DYMISTA- azelastine hydrochloride and fluticasone propionate spray, metered
Meda Pharmaceuticals Inc.
----------
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use DYMISTA™ Nasal Spray safely and effectively. See full prescribing information for DYMISTA Nasal Spray.
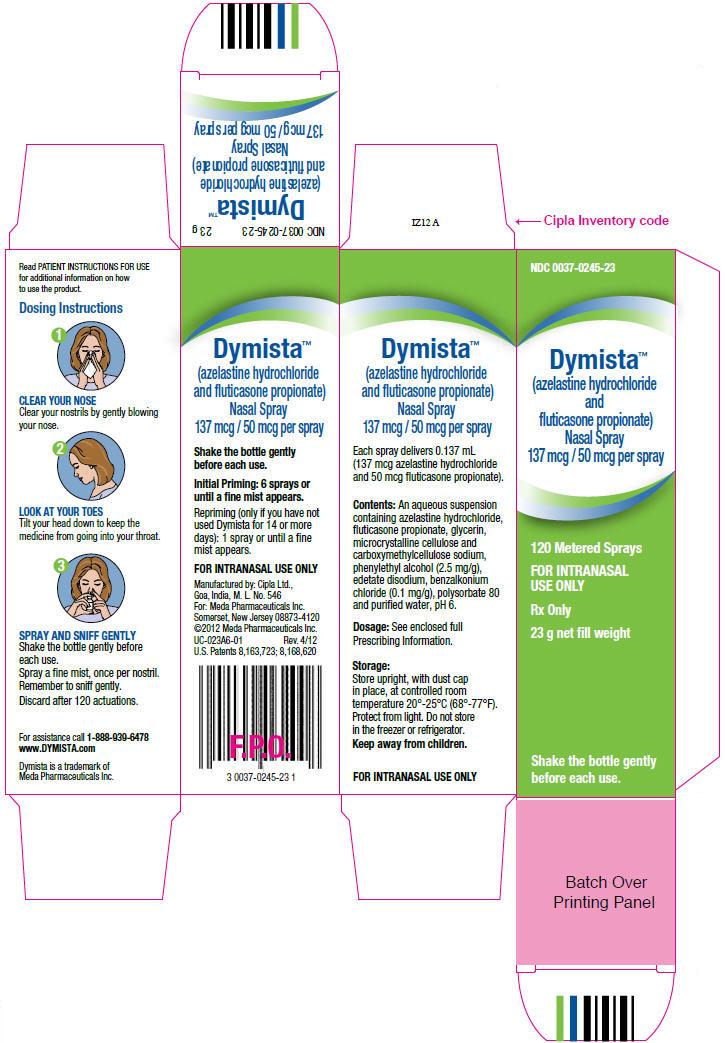
DYMISTA (azelastine hydrochloride and fluticasone propionate) Nasal Spray Initial U.S. Approval: 2012 INDICATIONS AND USAGEDymista Nasal Spray, containing an H1-receptor antagonist and a corticosteroid, is indicated for the relief of symptoms of seasonal allergic rhinitis in patients 12 years of age and older who require treatment with both azelastine hydrochloride and fluticasone propionate for symptomatic relief. (1) DOSAGE AND ADMINISTRATIONDOSAGE FORMS AND STRENGTHSDymista Nasal Spray: 137 mcg of azelastine hydrochloride and 50 mcg of fluticasone propionate (137 mcg/50 mcg) in each 0.137 mL spray. (3) CONTRAINDICATIONSNone. (4) WARNINGS AND PRECAUTIONS
ADVERSE REACTIONSThe most common adverse reactions (≥2% incidence) are: dysgeusia, epistaxis, and headache. (6.1) DRUG INTERACTIONSUSE IN SPECIFIC POPULATIONS
See 17 for PATIENT COUNSELING INFORMATION. Revised: 11/2012 |
FULL PRESCRIBING INFORMATION
1 INDICATIONS AND USAGE
Dymista Nasal Spray is indicated for the relief of symptoms of seasonal allergic rhinitis in patients 12 years of age and older who require treatment with both azelastine hydrochloride and fluticasone propionate for symptomatic relief.
2 DOSAGE AND ADMINISTRATION
2.1 Dosing Information
The recommended dose of Dymista Nasal Spray, 137 mcg/50 mcg, is 1 spray per nostril twice daily for seasonal allergic rhinitis. Each spray contains 137 mcg of azelastine hydrochloride and 50 mcg of fluticasone propionate (137 mcg/50 mcg).
