planning to become pregnant, should be advised to consult a physician prior to initiating or continuing therapy with DURAGESIC®.
- Patients should be informed that accidental exposure or misuse may lead to death or other serious medical problems.
Drug Interactions
Agents Affecting Cytochrome P450 3A4 Isoenzyme System
Fentanyl is metabolized mainly via the human cytochrome P450 3A4 isoenzyme system (CYP3A4), therefore potential interactions may occur when DURAGESIC® is given concurrently with agents that affect CYP3A4 activity. Coadminstration with agents that induce CYP3A4 activity may reduce the efficacy of DURAGESIC®. The concomitant use of transdermal fentanyl with all CYP3A4 inhibitors (such as ritonavir, ketoconazole, itraconazole, troleandomycin, clarithromycin, nelfanivir, nefazadone, amiodarone, amprenavir, aprepitant, diltiazem, erythromycin, fluconazole, fosamprenavir, grapefruit juice, and verapamil) may result in an increase in fentanyl plasma concentrations, which could increase or prolong adverse drug effects and may cause fatal respiratory depression. Patients receiving DURAGESIC® and any CYP3A4 inhibitor should be carefully monitored for an extended period of time, and dosage adjustments should be made if warranted (see BOX WARNING, CLINICAL PHARMACOLOGY – Drug Interactions, WARNINGS, and DOSAGE AND ADMINISTRATION for further information).
Central Nervous System Depressants
The concomitant use of DURAGESIC® (fentanyl transdermal system) with other central nervous system depressants, including but not limited to other opioids, sedatives, hypnotics, tranquilizers (e.g., benzodiazepines), general anesthetics, phenothiazines, skeletal muscle relaxants, and alcohol, may cause respiratory depression, hypotension, and profound sedation, or potentially result in coma or death. When such combined therapy is contemplated, the dose of one or both agents should be significantly reduced.
MAO Inhibitors
DURAGESIC® is not recommended for use in patients who have received MAOI within 14 days because severe and unpredictable potentiation by MAO inhibitors has been reported with opioid analgesics.
Carcinogenesis, Mutagenesis, and Impairment of Fertility
In a two-year carcinogenicity study conducted in rats, fentanyl was not associated with an increased incidence of tumors at subcutaneous doses up to 33 µg/kg/day in males or 100 µg/kg/day in females (0.16 and 0.39 times the human daily exposure obtained via the 100 mcg/h patch based on AUC0–24h comparison). There was no evidence of mutagenicity in the Ames Salmonella mutagenicity assay, the primary rat hepatocyte unscheduled DNA synthesis assay, the BALB/c 3T3 transformation test, and the human lymphocyte and CHO chromosomal aberration in-vitro assays.
The potential effects of fentanyl on male and female fertility were examined in the rat model via two separate experiments. In the male fertility study, male rats were treated with fentanyl (0, 0.025, 0.1 or 0.4 mg/kg/day) via continuous intravenous infusion for 28 days prior to mating; female rats were not treated. In the female fertility study, female rats were treated with fentanyl (0, 0.025, 0.1 or 0.4 mg/kg/day) via continuous intravenous infusion for 14 days prior to mating until day 16 of pregnancy; male rats were not treated. Analysis of fertility parameters in both studies indicated that an intravenous dose of fentanyl up to 0.4 mg/kg/day to either the male or the female alone produced no effects on fertility (this dose is approximately 1.6 times the daily human dose administered by a 100 mcg/hr patch on a mg/m2 basis). In a separate study, a single daily bolus dose of fentanyl was shown to impair fertility in rats when given in intravenous doses of 0.3 times the human dose for a period of 12 days.
Pregnancy
Pregnancy Category C
No epidemiological studies of congenital anomalies in infants born to women treated with fentanyl during pregnancy have been reported.
The potential effects of fentanyl on embryo-fetal development were studied in the rat, mouse, and rabbit models. Published literature reports that administration of fentanyl (0, 10, 100, or 500 µg/kg/day) to pregnant female Sprague-Dawley rats from day 7 to 21 via implanted microosmotic minipumps did not produce any evidence of teratogenicity (the high dose is approximately 2 times the daily human dose administered by a 100 mcg/hr patch on a mg/m2 basis). In contrast, the intravenous administration of fentanyl (0, 0.01, or 0.03 mg/kg) to bred female rats from gestation day 6 to 18 suggested evidence of embryotoxicity and a slight increase in mean delivery time in the 0.03 mg/kg/day group. There was no clear evidence of teratogenicity noted.
Pregnant female New Zealand White rabbits were treated with fentanyl (0, 0.025, 0.1, 0.4 mg/kg) via intravenous infusion from day 6 to day 18 of pregnancy. Fentanyl produced a slight decrease in the body weight of the live fetuses at the high dose, which may be attributed to maternal toxicity. Under the conditions of the assay, there was no evidence for fentanyl induced adverse effects on embryo-fetal development at doses up to 0.4 mg/kg (approximately 3 times the daily human dose administered by a 100 mcg/hr patch on a mg/m2 basis).
There are no adequate and well-controlled studies in pregnant women. DURAGESIC® should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Nonteratogenic Effects
Chronic maternal treatment with fentanyl during pregnancy has been associated with transient respiratory depression, behavioral changes, or seizures characteristic of neonatal abstinence syndrome in newborn infants. Symptoms of neonatal respiratory or neurological depression were no more frequent than expected in most studies of infants born to women treated acutely during labor with intravenous or epidural fentanyl. Transient neonatal muscular rigidity has been observed in infants whose mothers were treated with intravenous fentanyl.
The potential effects of fentanyl on prenatal and postnatal development were examined in the rat model. Female Wistar rats were treated with 0, 0.025, 0.1, or 0.4 mg/kg/day fentanyl via intravenous infusion from day 6 of pregnancy through 3 weeks of lactation. Fentanyl treatment (0.4 mg/kg/day) significantly decreased body weight in male and female pups and also decreased survival in pups at day 4. Both the mid-dose and high-dose of fentanyl animals demonstrated alterations in some physical landmarks of development (delayed incisor eruption and eye opening) and transient behavioral development (decreased locomotor activity at day 28 which recovered by day 50). The mid-dose and the high-dose are 0.4 and 1.6 times the daily human dose administered by a 100 mcg/hr patch on a mg/m2 basis.
