serevent (salmeterol xinafoate) aerosol
[GlaxoSmithKline]
WARNING
Data from a large placebo-controlled us study that compared the safety of salmeterol (SEREVENT Inhalation Aerosol) or placebo added to usual asthma therapy showed a small but significant increase in asthma-related deaths in patients receiving salmeterol (13 deaths out of 13,176 patients treated for 28 weeks) versus those on placebo (3 of 13,179) (see WARNINGS and CLINICAL TRIALS: Asthma: Salmeterol Multi-center Asthma Research Trial).
DESCRIPTION
SEREVENT (salmeterol xinafoate) Inhalation Aerosol contains salmeterol xinafoate as the racemic form of the 1-hydroxy-2-naphthoic acid salt of salmeterol. The active component of the formulation is salmeterol base, a highly selective beta2-adrenergic bronchodilator. The chemical name of salmeterol xinafoate is 4-hydroxy-α1-[[[6-(4-phenylbutoxy)hexyl]amino]methyl]-1,3-benzenedimethanol, 1-hydroxy-2-naphthalenecarboxylate. Salmeterol xinafoate has the following chemical structure:
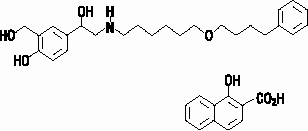
The molecular weight of salmeterol xinafoate is 603.8, and the empirical formula is C25H37NO4•C11H8O3. Salmeterol xinafoate is a white to off-white powder. It is freely soluble in methanol; slightly soluble in ethanol, chloroform, and isopropanol; and sparingly soluble in water.
SEREVENT Inhalation Aerosol is a pressurized, metered-dose aerosol unit for oral inhalation. It contains a microcrystalline suspension of salmeterol xinafoate in a mixture of 2 chlorofluorocarbon propellants (trichlorofluoromethane and dichlorodifluoromethane) with soya lecithin. 36.25 mcg of salmeterol xinafoate is equivalent to 25 mcg of salmeterol base. Each actuation delivers 25 mcg of salmeterol base (as salmeterol xinafoate) from the valve and 21 mcg of salmeterol base (as salmeterol xinafoate) from the actuator. Each 6.5-g canister provides 60 inhalations and each 13-g canister provides 120 inhalations.
CLINICAL PHARMACOLOGY
Mechanism of Action
Salmeterol is a long-acting beta2-adrenergic agonist. In vitro studies and in vivo pharmacologic studies demonstrate that salmeterol is selective for beta2-adrenoceptors compared with isoproterenol, which has approximately equal agonist activity on beta1- and beta2-adrenoceptors. In vitrostudies show salmeterol to be at least 50 times more selective for beta2-adrenoceptors than albuterol. Although beta2-adrenoceptors are the predominant adrenergic receptors in bronchial smooth muscle and beta1-adrenoceptors are the predominant receptors in the heart, there are also beta2-adrenoceptors in the human heart comprising 10% to 50% of the total beta-adrenoceptors. The precise function of these is not yet established, but they raise the possibility that even highly selective beta2-agonists may have cardiac effects.
The pharmacologic effects of beta2-adrenoceptor agonist drugs, including salmeterol, are at least in part attributable to stimulation of intracellular adenyl cyclase, the enzyme that catalyzes the conversion of adenosine triphosphate (ATP) to cyclic-3′,5′-adenosine monophosphate (cyclic AMP). Increased cyclic AMP levels cause relaxation of bronchial smooth muscle and inhibition of release of mediators of immediate hypersensitivity from cells, especially from mast cells.
In vitro tests show that salmeterol is a potent and long-lasting inhibitor of the release of mast cell mediators, such as histamine, leukotrienes, and prostaglandin D2, from human lung. Salmeterol inhibits histamine-induced plasma protein extravasation and inhibits platelet activating factor-induced eosinophil accumulation in the lungs of guinea pigs when administered by the inhaled route. In humans, single doses of salmeterol attenuate allergen-induced bronchial hyper-responsiveness.
Pharmacokinetics
Salmeterol xinafoate, an ionic salt, dissociates in solution so that the salmeterol and 1-hydroxy-2-naphthoic acid (xinafoate) moieties are absorbed, distributed, metabolized, and excreted independently. Salmeterol acts locally in the lung; therefore, plasma levels do not predict therapeutic effect.
Absorption
Because of the small therapeutic dose, systemic levels of salmeterol are low or undetectable after inhalation of recommended doses (42 mcg of salmeterol inhalation aerosol twice daily). Following chronic administration of an inhaled dose of 42 mcg twice daily, salmeterol was detected in plasma within 5 to 10 minutes in 6 patients with asthma; plasma concentrations were very low, with peak concentrations of 150 pg/mL and no accumulation with repeated doses. Larger inhaled doses gave approximately proportionally increased blood levels. In these patients, a second peak concentration of 115 pg/mL occurred at about 45 minutes, probably due to absorption of the swallowed portion of the dose (most of the dose delivered by a metered-dose inhaler is swallowed).
Distribution
Binding of salmeterol to human plasma proteins averages 96% in vitro over the concentration range of 8 to 7,722 ng of salmeterol base per milliliter, much higher than those achieved following therapeutic doses of salmeterol.
Metabolism
Salmeterol base is extensively metabolized by hydroxylation, with subsequent elimination predominantly in the feces. No significant amount of unchanged salmeterol base was detected in either urine or feces.
Excretion
In 2 healthy subjects who received 1 mg of radiolabeled salmeterol (as salmeterol xinafoate) orally, approximately 25% and 60% of the radiolabeled salmeterol was eliminated in urine and feces, respectively, over a period of 7 days. The terminal elimination half-life was about 5.5 hours (1 volunteer only).
The xinafoate moiety has no apparent pharmacologic activity. The xinafoate moiety is highly protein bound (>99%) and has a long elimination half-life of 11 days.
Special Populations
The pharmacokinetics of salmeterol base has not been studied in elderly patients or in patients with hepatic or renal impairment. Since salmeterol is predominantly cleared by hepatic metabolism, liver function impairment may lead to accumulation of salmeterol in plasma. Therefore, patients with hepatic disease should be closely monitored.
Pharmacodynamics
Inhaled salmeterol, like other beta-adrenergic agonist drugs, can in some patients produce dose-related cardiovascular effects and effects on blood glucose and/or serum potassium (see PRECAUTIONS). The cardiovascular effects (heart rate, blood pressure) associated with salmeterol occur with similar frequency, and are of similar type and severity, as those noted following albuterol administration.
