AVASTIN
-
bevacizumab injection, solution
Genentech, Inc.
----------
|
||||||||||||||||||||||
FULL PRESCRIBING INFORMATION
WARNING: GASTROINTESTINAL PERFORATIONS, SURGERY AND WOUND HEALING COMPLICATIONS, and HEMORRHAGE
Gastrointestinal Perforations
The incidence of gastrointestinal perforation, some fatal, in Avastin‑treated patients ranges from 0.3 to 2.4%. Discontinue Avastin in patients with gastrointestinal perforation. [ See Dosage and Administration (2.4), Warnings and Precautions (5.1). ]
Surgery and Wound Healing Complications
The incidence of wound healing and surgical complications, including serious and fatal complications, is increased in Avastin‑treated patients. Discontinue Avastin in patients with wound dehiscence. The appropriate interval between termination of Avastin and subsequent elective surgery required to reduce the risks of impaired wound healing/wound dehiscence has not been determined. Discontinue at least 28 days prior to elective surgery. Do not initiate Avastin for at least 28 days after surgery and until the surgical wound is fully healed. [ See Dosage and Administration (2.4), Warnings and Precautions (5.2), and Adverse Reactions (6.1). ]
Hemorrhage
Severe or fatal hemorrhage, including hemoptysis, gastrointestinal bleeding, central nervous systems (CNS) hemorrhage, epistaxis, and vaginal bleeding occurred up to five‑fold more frequently in patients receiving Avastin. Do not administer Avastin to patients with serious hemorrhage or recent hemoptysis. [ See Dosage and Administration (2.4), Warnings and Precautions (5.3), and Adverse Reactions (6.1). ]
1 INDICATIONS AND USAGE
1.1 Metastatic Colorectal Cancer (mCRC)
Avastin is indicated for the first‑ or second‑line treatment of patients with metastatic carcinoma of the colon or rectum in combination with intravenous 5‑fluorouracil‑based chemotherapy.
1.2 Non‑Squamous Non‑Small Cell Lung Cancer (NSCLC)
Avastin is indicated for the first‑line treatment of unresectable, locally advanced, recurrent or metastatic non‑squamous non‑small cell lung cancer in combination with carboplatin and paclitaxel.
1.3 Metastatic Breast Cancer (MBC)
Avastin is indicated for the treatment of patients who have not received chemotherapy for metastatic HER2‑negative breast cancer in combination with paclitaxel.
The effectiveness of Avastin in MBC is based on an improvement in progression free survival. There are no data demonstrating an improvement in disease‑related symptoms or increased survival with Avastin. [ See Clinical Studies (14.3). ]
Avastin is not indicated for patients with breast cancer that has progressed following anthracycline and taxane chemotherapy administered for metastatic disease.
1.4 Glioblastoma
Avastin is indicated for the treatment of glioblastoma with progressive disease following prior therapy as a single agent.
1.5 Metastatic Renal Cell Carcinoma (mRCC)
2 DOSAGE AND ADMINISTRATION
2.1 Administration
Do not administer as an intravenous push or bolus. Administer only as an intravenous (IV) infusion.
- Do not initiate Avastin until at least 28 days following major surgery. Administer Avastin after the surgical incision has fully healed.
- First infusion: Administer infusion over 90 minutes.
- Subsequent infusions: Administer second infusion over 60 minutes if first infusion is tolerated; administer all subsequent infusions over 30 minutes if infusion over 60 minutes is tolerated.
2.2 Recommended Doses and Schedules
Patients should continue treatment until disease progression or unacceptable toxicity.
Metastatic Colorectal Cancer (mCRC)
The recommended doses are 5 mg/kg or 10 mg/kg every 2 weeks when used in combination with intravenous 5‑FU‑based chemotherapy.
- Administer 5 mg/kg when used in combination with bolus‑IFL.
- Administer 10 mg/kg when used in combination with FOLFOX4.
Non‑Squamous Non‑Small Cell Lung Cancer (NSCLC)
The recommended dose is 15 mg/kg every 3 weeks in combination with carboplatin and paclitaxel.
Metastatic Breast Cancer (MBC)
The recommended dose is 10 mg/kg every 2 weeks in combination with paclitaxel.
Glioblastoma
The recommended dose is 10 mg/kg every 2 weeks.
Metastatic Renal Cell Carcinoma (mRCC)
2.3 Preparation for Administration
Use appropriate aseptic technique. Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit. Withdraw necessary amount of Avastin and dilute in a total volume of 100 mL of 0.9% Sodium Chloride Injection, USP. Discard any unused portion left in a vial, as the product contains no preservatives.
DO NOT ADMINISTER OR MIX WITH DEXTROSE SOLUTION.
2.4 Dose Modifications
There are no recommended dose reductions.
Discontinue Avastin for:
- Gastrointestinal perforations (gastrointestinal perforations, fistula formation in the gastrointestinal tract, intra‑abdominal abscess), fistula formation involving an internal organ [ See Boxed Warning , Warnings and Precautions (5.1, 5.4). ]
- Wound dehiscence and wound healing complications requiring medical intervention [ See Warnings and Precautions (5.2). ]
- Serious hemorrhage (i.e., requiring medical intervention) [ See Boxed Warning , Warnings and Precautions (5.3). ]
- Severe arterial thromboembolic events [ See Warnings and Precautions (5.5). ]
- Hypertensive crisis or hypertensive encephalopathy [ See Warnings and Precautions (5.6). ]
- Reversible posterior leukoencephalopathy syndrome (RPLS) [ See Warnings and Precautions (5.7). ]
- Nephrotic syndrome [ See Warnings and Precautions (5.8). ]
Temporarily suspend Avastin for:
- At least 4 weeks prior to elective surgery [ See Warnings and Precautions (5.2). ]
- Severe hypertension not controlled with medical management [ See Warnings and Precautions (5.6). ]
- Moderate to severe proteinuria pending further evaluation [ See Warnings and Precautions (5.8). ]
- Severe infusion reactions [ See Warnings and Precautions (5.9). ]
3 DOSAGE FORMS AND STRENGTHS
100 mg per 4 mL single‑use vial
400 mg per 16 mL single‑use vial
4 CONTRAINDICATIONS
None.
5 WARNINGS AND PRECAUTIONS
5.1 Gastrointestinal Perforations
Serious and sometimes fatal gastrointestinal perforation occurs at a higher incidence in Avastin treated patients compared to controls. The incidence of gastrointestinal perforation ranged from 0.3 to 2.4% across clinical studies. [ See Adverse Reactions (6.1). ]
The typical presentation may include abdominal pain, nausea, emesis, constipation, and fever. Perforation can be complicated by intra‑abdominal abscess and fistula formation. The majority of cases occurred within the first 50 days of initiation of Avastin.
Discontinue Avastin in patients with gastrointestinal perforation. [ See Boxed Warning, Dosage and Administration (2.4). ]
5.2 Surgery and Wound Healing Complications
Avastin impairs wound healing in animal models. [ See Nonclinical Toxicology (13.2). ] In clinical trials, administration of Avastin was not allowed until at least 28 days after surgery. In a controlled clinical trial, the incidence of wound healing complications, including serious and fatal complications, in patients with mCRC who underwent surgery during the course of Avastin treatment was 15% and in patients who did not receive Avastin, was 4%. [ See Adverse Reactions (6.1). ]
Avastin should not be initiated for at least 28 days following surgery and until the surgical wound is fully healed. Discontinue Avastin in patients with wound healing complications requiring medical intervention.