Labor and Delivery
Fentanyl readily passes across the placenta to the fetus; therefore, DURAGESIC® is not recommended for analgesia during labor and delivery.
Nursing Mothers
Fentanyl is excreted in human milk; therefore, DURAGESIC® is not recommended for use in nursing women because of the possibility of effects in their infants.
Pediatric Use
The safety of DURAGESIC® was evaluated in three open-label trials in 291 pediatric patients with chronic pain, 2 years of age through 18 years of age. Starting doses of 25 mcg/h and higher were used by 181 patients who had been on prior daily opioid doses of at least 45 mg/day of oral morphine or an equianalgesic dose of another opioid. Initiation of DURAGESIC® therapy in pediatric patients taking less than 60 mg/day of oral morphine or an equianalgesic dose of another opioid has not been evaluated in controlled clinical trials. Approximately 90% of the total daily opioid requirement (DURAGESIC® plus rescue medication) was provided by DURAGESIC®.
DURAGESIC® was not studied in children under 2 years of age.
DURAGESIC® should be administered to children only if they are opioid-tolerant and 2 years of age or older (see DOSAGE AND ADMINISTRATION and BOX WARNING).
To guard against accidental ingestion by children, use caution when choosing the application site for DURAGESIC® (see DOSAGE AND ADMINISTRATION) and monitor adhesion of the system closely.
Geriatric Use
Data from intravenous studies with fentanyl suggest that the elderly patients may have reduced clearance and a prolonged half-life. Moreover elderly patients may be more sensitive to the active substance than younger patients. A study conducted with the DURAGESIC® fentanyl transdermal patch in elderly patients demonstrated that fentanyl pharmacokinetics did not differ significantly from young adult subjects, although peak serum concentrations tended to be lower and mean half-life values were prolonged to approximately 34 hours.
Respiratory depression is the chief hazard in elderly or debilitated patients, usually following large initial doses in non-tolerant patients or when opioids are given in conjunction with other agents that depress respiration.
DURAGESIC® should be used with caution in elderly, cachectic, or debilitated patients as they may have altered pharmacokinetics due to poor fat stores, muscle wasting or altered clearance (see DOSAGE AND ADMINISTRATION).
ADVERSE REACTIONS
In post-marketing experience, deaths from hypoventilation due to use of DURAGESIC® (fentanyl transdermal system) have been reported (see BOX WARNING and CONTRAINDICATIONS).
Pre-Marketing Clinical Trial Experience
Although DURAGESIC® use in post-operative or acute pain and in patients who are not opioid-tolerant is CONTRAINDICATED, the safety of DURAGESIC® was originally evaluated in 357 post-operative adult patients for 1 to 3 days and 153 cancer patients for a total of 510 patients. The duration of DURAGESIC® use varied in cancer patients; 56% of patients used DURAGESIC® for over 30 days, 28% continued treatment for more than 4 months, and 10% used DURAGESIC® for more than 1 year.
Hypoventilation was the most serious adverse reaction observed in 13 (4%) post-operative patients and in 3 (2%) of the cancer patients. Hypotension and hypertension were observed in 11 (3%) and 4 (1%) of the opioid-naive patients.
Various adverse events were reported; a causal relationship to DURAGESIC® was not always determined. The frequencies presented here reflect the actual frequency of each adverse effect in patients who received DURAGESIC®. There has been no attempt to correct for a placebo effect, concomitant use of other opioids, or to subtract the frequencies reported by placebo-treated patients in controlled trials.
Adverse reactions reported in 153 cancer patients at a frequency of 1% or greater are presented in Table 1; similar reactions were seen in the 357 post-operative patients.
In the pediatric population, the safety of DURAGESIC® has been evaluated in 291 patients with chronic pain 2–18 years of age. The duration of DURAGESIC® use varied; 20% of pediatric patients were treated for ≤ 15 days; 46% for 16–30 days; 16% for 31–60 days; and 17% for at least 61 days. Twenty-five patients were treated with DURAGESIC® for at least 4 months and 9 patients for more than 9 months.
There was no apparent pediatric-specific risk associated with DURAGESIC® use in children as young as 2 years old when used as directed. The most common adverse events were fever (35%), vomiting (33%), and nausea (24%).
Adverse events reported in pediatric patients at a rate of ≥1% are presented in Table 1.
| Body System | Adults | Pediatrics |
|---|---|---|
| Body as a Whole | Abdominal pain*, headache*, fatigue*, back pain, fever, influenza-like symptoms*, accidental injury, rigors | Pain*, headache*, fever, syncope, abdominal pain, allergic reaction, flushing |
| Cardiovascular | Arrhythmia, chest pain | Hypertension, tachycardia |
| Digestive | Nausea†, vomiting†, constipation†, dry mouth†, anorexia*, diarrhea*, dyspepsia*, flatulence | Nausea†, vomiting†, constipation*, dry mouth, diarrhea |
| Nervous | Somnolence†, insomnia, confusion†, asthenia†, dizziness*, nervousness*, hallucinations*, anxiety*, depression*, euphoria*, tremor, abnormal coordination, speech disorder, abnormal thinking, abnormal gait, abnormal dreams, agitation, paresthesia, amnesia, syncope, paranoid reaction | Somnolence*, nervousness*, insomnia*, asthenia*, hallucinations, anxiety, depression, convulsions, dizziness, tremor, speech disorder, agitation, stupor, confusion, paranoid reaction |
| Respiratory | Dyspnea*, hypoventilation*, apnea*, hemoptysis, pharyngitis*, hiccups, bronchitis, rhinitis, sinusitis, upper respiratory tract infection* | Dyspnea, respiratory depression, rhinitis, coughing |
| Skin and Appendages | Sweating†, pruritus*, rash, application site reaction – erythema, papules, itching, edema | Pruritus*, application site reaction*, sweating increased, rash, rash erythematous, skin reaction localized |
| Urogenital | Urinary retention*, Micturition disorder | Urinary retention |
The following adverse effects have been reported in less than 1% of the 510 adult post-operative and cancer patients studied:
Cardiovascular: bradycardia
Digestive: abdominal distention
Nervous: aphasia, hypertonia, vertigo, stupor, hypotonia, depersonalization, hostility
Respiratory: stertorous breathing, asthma, respiratory disorder
Skin and Appendages, General: exfoliative dermatitis, pustules
Special Senses: amblyopia
Urogenital: bladder pain, oliguria, urinary frequency
Post-Marketing Experience - Adults
The following adverse reactions have been reported in association with the use of DURAGESIC® and not reported in the pre-marketing adverse reactions section above:
Body as a Whole: edema
Cardiovascular: tachycardia
Metabolic and Nutritional: weight loss
Special Senses: blurred vision
Urogenital: decreased libido, anorgasmia, ejaculatory difficulty
DRUG ABUSE AND ADDICTION
DURAGESIC® contains a high concentration of fentanyl, a potent Schedule II opioid agonist. Schedule II opioid substances, which include hydromorphone, methadone, morphine, oxycodone, and oxymorphone, have the highest potential for abuse and risk of fatal overdose due to respiratory depression. Fentanyl, like morphine and other opioids used in analgesia, can be abused and is subject to criminal diversion.