The effects of rising doses of salmeterol and standard inhaled doses of albuterol were studied in volunteers and in patients with asthma. Salmeterol doses up to 84 mcg administered as inhalation aerosol resulted in heart rate increases of 3 to 16 beats/min, about the same as albuterol dosed at 180 mcg by inhalation aerosol (4 to 10 beats/min). In 2 double-blind asthma studies, patients receiving either 42 mcg of salmeterol inhalation aerosol twice daily (N = 81) or 180 mcg of albuterol inhalation aerosol 4 times daily (N = 80) underwent continuous electrocardiographic monitoring during four 24-hour periods; no clinically significant dysrhythmias were noted. Continuous electrocardiographic monitoring was also performed in 2 double-blind studies in patients with chronic obstructive pulmonary disease (COPD) (see ADVERSE REACTIONS).
Studies in laboratory animals (minipigs, rodents, and dogs) have demonstrated the occurrence of cardiac arrhythmias and sudden death (with histologic evidence of myocardial necrosis) when beta-agonists and methylxanthines are administered concurrently. The clinical significance of these findings is unknown.
CLINICAL TRIALS
Asthma
In placebo- and albuterol-controlled, single-dose clinical trials with SEREVENT Inhalation Aerosol, the time to onset of effective bronchodilatation (>15% improvement in forced expiratory volume in 1 second [FEV1]) was 10 to 20 minutes after a 42-mcg dose. Maximum improvement in FEV1 generally occurred within 180 minutes, and clinically significant improvement continued for 12 hours in most patients.
In 2 large, randomized, double-blind studies, SEREVENT Inhalation Aerosol was compared with albuterol and placebo in patients with mild-to-moderate asthma, including both patients who did and who did not receive concomitant inhaled corticosteroids. The efficacy of SEREVENT Inhalation Aerosol was demonstrated over the 12-week period with no change in effectiveness over this period of time. There were no gender-related differences in safety or efficacy. No development of tachyphylaxis to the bronchodilator effect has been noted in these studies. FEV1 measurements (percent of predicted) from these two 12-week trials are shown in Figure 1 for both the first and last treatment days.
Figure 1. FEV1, as Percent of Predicted, From 2 Large 12-Week Clinical Trials
First Treatment Day
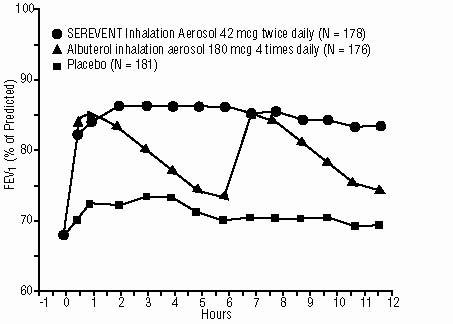
Last Treatment Day (Week 12)
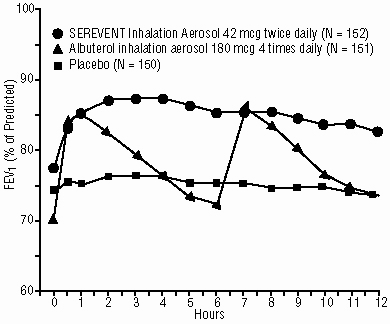
Table 1 shows the treatment effects seen during daily treatment with SEREVENT Inhalation Aerosol for 12 weeks in patients with asthma.
|
Parameter |
Time |
Placebo |
SEREVENT Inhalation Aerosol |
Albuterol Inhalation Aerosol |
|
No. of randomized subjects |
187 |
184 |
185 |
|
|
Mean AM peak expiratory flow (L/min) |
baseline 12 weeks |
412 414 |
409 438* |
398 390 |
|
Mean % days with no asthma symptoms |
baseline 12 weeks |
11 17 |
11 35* |
14 24 |
|
Mean % nights with no awakenings |
baseline 12 weeks |
67 74 |
67 87* |
65 74 |
|
Rescue medications (mean no. of inhalations per day) |
baseline 12 weeks |
4.4 3.3 |
4.1 1.3†‡ |
4.0 1.9 |
|
Asthma exacerbations |
17% |
11% |
14% |
*p<0.001 versus albuterol and placebo.
†p<0.05 versus albuterol.
‡p<0.001 versus placebo.
Safe usage with maintenance of efficacy for periods up to 1 year has been documented.
Effects in Patients With Asthma on Concomitant Inhaled Corticosteroids
In 4 clinical trials in adult and adolescent patients with asthma (N = 1,922), the effect of adding salmeterol to inhaled corticosteroid therapy was evaluated. The studies utilized the inhalation aerosol formulation of salmeterol xinafoate for a treatment period of 6 months. They compared the addition of salmeterol therapy to an increase (at least doubling) of the inhaled corticosteroid dose.
Two randomized, double-blind, parallel-group clinical trials (N = 997) enrolled patients (ages 18 to 82 years) with persistent asthma who were previously maintained but not adequately controlled on inhaled corticosteroid therapy. During the 2-week run-in period, all patients were switched to beclomethasone dipropionate 168 mcg twice daily. Patients still not adequately controlled were randomized to either the addition of SEREVENT Inhalation Aerosol 42 mcg twice daily or an increase of beclomethasone dipropionate to 336 mcg twice daily. As compared to the doubled dose of beclomethasone dipropionate, the addition of salmeterol resulted in statistically significantly greater improvements in pulmonary function and asthma symptoms, and statistically significantly greater reduction in supplemental albuterol use. The percent of patients who experienced asthma exacerbations overall was not different between groups (i.e., 16.2% in the salmeterol group versus 17.9% in the higher-dose beclomethasone dipropionate group).
Two randomized, double-blind, parallel-group clinical trials (N = 925) enrolled patients (ages 12 to 78 years) with persistent asthma who were previously maintained but not adequately controlled on prior therapy. During the 2- to 4-week run-in period, all patients were switched to fluticasone propionate 88 mcg twice daily. Patients still not adequately controlled were randomized to either the addition of SEREVENT Inhalation Aerosol 42 mcg twice daily or an increase of fluticasone propionate to 220 mcg twice daily. As compared to the increased (2.5 times) dose of fluticasone propionate, the addition of salmeterol resulted in statistically significantly greater improvements in pulmonary function and asthma symptoms, and statistically significantly greater reduction in supplemental albuterol use. Fewer patients receiving salmeterol experienced asthma exacerbations than those receiving the higher dose of fluticasone propionate (8.8% versus 13.8%).
Salmeterol Multi-center Asthma Research Trial
The Salmeterol Multi-center Asthma Research Trial (SMART) was a randomized, double-blind study that enrolled long-acting beta2-agonist−naive patients with asthma (average age of 39 years, 71% Caucasian, 18% African American, 8% Hispanic) to assess the safety of salmeterol (SEREVENTInhalation Aerosol, 42 mcg twice daily over 28 weeks) compared to placebo when added to usual asthma therapy. The primary endpoint was the combined number of respiratory-related deaths or respiratory-related life-threatening experiences (intubation and mechanical ventilation). Secondary endpoints included combined asthma-related deaths or life-threatening experiences and asthma-related deaths. A planned interim analysis was conducted when approximately half of the intended number of patients had been enrolled (N = 26,355).