Administer Dymista Nasal Spray by the intranasal route only.
2.2 Important Administration Instructions
Shake the bottle gently before each use.
Priming: Prime Dymista Nasal Spray before initial use by releasing 6 sprays or until a fine mist appears. When Dymista Nasal Spray has not been used for 14 or more days, reprime with 1 spray or until a fine mist appears. Avoid spraying Dymista Nasal Spray into the eyes. If sprayed in the eyes, flush eyes with water for at least 10 minutes.
3 DOSAGE FORMS AND STRENGTHS
Dymista is a nasal spray suspension. Each spray delivers a volume of 0.137 mL suspension containing 137 mcg of azelastine hydrochloride and 50 mcg of fluticasone propionate (137 mcg/50 mcg).
5 WARNINGS AND PRECAUTIONS
5.1 Somnolence
In clinical trials, the occurrence of somnolence has been reported in some patients (6 of 853 patients) taking Dymista Nasal Spray [see Adverse Reactions (6.1)]. Patients should be cautioned against engaging in hazardous occupations requiring complete mental alertness and motor coordination such as operating machinery or driving a motor vehicle after administration of Dymista Nasal Spray. Concurrent use of Dymista Nasal Spray with alcohol or other central nervous system depressants should be avoided because additional reductions in alertness and additional impairment of central nervous system performance may occur [see Drug Interactions (7.1)].
5.2 Local Nasal Effects
In clinical trials of 2 to 52 weeks' duration, epistaxis was observed more frequently in patients treated with Dymista Nasal Spray than those who received placebo [see Adverse Reactions (6)].
Instances of nasal ulceration and nasal septal perforation have been reported in patients following the intranasal application of corticosteroids. There were no instances of nasal ulceration or nasal septal perforation observed in clinical trials with Dymista Nasal Spray.
Because of the inhibitory effect of corticosteroids on wound healing, patients who have experienced recent nasal ulcers, nasal surgery, or nasal trauma should not use Dymista Nasal Spray until healing has occurred.
In clinical trials with fluticasone propionate administered intranasally, the development of localized infections of the nose and pharynx with Candida albicans has occurred. When such an infection develops, it may require treatment with appropriate local therapy and discontinuation of treatment with Dymista Nasal Spray. Patients using Dymista Nasal Spray over several months or longer should be examined periodically for evidence of Candida infection or other signs of adverse effects on the nasal mucosa.
5.3 Glaucoma and Cataracts
Nasal and inhaled corticosteroids may result in the development of glaucoma and/or cataracts. Therefore, close monitoring is warranted in patients with a change in vision or with a history of increased intraocular pressure, glaucoma, and/or cataracts.
Glaucoma and cataract formation were evaluated with intraocular pressure measurements and slit lamp examinations in a controlled 12-month study in 612 adolescent and adult patients aged 12 years and older with perennial allergic or vasomotor rhinitis (VMR). Of the 612 patients enrolled in the study, 405 were randomized to receive Dymista Nasal Spray (1 spray per nostril twice daily) and 207 were randomized to receive fluticasone propionate nasal spray (2 sprays per nostril once daily). In the Dymista Nasal Spray group, one patient had increased intraocular pressure at month 6. In addition, three patients had evidence of posterior subcapsular cataract at month 6 and one at month 12 (end of treatment). In the fluticasone propionate group, three patients had evidence of posterior subcapsular cataract at month 12 (end of treatment).
5.4 Immunosuppression
Persons who are using drugs, such as corticosteroids, that suppress the immune system are more susceptible to infections than healthy individuals. Chickenpox and measles, for example, can have a more serious or even fatal course in susceptible children or adults using corticosteroids. In children or adults who have not had these diseases or been properly immunized, particular care should be taken to avoid exposure. How the dose, route, and duration of corticosteroid administration affect the risk of developing a disseminated infection is not known. The contribution of the underlying disease and/or prior corticosteroid treatment to the risk is also not known. If exposed to chickenpox, prophylaxis with varicella zoster immune globulin (VZIG) may be indicated. If exposed to measles, prophylaxis with pooled intramuscular immunoglobulin (IG) may be indicated. (See the respective package inserts for complete VZIG and IG prescribing information.) If chickenpox develops, treatment with antiviral agents may be considered.
Corticosteroids should be used with caution, if at all, in patients with active or quiescent tuberculous infections of the respiratory tract; untreated local or systemic fungal or bacterial infections; systemic viral or parasitic infections; or ocular herpes simplex because of the potential for worsening of these infections.
