HAVRIX
-
hepatitis a virus inactivated antigen, a injection, suspension
GlaxoSmithKline Biologicals SA
----------
|
|||||||||||||||||||||
FULL PRESCRIBING INFORMATION
1 INDICATIONS AND USAGE
HAVRIX is a vaccine indicated for active immunization against disease caused by hepatitis A virus (HAV) for persons ≥12 months of age. Primary immunization should be administered at least 2 weeks prior to expected exposure to HAV.
2 DOSAGE AND ADMINISTRATION
2.1 Preparation for Administration
Shake vial or syringe well before withdrawal and use. Inspect HAVRIX visually for particulate matter, discoloration, and cracks in the vial or syringe prior to administration, whenever solution and container permit. If any of these conditions exist, the vaccine should not be administered. With thorough agitation, HAVRIX is a homogeneous, turbid, white suspension. Discard if it appears otherwise.
2.2 Recommended Dose and Schedule
HAVRIX should be administered by intramuscular injection. Do not administer intravenously, intradermally, or subcutaneously. In adults, the injection should be given in the deltoid region. HAVRIX should not be administered in the gluteal region; such injections may result in suboptimal response.
Children and Adolescents: Primary immunization for children and adolescents (12 months through 18 years of age) consists of a single 0.5-mL dose and a 0.5-mL booster dose administered anytime between 6 and 12 months later in order to ensure the highest antibody titers.
Adults: Primary immunization for adults consists of a single 1-mL dose and a 1-mL booster dose administered anytime between 6 and 12 months later in order to ensure the highest antibody titers.
3 DOSAGE FORMS AND STRENGTHS
HAVRIX is a suspension available in single-dose vials and prefilled syringes for intramuscular injection.
Each 0.5-mL pediatric dose of vaccine consists of 720 EL.U. of viral antigen.
Each 1-mL adult dose of vaccine consists of 1440 EL.U. of viral antigen.
4 CONTRAINDICATIONS
Severe allergic reaction (e.g., anaphylaxis) after a previous dose of any hepatitis A-containing vaccine, or to any component of HAVRIX, including neomycin, is a contraindication to administration of HAVRIX [see Description (11)].
5 WARNINGS AND PRECAUTIONS
5.1 Latex
The tip cap and the rubber plunger of the needleless prefilled syringes contain dry natural latex rubber that may cause allergic reactions in latex sensitive individuals. The vial stopper is latex-free.
5.2 Altered Immunocompetence
Immunocompromised persons may have a diminished immune response to HAVRIX, including individuals receiving immunosuppressant therapy.
5.3 Limitations of Vaccine Effectiveness
Hepatitis A has a relatively long incubation period (15 to 50 days). Hepatitis A vaccine may not prevent hepatitis A infection in individuals who have an unrecognized hepatitis A infection at the time of vaccination. Additionally, it may not prevent infection in individuals who do not achieve protective antibody titers (although the lowest titer needed to confer protection has not been determined).
5.4 Preventing and Managing Allergic Vaccine Reactions
Appropriate medical treatment and supervision must be available to manage possible anaphylactic reactions following administration of the vaccine.
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a vaccine cannot be directly compared to rates in the clinical trials of another vaccine, and may not reflect the rates observed in practice. As with any vaccine, there is the possibility that broad use of HAVRIX could reveal adverse reactions not observed in clinical trials.
The safety of HAVRIX has been evaluated in clinical trials involving approximately 32,500 individuals receiving doses ranging from 360 EL.U. to 1440 EL.U.
The frequency of solicited adverse events tended to decrease with successive doses of HAVRIX.
Of solicited adverse events in clinical trials, the most frequently reported by volunteers was injection-site soreness (56% of adults and 21% of children); however, less than 0.5% of soreness was reported as severe. Headache was reported by 14% of adults and less than 9% of children. Other solicited and unsolicited events occurring during clinical trials are listed below.
Incidence 1% to 10% of Injections: Metabolism and Nutrition Disorders: Anorexia.
Gastrointestinal Disorders: Nausea.
General Disorders and Administration Site Conditions: Fatigue, fever (>37.5°C), injection site induration, injection site redness, injection site swelling, malaise.
Incidence <1% of Injections: Infections and Infestations: Pharyngitis, upper respiratory tract infections.
Blood and Lymphatic System Disorders: Lymphadenopathy.
Psychiatric Disorders: Insomnia.
Nervous System Disorders: Dysgeusia, hypertonia.
Eye Disorders: Photophobia.
Ear and Labyrinth Disorders: Vertigo.
Gastrointestinal Disorders: Abdominal pain, diarrhea, vomiting.