The high content of fentanyl in the patches (DURAGESIC®) may be a particular target for abuse and diversion.
Addiction is a primary, chronic, neurobiologic disease, with genetic, psychosocial, and environmental factors influencing its development and manifestations. It is characterized by behaviors that include one or more of the following: impaired control over drug use, compulsive use, continued use despite harm, and craving. Drug addiction is a treatable disease, utilizing a multidisciplinary approach, but relapse is common.
"Drug seeking" behavior is very common in addicts and drug abusers. Drug-seeking tactics include emergency calls or visits near the end of office hours, refusal to undergo appropriate examination, testing or referral, repeated "loss" of prescriptions, tampering with prescriptions and reluctance to provide prior medical records or contact information for other treating physician(s). "Doctor shopping" to obtain additional prescriptions is common among drug abusers and people suffering from untreated addiction.
Abuse and addiction are separate and distinct from physical dependence and tolerance. Physicians should be aware that addiction may be accompanied by concurrent tolerance and symptoms of physical dependence. In addition, abuse of opioids can occur in the absence of true addiction and is characterized by misuse for non-medical purposes, often in combination with other psychoactive substances. Since DURAGESIC® may be diverted for non-medical use, careful record keeping of prescribing information, including quantity, frequency, and renewal requests is strongly advised.
Proper assessment of the patient, proper prescribing practices, periodic re-evaluation of therapy, and proper dispensing and storage are appropriate measures that help to limit abuse of opioid drugs.
DURAGESIC® patches are intended for transdermal use (to be applied on the skin) only. Do not use a DURAGESIC® patch if the pouch seal is broken or the patch is cut, damaged, or changed in any way.
OVERDOSAGE
Clinical Presentation
The manifestations of fentanyl overdosage are an extension of its pharmacologic actions with the most serious significant effect being hypoventilation.
Treatment
For the management of hypoventilation, immediate countermeasures include removing the DURAGESIC® (fentanyl transdermal system) system and physically or verbally stimulating the patient. These actions can be followed by administration of a specific narcotic antagonist such as naloxone. The duration of hypoventilation following an overdose may be longer than the effects of the narcotic antagonist's action (the half-life of naloxone ranges from 30 to 81 minutes). The interval between IV antagonist doses should be carefully chosen because of the possibility of re-narcotization after system removal; repeated administration of naloxone may be necessary. Reversal of the narcotic effect may result in acute onset of pain and the release of catecholamines.
Always ensure a patent airway is established and maintained, administer oxygen and assist or control respiration as indicated and use an oropharyngeal airway or endotracheal tube if necessary. Adequate body temperature and fluid intake should be maintained.
If severe or persistent hypotension occurs, the possibility of hypovolemia should be considered and managed with appropriate parenteral fluid therapy.
DOSAGE AND ADMINISTRATION
Special Precautions
DURAGESIC® contains a high concentration of a potent Schedule II opioid agonist, fentanyl. Schedule II opioid substances which include fentanyl, hydromorphone, methadone, morphine, oxycodone, and oxymorphone have the highest potential for abuse and associated risk of fatal overdose due to respiratory depression. Fentanyl can be abused and is subject to criminal diversion. The high content of fentanyl in the patches (DURAGESIC®) may be a particular target for abuse and diversion.
DURAGESIC® patches are intended for transdermal use (on intact skin) only. The DURAGESIC® patch should not be used if the pouch seal is broken, or the patch is cut, damaged, or changed in any way.
Each DURAGESIC® patch may be worn continuously for 72 hours. The next patch should be applied to a different skin site after removal of the previous transdermal system.
If problems with adhesion of the DURAGESIC® patch occur, the edges of the patch may be taped with first aid tape. If problems with adhesion persist, the patch may be overlayed with a transparent adhesive film dressing (e.g., Bioclusive™ or Tegaderm™).
If the patch falls off before 72 hours, dispose of it by folding in half and flushing down the toilet. A new patch may be applied to a different skin site.
DURAGESIC® is ONLY for use in patients who are already tolerant to opioid therapy of comparable potency. Use in non-opioid tolerant patients may lead to fatal respiratory depression. Overestimating the DURAGESIC® dose when converting patients from another opioid medication can result in fatal overdose with the first dose. Due to the mean half-life of approximately 20–27 hours, patients who are thought to have had a serious adverse event, including overdose, will require monitoring and treatment for at least 24 hours.
The concomitant use of DURAGESIC® with all cytochrome P450 3A4 inhibitors (such as ritonavir, ketoconazole, itraconazole, troleandomycin, clarithromycin, nelfinavir, nefazodone, amiodarone, amprenavir, aprepitant, diltiazem, erythromycin, fluconazole, fosamprenavir, grapefruit juice, and verapamil) may result in an increase in fentanyl plasma concentrations, which could increase or prolong adverse drug effects and may cause potentially fatal respiratory depression. Patients receiving DURAGESIC® and any CYP3A4 inhibitor should be carefully monitored for an extended period of time and dosage adjustments should be made if warranted (see BOX WARNING, CLINICAL PHARMACOLOGY – Drug Interactions, WARNINGS, and PRECAUTIONS for further information).
Pediatric patients converting to DURAGESIC® with a 25 mcg/h patch should be opioid-tolerant and receiving at least 60 mg of oral morphine or the equivalent per day. The dose conversion schedule described in Table C, and method of titration described below are recommended in opioid-tolerant pediatric patients over 2 years of age with chronic pain (see PRECAUTIONS – Pediatric Use).