Due to the low rate of primary events in the study, the findings of the planned interim analysis were not conclusive. However, analyses of secondary endpoints suggested that patients receiving salmeterol may be at increased risk for some of these events compared to patients receiving placebo. The analysis for the total population showed a relative risk of 1.40 (95% CI 0.91, 2.14) for the primary endpoint in the salmeterol group relative to the placebo group (50 out of 13,176 vs. 36 out of 13,179, respectively). In the total population, a higher number of asthma-related deaths (13 vs. 3, RR 4.37, 95% CI 1.25, 15.34) and combined asthma-related deaths or life-threatening experiences (37 vs. 22, RR 1.71, 95% CI 1.01, 2.89) occurred in patients treated with salmeterol than those treated with placebo. The analysis of the African American subgroup showed a relative risk of 4.10 (95% CI 1.54, 10.90) for the primary endpoint in patients treated with salmeterol relative to those treated with placebo (20 out of 2,366 vs. 5 out of 2,319, respectively). In African Americans, a higher number of asthma-related deaths (7 vs. 1, RR 7.26, 95% CI 0.89, 58.94) and combined asthma-related deaths or life-threatening experiences (19 vs. 4, RR 4.92, 95% CI 1.68, 14.45) occurred in patients treated with salmeterol than those treated with placebo. Analysis of the Caucasian population showed a relative risk of 1.05 (95% CI 0.62, 1.76) for the primary endpoint for those treated with salmeterol relative to those treated with placebo (29 out of 9,281 vs. 28 out of 9,361, respectively). In Caucasians, a higher number of asthma-related deaths (6 vs. 1, RR 5.82, 95% CI 0.70, 48.37) occurred in patients treated with salmeterol than in patients treated with placebo. In Caucasians, the relative risk was 1.08 (17 vs. 16, 95% CI 0.55, 2.14) for combined asthma-related deaths or life-threatening experiences in patients treated with salmeterol relative to placebo. The numbers of patients from other ethnic groups were too small to draw any conclusions in these populations. Even though SMART did not reach predetermined stopping criteria for the total population, the study was stopped due to the findings in African American patients and difficulties in enrollment.
Exercise-Induced Bronchospasm
Protection against exercise-induced bronchospasm (EIB) was examined in 3 controlled studies. Based on median values, patients who received SEREVENT Inhalation Aerosol had consistently less exercise-induced fall in FEV1 than patients who received placebo, and they were protected for a longer period of time than patients who received albuterol (see Table 2). There were, however, some patients who were not protected from EIB after SEREVENT administration and others in whom protection against EIB decreased with continued administration over a period of 4 weeks.
|
Clinical Trials/Time After Dose |
Treatment |
||
|
Placebo |
SEREVENT Inhalation Aerosol |
Albuterol Inhalation Aerosol |
|
|
Study A: 1st Dose |
|||
|
6 hours |
37 |
9* |
|
|
12 hours |
27 |
16* |
|
|
Study A: 4th Week |
|||
|
6 hours |
30 |
19 |
|
|
12 hours |
24 |
12 |
|
|
Study B: |
|||
|
1 hour |
37 |
0* |
2* |
|
6 hours |
37 |
5*† |
27 |
|
12 hours |
34 |
6*† |
33 |
|
Study C: |
|||
|
0.5 hour |
43 |
16* |
8* |
|
2.5 hours |
33 |
12*† |
30 |
|
4.5 hours |
-- |
12† |
36 |
|
6.0 hours |
-- |
19† |
41 |
*Statistically superior to placebo (p≤0.05).
†Statistically superior to albuterol (p≤0.05).
Chronic Obstructive Pulmonary Disease
In 2 large randomized, double-blind studies, SEREVENT Inhalation Aerosol administered twice daily was compared with placebo and ipratropium bromide inhalation aerosol administered 4 times daily in patients with COPD (emphysema and chronic bronchitis), including patients who were reversible (≥12% and ≥200 mL increase in baseline FEV1 after albuterol treatment) and nonreversible to albuterol. After a single 42-mcg dose of SEREVENT, significant improvement in pulmonary function (mean FEV1 increase of 12% or more) occurred within 30 minutes, reached a peak within 4 hours on average, and persisted for 12 hours with no loss in effectiveness observed over a 12-week treatment period. Figure 2 displays serial 12-hour measurements of FEV1 from these two 12-week trials for both the first and last treatment days.
Figure 2. FEV1 From 2 Large 12-Week Clinical Trials
First Treatment Day
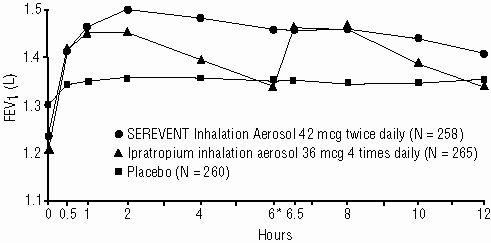
* Ipratropium inhalation aerosol (or matching placebo) administered immediately following hour 6 assessment.
Last Treatment Day (Week 12)
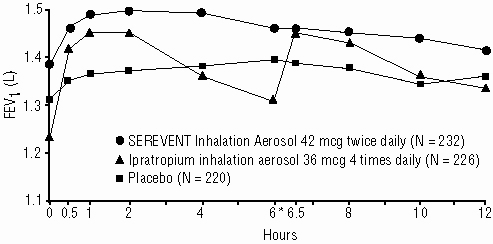
* Ipratropium inhalation aerosol (or matching placebo) administered immediately following hour 6 assessment.
INDICATIONS AND USAGE
Asthma
SEREVENT Inhalation Aerosol is indicated for long-term, twice-daily (morning and evening) administration in the maintenance treatment of asthma and in the prevention of bronchospasm in patients 12 years of age and older with reversible obstructive airway disease, including patients with symptoms of nocturnal asthma, who require regular treatment with inhaled, short-acting beta2-agonists. It should not be used in patients whose asthma can be managed by occasional use of inhaled, short-acting beta2-agonists.
SEREVENT Inhalation Aerosol may be used alone or in combination with inhaled or systemic corticosteroid therapy.
SEREVENT Inhalation Aerosol is also indicated for prevention of exercise-induced bronchospasm in patients 12 years of age and older.
Chronic Obstructive Pulmonary Disease
SEREVENT Inhalation Aerosol is indicated for long-term, twice daily (morning and evening) administration in the maintenance treatment of bronchospasm associated with COPD (including emphysema and chronic bronchitis).
CONTRAINDICATIONS
SEREVENT Inhalation Aerosol is contraindicated in patients with a history of hypersensitivity to salmeterol or any other component of the drug product (see DESCRIPTION).