Skin and Subcutaneous Tissue Disorders: Pruritus, rash, urticaria.
Musculoskeletal and Connective Tissue Disorders: Arthralgia, myalgia.
General Disorders and Administration Site Conditions: Injection site hematoma.
Investigations: Creatine phosphokinase increased.
Outbreak Setting and a Field Efficacy Trial: Safety data were obtained from 2 additional sources in which large populations were vaccinated. In an outbreak setting in which 4,930 individuals were immunized with a single dose of either 720 EL.U. or 1440 EL.U. of HAVRIX, no serious adverse events due to vaccination were reported. Overall, less than 10% of vaccinees reported solicited general adverse events following the vaccine. The most common solicited local adverse reaction was pain at the injection site, reported in 22.3% of subjects at 24 hours and decreasing to 2.4% by 72 hours.
In a field efficacy trial, 19,037 children received the 360 EL.U. dose of HAVRIX. The most commonly reported adverse events following administration of HAVRIX were injection-site pain (9.5%) and tenderness (8.1%), which were reported following first doses of HAVRIX. Other adverse events were infrequent and comparable to the control vaccine ENGERIX-B® [Hepatitis B Vaccine (Recombinant)]. Additionally, no serious adverse events due to the vaccine were reported. The large trial further allowed for analysis of rare adverse events, including hospitalization and death. No significant differences were found between the cohorts.
HAVRIX 720 EL.U./0.5 mL at 11 Months of Age and Older: In a multicenter study, parents/guardians recorded local and general symptoms on diary cards for 4 days (Days 0 to 3) after vaccination [see Clinical Studies (14.2)]. In the 3 groups of children who received HAVRIX alone, safety data were available for 723 children who received 1,396 documented doses of HAVRIX. Additional safety data were available for 181 children who received HAVRIX coadministered with INFANRIX® (Diphtheria and Tetanus Toxoids and Acellular Pertussis Vaccine Adsorbed) (DTaP) and Haemophilus influenzae type b (Hib) conjugate vaccine (tetanus toxoid conjugate) (PRP-T) (Sanofi Pasteur SA).
The frequencies of solicited local and general events following receipt of HAVRIX were monitored during the 4-day observation period. The following ranges of solicited adverse event rates were observed among 3 groups of children that received their first dose of HAVRIX alone at between 11 and 25 months of age: Injection site pain in 15 to 21% of subjects, redness in 16 to 21% of subjects, swelling in 8% of subjects, irritability in 24 to 36% of subjects, loss of appetite in 16 to 19% of subjects, drowsiness in 15 to 17% of subjects and fever >39.5°C in ≤2% of subjects. Following the booster dose of HAVRIX, among local reactions: Pain was reported in 16 to 21% of subjects, redness in 17 to 22%, swelling in 8 to 10% of subjects. Following the booster dose of HAVRIX, among general events, irritability was reported in 19 to 29% of subjects, loss of appetite in 14 to 18% of subjects, drowsiness in 13 to 16% of subjects and fever >39.5°C in ≤1% of subjects.
Drowsiness and loss of appetite occurred at statistically significantly higher rates in subjects 15 to 18 months of age who received Hib conjugate vaccine (PRP-T) (Sanofi Pasteur SA) and INFANRIX concomitantly with HAVRIX as compared to subjects 15 to 18 months of age who received Hib conjugate vaccine (PRP-T) and INFANRIX (drowsiness 34% and 22% and loss of appetite 29% and 19%, respectively). With the exception of fever (>39.5°C), the solicited general symptoms occurred at statistically significantly higher rates in subjects 15 to 18 months of age who received Hib conjugate vaccine (PRP-T) and INFANRIX concomitantly with HAVRIX as compared to subjects 15 to 18 months of age who received HAVRIX alone (irritability 46% and 30%, drowsiness 34% and 17%, and loss of appetite 29% and 17%, respectively).
A febrile seizure was reported in an 18-month-old subject 2 days after receiving the first dose of HAVRIX. Other serious adverse events reported during the course of this study included a single case each of hepatitis ~5 months post dose 1, insulin-dependent diabetes ~4 months post dose 1, and Kawasaki’s disease ~3½ months post dose 1. The association of these events with vaccination is unknown.
In a US multicenter study, children 15 months of age (range 14 to 16 months) received either HAVRIX coadministered with a US-licensed pneumococcal 7-valent conjugate vaccine (Wyeth Pharmaceuticals Inc.) followed by a second dose of HAVRIX 6 to 9 months later; HAVRIX administered alone followed by a second dose of HAVRIX 6 to 9 months later; or pneumococcal 7-valent conjugate vaccine administered alone followed by a first dose of HAVRIX one month later and a second dose of HAVRIX 6 to 9 months after the first [see Clinical Studies (14.5)]. Parents/guardians recorded local and general symptoms on diary cards for 4 days (Days 0 to 3) after vaccination.