Respiratory depression is the chief hazard in elderly or debilitated patients, usually following large initial doses in non-tolerant patients, or when opioids are given in conjunction with other agents that depress respiration.
DURAGESIC® should be used with caution in elderly, cachectic, or debilitated patients as they may have altered pharmacokinetics due to poor fat stores, muscle wasting, or altered clearance (see CLINICAL PHARMACOLOGY – Special Populations, Geriatric Use).
General Principles
DURAGESIC® is indicated for management of persistent, moderate to severe chronic pain that:
- requires continuous, around-the-clock opioid administration for an extended period of time
- cannot be managed by other means such as non-steroidal analgesics, opioid combination products, or immediate-release opioids.
DURAGESIC® should ONLY be used in patients who are already receiving opioid therapy, who have demonstrated opioid tolerance, and who require a total daily dose at least equivalent to DURAGESIC® 25 mcg/h. Patients who are considered opioid-tolerant are those who have been taking, for a week or longer, at least 60 mg of morphine daily, or at least 30 mg of oral oxycodone daily, or at least 8 mg oral hydromorphone daily, or an equianalgesic dose of another opioid.
Because serious or life-threatening hypoventilation could occur, DURAGESIC® (fentanyl transdermal system) is contraindicated:
- in patients who are not opioid-tolerant
- in the management of acute pain or in patients who require opioid analgesia for a short period of time.
- in the management of post-operative pain, including use after out-patient or day surgeries (e.g., tonsillectomies)
- in the management of mild pain
- in the management of intermittent pain (e.g., use on an as needed basis [prn])
(See CONTRAINDICATIONS for further information.)
Safety of DURAGESIC® has not been established in children under 2 years of age. DURAGESIC® should be administered to children only if they are opioid-tolerant and 2 years of age or older (see PRECAUTIONS - Pediatric Use).
Prescribers should individualize treatment using a progressive plan of pain management such as outlined by the World Health Organization, the Agency for Health Research and Quality, the Federation of State Medical Boards Model Policy, or the American Pain Society.
With all opioids, the safety of patients using the products is dependent on health care practitioners prescribing them in strict conformity with their approved labeling with respect to patient selection, dosing, and proper conditions for use.
As with all opioids, dosage should be individualized. The most important factor to be considered in determining the appropriate dose is the extent of pre-existing opioid-tolerance (see BOX WARNING and CONTRAINDICATIONS). Initial doses should be reduced in elderly or debilitated patients (see PRECAUTIONS).
DURAGESIC® (fentanyl transdermal system) should be applied to intact, non-irritated, and non-irradiated skin on a flat surface such as the chest, back, flank, or upper arm. In young children and persons with cognitive impairment, adhesion should be monitored and the upper back is the preferred location to minimize the potential of inappropriate patch removal. Hair at the application site should be clipped (not shaved) prior to system application. If the site of DURAGESIC® application must be cleansed prior to application of the patch, do so with clear water. Do not use soaps, oils, lotions, alcohol, or any other agents that might irritate the skin or alter its characteristics. Allow the skin to dry completely prior to patch application.
DURAGESIC® should be applied immediately upon removal from the sealed package. Do not use if the pouch seal is broken. Do not alter the patch (e.g., cut) in any way prior to application and do not use cut or damaged patches.
The transdermal system should be pressed firmly in place with the palm of the hand for 30 seconds, making sure the contact is complete, especially around the edges.
DURAGESIC® should be kept out of the reach of children. Used patches should be folded so that the adhesive side of the patch adheres to itself, then the patch should be flushed down the toilet immediately upon removal. Patients should dispose of any patches remaining from a prescription as soon as they are no longer needed. Unused patches should be removed from their pouches, folded so that the adhesive side of the patch adheres to itself, and flushed down the toilet.
Dose Selection
Doses must be individualized based upon the status of each patient and should be assessed at regular intervals after DURAGESIC® application. Reduced doses of DURAGESIC® are suggested for the elderly and other groups discussed in PRECAUTIONS.
DURAGESIC® is ONLY for use in patients who are already tolerant to opioid therapy of comparable potency. Use in non-opioid tolerant patients may lead to fatal respiratory depression.
In selecting an initial DURAGESIC® dose, attention should be given to 1) the daily dose, potency, and characteristics of the opioid the patient has been taking previously (e.g., whether it is a pure agonist or mixed agonist-antagonist), 2) the reliability of the relative potency estimates used to calculate the DURAGESIC® dose needed (potency estimates may vary with the route of administration), 3) the degree of opioid tolerance and 4) the general condition and medical status of the patient. Each patient should be maintained at the lowest dose providing acceptable pain control.
Initial DURAGESIC® Dose Selection
Overestimating the DURAGESIC® dose when converting patients from another opioid medication can result in fatal overdose with the first dose. Due to the mean half-life of approximately 20–27 hours, patients who are thought to have had a serious adverse event, including overdose, will require monitoring and treatment for at least 24 hours.
There has been no systematic evaluation of DURAGESIC® as an initial opioid analgesic in the management of chronic pain, since most patients in the clinical trials were converted to DURAGESIC® from other narcotics. The efficacy of DURAGESIC® 12 mcg/h as an initiating dose has not been determined. In addition, patients who are not opioid-tolerant have experienced hypoventilation and death during use of DURAGESIC®. Therefore, DURAGESIC® should be used only in patients who are opioid-tolerant.
To convert adult and pediatric patients from oral or parenteral opioids to DURAGESIC®, use Table C:
Alternatively, for adult and pediatric patients taking opioids or doses not listed in Table C, use the following methodology:
- Calculate the previous 24-hour analgesic requirement.
- Convert this amount to the equianalgesic oral morphine dose using Table D.