The appropriate interval between the last dose of Avastin and elective surgery is unknown; however, the half‑life of Avastin is estimated to be 20 days. Suspend Avastin for at least 28 days prior to elective surgery. Do not administer Avastin until the wound is fully healed. [ See Boxed Warning , Dosage and Administration (2.4). ]
5.3 Hemorrhage
Avastin can result in two distinct patterns of bleeding: minor hemorrhage, most commonly Grade 1 epistaxis; and serious, and in some cases fatal, hemorrhagic events. Severe or fatal hemorrhage, including hemoptysis, gastrointestinal bleeding, hematemesis, CNS hemorrhage, epistaxis, and vaginal bleeding occurred up to five‑fold more frequently in patients receiving Avastin compared to patients receiving only chemotherapy. Across indications, the incidence of Grade ≥3 hemorrhagic events among patients receiving Avastin ranged from 1.2 to 4.6%. [ See Adverse Reactions (6.1). ]
Serious or fatal pulmonary hemorrhage occurred in four of 13 (31%) patients with squamous cell histology and two of 53 (4%) patients with non‑squamous non‑small cell lung cancer receiving Avastin and chemotherapy compared to none of the 32 (0%) patients receiving chemotherapy alone.
Intracranial hemorrhage occurred in 8 of 163 patients with previously treated glioblastoma; two patients had Grade 3–4 hemorrhage.
Do not administer Avastin to patients with recent history of hemoptysis of ≥1/2 teaspoon of red blood. Discontinue Avastin in patients with hemorrhage. [ See Boxed Warning, Dosage and Administration (2.4). ]
5.4 Non‑Gastrointestinal Fistula Formation
Serious and sometimes fatal non‑gastrointestinal fistula formation involving tracheo‑esophageal, bronchopleural, biliary, vaginal, renal and bladder sites occurs at a higher incidence in Avastin‑treated patients compared to controls. The incidence of non‑gastrointestinal perforation was ≤0.3% in clinical studies. Most events occurred within the first 6 months of Avastin therapy.
Discontinue Avastin in patients with fistula formation involving an internal organ. [ See Dosage and Administration (2.4). ]
5.5 Arterial Thromboembolic Events
Serious, sometimes fatal, arterial thromboembolic events (ATE) including cerebral infarction, transient ischemic attacks, myocardial infarction, angina, and a variety of other ATE occurred at a higher incidence in patients receiving Avastin compared to those in the control arm. Across indications, the incidence of Grade ≥ 3 ATE in the Avastin containing arms was 2.4% compared to 0.7% in the control arms. Among patients receiving Avastin in combination with chemotherapy, the risk of developing ATE during therapy was increased in patients with a history of arterial thromboembolism, or age greater than 65 years. [ See Use in Specific Populations (8.5). ]
The safety of resumption of Avastin therapy after resolution of an ATE has not been studied. Discontinue Avastin in patients who experience a severe ATE. [ See Dosage and Administration (2.4). ]
5.6 Hypertension
The incidence of severe hypertension is increased in patients receiving Avastin as compared to controls. Across clinical studies the incidence of Grade 3 or 4 hypertension ranged from 5–18%.
Monitor blood pressure every two to three weeks during treatment with Avastin. Treat with appropriate anti‑hypertensive therapy and monitor blood pressure regularly. Continue to monitor blood pressure at regular intervals in patients with Avastin‑induced or ‑exacerbated hypertension after discontinuation of Avastin.
Temporarily suspend Avastin in patients with severe hypertension that is not controlled with medical management. Discontinue Avastin in patients with hypertensive crisis or hypertensive encephalopathy. [ See Dosage and Administration (2.4). ]
5.7 Reversible Posterior Leukoencephalopathy Syndrome (RPLS)
RPLS has been reported with an incidence of <0.1% in clinical studies. The onset of symptoms occurred from 16 hours to 1 year after initiation of Avastin. RPLS is a neurological disorder which can present with headache, seizure, lethargy, confusion, blindness and other visual and neurologic disturbances. Mild to severe hypertension may be present. Magnetic resonance imaging (MRI) is necessary to confirm the diagnosis of RPLS.
Discontinue Avastin in patients developing RPLS. Symptoms usually resolve or improve within days, although some patients have experienced ongoing neurologic sequelae. The safety of reinitiating Avastin therapy in patients previously experiencing RPLS is not known. [ See Dosage and Administration (2.4). ]
5.8 Proteinuria
The incidence and severity of proteinuria is increased in patients receiving Avastin as compared to controls. Nephrotic syndrome occurred in < 1% of patients receiving Avastin in clinical trials, in some instances with fatal outcome. [ See Adverse Reactions (6.1). ] In a published case series, kidney biopsy of six patients with proteinuria showed findings consistent with thrombotic microangiopathy.
Monitor proteinuria by dipstick urine analysis for the development or worsening of proteinuria with serial urinalyses during Avastin therapy. Patients with a 2+ or greater urine dipstick reading should undergo further assessment with a 24‑hour urine collection.
Suspend Avastin administration for ≥ 2 grams of proteinuria/24 hours and resume when proteinuria is < 2 gm/24 hours. Discontinue Avastin in patients with nephrotic syndrome. Data from a postmarketing safety study showed poor correlation between UPCR (Urine Protein/Creatinine Ratio) and 24 hour urine protein (Pearson Correlation 0.39 (95% CI 0.17, 0.57). [ See Use in Specific Populations (8.5). ] The safety of continued Avastin treatment in patients with moderate to severe proteinuria has not been evaluated. [ See Dosage and Administration (2.4). ]
5.9 Infusion Reactions
Infusion reactions reported in the clinical trials and post‑marketing experience include hypertension, hypertensive crises associated with neurologic signs and symptoms, wheezing, oxygen desaturation, Grade 3 hypersensitivity, chest pain, headaches, rigors, and diaphoresis. In clinical studies, infusion reactions with the first dose of Avastin were uncommon (< 3%) and severe reactions occurred in 0.2% of patients.
Stop infusion if a severe infusion reaction occurs and administer appropriate medical therapy. [ See Dosage and Administration (2.4). ]
6 ADVERSE REACTIONS
The following serious adverse reactions are discussed in greater detail in other sections of the label:
- Gastrointestinal Perforations [ See Boxed Warning , Dosage and Administration (2.4), Warnings and Precautions (5.1). ]
- Surgery and Wound Healing Complications [ See Boxed Warning, Dosage and Administration (2.4), Warnings and Precautions (5.2). ]
- Hemorrhage [ See Boxed Warning, Dosage and Administration (2.4), Warnings and Precautions (5.3). ]
- Non‑Gastrointestinal Fistula Formation [ See Dosage and Administration (2.4), Warnings and Precautions (5.4). ]
- Arterial Thromboembolic Events [ See Dosage and Administration (2.4), Warnings and Precautions (5.5). ]
- Hypertensive Crisis [ See Dosage and Administration (2.4), Warnings and Precautions (5.6). ]
- Reversible Posterior Leukoencephalopathy Syndrome [ See Dosage and Administration (2.4), Warnings and Precautions (5.7). ]
- Proteinuria [ See Dosage and Administration (2.4), Warnings and Precautions (5.8). ]
The most common adverse reactions observed in Avastin patients at a rate > 10% and at least twice the control arm rate, are epistaxis, headache, hypertension, rhinitis, proteinuria, taste alteration, dry skin, rectal hemorrhage, lacrimation disorder, back pain and exfoliative dermatitis.
Across all studies, Avastin was discontinued in 8.4 to 21% of patients because of adverse reactions.
6.1 Clinical Trial Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The data below reflect exposure to Avastin in 2661 patients with mCRC, non‑squamous NSCLC, MBC, glioblastoma, or mRCC in controlled (Studies 1, 2, 4, 5, 6 and 9) or uncontrolled, single arm (Study 7) trials treated at the recommended dose and schedule for a median of 8 to 16 doses of Avastin. [ See Clinical Studies (14). ] The population was aged 21–88 years (median 59), 46.0% male and 84.1% white. The population included 1089 first‑ and second‑line mCRC patients who received a median of 11 doses of Avastin, 480 first‑line metastatic NSCLC patients who received a median of 8 doses of Avastin, 592 MBC patients who had not received chemotherapy for metastatic disease received a median of 8 doses of Avastin, 163 glioblastoma patients who received a median of 9 doses of Avastin, and 337 mRCC patients who received a median of 16 doses of Avastin.