Solicited local adverse events were reported as follows among children who received the first dose HAVRIX coadministered with pneumococcal 7-valent conjugate vaccine: Pain was reported in 36% of subjects, redness in 41% of subjects, and swelling in 29% of subjects. The reported rates of these local adverse events were similar to those reported in children who received the first dose of pneumococcal 7-valent conjugate vaccine alone (44%, 46%, and 27%, respectively). Among children who received the first dose of HAVRIX alone, pain was reported in 28% of subjects, redness in 22% of subjects, and swelling in 7% of subjects.
Solicited general adverse events were reported as follows among children who received the first dose HAVRIX coadministered with pneumococcal 7-valent conjugate vaccine: Irritability was reported in 35% of subjects, drowsiness in 26% of subjects, loss of appetite in 25% of subjects, and fever in 14% of subjects. The reported rates of these general adverse events were similar to those reported in children who received the first dose of pneumococcal 7-valent conjugate vaccine alone (41%, 32%, 25%, and 16%, respectively). Among children who received the first dose of HAVRIX alone, irritability was reported in 35% of subjects, drowsiness in 29% of subjects, loss of appetite in 26% of subjects, and fever in 9% of subjects.
6.2 Postmarketing Experience
In addition to reports in clinical trials, worldwide voluntary reports of adverse events received for HAVRIX since market introduction of this vaccine are listed below. This list includes serious adverse events or events which have a suspected causal connection to components of HAVRIX or other vaccines or drugs. Because these events are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to the vaccine.
Infections and Infestations: Rhinitis.
Blood and Lymphatic System Disorders: Thrombocytopenia.
Immune System Disorders: Anaphylactic reaction, anaphylactoid reaction, serum sickness–like syndrome.
Nervous System Disorders: Convulsion, dizziness, encephalopathy, Guillain-Barré syndrome, hypoesthesia, multiple sclerosis, myelitis, neuropathy, paresthesia, somnolence, syncope.
Vascular Disorders: Vasculitis.
Respiratory, Thoracic, and Mediastinal Disorders: Dyspnea.
Hepatobiliary Disorders: Hepatitis, jaundice.
Skin and Subcutaneous Tissue Disorders: Angioedema, erythema multiforme, hyperhidrosis.
Congenital, Familial, and Genetic Disorders: Congenital anomaly.
Musculoskeletal and Connective Tissue Disorders: Musculoskeletal stiffness.
General Disorders and Administration Site Conditions: Chills, influenza-like symptoms, injection site reaction, local swelling.
7 DRUG INTERACTIONS
7.1 Concomitant Administration With Vaccines and Immune Globulin (IG)
HAVRIX may be given concurrently with Haemophilus influenzae type b (Hib) conjugate vaccine (tetanus toxoid conjugate) (PRP-T) (Sanofi Pasteur SA) in children 15 to 18 months of age [see Adverse Reactions (6.1) and Clinical Studies (14.5)].
HAVRIX may be given concurrently with the fourth dose of pneumococcal 7-valent conjugate vaccine (Wyeth Pharmaceuticals Inc.) in children 15 months of age (range 14 to 16 months) [see Adverse Reactions (6.1) and Clinical Studies (14.5)].
The safety of HAVRIX given concomitantly with INFANRIX has been evaluated [see Adverse Reactions (6.1)]. Insufficient data are available to assess the immune response of a fourth dose of DTaP vaccine when administered with HAVRIX.
HAVRIX may be administered concomitantly with IG.
When concomitant administration of other vaccines or IG is required, they should be given with different syringes and at different injection sites. Do not mix HAVRIX with any other vaccine or product in the same syringe or vial.
7.2 Immunosuppressive Therapies
Immunosuppressive therapies, including irradiation, antimetabolites, alkylating agents, cytotoxic drugs, and corticosteroids (used in greater than physiologic doses), may reduce the immune response to HAVRIX.
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category C
Animal reproduction studies have not been conducted with HAVRIX. It is also not known whether HAVRIX can cause fetal harm when administered to a pregnant woman or can affect reproduction capacity. HAVRIX should be given to a pregnant woman only if clearly needed.
8.3 Nursing Mothers
It is not known whether HAVRIX is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when HAVRIX is administered to a nursing woman.