- Table E displays the range of 24-hour oral morphine doses that are recommended for conversion to each DURAGESIC® dose. Use this table to find the calculated 24-hour morphine dose and the corresponding DURAGESIC® dose. Initiate DURAGESIC® treatment using the recommended dose and titrate patients upwards (no more frequently than every 3 days after the initial dose or than every 6 days thereafter) until analgesic efficacy is attained. The recommended starting dose when converting from other opioids to DURAGESIC® is likely too low for 50% of patients. This starting dose is recommended to minimize the potential for overdosing patients with the first dose. For delivery rates in excess of 100 mcg/h, multiple systems may be used.
| Current Analgesic | Daily Dosage (mg/d) | |||
|---|---|---|---|---|
| Alternatively, for adult and pediatric patients taking opioids or doses not listed in Table C, use the conversion methodology outlined above with Table D. | ||||
|
||||
| Oral morphine | 60–134 | 135–224 | 225–314 | 315–404 |
| IM/IV morphine | 10–22 | 23–37 | 38–52 | 53–67 |
| Oral oxycodone | 30–67 | 67.5–112 | 112.5–157 | 157.5–202 |
| IM/IV oxycodone | 15–33 | 33.1–56 | 56.1–78 | 78.1–101 |
| Oral codeine | 150–447 | 448–747 | 748–1047 | 1048–1347 |
| Oral hydromorphone | 8–17 | 17.1–28 | 28.1–39 | 39.1–51 |
| IV hydromorphone | 1.5–3.4 | 3.5–5.6 | 5.7–7.9 | 8–10 |
| IM meperidine | 75–165 | 166–278 | 279–390 | 391–503 |
| Oral methadone | 20–44 | 45–74 | 75–104 | 105–134 |
| IM methadone | 10–22 | 23–37 | 38–52 | 53–67 |
| ⇓ | ⇓ | ⇓ | ⇓ | |
| Recommended DURAGESIC® Dose | 25 mcg/h | 50 mcg/h | 75 mcg/h | 100 mcg/h |
| Name | Equianalgesic Dose (mg) | |
|---|---|---|
| IM‡,§ | PO | |
|
||
| Morphine | 10 | 60 (30)¶ |
| Hydromorphone (Dilaudid®) | 1.5 | 7.5 |
| Methadone (Dolophine®) | 10 | 20 |
| Oxycodone | 15 | 30 |
| Levorphanol (Levo-Dromoran®) | 2 | 4 |
| Oxymorphone (Numorphan®) | 1 | 10 (PR) |
| Meperidine (Demerol®) | 75 | — |
| Codeine | 130 | 200 |
| Oral 24-hour Morphine (mg/day) | DURAGESIC®
Dose (mcg/h) |
|---|---|
| NOTE: In clinical trials, these ranges of daily oral morphine doses were used as a basis for conversion to DURAGESIC®. | |
|
|
| 60–134 | 25 |
| 135–224 | 50 |
| 225–314 | 75 |
| 315–404 | 100 |
| 405–494 | 125 |
| 495–584 | 150 |
| 585–674 | 175 |
| 675–764 | 200 |
| 765–854 | 225 |
| 855–944 | 250 |
| 945–1034 | 275 |
| 1035–1124 | 300 |
The majority of patients are adequately maintained with DURAGESIC® administered every 72 hours. Some patients may not achieve adequate analgesia using this dosing interval and may require systems to be applied every 48 hours rather than every 72 hours. An increase in the DURAGESIC® dose should be evaluated before changing dosing intervals in order to maintain patients on a 72-hour regimen. Dosing intervals less than every 72 hours were not studied in children and adolescents and are not recommended.
Because of the increase in serum fentanyl concentration over the first 24 hours following initial system application, the initial evaluation of the maximum analgesic effect of DURAGESIC® cannot be made before 24 hours of wearing. The initial DURAGESIC® dose may be increased after 3 days (see DOSAGE AND ADMINISTRATION - Dose Titration).
During the initial application of DURAGESIC®, patients should use short-acting analgesics as needed until analgesic efficacy with DURAGESIC® is attained. Thereafter, some patients still may require periodic supplemental doses of other short-acting analgesics for "breakthrough" pain.
Dose Titration
The recommended initial DURAGESIC® dose based upon the daily oral morphine dose is conservative, and 50% of patients are likely to require a dose increase after initial application of DURAGESIC®. The initial DURAGESIC® dose may be increased after 3 days based on the daily dose of supplemental opioid analgesics required by the patient in the second or third day of the initial application.
Physicians are advised that it may take up to 6 days after increasing the dose of DURAGESIC® for the patient to reach equilibrium on the new dose (see graph in CLINICAL PHARMACOLOGY). Therefore, patients should wear a higher dose through two applications before any further increase in dosage is made on the basis of the average daily use of a supplemental analgesic.
Appropriate dosage increments should be based on the daily dose of supplementary opioids, using the ratio of 45 mg/24 hours of oral morphine to a 12.5 mcg/h increase in DURAGESIC® dose. DURAGESIC®-12 delivers 12.5 mcg/h of fentanyl.
Discontinuation of DURAGESIC®
To convert patients to another opioid, remove DURAGESIC® and titrate the dose of the new analgesic based upon the patient's report of pain until adequate analgesia has been attained. Upon system removal, 17 hours or more are required for a 50% decrease in serum fentanyl concentrations. Opioid withdrawal symptoms (such as nausea, vomiting, diarrhea, anxiety, and shivering) are possible in some patients after conversion or dose adjustment. For patients requiring discontinuation of opioids, a gradual downward titration is recommended since it is not known at what dose level the opioid may be discontinued without producing the signs and symptoms of abrupt withdrawal.
Tables C, D, and E should not be used to convert from DURAGESIC® to other therapies. Because the conversion to DURAGESIC® is conservative, use of Tables C, D, and E for conversion to other analgesic therapies can overestimate the dose of the new agent. Overdosage of the new analgesic agent is possible.
HOW SUPPLIED
DURAGESIC® (fentanyl transdermal system) is supplied in cartons containing 5 individually packaged systems. See chart for information regarding individual systems.
| DURAGESIC® Dose (mcg/h) | System Size (cm2) | Fentanyl Content (mg) | NDC Number |
|---|---|---|---|
| DURAGESIC®-12 | 5.25 | 2.1 | 50458-090-05 |
| DURAGESIC®-25 | 10.5 | 4.2 | 50458-091-05 |
| DURAGESIC®-50 | 21 | 8.4 | 50458-092-05 |
| DURAGESIC®-75 | 31.5 | 12.6 | 50458-093-05 |
| DURAGESIC®-100 | 42 | 16.8 | 50458-094-05 |
Safety and Handling
DURAGESIC® is supplied in sealed transdermal systems which pose little risk of exposure to health care workers. Do not use a DURAGESIC® patch if the pouch seal is broken or the patch is cut, damaged, or changed in any way.
KEEP DURAGESIC® OUT OF THE REACH OF CHILDREN AND PETS.