Surgery and Wound Healing Complications
The incidence of post‑operative wound healing and/or bleeding complications was increased in patients with mCRC receiving Avastin as compared to patients receiving only chemotherapy. Among patients requiring surgery on or within 60 days of receiving study treatment, wound healing and/or bleeding complications occurred in 15% (6/39) of patients receiving bolus‑IFL plus Avastin as compared to 4% (1/25) of patients who received bolus‑IFL alone.
In Study 7, events of post‑operative wound healing complications (craniotomy site wound dehiscence and cerebrospinal fluid leak) occurred in patients with previously treated glioblastoma: 3/84 patients in the Avastin alone arm and 1/79 patients in the Avastin plus irinotecan arm. [ See Boxed Warning, Dosage and Administration (2.4), Warnings and Precautions (5.2). ]
Hemorrhage
The incidence of epistaxis was higher (35% vs. 10%) in patients with mCRC receiving bolus‑IFL plus Avastin compared with patients receiving bolus‑IFL plus placebo. All but one of these events were Grade 1 in severity and resolved without medical intervention. Grade 1 or 2 hemorrhagic events were more frequent in patients receiving bolus‑IFL plus Avastin when compared to those receiving bolus‑IFL plus placebo and included gastrointestinal hemorrhage (24% vs. 6%), minor gum bleeding (2% vs. 0), and vaginal hemorrhage (4% vs. 2%). [ See Boxed Warning, Dosage and Administration (2.4), Warnings and Precautions (5.3). ]
Venous Thromboembolic Events
The incidence of Grade 3–4 venous thromboembolic events was higher in patients with mCRC or NSCLC receiving Avastin with chemotherapy as compared to those receiving chemotherapy alone. The risk of developing a second subsequent thromboembolic event in mCRC patients receiving Avastin and chemotherapy was increased compared to patients receiving chemotherapy alone. In Study 1, 53 patients (14%) on the bolus‑IFL plus Avastin arm and 30 patients (8%) on the bolus‑IFL plus placebo arm received full dose warfarin following a venous thromboembolic event. Among these patients, an additional thromboembolic event occurred in 21% (11/53) of patients receiving bolus‑IFL plus Avastin and 3% (1/30) of patients receiving bolus‑IFL alone.
The overall incidence of Grade 3–4 venous thromboembolic events in Study 1 was 15.1% in patients receiving bolus‑IFL plus Avastin and 13.6% in patients receiving bolus‑IFL plus placebo. In Study 1, the incidence of the following Grade 3–4 venous thromboembolic events was higher in patients receiving bolus‑IFL plus Avastin as compared to patients receiving bolus‑IFL plus placebo: deep venous thrombosis (34 vs. 19 patients) and intra‑abdominal venous thrombosis (10 vs. 5 patients).
Neutropenia and Infection
The incidences of neutropenia and febrile neutropenia are increased in patients receiving Avastin plus chemotherapy compared to chemotherapy alone. In Study 1, the incidence of Grade 3 or 4 neutropenia was increased in mCRC patients receiving IFL plus Avastin (21%) compared to patients receiving IFL alone (14%). In Study 4, the incidence of Grade 4 neutropenia was increased in NSCLC patients receiving paclitaxel/carboplatin (PC) plus Avastin (26.2%) compared with patients receiving PC alone (17.2%). Febrile neutropenia was also increased (5.4% for PC plus Avastin vs. 1.8% for PC alone). There were 19 (4.5%) infections with Grade 3 or 4 neutropenia in the PC plus Avastin arm of which 3 were fatal compared to 9 (2%) neutropenic infections in patients receiving PC alone, of which none were fatal. During the first 6 cycles of treatment, the incidence of serious infections including pneumonia, febrile neutropenia, catheter infections and wound infections was increased in the PC plus Avastin arm [58 patients (13.6%)] compared to the PC alone arm [29 patients (6.6%)].
In Study 7, one fatal event of neutropenic infection occurred in a patient with previously treated glioblastoma receiving Avastin alone. The incidence of any grade of infection in patients receiving Avastin alone was 55% and the incidence of Grade 3–5 infection was 10%.
Proteinuria
Grade 3‑4 proteinuria ranged from 0.7 to 7.4% in Studies 1, 2, 4 and 9. The overall incidence of proteinuria (all grades) was only adequately assessed in Study 9, in which the incidence was 20%. Median onset of proteinuria was 5.6 months (range 15 days to 37 months) after initiation of Avastin. Median time to resolution was 6.1 months (95% CI 2.8 months, 11.3 months). Proteinuria did not resolve in 40% of patients after median follow up of 11.2 months and required permanent discontinuation of Avastin in 30% of the patients who developed proteinuria (Study 9). [ See Warnings and Precautions (5.8). ]
Congestive Heart Failure
The incidence of Grade ≥ 3 left ventricular dysfunction was 1.0% in patients receiving Avastin compared to 0.6% in the control arm across indications. In patients with MBC, the incidence of Grade 3–4 congestive heart failure (CHF) was increased in patients in the Avastin plus paclitaxel arm (2.2 %) as compared to the control arm (0.3%). Among patients receiving prior anthracyclines for MBC, the rate of CHF was 3.8% for patients receiving Avastin as compared to 0.6 % for patients receiving paclitaxel alone. The safety of continuation or resumption of Avastin in patients with cardiac dysfunction has not been studied.
Metastatic Colorectal Cancer (mCRC)
The data in Table 1 and Table 2 were obtained in Study 1, a randomized, double‑blind, controlled trial comparing chemotherapy plus Avastin with chemotherapy plus placebo. Avastin was administered at 5 mg/kg every 2 weeks.
All Grade 3–4 adverse events and selected Grade 1–2 adverse events (hypertension, proteinuria, thromboembolic events) were collected in the entire study population. Severe and life‑threatening (Grade 3–4) adverse events, which occurred at a higher incidence (≥ 2%) in patients receiving bolus‑IFL plus Avastin as compared to bolus‑IFL plus placebo, are presented in Table 1.
| Arm 1 IFL + Placebo (n = 396) | Arm 2 IFL + Avastin (n = 392) |
|
| a Central laboratories were collected on Days 1 and 21 of each cycle. Neutrophil counts are available in 303 patients in Arm 1 and 276 in Arm 2. | ||
| NCI‑CTC Grade 3–4 Events | 74% | 87% |
| Body as a Whole | ||
| Asthenia | 7% | 10% |
| Abdominal Pain | 5% | 8% |
| Pain | 5% | 8% |
| Cardiovascular | ||
| Hypertension | 2% | 12% |
| Deep Vein Thrombosis | 5% | 9% |
| Intra‑Abdominal Thrombosis | 1% | 3% |
| Syncope | 1% | 3% |
| Digestive | ||
| Diarrhea | 25% | 34% |
| Constipation | 2% | 4% |
| Hemic/Lymphatic | ||
| Leukopenia | 31% | 37% |
| Neutropeniaa | 14% | 21% |
Grade 1–4 adverse events which occurred at a higher incidence (≥5%) in patients receiving bolus‑IFL plus Avastin as compared to the bolus‑IFL plus placebo arm, are presented in Table 2. Grade 1–4 adverse events were collected for the first approximately 100 patients in each of the three treatment arms who were enrolled until enrollment in Arm 3 (5‑FU/LV + Avastin) was discontinued.