8.4 Pediatric Use
The safety and effectiveness of HAVRIX have been evaluated in 20,869 subjects 1 year to 18 years of age.
The safety and effectiveness of HAVRIX have not been established in subjects younger than 12 months of age.
8.5 Geriatric Use
Clinical studies of HAVRIX did not include sufficient numbers of subjects 65 years of age and older to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in overall safety between these subjects and younger adult subjects.
8.6 Hepatic Impairment
Subjects with chronic liver disease had a lower antibody response to HAVRIX than healthy subjects [see Clinical Studies (14.3)].
11 DESCRIPTION
HAVRIX (Hepatitis A Vaccine) is a sterile suspension of inactivated virus for intramuscular administration. The virus (strain HM175) is propagated in MRC-5 human diploid cells. After removal of the cell culture medium, the cells are lysed to form a suspension. This suspension is purified through ultrafiltration and gel permeation chromatography procedures. Treatment of this lysate with formalin ensures viral inactivation. Viral antigen activity is referenced to a standard using an enzyme linked immunosorbent assay (ELISA), and is therefore expressed in terms of ELISA Units (EL.U.).
Each 1-mL adult dose of vaccine consists of 1440 EL.U. of viral antigen, adsorbed on 0.5 mg of aluminum as aluminum hydroxide.
Each 0.5-mL pediatric dose of vaccine consists of 720 EL.U. of viral antigen, adsorbed onto 0.25 mg of aluminum as aluminum hydroxide.
HAVRIX contains the following excipients: Amino acid supplement (0.3% w/v) in a phosphate-buffered saline solution and polysorbate 20 (0.05 mg/mL). From the manufacturing process, HAVRIX also contains residual MRC-5 cellular proteins (not more than 5 mcg/mL), formalin (not more than 0.1 mg/mL), and neomycin sulfate (not more than 40 ng/mL), an aminoglycoside antibiotic included in the cell growth media.
HAVRIX is formulated without preservatives.
The tip cap and the rubber plunger of the needleless prefilled syringes contain dry natural latex rubber. The vial stopper is latex-free.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
The hepatitis A virus belongs to the picornavirus family. It is one of several hepatitis viruses that cause systemic disease with pathology in the liver.
The incubation period for hepatitis A averages 28 days (range: 15 to 50 days).1 The course of hepatitis A infection is extremely variable, ranging from asymptomatic infection to icteric hepatitis and death.
The presence of antibodies to HAV confers protection against hepatitis A infection. However, the lowest titer needed to confer protection has not been determined.
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
HAVRIX has not been evaluated for its carcinogenic potential, mutagenic potential, or potential for impairment of fertility.
14 CLINICAL STUDIES
14.1 Pediatric Effectiveness Studies
Protective efficacy with HAVRIX has been demonstrated in a double-blind, randomized controlled study in school children (age 1 to 16 years) in Thailand who were at high risk of HAV infection. A total of 40,119 children were randomized to be vaccinated with either HAVRIX 360 EL.U. or ENGERIX-B at 0, 1, and 12 months. 19,037 children received a primary course (doses at 0 and 1 months) of HAVRIX and 19,120 children received a primary course (doses at 0 and 1 months) of ENGERIX-B. 38,157 children entered surveillance at day 138 and were observed for an additional 8 months. Using the protocol-defined endpoint (≥2 days absence from school, ALT level >45 U/mL, and a positive result in the HAVAB-M test), 32 cases of clinical hepatitis A occurred in the control group. In the HAVRIX group, 2 cases were identified. These 2 cases were mild in terms of both biochemical and clinical indices of hepatitis A disease. Thus the calculated efficacy rate for prevention of clinical hepatitis A was 94% (95% Confidence Interval [CI]: 74, 98).
In outbreak investigations occurring in the trial, 26 clinical cases of hepatitis A (of a total of 34 occurring in the trial) occurred. No cases occurred in vaccinees who received HAVRIX.
Using additional virological and serological analyses post hoc, the efficacy of HAVRIX was confirmed. Up to 3 additional cases of mild clinical illness may have occurred in vaccinees. Using available testing, these illnesses could neither be proven nor disproven to have been caused by HAV. By including these as cases, the calculated efficacy rate for prevention of clinical hepatitis A would be 84% (95% CI: 60, 94).
In a study designed to interrupt an epidemic of hepatitis A among Native Americans in Alaska, vaccination with a single dose of HAVRIX (1440 EL.U./mL in adults, 720 EL.U./0.5 mL in children and adolescents) appeared to be efficacious.