Store in original unopened pouch. Store up to 25°C (77°F); excursions permitted to 15 – 30°C (59 – 86°F). Apply immediately after removal from individually sealed pouch. Do not use if the pouch seal is broken. For transdermal use only.
Bioclusive™ is a trademark of Ethicon, Inc.
Tegaderm™ is a trademark of 3M
A schedule CII narcotic. DEA order form required.
Manufactured by:
ALZA Corporation
Vacaville, CA 95688
Manufactured for:
PriCara®, Division of Ortho-McNeil-Janssen Pharmaceuticals, Inc.
Raritan, NJ 08869
Insert new code
Revised July 2009
© Ortho-McNeil-Janssen Pharmaceuticals, Inc. 2009
MEDICATION GUIDE
DURAGESIC®
(Dur-ah-GEE-zik)
(FENTANYL TRANSDERMAL SYSTEM)
CII
IMPORTANT:
- Keep DURAGESIC® in a safe place away from children and pets. Accidental use by a child or pet is a medical emergency and may result in death. If a child or pet accidentally uses DURAGESIC®, get emergency help right away.
- Make sure you read the separate "Instructions for Applying a DURAGESIC® Patch." Always use a DURAGESIC® Patch the right way. DURAGESIC® can cause serious breathing problems and death, especially if it is used the wrong way.
- DURAGESIC® is a federally controlled substance (C-II) because it can be abused. Keep DURAGESIC® in a safe place to prevent theft. Selling or giving away DURAGESIC® may harm others, and is against the law.
- Tell your doctor if you (or a family member) have ever abused or been dependent on alcohol, prescription medicines or street drugs.
Read the Medication Guide that comes with DURAGESIC® before you start using it and each time you get a new prescription. There may be new information. This Medication Guide does not take the place of talking to your healthcare provider about your medical condition or your treatment. Make sure you read and understand all the instructions for using DURAGESIC®. Do not use DURAGESIC® unless you understand everything. Talk to your healthcare provider if you have questions.
What is the most important information I should know about DURAGESIC®?
DURAGESIC® is a skin patch that contains fentanyl. Fentanyl is a very strong opioid narcotic pain medicine that can cause serious and life-threatening breathing problems. Serious and life-threatening breathing problems can happen because of an overdose or if the dose you are using is too high for you. Call your doctor right away or get emergency medical help if you:
- have trouble breathing, or have slow or shallow breathing
- have a slow heartbeat
- have severe sleepiness
- have cold, clammy skin
- feel faint, dizzy, confused, or cannot think, walk, or talk normally
- have a seizure
- have hallucinations
DURAGESIC® is only for adults and children over the age of two with persistent, moderate to severe chronic pain and who:
- are already using another strong opioid narcotic pain medicine around-the-clock, and have been using the medicine regularly for a week or longer. This is called being opioid-tolerant.
- have pain that cannot be controlled with other medicines
Do not use DURAGESIC®:
- if you are not already using another opioid narcotic medicine and are not opioid tolerant
- if you need opioid pain medicines for only a short time
- for pain from surgery, medical or dental procedures
- if your pain can be taken care of by occasional use of other pain medicines
- in children who are less than 2 years of age
- if you have asthma symptoms or have severe asthma
A DURAGESIC® patch must be used only on the skin of the person for whom it was prescribed. If the patch comes off and accidentally sticks to the skin of another person, take the patch off of that person right away, wash the area with water, and get medical care for them right away.
DURAGESIC® patch is not safe for everyone. Tell your doctor about all of your medical conditions.
Tell your doctor if you are planning to become pregnant, are pregnant, or breastfeeding. DURAGESIC® may cause serious harm to a baby.
Tell your doctor about all the medicines you take. Some medicines may cause serious or life-threatening side effects when used with DURAGESIC®. Your doctor will tell you if it is safe to take other medicines while you are using DURAGESIC®.
Know the medicines you take. Keep a list of your medicines to show to your doctor and pharmacist.
How should I use DURAGESIC®?
Read the separate "Instructions for Applying a DURAGESIC® Patch".
-
You must always use DURAGESIC® patches the right way:
- Do not use a DURAGESIC® patch if the pouch seal is broken, or the patch is cut, damaged, or changed in any way.
- Do not use heat sources such as heating pads, electric blankets, heat lamps, tanning lamps, saunas, hot tubs, or heated waterbeds while wearing a DURAGESIC® patch.
- Do not take hot baths or sunbathe while wearing a DURAGESIC® patch.
-
If you have problems with the DURAGESIC® patch not sticking:
- Apply first aid tape only to the edges of the patch.
- If problems with the patch not sticking persist, cover the patch with Bioclusive™ or Tegaderm™. These are special see-through adhesive dressings. Never cover a DURAGESIC® patch with any other bandage or tape.
- If your DURAGESIC® patch falls off before 3 days or 72 hours, fold the sticky side together and flush down a toilet. Put a new one on at a different skin site.
- Do not change your dose unless your doctor tells you to. Your doctor may change your dose after seeing how the medicine affects you. Do not use DURAGESIC® more often than prescribed. Call your doctor if your pain is not well controlled while using DURAGESIC®.
- Do not stop using DURAGESIC® suddenly. Stopping DURAGESIC® suddenly can make you sick with withdrawal symptoms (for example, nausea, vomiting, diarrhea, anxiety, and shivering). Your body can develop a physical dependence on DURAGESIC®. If your doctor decides you no longer need DURAGESIC®, ask how to slowly reduce this medicine so you don't have withdrawal symptoms. Do not stop taking DURAGESIC® without talking to your doctor.
- Do not wear more than one DURAGESIC® patch at a time, unless your doctor tells you to do so.
-
Call your doctor right away if
- You get a fever higher than 102°F
- Your body temperature increases from exercise
A fever or increase in body temperature may cause too much of the medicine in DURAGESIC® to pass into your body.
- If you use more DURAGESIC® than your doctor has prescribed, get emergency medical help right away.
- Do not drink any alcohol while using DURAGESIC®. Alcohol can increase your chances of having serious side effects.
- Do not drive, operate heavy machinery, or do other possibly dangerous activities until you know how DURAGESIC® affects you. DURAGESIC® can make you sleepy. Ask your doctor to tell you when it is okay to do these activities.