5.5 Hypothalamic-Pituitary-Adrenal (HPA) Axis Effects
When intranasal steroids are used at higher than recommended dosages or in susceptible individuals at recommended dosages, systemic corticosteroid effects such as hypercorticism and adrenal suppression may appear. If such changes occur, the dosage of Dymista Nasal Spray should be discontinued slowly, consistent with accepted procedures for discontinuing oral corticosteroid therapy. The concomitant use of intranasal corticosteroids with other inhaled corticosteroids could increase the risk of signs or symptoms of hypercorticism and/or suppression of the HPA axis.
The replacement of a systemic corticosteroid with a topical corticosteroid can be accompanied by signs of adrenal insufficiency, and in addition some patients may experience symptoms of withdrawal, e.g., joint and/or muscular pain, lassitude, and depression. Patients previously treated for prolonged periods with systemic corticosteroids and transferred to topical corticosteroids should be carefully monitored for acute adrenal insufficiency in response to stress. In those patients who have asthma or other clinical conditions requiring long-term systemic corticosteroid treatment, too rapid a decrease in systemic corticosteroids may cause a severe exacerbation of their symptoms.
5.6 Use of Cytochrome P450 3A4 Inhibitors
Ritonavir and other strong cytochrome P450 3A4 (CYP3A4) inhibitors can significantly increase plasma fluticasone propionate exposure, resulting in significantly reduced serum cortisol concentrations [see Drug Interactions (7.2) and Clinical Pharmacology (12.3)]. During postmarketing use, there have been reports of clinically significant drug interactions in patients receiving fluticasone propionate and ritonavir, resulting in systemic corticosteroid effects including Cushing syndrome and adrenal suppression. Therefore, coadministration of Dymista Nasal Spray and ritonavir is not recommended unless the potential benefit to the patient outweighs the risk of systemic corticosteroid side effects.
Use caution with the coadministration of Dymista Nasal Spray and other potent CYP3A4 inhibitors, such as ketoconazole [see Drug Interactions (7.2) and Clinical Pharmacology (12.3)].
5.7 Effect on Growth
Corticosteroids may cause a reduction in growth velocity when administered to pediatric patients. Monitor the growth routinely of pediatric patients receiving Dymista Nasal Spray [see Use in Specific Populations (8.4)].
6 ADVERSE REACTIONS
Systemic and local corticosteroid use may result in the following:
- Somnolence [see Warnings and Precautions (5.1)]
- Local nasal effects, including epistaxis, nasal ulceration, nasal septal perforation, impaired wound healing, and Candida albicans infection [see Warnings and Precautions (5.2)]
- Glaucoma and cataracts [see Warnings and Precautions (5.3)]
- Immunosuppression [see Warnings and Precautions (5.4)]
- Hypothalamic-pituitary-adrenal (HPA) axis effects, including growth reduction [see Warnings and Precautions (5.5 and 5.7), Use in Specific Populations (8.4)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect rates observed in practice.
The safety data described below reflect exposure to Dymista Nasal Spray in 853 patients (12 years of age and older; 36% male and 64% female) with seasonal allergic rhinitis in 3 double-blind, placebo-controlled clinical trials of 2-week duration. The racial distribution for the 3 clinical trials was 80% white, 16% black, 2% Asian, and 1% other. In the 12-month open-label, active-controlled clinical trial, 404 Asian patients (240 males and 164 females) with perennial allergic rhinitis or vasomotor rhinitis were treated with Dymista Nasal Spray, 1 spray per nostril twice daily.
Adults and Adolescents 12 Years of Age and Older
In the 3 placebo controlled clinical trials of 2-week duration, 3411 patients with seasonal allergic rhinitis were treated with 1 spray per nostril of Dymista Nasal Spray, azelastine hydrochloride nasal spray, fluticasone propionate nasal spray, or placebo, twice daily. The azelastine hydrochloride and fluticasone propionate comparators use the same vehicle and device as Dymista Nasal Spray and are not commercially marketed. Overall, adverse reactions were 16% in the Dymista Nasal Spray treatment groups, 15% in the azelastine hydrochloride nasal spray groups, 13% in the fluticasone propionate nasal spray groups, and 12% in the placebo groups. Overall, 1% of patients in both the Dymista Nasal Spray and placebo groups discontinued due to adverse reactions.