14.2 Immunogenicity in Children and Adolescents
Immune Response to HAVRIX 720 EL.U./0.5 mL at 11 Months of Age and Older: In a prospective, open-label, multicenter study, 1,085 children were enrolled into one of 5 groups:
(1) Children 11 to 13 months of age who received HAVRIX on a 0- and 6-month schedule;
(2) Children 15 to 18 months of age who received HAVRIX on a 0- and 6-month schedule;
(3) Children 15 to 18 months of age who received HAVRIX coadministered with INFANRIX and Hib conjugate vaccine (PRP-T) (Sanofi Pasteur SA) at month 0 and HAVRIX at month 6;
(4) Children 15 to 18 months of age who received INFANRIX coadministered with Hib conjugate vaccine (PRP-T) (Sanofi Pasteur SA) at month 0 and HAVRIX at months 1 and 7;
(5) Children 23 to 25 months of age who received HAVRIX on a 0- and 6-month schedule.
Among subjects in all groups, 52% were male; 61% of subjects were White, 9% Black, 3% Asian, and 27% were of other racial groups. The anti-hepatitis A antibody vaccine responses and GMTs, calculated on responders for groups 1, 2, and 5 are presented in Table 1. Vaccine response rates were similar among the 3 age groups that received HAVRIX. One month after the second dose of HAVRIX, the GMT in each of the younger age groups (11 to 13 and 15 to 18 months of age) was shown to be similar to that achieved in the 23 to 25 months of age group.
| Age group | N | Vaccine Response |
GMT (mIU/mL) |
|
| % | 95% CI | |||
| 11-13 months (Group 1) | 218 | 99 | 97, 100 | 1,461a |
| 15-18 months (Group 2) | 200 | 100 | 98, 100 | 1,635a |
| 23-25 months (Group 5) | 211 | 100 | 98, 100 | 1,911 |
Vaccine response = Seroconversion (anti-HAV ≥15 mIU/mL [lower limit of antibody measurement by assay]) in children initially seronegative or at least the maintenance of the pre-vaccination anti-HAV concentration in initially seropositive children.
CI = Confidence Interval; GMT = Geometric mean antibody titer.
aCalculated on vaccine responders one month post-dose 2. GMTs in children 11 to 13 months of age and 15 to 18 months of age were non-inferior (similar) to the GMT in children 23 to 25 months of age (i.e., the lower limit of the two-sided 95% CI on the GMT ratio for Group 1/Group 5 and for Group 2/Group 5 were both ≥0.5).
Immune Response to HAVRIX 360 EL.U. at 2 Years of Age and Older: In 6 clinical studies of subjects 2 to 18 years of age (n = 762) who received 2 doses of HAVRIX (360 EL.U.) given 1 month apart, the GMT ranged from 197 to 660 mIU/mL. Ninety-nine percent of subjects seroconverted following 2 doses. When a booster (third) dose of HAVRIX 360 EL.U. was administered 6 months following the initial dose, all subjects were seropositive 1 month following the booster dose, with GMTs rising to a range of 3,388 to 4,643 mIU/mL. In 1 study in which children were followed for an additional 6 months, all subjects remained seropositive.
Immune Response to HAVRIX 720 EL.U./0.5 mL at 2 Years of Age and Older: In 4 clinical studies, children and adolescents (n = 314), ranging from 2 to 19 years of age, were immunized with 2 doses of HAVRIX 720 EL.U./0.5 mL given 6 months apart. One month after the first dose, seroconversion (anti-HAV ≥20 mIU/mL [lower limit of antibody measurement by assay]) ranged from 96.8% to 100%, with GMTs of 194 mIU/mL to 305 mIU/mL. In studies in which sera were obtained 2 weeks following the initial dose, seroconversion ranged from 91.6% to 96.1%. One month following a booster dose at month 6, all subjects were seropositive, with GMTs ranging from 2,495 mIU/mL to 3,644 mIU/mL.
In an additional study in which the booster dose was delayed until 1 year following the initial dose, 95.2% of the subjects were seropositive just prior to administration of the booster dose. One month later, all subjects were seropositive, with a GMT of 2,657 mIU/mL.
Also, HAVRIX has been found to be efficacious in a clinical study of children at high risk of HAV infection [see Clinical Studies (14.1)].
14.3 Immunogenicity in Adults
Over 400 healthy adults 18 to 50 years of age in 3 clinical studies were given a single 1440 EL.U. dose of HAVRIX. All subjects were seronegative for hepatitis A antibodies at baseline. Specific humoral antibodies against HAV were elicited in more than 96% of subjects when measured 1 month after vaccination. By day 15, 80% to 98% of vaccinees had already seroconverted (anti-HAV ≥20 mIU/mL [lower limit of antibody measurement by assay]). GMTs of seroconverters ranged from 264 to 339 mIU/mL at day 15 and increased to a range of 335 to 637 mIU/mL by 1 month following vaccination.