- When you remove your DURAGESIC® patch, fold the sticky sides of a used DURAGESIC® patch together and flush it down the toilet. Do not put used DURAGESIC® patches in a trash can.
What are the possible side effects of DURAGESIC®?
Serious side effects include:
- Life-threatening breathing problems. See "What is the most important information I should know about DURAGESIC®?"
- Low blood pressure. This can make you feel dizzy if you get up too fast from sitting or lying down.
The common side effects with DURAGESIC® are nausea, vomiting, constipation, dry mouth, sleepiness, confusion, weakness, sweating, and pain and redness where the patch was applied.
Constipation is a very common side effect of all opioid medicines. Talk to your doctor about the use of laxatives and stool softeners to prevent or treat constipation while taking DURAGESIC®.
Talk to your doctor about any side effect that concerns you.
These are not all the possible side effects of DURAGESIC®. For a complete list, ask your doctor or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store DURAGESIC®?
- Store in original unopened pouch at room temperature.
- Keep a DURAGESIC® patch in its protective pouch until you are ready to use it.
- Keep DURAGESIC® in a safe place out of the reach of children and pets.
- Dispose of DURAGESIC® patches you no longer need. Open the unused packages, fold the sticky sides of the patches together, and flush them down the toilet.
General information about the safe and effective use of DURAGESIC®
- Do not use DURAGESIC® for a condition for which it was not prescribed.
- Do not give DURAGESIC® to other people, even if they have the same symptoms you have. DURAGESIC® can harm other people and even cause death. Sharing DURAGESIC® is against the law.
This Medication Guide summarizes the most important information about DURAGESIC®. If you would like more information, talk with your doctor. You can ask your doctor or pharmacist for information about DURAGESIC® that is written for doctors.
For questions about DURAGESIC®, call the Ortho-McNeil Janssen Scientific Affairs Customer Communications Center at 1-800-526-7736. If this is a medical emergency, please call 911.
What are the ingredients of DURAGESIC®?
Active Ingredient: fentanyl
Inactive ingredients: polyester/ethyl vinyl acetate film backing, polyacrylate adhesive.
This Medication Guide has been approved by the United States Food and Drug Administration.
Bioclusive™ is a trademark of Ethicon, Inc.
Tegaderm™ is a trademark of 3M
Manufactured by:
ALZA Corporation
Vacaville, CA 95688
Manufactured for:
PriCara®, Division of Ortho-McNeil-Janssen Pharmaceuticals, Inc.
Raritan, NJ 08869
Insert New Code
July 2009
© Ortho-McNeil-Janssen Pharmaceuticals, Inc. 2009
DURAGESIC® (Dur-ah-GEE-zik)
(Fentanyl Transdermal System) CII
Instructions for Applying a DURAGESIC® patch
Before Applying DURAGESIC®
- Each DURAGESIC® patch is sealed in its own protective pouch. Do not remove a DURAGESIC® patch from the pouch until you are ready to use it.
- Do not use a DURAGESIC® patch if the pouch seal is broken or the patch is cut, damaged or changed in any way.
- DURAGESIC® patches are available in 5 different doses and patch sizes. Make sure you have the right dose patch or patches that have been prescribed for you.
Applying a DURAGESIC® Patch
| Figure 1 Figure 2 Figure 3
Figure 4
Figure 5 |
| |
| Figure 6 |
| Figure 7 |
| Figure 8 |
| |
| |
Water and DURAGESIC®
| |
| Figure 9 Figure 10 |
Bioclusive™ is a trademark of Ethicon, Inc.
Tegaderm™ is a trademark of 3M
Rx Only
Manufactured by:
ALZA Corporation
Vacaville, CA 95688
Manufactured for:
PriCara®, Division of Ortho-McNeil-Janssen Pharmaceuticals, Inc.
Raritan, NJ 08869
July 2009
Insert new code
© Ortho-McNeil-Janssen Pharmaceuticals, Inc. 2009
PRINCIPAL DISPLAY PANEL - Foil Pouch
NDC 50458-091-05
One (25mcg/h) System
DURAGESIC® 25mcg/h
CII
(FENTANYL TRANSDERMAL SYSTEM)
In vivo delivery of 25mcg/h fentanyl for 72 hours
Each transdermal system contains: 4.2mg fentanyl
Because it can cause trouble breathing which
can be fatal, DO NOT USE DURAGESIC®:
-
For short term or any post-operative pain, or
occasional pain -
For mild pain or pain that can be treated with
non-opioid or as-needed opioid medication -
Unless you have been using other narcotic
opioid medicines (must be opioid tolerant)
Read enclosed DURAGESIC® Medication Guide
for important safety information.
KEEP OUT OF REACH OF CHILDREN
Rx only
ONLY for pain requiring
opioid medicine
around-the-
clock
PriCara®
Division of Ortho-McNeil-Janssen
Pharmaceuticals, Inc.