WARNINGS
DATA FROM A LARGE PLACEBO-CONTROLLED SAFETY STUDY THAT WAS STOPPED EARLY SUGGEST THAT SALMETEROL MAY BE ASSOCIATED WITH RARE SERIOUS ASTHMA EPISODES OR ASTHMA-RELATED DEATHS. Data from this study, called the Salmeterol Multi-center Asthma Research Trial (SMART), further suggest that the risk might be greater in African American patients. These results led to stopping the study prematurely (see CLINICAL TRIALS: Asthma: Salmeterol Multi-center Asthma Research Trial). The data from the SMART study are not adequate to determine whether concurrent use of inhaled corticosteroids provides protection from this risk. Given the similar basic mechanisms of action of beta2-agonists, it is possible that the findings seen in the SMART study may be consistent with a class effect.
Findings similar to the SMART study findings were reported in a prior 16-week clinical study performed in the United Kingdom, the Salmeterol Nationwide Surveillance (SNS) study. In the SNS study, the incidence of asthma-related death was numerically, though not statistically, greater in patients with asthma treated with salmeterol (42 mcg twice daily) versus albuterol (180 mcg 4 times daily) added to usual asthma therapy.
SEREVENT INHALATION AEROSOL SHOULD NOT BE INITIATED IN PATIENTS WITH SIGNIFICANTLY WORSENING OR ACUTELY DETERIORATING ASTHMA, WHICH MAY BE A LIFE-THREATENING CONDITION. Serious acute respiratory events, including fatalities, have been reported, both in the United States and worldwide, when SEREVENT Inhalation Aerosol has been initiated in this situation.
Although it is not possible from these reports to determine whether SEREVENT Inhalation Aerosol contributed to these adverse events or simply failed to relieve the deteriorating asthma, the use of SEREVENT Inhalation Aerosol in this setting is inappropriate.
SEREVENT INHALATION AEROSOL SHOULD NOT BE USED TO TREAT ACUTE SYMPTOMS. It is crucial to inform patients of this and prescribe an inhaled, short-acting beta2-agonist for this purpose as well as warn them that increasing inhaled beta2-agonist use is a signal of deteriorating asthma.
SEREVENT INHALATION AEROSOL IS NOT A SUBSTITUTE FOR INHALED OR ORAL CORTICOSTEROIDS. Corticosteroids should not be stopped or reduced when SEREVENT Inhalation Aerosol is initiated.
(See PRECAUTIONS: Information for Patients and the PATIENT'S INSTRUCTIONS FOR USE accompanying the product.)
1. Do Not Introduce SEREVENT Inhalation Aerosol as a Treatment for Acutely Deteriorating Asthma: SEREVENT Inhalation Aerosol is intended for the maintenance treatment of asthma (see INDICATIONS AND USAGE) and should not be introduced in acutely deteriorating asthma, which is a potentially life-threatening condition. There are no data demonstrating that SEREVENT Inhalation Aerosol provides greater efficacy than or additional efficacy to inhaled, short-acting beta2-agonists in patients with worsening asthma. Serious acute respiratory events, including fatalities, have been reported both in the United States and worldwide in patients receiving SEREVENT Inhalation Aerosol. In most cases, these have occurred in patients with severe asthma (e.g., patients with a history of corticosteroid dependence, low pulmonary function, intubation, mechanical ventilation, frequent hospitalizations, or previous lifethreatening acute asthma exacerbations) and/or in some patients in whom asthma has been acutely deteriorating (e.g., unresponsive to usual medications; increasing need for inhaled, shortacting beta2-agonists; increasing need for systemic corticosteroids; significant increase in symptoms; recent emergency room visits; sudden or progressive deterioration in pulmonary function). However, they have occurred in a few patients with less severe asthma as well. It was not possible from these reports to determine whether SEREVENT Inhalation Aerosol contributed to these events or simply failed to relieve the deteriorating asthma.
2. Do Not Use SEREVENT Inhalation Aerosol to Treat Acute Symptoms: An inhaled, short-acting beta2-agonist, not SEREVENT Inhalation Aerosol, should be used to relieve acute asthma or COPD symptoms. When prescribing SEREVENT Inhalation Aerosol, the physician must also provide the patient with an inhaled, short-acting beta2-agonist (e.g., albuterol) for treatment of symptoms that occur acutely, despite regular twice-daily (morning and evening) use of SEREVENT Inhalation Aerosol.
When beginning treatment with SEREVENT Inhalation Aerosol, patients who have been taking inhaled, short-acting beta2-agonists on a regular basis (e.g., 4 times a day) should be instructed to discontinue the regular use of these drugs and use them only for symptomatic relief of acute asthma or COPD symptoms (see PRECAUTIONS: Information for Patients).
3. Watch for Increasing Use of Inhaled, Short-Acting Beta2-Agonists, Which Is a Marker of Deteriorating Asthma: Asthma may deteriorate acutely over a period of hours or chronically over several days or longer. If the patient’s inhaled, short-acting beta2-agonist becomes less effective or the patient needs more inhalations than usual, this may be a marker of destabilization of asthma. In this setting, the patient requires immediate reevaluation with reassessment of the treatment regimen, giving special consideration to the possible need for corticosteroids. If the patient uses 4 or more inhalations per day of an inhaled, short-acting beta2-agonist for 2 or more consecutive days, or if more than 1 canister (200 inhalations per canister) of inhaled, short-acting beta2-agonist is used in an 8-week period in conjunction with SEREVENT Inhalation Aerosol, then the patient should consult the physician for reevaluation. Increasing the daily dosage of SEREVENT Inhalation Aerosol in this situation is not appropriate. SEREVENT Inhalation Aerosol should not be used more frequently than twice daily (morning and evening) at the recommended dose of 2 inhalations.
4. Do Not Use SEREVENT Inhalation Aerosol as a Substitute for Oral or Inhaled Corticosteroids: The use of beta-adrenergic agonist bronchodilators alone may not be adequate to control asthma in many patients. Early consideration should be given to adding anti-inflammatory agents, e.g., corticosteroids. There are no data demonstrating that SEREVENT Inhalation Aerosol has a clinical anti-inflammatory effect and could be expected to take the place of corticosteroids. Patients who already require oral or inhaled corticosteroids for treatment of asthma should be continued on this type of treatment even if they feel better as a result of initiating SEREVENT Inhalation Aerosol. Any change in corticosteroid dosage should be made ONLY after clinical evaluation (see PRECAUTIONS: Information for Patients).
5. Do Not Exceed Recommended Dosage: As with other inhaled beta2-adrenergic drugs, SEREVENT Inhalation Aerosol should not be used more often or at higher doses than recommended. Fatalities have been reported in association with excessive use of inhaled sympathomimetic drugs. Large doses of inhaled or oral salmeterol (12 to 20 times the recommended dose) have been associated with clinically significant prolongation of the QTc interval, which has the potential for producing ventricular arrhythmias.