The GMTs obtained following a single dose of HAVRIX are at least several times higher than that expected following receipt of IG.
In a clinical study using 2.5 to 5 times the standard dose of IG (standard dose = 0.02 to 0.06 mL/kg), the GMT in recipients was 146 mIU/mL at 5 days post-administration, 77 mIU/mL at month 1, and 63 mIU/mL at month 2.
In 2 clinical trials in which a booster dose of 1440 EL.U. was given 6 months following the initial dose, 100% of vaccinees (n = 269) were seropositive 1 month after the booster dose, with GMTs ranging from 3,318 mIU/mL to 5,925 mIU/mL. The titers obtained from this additional dose approximate those observed several years after natural infection.
In a subset of vaccinees (n = 89), a single dose of HAVRIX 1440 EL.U. elicited specific anti-HAV neutralizing antibodies in more than 94% of vaccinees when measured 1 month after vaccination. These neutralizing antibodies persisted until month 6. One hundred percent of vaccinees had neutralizing antibodies when measured 1 month after a booster dose given at month 6.
Immunogenicity of HAVRIX was studied in subjects with chronic liver disease of various etiologies. 189 healthy adults and 220 adults with either chronic hepatitis B (n = 46), chronic hepatitis C (n = 104), or moderate chronic liver disease of other etiology (n = 70) were vaccinated with HAVRIX 1440 EL.U. on a 0- and 6-month schedule. The last group consisted of alcoholic cirrhosis (n = 17), autoimmune hepatitis (n = 10), chronic hepatitis/cryptogenic cirrhosis (n = 9), hemochromatosis (n = 2), primary biliary cirrhosis (n = 15), primary sclerosing cholangitis (n = 4), and unspecified (n = 13). At each time point, geometric mean antibody titers (GMTs) were lower for subjects with chronic liver disease than for healthy subjects. At month 7, the GMTs ranged from 478 mIU/mL (chronic hepatitis C) to 1,245 mIU/mL (healthy). One month after the first dose, seroconversion rates in adults with chronic liver disease were lower than in healthy adults. However, 1 month after the booster dose at month 6, seroconversion rates were similar in all groups; rates ranged from 94.7% to 98.1%. The relevance of these data to the duration of protection afforded by HAVRIX is unknown.
In subjects with chronic liver disease, local injection site reactions with HAVRIX were similar among all 4 groups, and no serious adverse events attributed to the vaccine were reported in subjects with chronic liver disease.
14.4 Duration of Immunity
The duration of immunity following a complete schedule of immunization with HAVRIX has not been established.
14.5 Immune Response to Concomitantly Administered Vaccines
Concomitant Administration With Hib Conjugate Vaccine (PRP-T): The concomitant administration of Hib conjugate vaccine (PRP-T) (Sanofi Pasteur SA) and INFANRIX with HAVRIX was evaluated in children receiving their first dose of HAVRIX at 15 to 18 months of age followed by a second dose of HAVRIX 6 months later. Anti-hepatitis A vaccine response was defined as seroconversion (anti-HAV ≥15 mIU/mL [lower limit of antibody measurement by assay]) in subjects initially seronegative or at least maintenance of pre-vaccination antibody concentration in subjects initially seropositive. One month after the second dose of HAVRIX, the vaccine response (100%) in those receiving the first dose of HAVRIX coadministered with INFANRIX and Hib conjugate vaccine (PRP-T) (Sanofi Pasteur SA) was shown to be non-inferior to that achieved (100%) in 15- to 18-month-olds who received HAVRIX alone (lower limit of 95% CI on difference for coadministered vaccine group minus HAVRIX alone group >-5%).
One month after vaccination with Hib conjugate vaccine (PRP-T) (Sanofi Pasteur SA), the seroprotection rates to this vaccine were shown to be non-inferior in subjects who received Hib conjugate vaccine (PRP-T) concomitantly with their first dose of HAVRIX (100% achieved ≥1 mcg/mL of anti-PRP antibody; 95% CI: 97, 100) as compared to those who did not receive HAVRIX (100% achieved ≥1 mcg/mL of anti-PRP antibody; 95% CI: 97, 100). Both groups received INFANRIX concomitantly with Hib conjugate vaccine (PRP-T) with and without HAVRIX.