| Arm 1 IFL + Placebo (n = 98) | Arm 2 IFL + Avastin (n = 102) | Arm 3 5‑FU/LV + Avastin (n = 109) |
|
| Body as a Whole | |||
| Pain | 55% | 61% | 62% |
| Abdominal Pain | 55% | 61% | 50% |
| Headache | 19% | 26% | 26% |
| Cardiovascular | |||
| Hypertension | 14% | 23% | 34% |
| Hypotension | 7% | 15% | 7% |
| Deep Vein Thrombosis | 3% | 9% | 6% |
| Digestive | |||
| Vomiting | 47% | 52% | 47% |
| Anorexia | 30% | 43% | 35% |
| Constipation | 29% | 40% | 29% |
| Stomatitis | 18% | 32% | 30% |
| Dyspepsia | 15% | 24% | 17% |
| GI Hemorrhage | 6% | 24% | 19% |
| Weight Loss | 10% | 15% | 16% |
| Dry Mouth | 2% | 7% | 4% |
| Colitis | 1% | 6% | 1% |
| Hemic/Lymphatic | |||
| Thrombocytopenia | 0% | 5% | 5% |
| Nervous | |||
| Dizziness | 20% | 26% | 19% |
| Respiratory | |||
| Upper Respiratory Infection | 39% | 47% | 40% |
| Epistaxis | 10% | 35% | 32% |
| Dyspnea | 15% | 26% | 25% |
| Voice Alteration | 2% | 9% | 6% |
| Skin/Appendages | |||
| Alopecia | 26% | 32% | 6% |
| Skin Ulcer | 1% | 6% | 6% |
| Special Senses | |||
| Taste Disorder | 9% | 14% | 21% |
| Urogenital | |||
| Proteinuria | 24% | 36% | 36% |
Avastin in Combination with FOLFOX4 in Second‑line mCRC
Only Grade 3–5 non‑hematologic and Grade 4–5 hematologic adverse events related to treatment were collected in Study 2. The most frequent adverse events (selected Grade 3–5 non‑hematologic and Grade 4‑5 hematologic adverse events) occurring at a higher incidence (≥ 2%) in 287 patients receiving FOLFOX4 plus Avastin compared to 285 patients receiving FOLFOX4 alone were fatigue (19% vs. 13%), diarrhea (18% vs. 13%), sensory neuropathy (17% vs. 9%), nausea (12% vs. 5%), vomiting (11% vs. 4%), dehydration (10% vs. 5%), hypertension (9% vs. 2%), abdominal pain (8% vs. 5%), hemorrhage (5% vs. 1%), other neurological (5% vs. 3%), ileus (4% vs. 1%) and headache (3% vs. 0%). These data are likely to under‑estimate the true adverse event rates due to the reporting mechanisms used in Study 2.
Unresectable Non‑Squamous Non‑Small Cell Lung Cancer (NSCLC)
Only Grade 3–5 non‑hematologic and Grade 4–5 hematologic adverse events were collected in Study 4. Grade 3–5 non‑hematologic and Grade 4–5 hematologic adverse events (occurring at a higher incidence (≥ 2%) in 427 patients receiving PC plus Avastin compared with 441 patients receiving PC alone were neutropenia (27% vs. 17%), fatigue (16% vs. 13%), hypertension (8% vs. 0.7%), infection without neutropenia (7% vs. 3%), venous thrombus/embolism (5% vs. 3%), febrile neutropenia (5% vs. 2%), pneumonitis/pulmonary infiltrates (5% vs. 3%), infection with Grade 3 or 4 neutropenia (4% vs. 2%), hyponatremia (4% vs. 1%), headache (3% vs. 1%) and proteinuria (3% vs. 0%).
Metastatic Breast Cancer (MBC)
Only Grade 3–5 non‑hematologic and Grade 4–5 hematologic adverse events were collected in Study 5. Grade 3–4 adverse events occurring at a higher incidence (≥ 2%) in 363 patients receiving paclitaxel plus Avastin compared with 348 patients receiving paclitaxel alone were sensory neuropathy (24% vs. 18%), hypertension (16% vs. 1%), fatigue (11% vs. 5%), infection without neutropenia (9% vs. 5%), neutrophils (6% vs. 3%), vomiting (6% vs. 2%), diarrhea (5% vs. 1%), bone pain (4% vs. 2%), headache (4% vs. 1%), nausea (4% vs. 1%), cerebrovascular ischemia (3% vs. 0%), dehydration (3% vs. 1%), infection with unknown ANC (3% vs. 0.3%), rash/desquamation (3% vs. 0.3%) and proteinuria (3% vs. 0%).
Sensory neuropathy, hypertension, and fatigue were reported at a ≥ 5% higher absolute incidence in the paclitaxel plus Avastin arm compared with the paclitaxel alone arm.
Fatal adverse reactions occurred in 6/363 (1.7%) of patients who received paclitaxel plus Avastin. Causes of death were gastrointestinal perforation (2), myocardial infarction (2), diarrhea/abdominal, and pain/weakness/hypotension (2).
Avastin is not approved for use in combination with capecitabine or for use in second or third line treatment of MBC. The data below are presented to provide information on the overall safety profile of Avastin in women with breast cancer since Study 6 is the only randomized, controlled study in which all adverse events were collected for all patients. All patients in Study 6 received prior anthracycline and taxane therapy in the adjuvant setting or for metastatic disease. Grade 1–4 events which occurred at a higher incidence (≥5%) in patients receiving capecitabine plus Avastin compared to the capecitabine alone arm are presented in Table 3.
|
Capecitabine (n = 215) |
Capecitabine + Avastin (n = 229) |
|
| Body as a Whole | ||
| Asthenia | 47% | 57% |
| Headache | 13% | 33% |
| Pain | 25% | 31% |
| Cardiovascular | ||
| Hypertension | 2% | 24% |
| Digestive | ||
| Stomatitis | 19% | 25% |
| Metabolic/Nutrition | ||
| Weight loss | 4% | 9% |
| Musculoskeletal | ||
| Myalgia | 8% | 14% |
| Respiratory | ||
| Dyspnea | 18% | 27% |
| Epistaxis | 1% | 16% |
| Skin/Appendages | ||
| Exfoliative dermatitis | 75% | 84% |
| Urogenital | ||
| Albuminuria | 7% | 22% |
Glioblastoma
All adverse events were collected in 163 patients enrolled in Study 7 who either received Avastin alone or Avastin plus irinotecan. All patients received prior radiotherapy and temozolomide. Avastin was administered at 10 mg/kg every 2 weeks alone or in combination with irinotecan. Avastin was discontinued due to adverse events in 4.8% of patients treated with Avastin alone.
In patients receiving Avastin alone (N=84), the most frequently reported adverse events of any grade were infection (55%), fatigue (45%), headache (37%), hypertension (30%), epistaxis (19%) and diarrhea (21%). Of these, the incidence of Grade ≥3 adverse events was infection (10%), fatigue (4%), headache (4%), hypertension (8%) and diarrhea (1%). Two deaths on study were possibly related to Avastin: one retroperitoneal hemorrhage and one neutropenic infection.
In patients receiving Avastin alone or Avastin plus irinotecan (N=163), the incidence of Avastin–related adverse events (Grade 1–4) were bleeding/hemorrhage (40%), epistaxis (26%), CNS hemorrhage (5%), hypertension (32%), venous thromboembolic event (8%), arterial thromboembolic event (6%), wound‑healing complications (6%), proteinuria (4%), gastrointestinal perforation (2%), and RPLS (1%). The incidence of Grade 3–5 events in these 163 patients were bleeding/hemorrhage (2%), CNS hemorrhage (1%), hypertension (5%), venous thromboembolic event (7%), arterial thromboembolic event (3%), wound‑healing complications (3%), proteinuria (1%), and gastrointestinal perforation (2%).