6. Paradoxical Bronchospasm: SEREVENT Inhalation Aerosol can produce paradoxical bronchospasm, which may be life threatening. If paradoxical bronchospasm occurs, SEREVENT Inhalation Aerosol should be discontinued immediately and alternative therapy instituted. It should be recognized that paradoxical bronchospasm, when associated with inhaled formulations, frequently occurs with the first use of a new canister or vial.
7. Immediate Hypersensitivity Reactions: Immediate hypersensitivity reactions may occur after administration of SEREVENT Inhalation Aerosol, as demonstrated by rare cases of urticaria, angioedema, rash, and bronchospasm.
8. Upper Airway Symptoms: Symptoms of laryngeal spasm, irritation, or swelling, such as stridor and choking, have been reported rarely in patients receiving SEREVENT Inhalation Aerosol.
SEREVENT Inhalation Aerosol, like all other beta-adrenergic agonists, can produce a clinically significant cardiovascular effect in some patients as measured by pulse rate, blood pressure, and/or symptoms. Although such effects are uncommon after administration of SEREVENT Inhalation Aerosol at recommended doses, if they occur, the drug may need to be discontinued. In addition, beta-agonists have been reported to produce electrocardiogram (ECG) changes, such as flattening of the T wave, prolongation of the QTc interval, and ST segment depression. The clinical significance of these findings is unknown. Therefore, SEREVENT Inhalation Aerosol, like all sympathomimetic amines, should be used with caution in patients with cardiovascular disorders, especially coronary insufficiency, cardiac arrhythmias, and hypertension.
PRECAUTIONS
General
1. Use With Spacer or Other Devices: The safety and effectiveness of SEREVENT Inhalation Aerosol when used with a spacer or other devices have not been adequately studied.
2. Cardiovascular and Other Effects: No effect on the cardiovascular system is usually seen after the administration of inhaled salmeterol in recommended doses, but the cardiovascular and central nervous system effects seen with all sympathomimetic drugs (e.g., increased blood pressure, heart rate, excitement) can occur after use of salmeterol and may require discontinuation of the drug. SEREVENT Inhalation Aerosol, like all sympathomimetic amines, should be used with caution in patients with cardiovascular disorders, especially coronary insufficiency, cardiac arrhythmias, and hypertension; in patients with convulsive disorders or thyrotoxicosis; and in patients who are unusually responsive to sympathomimetic amines.
As has been described with other beta-adrenergic agonist bronchodilators, clinically significant changes in systolic and/or diastolic blood pressure, pulse rate, and ECGs have been seen infrequently in individual patients in controlled clinical studies with salmeterol.
3. Metabolic Effects: Doses of the related beta2-adrenoceptor agonist albuterol, when administered intravenously, have been reported to aggravate preexisting diabetes mellitus and ketoacidosis. No effects on glucose have been seen with SEREVENT Inhalation Aerosol at recommended doses. Beta-adrenergic agonist medications may produce significant hypokalemia in some patients, possibly through intracellular shunting, which has the potential to produce adverse cardiovascular effects. The decrease is usually transient, not requiring supplementation.
Clinically significant changes in blood glucose and/or serum potassium were seen rarely during clinical studies with long-term administration of SEREVENT Inhalation Aerosol at recommended doses.
Information for Patients
See illustrated PATIENT’S INSTRUCTIONS FOR USE. SHAKE WELL BEFORE USING.
It is important that patients understand how to use SEREVENT Inhalation Aerosol appropriately and how it should be used in relation to other asthma or COPD medications they are taking. Patients should be given the following information:
- Shake well before using.
- The action of SEREVENT Inhalation Aerosol may last up to 12 hours or longer. The recommended dosage (2 inhalations twice daily, morning and evening) should not be exceeded.
- SEREVENT Inhalation Aerosol is not meant to relieve acute asthma or COPD symptoms and extra doses should not be used for that purpose. Acute symptoms should be treated with an inhaled, short-acting beta2-agonist such as albuterol (the physician should provide the patient with such medication and instruct the patient in how it should be used).
- Patients should not stop SEREVENT therapy for asthma or COPD without physician/provider guidance since symptoms may recur after discontinuation.
- The physician should be notified immediately if any of the following
situations occur, which may be a sign of seriously worsening asthma.
- Decreasing effectiveness of inhaled, short-acting beta2-agonists
- Need for more inhalations than usual of inhaled, short-acting beta2-agonists
- Use of 4 or more inhalations per day of a short-acting beta2-agonist for 2 or more days consecutively
- Use of more than one 200-inhalation canister of an inhaled, short-acting beta2-agonist (e.g., albuterol) in an 8-week period
- SEREVENT Inhalation Aerosol should not be used as a substitute for oral or inhaled corticosteroids. The dosage of these medications should not be changed and they should not be stopped without consulting the physician, even if the patient feels better after initiating treatment with SEREVENT Inhalation Aerosol.
- Patients should be cautioned regarding common adverse cardiovascular effects, such as palpitations, chest pain, rapid heart rate, tremor, or nervousness.
- In patients receiving SEREVENT Inhalation Aerosol, other inhaled medications should be used only as directed by the physician.
- When using SEREVENT Inhalation Aerosol to prevent exercise-induced bronchospasm, patients should take the dose at least 30 to 60 minutes before exercise.
- Patients who are pregnant or nursing should contact the physician about the use of SEREVENT Inhalation Aerosol.
- Effective and safe use of SEREVENT Inhalation Aerosol includes an understanding of the way that it should be administered.
Drug Interactions
Short-Acting Beta2-Agonists
Monoamine Oxidase Inhibitors and Tricyclic Antidepressants
Salmeterol should be administered with extreme caution to patients being treated with monoamine oxidase inhibitors or tricyclic antidepressants, or within 2 weeks of discontinuation of such agents, because the action of salmeterol on the vascular system may be potentiated by these agents.
Corticosteroids and Cromoglycate
In clinical trials, inhaled corticosteroids and/or inhaled cromolyn sodium did not alter the safety profile of SEREVENT Inhalation Aerosol when administered concurrently.
Methylxanthines
The concurrent use of intravenously or orally administered methylxanthines (e.g., aminophylline, theophylline) by patients receiving SEREVENT Inhalation Aerosol has not been completely evaluated. In 1 clinical asthma trial, 87 patients receiving SEREVENT Inhalation Aerosol 42 mcg twice daily concurrently with a theophylline product had adverse event rates similar to those in 71 patients receiving SEREVENT Inhalation Aerosol without theophylline. Resting heart rates were slightly higher in the patients on theophylline but were little affected by SEREVENT Inhalation Aerosol therapy.