Concomitant Administration With Pneumococcal 7-Valent Conjugate Vaccine: In a US multicenter study, children 15 months of age (range 14 to 16 months) received one of 3 regimens: (Group 1) HAVRIX coadministered with pneumococcal 7-valent conjugate vaccine (Wyeth Pharmaceuticals Inc.) followed by a second dose of HAVRIX 6 to 9 months later; (Group 2) HAVRIX administered alone followed by a second dose of HAVRIX 6 to 9 months later; or (Group 3) pneumococcal 7-valent conjugate vaccine administered alone followed by a first dose of HAVRIX one month later and a second dose of HAVRIX 6 to 9 months after the first.
One month after the second dose, the anti-hepatitis A GMT of HAVRIX coadministered with pneumococcal 7-valent conjugate vaccine was non-inferior to HAVRIX given alone (Group 1 GMT = 1,518 mIU/mL; Group 2 GMT = 1,666 mIU/mL). The difference in anti-hepatitis A seropositivity rates between groups (HAVRIX coadministered with pneumococcal 7-valent conjugate vaccine minus HAVRIX alone) was marginally lower than the pre-defined non-inferiority limit of -5% (lower limit of the two-sided 95% CI -5.78%). However, in all 3 groups, the seropositivity rate ranged between 98% and 100% one month after the second dose of HAVRIX (Group 1, 93/94; Group 2, 106/106; Group 3, 113/115).
One month after vaccination, non-inferiority was demonstrated with respect to GMTs for anti-pneumococcal antibodies to all 7 serotypes after the coadministration of pneumococcal 7-valent conjugate vaccine with HAVRIX compared to pneumococcal 7-valent conjugate vaccine alone. At least 98% of subjects who received pneumococcal 7-valent conjugate vaccine coadministered with HAVRIX and those who received pneumococcal 7-valent conjugate vaccine alone were seropositive for all 7 pneumococcal serotypes.
There are limited data on the coadministration of HAVRIX with other vaccines.
15 REFERENCES
- Centers for Disease Control and Prevention. Prevention of hepatitis A through active or passive immunization: Recommendations of the Immunization Practices Advisory Committee (ACIP). MMWR 2006;55(RR-7):1-23.
- Centers for Disease Control and Prevention. Update: Prevention of hepatitis A after exposure to hepatitis A virus and in international travelers. Updated Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR 2007;56(41):1080-1084.
16 HOW SUPPLIED/STORAGE AND HANDLING
HAVRIX is available in single-dose vials and prefilled TIP-LOK® syringes.
720 EL.U./0.5 mL in Single-Dose Vials and Prefilled Syringes (Preservative Free Formulation)
NDC 58160-825-11 Package of 10 Single-Dose Vials
NDC 58160-825-46 Package of 5 Prefilled Disposable TIP-LOK Syringes (packaged without needles)
NDC 58160-825-51 Package of 10 Prefilled Disposable TIP-LOK Syringes (packaged without needles)
1440 EL.U./mL in Single-Dose Vials and Prefilled Syringes (Preservative Free Formulation)
NDC 58160-826-11 Package of 10 Single-Dose Vials
NDC 58160-826-46 Package of 5 Prefilled Disposable TIP-LOK Syringes (packaged without needles)
Store refrigerated between 2° and 8°C (36° and 46°F). Do not freeze. Discard if the vaccine has been frozen. Do not dilute to administer.
17 PATIENT COUNSELING INFORMATION
Vaccine recipients and parents or guardians should be:
- informed of the potential benefits and risks of immunization with HAVRIX.
- educated regarding potential side effects, emphasizing that HAVRIX contains non-infectious killed viruses and cannot cause hepatitis A infection.
- instructed to report any adverse events to their healthcare provider where the vaccine was administered.
- given the Vaccine Information Statements, which are required by the National Childhood Vaccine Injury Act of 1986 to be given prior to immunization. These materials are available free of charge at the Centers for Disease Control and Prevention (CDC) website (www.cdc.gov/vaccines).
HAVRIX, ENGERIX-B, INFANRIX, and TIP-LOK are registered trademarks of GlaxoSmithKline.
Manufactured by GlaxoSmithKline Biologicals
Rixensart, Belgium, US License No. 1617
Distributed by GlaxoSmithKline
Research Triangle Park, NC 27709
©2009, GlaxoSmithKline. All rights reserved.