Metastatic Renal Cell Carcinoma (mRCC)
All grade adverse events were collected in Study 9. Grade 3–5 adverse events occurring at a higher incidence (≥2%) in 337 patients receiving interferon alfa (IFN‑α) plus Avastin compared to 304 patients receiving IFN‑α plus placebo arm were fatigue (13% vs. 8%), asthenia (10% vs. 7%), proteinuria (7% vs. 0%), hypertension (6% vs. 1%; including hypertension and hypertensive crisis), and hemorrhage (3% vs. 0.3%; including epistaxis, small intestinal hemorrhage, aneurysm ruptured, gastric ulcer hemorrhage, gingival bleeding, haemoptysis, hemorrhage intracranial, large intestinal hemorrhage, respiratory tract hemorrhage, and traumatic hematoma).
Grade 1–5 adverse events occurring at a higher incidence (≥5%) in patients receiving IFN‑α plus Avastin compared to the IFN‑α plus placebo arm are presented in Table 4.
| System Organ Class/Preferred term* |
IFN‑α + Placebo (n = 304) |
IFN‑α + Avastin (n = 337) |
|
||
| Gastrointestinal disorders | ||
| Diarrhea | 16% | 21% |
| General disorders and administration site conditions | ||
| Fatigue | 27% | 33% |
| Investigations | ||
| Weight decreased | 15% | 20% |
| Metabolism and nutrition disorders | ||
| Anorexia | 31% | 36% |
| Musculoskeletal and connective tissue disorders | ||
| Myalgia | 14% | 19% |
| Back pain | 6% | 12% |
| Nervous system disorders | ||
| Headache | 16% | 24% |
| Renal and urinary disorders | ||
| Proteinuria | 3% | 20% |
| Respiratory, thoracic and mediastinal disorders | ||
| Epistaxis | 4% | 27% |
| Dysphonia | 0% | 5% |
| Vascular disorders | ||
| Hypertension | 9% | 28% |
The following adverse events were reported at a 5‑fold greater incidence in the IFN‑α plus Avastin arm compared to IFN‑α alone and not represented in Table 4: gingival bleeding (13 patients vs. 1 patient); rhinitis (9 vs.0 ); blurred vision (8 vs. 0); gingivitis (8 vs. 1); gastroesophageal reflux disease (8 vs.1 ); tinnitus (7 vs. 1); tooth abscess (7 vs.0); mouth ulceration (6 vs. 0); acne (5 vs. 0); deafness (5 vs. 0); gastritis (5 vs. 0); gingival pain (5 vs. 0) and pulmonary embolism (5 vs. 1).
6.2 Immunogenicity
As with all therapeutic proteins, there is a potential for immunogenicity. The incidence of antibody development in patients receiving Avastin has not been adequately determined because the assay sensitivity was inadequate to reliably detect lower titers. Enzyme‑linked immunosorbent assays (ELISAs) were performed on sera from approximately 500 patients treated with Avastin, primarily in combination with chemotherapy. High titer human anti‑Avastin antibodies were not detected.
Immunogenicity data are highly dependent on the sensitivity and specificity of the assay. Additionally, the observed incidence of antibody positivity in an assay may be influenced by several factors, including sample handling, timing of sample collection, concomitant medications, and underlying disease. For these reasons, comparison of the incidence of antibodies to Avastin with the incidence of antibodies to other products may be misleading.
6.3 Postmarketing Experience
The following adverse reactions have been identified during post‑approval use of Avastin. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Body as a Whole: Polyserositis
Cardiovascular: Pulmonary hypertension, RPLS
Digestive: Intestinal necrosis, mesenteric venous occlusion, anastomotic ulceration
Hemic and lymphatic: Pancytopenia
Renal: Renal thrombotic microangiopathy (manifested as severe proteinuria)
Respiratory: Nasal septum perforation, dysphonia
7 DRUG INTERACTIONS
A drug interaction study was performed in which irinotecan was administered as part of the FOLFIRI regimen with or without Avastin. The results demonstrated no significant effect of bevacizumab on the pharmacokinetics of irinotecan or its active metabolite SN38.
In a randomized study in 99 patients with NSCLC, based on limited data, there did not appear to be a difference in the mean exposure of either carboplatin or paclitaxel when each was administered alone or in combination with Avastin. However, 3 of the 8 patients receiving Avastin plus paclitaxel/carboplatin had substantially lower paclitaxel exposure after four cycles of treatment (at Day 63) than those at Day 0, while patients receiving paclitaxel/carboplatin without Avastin had a greater paclitaxel exposure at Day 63 than at Day 0.
In Study 9, there was no difference in the mean exposure of interferon alfa administered in combination with Avastin when compared to interferon alfa alone.
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category C
There are no studies of bevacizumab in pregnant women. Reproduction studies in rabbits treated with approximately 1 to 12 times the recommended human dose of bevacizumab resulted in teratogenicity, including an increased incidence of specific gross and skeletal fetal alterations. Adverse fetal outcomes were observed at all doses tested. Other observed effects included decreases in maternal and fetal body weights and an increased number of fetal resorptions. [ See Nonclinical Toxicology (13.3). ]
Human IgG is known to cross the placental barrier; therefore, bevacizumab may be transmitted from the mother to the developing fetus, and has the potential to cause fetal harm when administered to pregnant women. Because of the observed teratogenic effects of known inhibitors of angiogenesis in humans, bevacizumab should be used during pregnancy only if the potential benefit to the pregnant woman justifies the potential risk to the fetus.
8.3 Nursing Mothers
It is not known whether Avastin is secreted in human milk, but human IgG is excreted in human milk. Published data suggest that breast milk antibodies do not enter the neonatal and infant circulation in substantial amounts. Because many drugs are secreted in human milk and because of the potential for serious adverse reactions in nursing infants from bevacizumab, a decision should be made whether to discontinue nursing or discontinue drug, taking into account the half‑life of the bevacizumab (approximately 20 days [range 11–50 days]) and the importance of the drug to the mother. [ See Clinical Pharmacology (12.3). ]
8.4 Pediatric Use
The safety, effectiveness and pharmacokinetic profile of Avastin in pediatric patients have not been established.
Juvenile cynomolgus monkeys with open growth plates exhibited physeal dysplasia following 4 to 26 weeks exposure at 0.4 to 20 times the recommended human dose (based on mg/kg and exposure). The incidence and severity of physeal dysplasia were dose‑related and were partially reversible upon cessation of treatment.
8.5 Geriatric Use
In Study 1, severe adverse events that occurred at a higher incidence ( ≥ 2%) in patients aged ≥ 65 years as compared to younger patients were asthenia, sepsis, deep thrombophlebitis, hypertension, hypotension, myocardial infarction, congestive heart failure, diarrhea, constipation, anorexia, leukopenia, anemia, dehydration, hypokalemia, and hyponatremia. The effect of Avastin on overall survival was similar in elderly patients as compared to younger patients.
In Study 2, patients aged ≥ 65 years receiving Avastin plus FOLFOX4 had a greater relative risk as compared to younger patients for the following adverse events: nausea, emesis, ileus, and fatigue.
In Study 4, patients aged ≥ 65 years receiving carboplatin, paclitaxel, and Avastin had a greater relative risk for proteinuria as compared to younger patients. [ See Warnings and Precautions (5.8). ]
In Study 5, there were insufficient numbers of patients ≥ 65 years old to determine whether the overall adverse events profile was different in the elderly as compared with younger patients.
Of the 742 patients enrolled in Genentech‑sponsored clinical studies in which all adverse events were captured, 212 (29%) were age 65 or older and 43 (6%) were age 75 or older. Adverse events of any severity that occurred at a higher incidence in the elderly as compared to younger patients, in addition to those described above, were dyspepsia, gastrointestinal hemorrhage, edema, epistaxis, increased cough, and voice alteration.
In an exploratory, pooled analysis of 1745 patients treated in five randomized, controlled studies, there were 618 (35%) patients aged ≥ 65 years and 1127 patients < 65 years of age. The overall incidence of arterial thromboembolic events was increased in all patients receiving Avastin with chemotherapy as compared to those receiving chemotherapy alone, regardless of age. However, the increase in arterial thromboembolic events incidence was greater in patients aged ≥ 65 years (8.5% vs. 2.9%) as compared to those < 65 years (2.1% vs. 1.4%). [ See Warnings and Precautions (5.5). ]
10 OVERDOSAGE
The highest dose tested in humans (20 mg/kg IV) was associated with headache in nine of 16 patients and with severe headache in three of 16 patients.