Beta-adrenergic receptor blocking agents not only block the pulmonary effect of beta-agonists, such as SEREVENT Inhalation Aerosol, but may also produce severe bronchospasm in patients with asthma. Therefore, patients with asthma should not normally be treated with beta-blockers. However, under certain circumstances, e.g., as prophylaxis after myocardial infarction, there may be no acceptable alternatives to the use of beta-adrenergic blocking agents in patients with asthma. In this setting, cardioselective beta-blockers could be considered, although they should be administered with caution.
The ECG changes and/or hypokalemia that may result from the administration of nonpotassium-sparing diuretics (such as loop or thiazide diuretics) can be acutely worsened by beta-agonists, especially when the recommended dose of the beta-agonist is exceeded. Although the clinical significance of these effects is not known, caution is advised in the coadministration of beta-agonists with nonpotassium-sparing diuretics.
Carcinogenesis, Mutagenesis, Impairment of Fertility
In an 18-month oral carcinogenicity study in CD-mice, salmeterol xinafoate at oral doses of 1.4 mg/kg and above (approximately 9 times the maximum recommended daily inhalation dose in adults based on comparison of the areas under the plasma concentration versus time curves [AUCs]) caused dose-related increases in the incidence of smooth muscle hyperplasia, cystic glandular hyperplasia, leiomyomas of the uterus, and cysts in the ovaries. The incidence of leiomyosarcomas was not statistically significant. No tumors were seen at 0.2 mg/kg (comparable to the maximum recommended human daily inhalation dose in adults based on comparison of the AUCs).
In a 24-month inhalation and oral carcinogenicity study in Sprague Dawley rats, salmeterol caused dose-related increases in the incidence of mesovarian leiomyomas and ovarian cysts at inhalation and oral doses of 0.68 mg/kg/day and above (approximately 55 times the maximum recommended human daily inhalation dose in adults on a mg/m2 basis). No tumors were seen at 0.21 mg/kg/day (approximately 15 times the maximum recommended human daily inhalation dose in adults on a mg/m2 basis). These findings in rodents are similar to those reported previously for other beta-adrenergic agonist drugs. The relevance of these findings to human use is unknown.
Salmeterol xinafoate produced no detectable or reproducible increases in microbial and mammalian gene mutation in vitro. No clastogenic activity occurred in vitro in human lymphocytes or in vivo in a rat micronucleus test. No effects on fertility were identified in male and female rats treated orally with salmeterol xinafoate at doses up to 2 mg/kg (approximately 160 times the maximum recommended human daily inhalation dose in adults on a mg/m2 basis).
Pregnancy
Teratogenic Effects
Pregnancy Category C. No teratogenic effects occurred in the rat at oral doses up to 2 mg/kg (approximately 160 times the maximum recommended human daily inhalation dose in adults on a mg/m2 basis). In pregnant Dutch rabbits administered oral doses of 1 mg/kg and above (approximately 20 times the maximum recommended human daily inhalation dose in adults based on the comparison of the AUCs), salmeterol xinafoate exhibited fetal toxic effects characteristically resulting from beta-adrenoceptor stimulation; these included precocious eyelid openings, cleft palate, sternebral fusion, limb and paw flexures, and delayed ossification of the frontal cranial bones. No significant effects occurred at an oral dose of 0.6 mg/kg (approximately 10 times the maximum recommended human daily inhalation dose in adults based on comparison of the AUCs).
New Zealand White rabbits were less sensitive since only delayed ossification of the frontal cranial bones was seen at oral doses of 10 mg/kg (approximately 1,600 times the maximum recommended human daily inhalation dose on a mg/m2 basis). Extensive use of other beta-agonists has provided no evidence that these class effects in animals are relevant to use in humans. There are no adequate and well-controlled studies with SEREVENT Inhalation Aerosol in pregnant women. SEREVENT Inhalation Aerosol should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Use in Labor and Delivery
There are no well-controlled human studies that have investigated effects of salmeterol on preterm labor or labor at term. Because of the potential for beta-agonist interference with uterine contractility, use of SEREVENT Inhalation Aerosol for prevention of bronchospasm during labor should be restricted to those patients in whom the benefits clearly outweigh the risks.
Nursing Mothers
Plasma levels of salmeterol after inhaled therapeutic doses are very low. In rats, salmeterol xinafoate is excreted in milk. However, since there is no experience with use of SEREVENT Inhalation Aerosol by nursing mothers, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother. Caution should be exercised when salmeterol xinafoate is administered to a nursing woman.
Pediatric Use
The safety and effectiveness of SEREVENT Inhalation Aerosol in children younger than 12 years of age have not been established.
Geriatric Use
Of the total number of patients who received SEREVENT Inhalation Aerosol in all asthma clinical studies, 241 were 65 years of age and older. Geriatric patients (65 years and older) with reversible obstructive airway disease were evaluated in 4 well-controlled studies of 3 weeks’ to 3 months’ duration. Two placebo-controlled, crossover studies evaluated twice-daily dosing with salmeterol for 21 to 28 days in 45 patients. An additional 75 geriatric patients were treated with salmeterol for 3 months in 2 large parallel-group, multicenter studies. These 120 patients experienced increases in AM and PM PEF and decreases in diurnal variation in PEF similar to responses seen in the total populations of the 2 latter studies. The adverse event type and frequency in geriatric patients were not different from those of the total populations studied.
In 2 large, randomized, double-blind, placebo-controlled 3-month studies involving patients with COPD, 133 patients using SEREVENT Inhalation Aerosol were 65 years and older. These patients experienced similar improvements in FEV1 as observed for patients younger than 65.
No apparent differences in the efficacy and safety of SEREVENT Inhalation Aerosol were observed when geriatric patients were compared with younger patients in asthma and COPD clinical trials. As with other beta2-agonists, however, special caution should be observed when using SEREVENT Inhalation Aerosol in geriatric patients who have concomitant cardiovascular disease that could be adversely affected by this class of drug. Based on available data, no adjustment of salmeterol dosage in geriatric patients is warranted.
ADVERSE REACTIONS
Adverse reactions to salmeterol are similar in nature to reactions to other selective beta2-adrenoceptor agonists, i.e., tachycardia; palpitations;immediate hypersensitivity reactions, including urticaria, angioedema, rash, bronchospasm (see WARNINGS); headache; tremor; nervousness; and paradoxical bronchospasm (see WARNINGS).