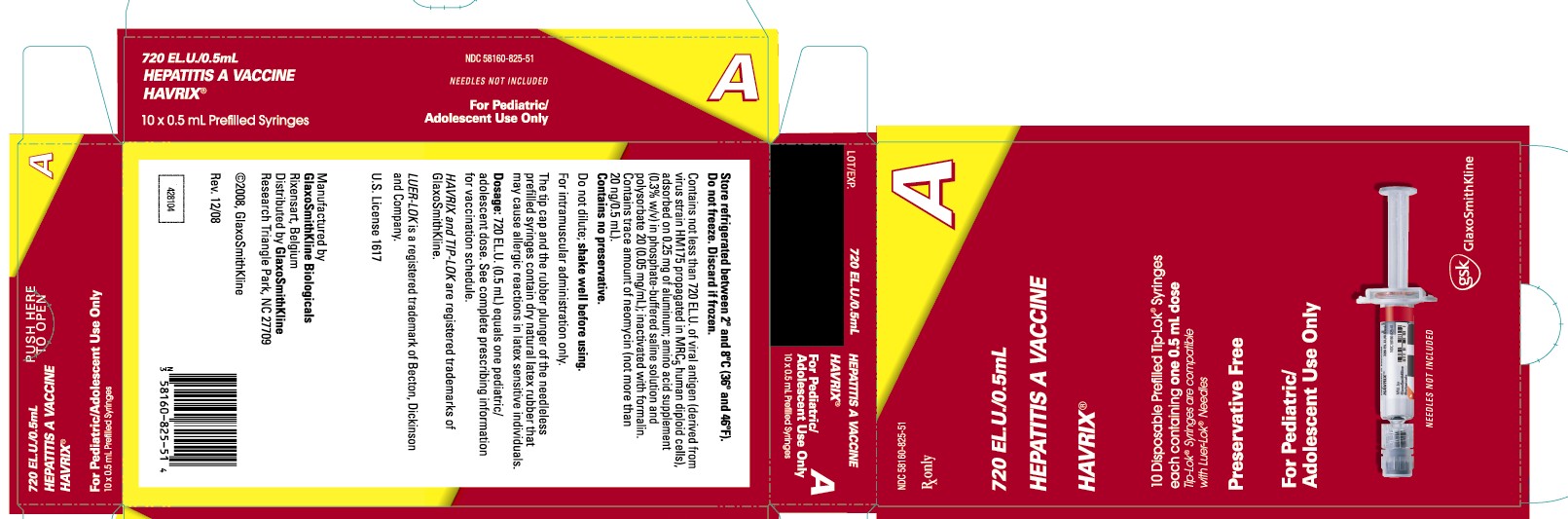
Principal Display Panel
NDC 58160-825-51
HAVRIX®
HEPATITIS A VACCINE
720 EL.U./0.5mL
10 x 0.5 mL Prefilled Syringes
NEEDLES NOT INCLUDED
For Pediatric/ Adolescent Use Only
Rx only
10 Disposable Prefilled Tip-Lok® Syringes each containing one 0.5 mL dose
Tip-Lok® Syringes are compatible with Luer-Lok® Needles
Preservative Free
Store refrigerated between 2o and 8oC (36o and 46oF).
Do not freeze. Discard if frozen.
Contains not less than 720 EL.U. of viral antigen (derived from virus strain HM175 propagated in MRC5 human diploid cells), adsorbed on 0.25 mg of aluminum; amino acid supplement (0.3% w/v) in phosphate-buffered saline solution and polysorbate 20 (0.05 mg/mL); inactivated with formalin. Contains trace amount of neomycin (not more than 20 ng/0.5mL).
Contains no preservatives.
Do not dilute; shake well before using.
For intramuscular administration only.
The tip cap and the rubber plunger of the needleless prefilled syringes contain dry natural latex rubber that may cause allergic reactions in latex sensitive individuals.
Dosage: 720 EL.U. (0.5mL) equals one pediatric/ adolescent dose. See complete prescribing information for vaccination schedule.
HAVRIX and TIP-LOK are registered trademarks of GlaxoSmithKline.
LUER-LOK is a registered trademark of Becton, Dickinson and Company.
U.S. License 1617
Manufactured by
GlaxoSmithKline Biologicals
Rixensart, Belgium
Distributed by GlaxoSmithKline
Research Triangle Park, 27709
©2008, GlaxoSmithKline
Rev. 12/08
428104
| HAVRIX
hepatitis a vaccine injection, suspension |
|||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||
| Marketing Information | |||
| Marketing Category | Application Number or Monograph Citation | Marketing Start Date | Marketing End Date |
| BLA | BLA103475 | 02/16/2007 | |
| HAVRIX
hepatitis a vaccine injection, suspension |
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
| Marketing Information | |||
| Marketing Category | Application Number or Monograph Citation | Marketing Start Date | Marketing End Date |
| BLA | BLA103475 | 04/13/2007 | |
| Labeler - GlaxoSmithKline Biologicals SA (372748392) |