11 DESCRIPTION
Avastin (bevacizumab) is a recombinant humanized monoclonal IgG1 antibody that binds to and inhibits the biologic activity of human vascular endothelial growth factor (VEGF) in in vitro and in vivo assay systems. Bevacizumab contains human framework regions and the complementarity‑determining regions of a murine antibody that binds to VEGF. Avastin has an approximate molecular weight of 149 kD. Bevacizumab is produced in a mammalian cell (Chinese Hamster Ovary) expression system in a nutrient medium containing the antibiotic gentamicin. Gentamicin is not detectable in the final product.
Avastin is a clear to slightly opalescent, colorless to pale brown, sterile, pH 6.2 solution for intravenous infusion. Avastin is supplied in 100 mg and 400 mg preservative‑free, single‑use vials to deliver 4 mL or 16 mL of Avastin (25 mg/mL). The 100 mg product is formulated in 240 mg α,α‑trehalose dihydrate, 23.2 mg sodium phosphate (monobasic, monohydrate), 4.8 mg sodium phosphate (dibasic, anhydrous), 1.6 mg polysorbate 20, and Water for Injection, USP. The 400 mg product is formulated in 960 mg α,α‑trehalose dihydrate, 92.8 mg sodium phosphate (monobasic, monohydrate), 19.2 mg sodium phosphate (dibasic, anhydrous), 6.4 mg polysorbate 20, and Water for Injection, USP.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Bevacizumab binds VEGF and prevents the interaction of VEGF to its receptors (Flt‑1 and KDR) on the surface of endothelial cells. The interaction of VEGF with its receptors leads to endothelial cell proliferation and new blood vessel formation in in vitro models of angiogenesis. Administration of bevacizumab to xenotransplant models of colon cancer in nude (athymic) mice caused reduction of microvascular growth and inhibition of metastatic disease progression.
12.3 Pharmacokinetics
The pharmacokinetic profile of bevacizumab was assessed using an assay that measures total serum bevacizumab concentrations (i.e., the assay did not distinguish between free bevacizumab and bevacizumab bound to VEGF ligand). Based on a population pharmacokinetic analysis of 491 patients who received 1 to 20 mg/kg of Avastin weekly, every 2 weeks, or every 3 weeks, the estimated half‑life of bevacizumab was approximately 20 days (range 11–50 days). The predicted time to reach steady state was 100 days. The accumulation ratio following a dose of 10 mg/kg of bevacizumab every 2 weeks was 2.8.
The clearance of bevacizumab varied by body weight, gender, and tumor burden. After correcting for body weight, males had a higher bevacizumab clearance (0.262 L/day vs. 0.207 L/day) and a larger Vc (3.25 L vs. 2.66 L) than females. Patients with higher tumor burden (at or above median value of tumor surface area) had a higher bevacizumab clearance (0.249 L/day vs. 0.199 L/day) than patients with tumor burdens below the median. In Study 1, there was no evidence of lesser efficacy (hazard ratio for overall survival) in males or patients with higher tumor burden treated with Avastin as compared to females and patients with low tumor burden. The relationship between bevacizumab exposure and clinical outcomes has not been explored.
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
No carcinogenicity or mutagenicity studies of bevacizumab have been conducted.
Bevacizumab may impair fertility. Female cynomolgus monkeys treated with 0.4 to 20 times the recommended human dose of bevacizumab exhibited arrested follicular development or absent corpora lutea as well as dose‑related decreases in ovarian and uterine weights, endometrial proliferation, and the number of menstrual cycles. Following a 4‑ or 12‑week recovery period, there was a trend suggestive of reversibility. After the 12‑week recovery period, follicular maturation arrest was no longer observed, but ovarian weights were still moderately decreased. Reduced endometrial proliferation was no longer observed at the 12‑week recovery time point; however, decreased uterine weight, absent corpora lutea, and reduced number of menstrual cycles remained evident.
13.2 Animal Toxicology and/or Pharmacology
In cynomolgus monkeys, when bevacizumab was administered at doses of 0.4 to 20 times the weekly human exposure, anatomical pathology revealed several adverse effects on general growth and skeletal development, fertility and wound healing capacity. Severe physeal dysplasia was consistently reported in juvenile monkeys with open growth plates receiving 0.4 to 20 times the human dose. The physeal dysplasia was characterized by a linear cessation of growth line and chondrocyte hyperplasia which did not completely resolve after the 4 to 12 weeks recovery period without drug exposure.
Rabbits dosed with bevacizumab exhibited reduced wound healing capacity. Using full‑thickness skin incision and partial thickness circular dermal wound models, bevacizumab dosing resulted in reductions in wound tensile strength, decreased granulation and re‑epithelialization, and delayed time to wound closure.
13.3 Reproductive and Developmental Toxicology
Pregnant rabbits dosed with 1 to 12 times the human dose of bevacizumab every three days during the period of organogenesis (gestation day 6–18) exhibited teratogenic effects, decreases in maternal and fetal body weights, and increased number of fetal resorptions. Teratogenic effects included: reduced or irregular ossification in the skull, jaw, spine, ribs, tibia and bones of the paws; meningocele; fontanel, rib and hindlimb deformities; corneal opacity; and absent hindlimb phalanges. There are no data available regarding the level of bevacizumab exposure in the offspring.
14 CLINICAL STUDIES
14.1 Metastatic Colorectal Cancer (mCRC)
Study 1
In this double-blind, active‑controlled study, patients were randomized (1:1:1) to IV bolus‑IFL(irinotecan 125 mg/m2, 5‑FU 500 mg/m2, and leucovorin (LV) 20 mg/m2 given once weekly for 4 weeks every 6 weeks) plus placebo (Arm 1), bolus‑IFL plus Avastin (5 mg/kg every 2 weeks) (Arm 2), or 5‑FU/LV plus Avastin (5 mg/kg every 2 weeks) (Arm 3). Enrollment in Arm 3 was discontinued, as pre‑specified, when the toxicity of Avastin in combination with the bolus‑IFL regimen was deemed acceptable. The main outcome measure was overall survival (OS).
Of the 813 patients randomized to Arms 1 and 2, the median age was 60, 40% were female, 79% were Caucasian, 57% had an ECOG performance status of 0, 21% had a rectal primary and 28% received prior adjuvant chemotherapy. In 56% of the patients, the dominant site of disease was extra‑abdominal, while the liver was the dominant site in 38% of patients.
The addition of Avastin resulted in an improvement in survival across subgroups defined by age (< 65 yrs, ≥ 65 yrs) and gender. Results are presented in Table 5 and Figure 1.
| IFL + Placebo | IFL + Avastin 5 mg/kg q 2 wks |
|
|---|---|---|
| a p < 0.001 by stratified log rank test. b p < 0.01 by χ2 test. |
||
| Number of Patients | 411 | 402 |
| Overall Survivala | ||
| Median (months) | 15.6 | 20.3 |
| Hazard ratio | 0.66 | |
| Progression‑free Survivala | ||
| Median (months) | 6.2 | 10.6 |
| Hazard ratio | 0.54 | |
| Overall Response Rateb | ||
| Rate (percent) | 35% | 45% |
| Duration of Response | ||
| Median (months) | 7.1 | 10.4 |
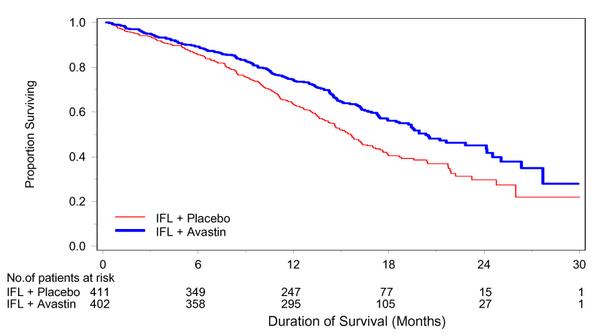 |
Among the 110 patients enrolled in Arm 3, median OS was 18.3 months, median progression‑free survival (PFS) was 8.8 months, objective response rate (ORR) was 39%, and median duration of response was 8.5 months.