Asthma
Two multicenter, 12-week, controlled studies have evaluated twice-daily doses of SEREVENT Inhalation Aerosol in patients 12 years of age and older with asthma. Table 3 reports the incidence of adverse events in these 2 studies.
|
Adverse Event |
Percent of Patients |
||
|
Placebo (N = 187) |
SEREVENT Inhalation Aerosol 42 mcg Twice Daily (N = 184) |
Albuterol Inhalation Aerosol 180 mcg 4 Times Daily (N = 185) |
|
|
Ear, nose, and throat |
|||
|
Upper respiratory tract infection |
13 |
14 |
16* |
|
Nasopharyngitis |
12 |
14 |
11 |
|
Disease of nasal cavity/sinus |
4 |
6 |
1 |
|
Sinus headache |
2 |
4 |
<1 |
|
Gastrointestinal |
|||
|
Stomachache |
0 |
4 |
0 |
| Neurological | |||
|
Headache |
23 |
28 |
27 |
|
Tremor |
2 |
4 |
3 |
|
Respiratory |
|||
|
Cough |
6 |
7 |
3 |
|
Lower respiratory infection |
2 |
4 |
2 |
* The only adverse event classified as serious was 1 case of upper respiratory tract infection in a patient treated with albuterol.
Table 3 includes all events (whether considered drug-related or nondrug-related by the investigator) that occurred at a rate of over 3% in the group treated with SEREVENT Inhalation Aerosol and were more common in the group treated with SEREVENT Inhalation Aerosol than in the placebo group.
Pharyngitis, allergic rhinitis, dizziness/giddiness, and influenza occurred at 3% or more but were equally common on placebo. Other events occurring in the group treated with SEREVENT Inhalation Aerosol at a frequency of 1% to 3% were as follows:
Cardiovascular
Tachycardia, palpitations.
Ear, Nose, and Throat
Rhinitis, laryngitis.
Gastrointestinal
Nausea, viral gastroenteritis, nausea and vomiting, diarrhea, abdominal pain.
Hypersensitivity
Urticaria.
Mouth and Teeth
Dental pain.
Musculoskeletal
Pain in joint, back pain, muscle cramp/contraction, myalgia/myositis, muscular soreness.
Neurological
Nervousness, malaise/fatigue.
Respiratory
Tracheitis/bronchitis.
Skin
Rash/skin eruption.
Urogenital
Dysmenorrhea.
Data from small dose-response studies show an apparent dose relationship for tremor, nervousness, and palpitations.
In clinical trials evaluating concurrent therapy of salmeterol with inhaled corticosteroids, adverse events were consistent with those previously reported for salmeterol, or might otherwise be expected with the use of inhaled corticosteroids.
Chronic Obstructive Pulmonary Disease
Two multicenter, 12-week, controlled studies have evaluated twice-daily doses of SEREVENT Inhalation Aerosol in patients with COPD. Table 4 reports the incidence of adverse events in these 2 studies.
|
Adverse Event |
Percent of Patients |
||
|
Placebo (N = 278) |
SEREVENT Inhalation Aerosol 42 mcg Twice Daily (N = 267) |
Ipratropium Inhalation Aerosol 36 mcg 4 Times Daily (N = 271) |
|
|
Ear, nose, and throat |
|||
| Upper respiratory tract infection |
7 |
9 |
9 |
|
Sore throat |
3 |
8 |
6 |
|
Nasal sinus infection |
1 |
4 |
2 |
|
Gastrointestinal |
|||
|
Diarrhea |
3 |
5 |
4 |
|
Musculoskeletal |
|||
|
Back pain |
3 |
4 |
3 |
|
Neurological |
|||
|
Headache |
10 |
12 |
8 |
|
Respiratory |
|||
|
Chest congestion |
3 |
4 |
3 |
Table 4 includes all events (whether considered drug-related or nondrug-related by the investigator) that occurred at a rate of over 3% in the group treated with SEREVENT Inhalation Aerosol and were more common in the group treated with SEREVENT Inhalation Aerosol than in the placebo group.
Common cold, rhinorrhea, bronchitis, cough, exacerbation of chest congestion, chest pain, and dizziness occurred at 3% or more but were equally common on placebo. Other events occurring in the group treated with SEREVENT Inhalation Aerosol at a frequency of 1% to 3% were as follows:
Ear, Nose, and Throat
Cold symptoms, earache, epistaxis, nasal congestion, nasal sinus congestion, sneezing.
Gastrointestinal
Nausea, dyspepsia, gastric pain, gastric upset, abdominal pain, constipation, heartburn, oral candidiasis, xerostomia, vomiting, surgical removal of tooth.
Musculoskeletal
Leg cramps, myalgia, neck pain, pain in arm, shoulder pain, muscle injury of neck.
Neurological
Insomnia, sinus headache.
Non-Site Specific
Fatigue, fever, pain in body, discomfort in chest.
Respiratory
Acute bronchitis, dyspnea, influenza, lower respiratory tract infection, pneumonia, respiratory tract infection, shortness of breath, wheezing.
Urogenital
Urinary tract infection.
Electrocardiographic Monitoring in Patients With Chronic Obstructive Pulmonary Disease
Continuous electrocardiographic (Holter) monitoring was performed on 284 patients in 2 large COPD clinical trials during five 24-hour periods. No cases of sustained ventricular tachycardia were observed. At baseline, non-sustained, asymptomatic ventricular tachycardia was recorded for 7 (7.1%), 8 (9.4%), and 3 (3.0%) patients in the placebo, SEREVENT, and ipratropium groups, respectively. During treatment, nonsustained, asymptomatic ventricular tachycardia that represented a clinically significant change from baseline was reported for 11 (11.6%), 15 (18.3%), and 20 (20.8%) patients receiving placebo, SEREVENT, and ipratropium, respectively. Four of these cases of ventricular tachycardia were reported as adverse events (1 placebo, 3 SEREVENT) by 1 investigator based upon review of Holter data. One case of ventricular tachycardia was observed during ECG evaluation of chest pain (ipratropium) and reported as an adverse event.
Observed During Clinical Practice
In extensive US and worldwide postmarketing experience, serious exacerbations of asthma, including some that have been fatal, have been reported. In most cases, these have occurred in patients with severe asthma and/or in some patients in whom asthma has been acutely deteriorating (see WARNINGS no. 1), but they have occurred in a few patients with less severe asthma as well. It was not possible from these reports to determine whether SEREVENT Inhalation Aerosol contributed to these events or simply failed to relieve the deteriorating asthma.
The following events have also been identified during postapproval use of SEREVENT in clinical practice. Because they are reported voluntarily from a population of unknown size, estimates of frequency cannot be made. These events have been chosen for inclusion due to a combination of their seriousness, frequency of reporting, or potential causal connection to SEREVENT.
Respiratory
Rare reports of upper airway symptoms of laryngeal spasm, irritation, or swelling such as stridor or choking; oropharyngeal irritation.
Cardiovascular
Hypertension, arrhythmias (including atrial fibrillation, supraventricular tachycardia, extrasystoles).