0017977-2
Revised May 2009
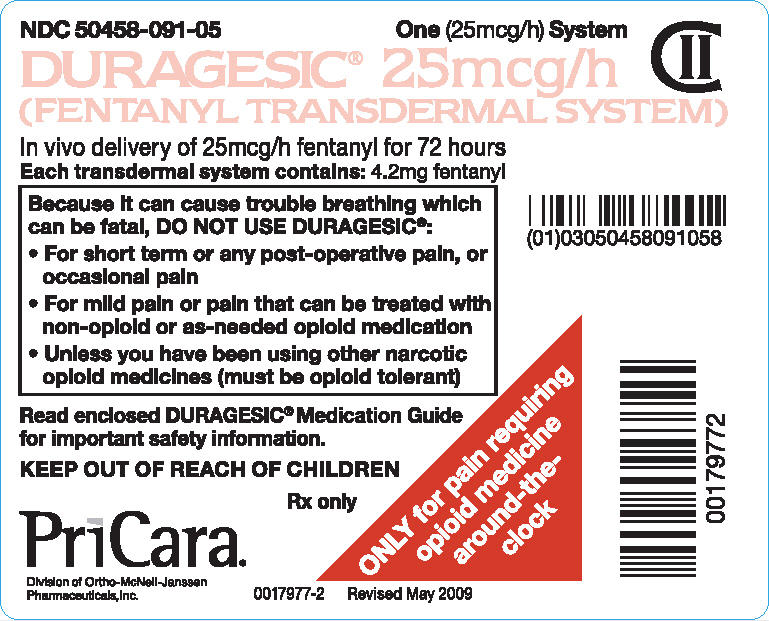
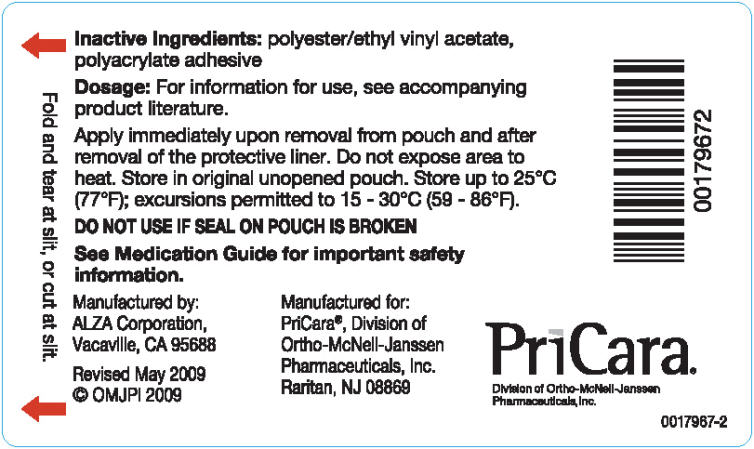
PRINCIPAL DISPLAY PANEL - Foil Pouch Carton
NDC 50458-091-05
Five (25mcg/h) Systems
DURAGESIC® 25 mcg/h
CII
(FENTANYL TRANSDERMAL SYSTEM)
In vivo delivery of 25mcg/h fentanyl for 72 hours
Because it can cause trouble breathing which can be fatal,
DO NOT USE DURAGESIC®:
- For short term or any post-operative pain, or occasional pain
-
For mild pain or pain that can be treated with non-opioid or
as-needed opioid medication -
Unless you have been using other narcotic opioid medicines
(must be opioid tolerant)
Each transdermal system contains: 4.2mg fentanyl
DO NOT USE IF SEAL ON POUCH IS BROKEN
KEEP OUT OF REACH OF CHILDREN
Read enclosed DURAGESIC® Medication Guide
for important safety information.
Rx only
ONLY for pain requiring
opioid medicine
around-the-
clock
PriCara®
Division of Ortho-McNeil-Janssen
Pharmaceuticals, Inc.
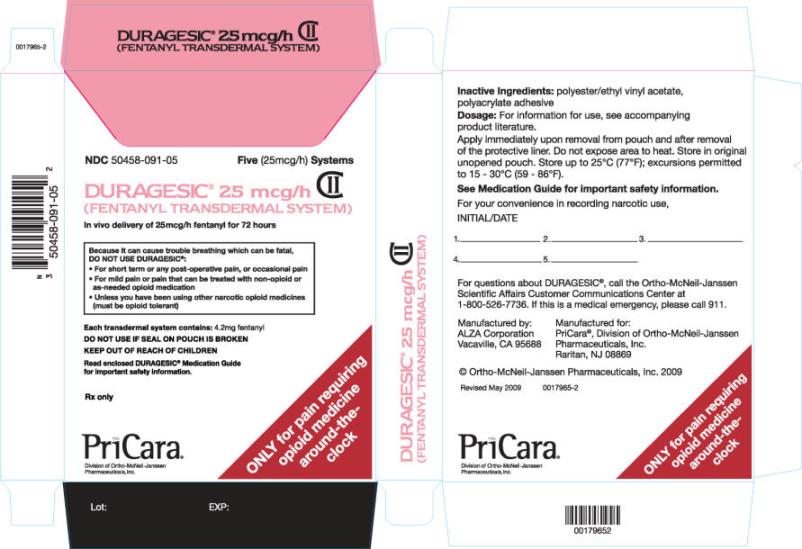
| DURAGESIC
fentanyl patch |
|||||||||||||||||||||
|
|||||||||||||||||||||
|
|||||||||||||||||||||
|
|||||||||||||||||||||
|
|||||||||||||||||||||
|
|||||||||||||||||||||
| Marketing Information | |||
| Marketing Category | Application Number or Monograph Citation | Marketing Start Date | Marketing End Date |
| NDA | NDA019813 | 08/07/1990 | |
| DURAGESIC
fentanyl patch |
|||||||||||||||||||||
|
|||||||||||||||||||||
|
|||||||||||||||||||||
|
|||||||||||||||||||||
|
|||||||||||||||||||||
|
|||||||||||||||||||||
| Marketing Information | |||
| Marketing Category | Application Number or Monograph Citation | Marketing Start Date | Marketing End Date |
| NDA | NDA019813 | 08/07/1990 | |
| DURAGESIC
fentanyl patch |
|||||||||||||||||||||
|
|||||||||||||||||||||
|
|||||||||||||||||||||
|
|||||||||||||||||||||
|
|||||||||||||||||||||
|
|||||||||||||||||||||
| Marketing Information | |||
| Marketing Category | Application Number or Monograph Citation | Marketing Start Date | Marketing End Date |
| NDA | NDA019813 | 08/07/1990 | |
| DURAGESIC
fentanyl patch |
|||||||||||||||||||||
|
|||||||||||||||||||||
|
|||||||||||||||||||||
|
|||||||||||||||||||||
|
|||||||||||||||||||||
|
|||||||||||||||||||||
| Marketing Information | |||
| Marketing Category | Application Number or Monograph Citation | Marketing Start Date | Marketing End Date |
| NDA | NDA019813 | 08/07/1990 | |
| DURAGESIC
fentanyl patch |
|||||||||||||||||||||
|
|||||||||||||||||||||
|
|||||||||||||||||||||
|
|||||||||||||||||||||
|
|||||||||||||||||||||
|
|||||||||||||||||||||
| Marketing Information | |||
| Marketing Category | Application Number or Monograph Citation | Marketing Start Date | Marketing End Date |
| NDA | NDA019813 | 08/07/1990 | |
| Labeler - Ortho-McNeil-Janssen Pharmaceuticals, Inc. (063137772) |
| Establishment | |||
| Name | Address | ID/FEI | Operations |
| Alza Corporation | 175417641 | MANUFACTURE, ANALYSIS | |
| Establishment | |||
| Name | Address | ID/FEI | Operations |
| Johnson Matthey Inc. | 002326734 | MANUFACTURE | |