Study 2
Study 2 was a randomized, open‑label, active‑controlled trial in patients who were previously treated with irinotecan +/- 5‑FU for initial therapy for metastatic disease or as adjuvant therapy. Patients were randomized (1:1:1) to IV FOLFOX4 (Day 1: oxaliplatin 85 mg/m2 and LV 200 mg/m2 concurrently, then 5‑FU 400 mg/m2 bolus followed by 600 mg/m2 continuously; Day 2: LV 200 mg/m2, then 5‑FU 400 mg/m2 bolus followed by 600 mg/m2 continuously; repeated every 2 weeks), FOLFOX4 plus Avastin (10 mg/kg every 2 weeks prior to FOLFOX4 on Day 1), or Avastin monotherapy (10 mg/kg every 2 weeks). The main outcome measure was OS.
The Avastin monotherapy arm was closed to accrual after enrollment of 244 of the planned 290 patients following a planned interim analysis by the data monitoring committee based on evidence of decreased survival compared to FOLFOX4 alone.
Of the 829 patients randomized to the three arms, the median age was 61 years, 40% were female, 87% were Caucasian, 49% had an ECOG performance status of 0, 26% received prior radiation therapy, and 80% received prior adjuvant chemotherapy, 99% received prior irinotecan, with or without 5‑FU as therapy for metastatic disease, and 1% received prior irinotecan and 5‑FU as adjuvant therapy.
The addition of Avastin to FOLFOX4 resulted in significantly longer survival as compared to FOLFOX4 alone (median OS 13.0 months vs. 10.8 months; hazard ratio 0.75 [95% CI 0.63, 0.89], p = 0.001 stratified log rank test) with clinical benefit seen in subgroups defined by age (< 65 yrs, ≥ 65 yrs) and gender. PFS and ORR based on investigator assessment were higher in the Avastin plus FOLFOX4 arm.
Study 3
The activity of Avastin in combination with bolus or infusional 5‑FU/LV was evaluated in a single arm study enrolling 339 patients with mCRC with disease progression following both irinotecan‑ and oxaliplatin‑containing chemotherapy regimens. Seventy‑three percent of patients received concurrent bolus 5‑FU/LV. One objective partial response was verified in the first 100 evaluable patients for an overall response rate of 1% (95% CI 0–5.5%).
14.2 Unresectable Non‑Squamous Non‑Small Cell Lung Cancer (NSCLC)
Study 4
The safety and efficacy of Avastin as first line treatment of patients with locally advanced, metastatic, or recurrent non‑squamous NSCLC was studied in a single, large, randomized, active‑controlled, open‑label, multicenter study.
Chemotherapy‑naïve patients with locally advanced, metastatic or recurrent non–squamous NSCLC were randomized (1:1) to receive six 21‑day cycles of paclitaxel 200 mg/m2 and carboplatin AUC=6.0, by IV on day 1 (PC) or PC in combination with Avastin 15 mg/kg by IV on day 1 (PC plus Avastin). After completion or upon discontinuation of chemotherapy, patients in the PC plus Avastin arm continued to receive Avastin alone until disease progression or until unacceptable toxicity. Patients with predominant squamous histology (mixed cell type tumors only), central nervous system (CNS) metastasis, gross hemoptysis (≥1/2 tsp of red blood), unstable angina, or receiving therapeutic anticoagulation were excluded. The main outcome measure was duration of survival.
Of the 878 patients randomized, the median age was 63, 46% were female, 43% were ≥ age 65, and 28% had ≥ 5% weight loss at study entry. Eleven percent had recurrent disease and of the 89% with newly diagnosed NSCLC, 12% had Stage IIIB with malignant pleural effusion and 76% had Stage IV disease.
The results are presented in Figure 2. OS was statistically significantly higher among patients receiving PC plus Avastin compared with those receiving PC alone; median OS was 12.3 months vs. 10.3 months [hazard ratio 0.80 (repeated 95% CI 0.68, 0.94), final p‑ value 0.013, stratified log‑rank test]. Based on investigator assessment which was not independently verified, patients were reported to have longer PFS with Avastin in combination with PC compared to PC alone.
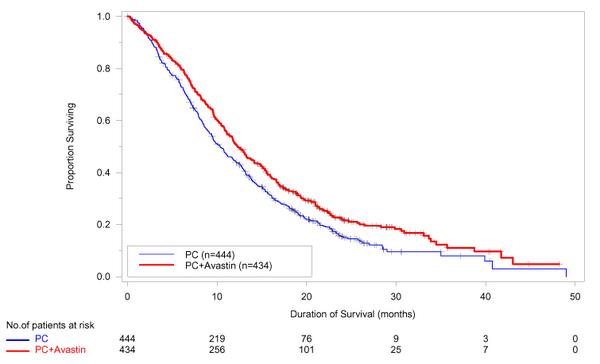 |
In an exploratory analyses across patient subgroups, the impact of Avastin on OS was less robust in the following: women [HR = 0.99 (95% CI: 0.79, 1.25)], age ≥ 65 years [HR = 0.91 (95% CI: 0.72, 1.14)] and patients with ≥5% weight loss at study entry [HR = 0.96 (95% CI: 0.73, 1.26)].
14.3 Metastatic Breast Cancer (MBC)
Study 5
The efficacy and safety of Avastin as first-line treatment of patients with MBC was studied in a single, open‑label, randomized, multicenter study. Patients who had not received chemotherapy for locally recurrent or MBC were randomized (1:1) to receive paclitaxel (90 mg/m2 IV once weekly for 3 out of 4 weeks) alone or in combination with Avastin (10 mg/kg IV infusion every 2 weeks). Patients were treated until disease progression or unacceptable toxicity. In situations where paclitaxel was discontinued or held, treatment with Avastin alone could be continued until disease progression. Patients with breast cancer overexpressing HER2 were not eligible unless they had received prior therapy with trastuzumab.
Prior hormonal therapy for the treatment of metastatic disease was allowed, as was prior adjuvant chemotherapy or hormonal therapy. Adjuvant taxane therapy, if received, must have been completed 12 or more months prior to study entry. Patients with central nervous system metastasis were excluded. The main outcome measure of the study was PFS as assessed by independent radiographic review. Secondary outcome measures were OS and ORR.
Of the 722 patients randomized, the median age was 55 years, 76% were white, 55% were postmenopausal, and 64% were ER and/or PR positive. Patient characteristics were similar across treatment arms. Thirty‑six percent had received prior hormonal therapy for advanced disease, and 66% had received adjuvant chemotherapy, including 20% with prior taxane use and 50% with prior anthracycline use. Efficacy results are summarized in Table 6.
| Efficacy Parameter | Avastin + Paclitaxel (n=368) | Paclitaxel Alone (n=354) | p-value | HR (95% CI) |
|---|---|---|---|---|
| 1 Includes only patients with measurable disease 2 The difference in partial response rates is 26.7% with a 95% CI (18.4%, 35.0%). |
||||
| Progression-free Survival | 11.3 | 5.8 | 0.48 | |
| [median, months (95% CI)] | (10.5, 13.3) | (5.4, 8.2) | <0.0001 | (0.39, 0.61) |
| Overall Survival | 26.5 | 24.8 | 0.87 | |
| [median, months (95% CI)] | (23.7, 29.2) | (21.4, 27.4) | 0.14 | (0.72, 1.05) |
| Partial Response Rate1 (PR) | 48.9% 2 | 22.2% | <0.001 | — |
The addition of Avastin to paclitaxel resulted in an improvement in PFS with no significant improvement in OS. Partial response rates in patients with measurable disease were higher with Avastin plus paclitaxel. No complete responses were observed.