OVERDOSAGE
The expected signs and symptoms with overdosage are those of excessive beta-adrenergic stimulation and/or occurrence or exaggeration of any of the symptoms listed under ADVERSE REACTIONS, e.g., seizures, angina, hypertension or hypotension, tachycardia with rates up to 200 beats/min, arrhythmias, nervousness, headache, tremor, muscle cramps, dry mouth, palpitation, nausea, dizziness, fatigue, malaise, and insomnia. Overdosage with SEREVENT Inhalation Aerosol may be expected to result in exaggeration of the pharmacologic adverse effects associated with beta-adrenoceptor agonists, including tachycardia and/or arrhythmia, tremor, headache, and muscle cramps. Overdosage with SEREVENT Inhalation Aerosol can lead to clinically significant prolongation of the QTc interval, which can produce ventricular arrhythmias. Other signs of overdosage may include hypokalemia and hyperglycemia.
As with all sympathomimetic aerosol medications, cardiac arrest and even death may be associated with abuse of SEREVENT Inhalation Aerosol.
Treatment consists of discontinuation of SEREVENT Inhalation Aerosol together with appropriate symptomatic therapy. The judicious use of a cardioselective beta-receptor blocker may be considered, bearing in mind that such medication can produce bronchospasm. There is insufficient evidence to determine if dialysis is beneficial for overdosage of SEREVENT Inhalation Aerosol. Cardiac monitoring is recommended in cases of overdosage.
No deaths were seen in rats at inhalation doses of 2.9 mg/kg (approximately 240 times the maximum recommended human daily inhalation dose on a mg/m2 basis) and in dogs at 0.7 mg/kg (approximately 190 times the maximum recommended human daily inhalation dose on a mg/m2 basis). By the oral route, no deaths occurred in mice at 150 mg/kg (approximately 6,100 times the maximum recommended human daily inhalation dose on a mg/m2 basis) and in rats at 1,000 mg/kg (approximately 81,000 times the maximum recommended human daily inhalation dose on a mg/m2 basis).
DOSAGE AND ADMINISTRATION
SEREVENT Inhalation Aerosol should be administered by the orally inhaled route only (see PATIENT’S INSTRUCTIONS FOR USE). It is recommended to “test spray” SEREVENT Inhalation Aerosol into the air 4 times before using for the first time and in cases where the aerosol has not been used for a prolonged period of time (i.e., more than 4 weeks).
Asthma
For maintenance of bronchodilatation and prevention of symptoms of asthma, including the symptoms of nocturnal asthma, the usual dosage for patients 12 years of age and older is 2 inhalations (42 mcg) twice daily (morning and evening, approximately 12 hours apart). Adverse effects are more likely to occur with higher doses of salmeterol, and more frequent administration or administration of a larger number of inhalations is not recommended.
To gain full therapeutic benefit, SEREVENT Inhalation Aerosol should be administered twice daily (morning and evening) in the treatment of reversible airway obstruction.
If a previously effective dosage regimen fails to provide the usual response, medical advice should be sought immediately as this is often a sign of destabilization of asthma. Under these circumstances, the therapeutic regimen should be re-evaluated and additional therapeutic options, such as inhaled or systemic corticosteroids, should be considered. If symptoms arise in the period between doses, an inhaled, short-acting beta2-agonist should be taken for immediate relief.
Chronic Obstructive Pulmonary Disease
For maintenance treatment of bronchospasm associated with COPD (including chronic bronchitis and emphysema), the usual dosage for adults is 2 inhalations (42 mcg) twice daily (morning and evening, approximately 12 hours apart).
Prevention of Exercise-Induced Bronchospasm
Two inhalations at least 30 to 60 minutes before exercise have been shown to protect against EIB in many patients for up to 12 hours. Additional doses of SEREVENT Inhalation Aerosol should not be used for 12 hours after the administration of this drug. Patients who are receiving SEREVENT Inhalation Aerosol twice daily (morning and evening) shouldnotuse additional SEREVENT Inhalation Aerosol for prevention of EIB. If this dose is not effective, other appropriate therapy for EIB should be considered.
Geriatric Use
In studies where geriatric patients (65 years of age or older, see PRECAUTIONS) have been treated with SEREVENT Inhalation Aerosol, efficacy and safety of 42 mcg given twice daily (morning and evening) did not differ from that in younger patients. Consequently, no dosage adjustment is recommended.
HOW SUPPLIED
SEREVENT Inhalation Aerosol is supplied in 13-g canisters containing 120 metered actuations in boxes of 1. Each actuation delivers 25 mcg of salmeterol base (as salmeterol xinafoate) from the valve and 21 mcg of salmeterol base (as salmeterol xinafoate) from the actuator. Each canister is supplied with a green plastic actuator with a teal strapcap and patient's instructions (NDC 0173-0464-00). Also available, SEREVENT Inhalation Aerosol Refill (NDC 0173-0465-00), a 13-g canister only with patient’s instructions.
SEREVENT Inhalation Aerosol is also supplied in institutional packs that consist of a 6.5-g canister containing 60 metered actuations in boxes of 1. Each actuation delivers 25 mcg of salmeterol base (as salmeterol xinafoate) from the valve and 21 mcg of salmeterol base from the actuator (as salmeterol xinafoate). Each canister is supplied with a green plastic actuator with a teal strapcap and patient's instructions (NDC 0173-0467-00).
For use with SEREVENT Inhalation Aerosol actuator only. The green actuator with SEREVENT Inhalation Aerosol should not be used with other aerosol medications, and actuators from other aerosol medications should not be used with a SEREVENT Inhalation Aerosol canister.
The correct amount of medication in each inhalation cannot be assured after 120 actuations from the 13-g canister or 60 actuations from the 6.5-g canister even though the canister is not completely empty. The canister should be discarded when the labeled number of actuations has been used.
Store between 15° and 30°C (59° and 86°F). Store canister with nozzle end down. Protect from freezing temperatures and direct sunlight.
Avoid spraying in eyes. Contents under pressure. Do not puncture or incinerate. Do not store at temperatures above 120°F. Keep out of reach of children. As with most inhaled medications in aerosol canisters, the therapeutic effect of this medication may decrease when the canister is cold; for best results, the canister should be at room temperature before use. Shake well before using.
Note: The indented statement below is required by the Federal government’s Clean Air Act for all products containing or manufactured with chlorofluorocarbons (CFCs).
WARNING: Contains trichlorofluoromethane and dichlorodifluoromethane, substances that harm public health and environment by destroying ozone in the upper atmosphere.
A notice similar to the above WARNING has been placed in the patient information leaflet of this product pursuant to EPA regulations. The patient’s warning states that the patient should consult his or her physician if there are questions about alternatives.
GlaxoSmithKline
Research Triangle Park, NC 27709
©2004, GlaxoSmithKline. All rights reserved.
| SEREVENT (salmeterol xinafoate) | ||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
Revised: 05/2006GlaxoSmithKline