Thirty‑four percent of the patients had incomplete follow‑up for disease progression; therefore an exploratory analysis using similar imputation between arms was performed, which yielded a hazard ratio of 0.57.
Study 6
The efficacy and safety of Avastin as second‑ and third‑line treatment of patients with MBC was studied in a single open‑label randomized study. Patients who had received prior anthracycline and taxane therapy in the adjuvant setting or for their MBC were randomized (1:1) to receive capecitabine alone or in combination with Avastin. Of the 462 enrolled patients, the median age was 51 years, 81% were white, and 50% were ER positive. Patient characteristics were similar across the treatment arms.
The study failed to demonstrate a statistically significant effect on PFS or OS. The median PFS was 4.2 months in the capecitabine arm and 4.9 months in the capecitabine plus Avastin arm (log‑rank p‑value = 0.86, hazard ratio 0.98). The median OS was 14.5 months in the capecitabine arm and 15.1 months in the capecitabine plus Avastin arm (hazard ratio of 1.08).
14.4 Glioblastoma
Study 7
The efficacy and safety of Avastin was evaluated in Study 7, an open‑label, multicenter, randomized, non‑comparative study of patients with previously treated glioblastoma. Patients received Avastin (10 mg/kg IV) alone or Avastin plus irinotecan every 2 weeks until disease progression or until unacceptable toxicity. All patients received prior radiotherapy (completed at least 8 weeks prior to receiving Avastin) and temozolomide. Patients with active brain hemorrhage were excluded.
Of the 85 patients randomized to the Avastin arm, the median age was 54 years, 32% were female, 81% were in first relapse, Karnofsky performance status was 90–100 for 45% and 70–80 for 55%.
The efficacy of Avastin was demonstrated using response assessment based on both WHO radiographic criteria and by stable or decreasing corticosteroid use, which occurred in 25.9% (95% CI 17.0%, 36.1%) of the patients. Median duration of response was 4.2 months (95% CI 3.0, 5.7). Radiologic assessment was based on MRI imaging (using T1 and T2/FLAIR). MRI does not necessarily distinguish between tumor, edema, and radiation necrosis.
Study 8
Study 8, was a single‑arm, single institution trial with 56 patients with glioblastoma. All patients had documented disease progression after receiving temozolomide and radiation therapy. Patients received Avastin 10 mg/kg IV every 2 weeks until disease progression or unacceptable toxicity.
The median age was 54, 54% were male, 98% Caucasian, and 68% had a Karnofsky Performance Status of 90–100.
The efficacy of Avastin was supported by an objective response rate of 19.6% (95% CI 10.9%, 31.3%) using the same response criteria as in Study 7. Median duration of response was 3.9 months (95% CI 2.4, 17.4).
14.5 Metastatic Renal Cell Carcinoma (mRCC)
Study 9
Patients with treatment naïve mRCC were evaluated in a multicenter, randomized, double‑blind, international study comparing Avastin plus interferon alfa 2a (IFN‑α2a) versus placebo plus IFN‑α2a. A total of 649 patients who had undergone a nephrectomy were randomized (1:1) to receive either Avastin (10 mg/kg IV infusion every 2 weeks; n = 327) or placebo (IV every 2 weeks; n = 322) in combination with IFN‑α2a (9 MIU subcutaneously three times weekly, for a maximum of 52 weeks). Patients were treated until disease progression or unacceptable toxicity. The main outcome measure of the study was investigator‑assessed PFS. Secondary outcome measures were ORR and OS.
The median age was 60 years (range 18–82), 96% were white, and 70% were male. The study population was characterized by Motzer scores as follows: 28% favorable (0), 56% intermediate (1‑2), 8% poor (3‑5), and 7% missing.
The results are presented in Figure 3. PFS was statistically significantly prolonged among patients receiving Avastin plus IFN‑α2a compared to those receiving IFN‑α2a alone; median PFS was 10.2 months vs. 5.4 months [HR 0.60 (95% CI 0.49, 0.72), p‐value < 0.0001, stratified log‑rank test]. Among the 595 patients with measureable disease, ORR was also significantly higher (30% vs. 12%, p < 0.0001, stratified CMH test). There was no improvement in OS based on the final analysis conducted after 444 deaths, with a median OS of 23 months in the Avastin plus IFN‑α2a arm and 21 months in the IFN‑α2a plus placebo arm [HR 0.86, (95% CI 0.72, 1.04)].
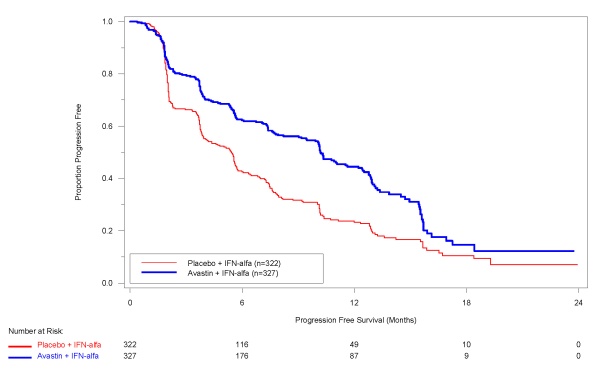 |
16 HOW SUPPLIED/STORAGE AND HANDLING
Avastin vials [100 mg (NDC‑50242‑060‑01) and 400 mg (NDC 50242‑061‑01)] are stable at 2–8°C (36–42°F). Avastin vials should be protected from light. Do not freeze or shake.
Diluted Avastin solutions may be stored at 2–8°C (36–46°F) for up to 8 hours. Store in the original carton until time of use. No incompatibilities between Avastin and polyvinylchloride or polyolefin bags have been observed.
17 PATIENT COUNSELING INFORMATION
Advise patients:
- To undergo routine blood pressure monitoring and to contact their health care provider if blood pressure is elevated.
- To immediately contact their health care provider for unusual bleeding, high fever, rigors, sudden onset of worsening neurological function, or persistent or severe abdominal pain, severe constipation, or vomiting.
- Of increased risk of wound healing complications during and following Avastin.
- Of increased risk of an arterial thromboembolic event.
- Of the potential risk to the fetus during and following Avastin and the need to continue adequate contraception for at least 6 months following last dose of Avastin.
Manufactured by:
Genentech, Inc.
1 DNA Way
South San Francisco,
CA 94080‑4990
7455316
LV0017
4835706
Initial U.S. Approval: February
2004
Code Revision Date: July 2009
© 2009 Genentech, Inc.
Avastin 100mg Principal Display Panel

Avastin 400mg Principal Display Panel
| AVASTIN
bevacizumab injection, solution |
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
| Marketing Information | |||
| Marketing Category | Application Number or Monograph Citation | Marketing Start Date | Marketing End Date |
| BLA | BLA125085 | 02/26/2004 | |
| AVASTIN
bevacizumab injection, solution |
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
| Marketing Information | |||
| Marketing Category | Application Number or Monograph Citation | Marketing Start Date | Marketing End Date |
| BLA | BLA125085 | 02/26/2004 | |
| Labeler - Genentech, Inc. (080129000) |
| Registrant - Genentech, Inc. (080129000) |
| Establishment | |||
| Name | Address | ID/FEI | Operations |
| Genentech, Inc. (SSF) | 010024839 | manufacture, analysis | |
| Establishment | |||
| Name | Address | ID/FEI | Operations |
| Genentech, Inc. (Vacaville) | 004074162 | manufacture | |
| Establishment | |||
| Name | Address | ID/FEI | Operations |
| Genentech, Inc. (Oceanside) | 146373191 | manufacture | |