Table 1 contains adverse reactions reported with frequencies greater than or equal to 2% and more frequently than placebo in patients treated with Dymista Nasal Spray in the seasonal allergic rhinitis controlled clinical trials.
| *Safety population N=853, intent-to-treat population N=848
† Not commercially marketed |
||||
| 1 spray per nostril twice daily | ||||
| Dymista Nasal Spray (N=853)* | Azelastine Hydrochloride Nasal Spray† (N=851) | Fluticasone Propionate Nasal Spray† (N=846) | Vehicle Placebo (N=861) |
|
| Dysgeusia | 30(4%) | 44(5%) | 4(1%) | 2(<1%) |
| Headache | 18(2%) | 20(2%) | 20(2%) | 10(1%) |
| Epistaxis | 16(2%) | 14(2%) | 14(2%) | 15(2%) |
In the above trials, somnolence was reported in <1% of patients treated with Dymista Nasal Spray (6 of 853) or vehicle placebo (1 of 861) [see Warnings and Precautions (5.1)].
Long-Term (12-Month) Safety Trial:
In the 12-month, open-label, active-controlled, long-term safety trial, 404 patients (12 years of age and older) with perennial allergic rhinitis or vasomotor rhinitis were treated with Dymista Nasal Spray 1 spray per nostril twice daily and 207 patients were treated with fluticasone propionate nasal spray, 2 sprays per nostril once daily. Overall, adverse reactions were 47% in the Dymista Nasal Spray treatment group and 44% in the fluticasone propionate nasal spray group. The most frequently reported adverse reactions (≥ 2%) with Dymista Nasal Spray were headache, pyrexia, cough, nasal congestion, rhinitis, dysgeusia, viral infection, upper respiratory tract infection, pharyngitis, pain, diarrhea, and epistaxis. In the Dymista Nasal Spray treatment group, 7 patients (2%) had mild epistaxis and 1 patient (<1%) had moderate epistaxis. In the fluticasone propionate nasal spray treatment group 1 patient (<1%) had mild epistaxis. No patients had reports of severe epistaxis. Focused nasal examinations were performed and no nasal ulcerations or septal perforations were observed. Eleven of 404 patients (3%) treated with Dymista Nasal Spray and 6 of 207 patients (3%) treated with fluticasone propionate nasal spray discontinued from the trial due to adverse events.
6.2 Postmarketing Experience
Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
The following spontaneous adverse events have been reported during the marketing of azelastine hydrochloride nasal spray and causal relationship with the drug is unknown: anaphylactoid reaction, application site irritation, atrial fibrillation, chest pain, confusion, dyspnea, facial edema, involuntary muscle contractions, nasal sores, palpitations, paresthesia, parosmia, pruritus, rash, disturbance or loss of sense of smell and/or taste, tolerance, urinary retention, vision abnormal and xerophthalmia.
In addition, the following events have been identified during post-approval use of fluticasone propionate nasal spray. These events have been chosen for inclusion due to either their seriousness, frequency of reporting, or causal connection to fluticasone propionate or a combination of these factors.
General: Hypersensitivity reactions, including angioedema, skin rash, edema of the face and tongue, pruritus, urticaria, bronchospasm, wheezing, dyspnea, and anaphylaxis/anaphylactoid reactions, which in rare instances were severe.
Ear, Nose, and Throat: Alteration or loss of sense of taste and/or smell and, rarely, nasal septal perforation, nasal ulcer, sore throat, throat irritation and dryness, cough, hoarseness, and voice changes.
Eye: Dryness and irritation, conjunctivitis, blurred vision, glaucoma, increased intraocular pressure, and cataracts.
Cases of growth suppression have been reported for intranasal corticosteroids, including fluticasone propionate [see Use in Specific Populations (8.4)].
7 DRUG INTERACTIONS
No formal drug interaction studies have been performed with Dymista Nasal Spray. The drug interactions of the combination are expected to reflect those of the individual components.
7.1 Central Nervous System Depressants
Concurrent use of Dymista Nasal Spray with alcohol or other central nervous system depressants should be avoided because somnolence and impairment of central nervous system performance may occur [see Warnings and Precautions (5.1)].
7.2 Cytochrome P450 3A4
Ritonavir (a strong CYP3A4 inhibitor) significantly increased plasma fluticasone propionate exposure following administration of fluticasone propionate aqueous nasal spray, resulting in significantly reduced serum cortisol concentrations [see Clinical Pharmacology (12.3)]. During postmarketing use, there have been reports of clinically significant drug interactions in patients receiving fluticasone propionate and ritonavir, resulting in systemic corticosteroid effects including Cushing syndrome and adrenal suppression. Therefore, coadministration of fluticasone propionate and ritonavir is not recommended unless the potential benefit to the patient outweighs the risk of systemic corticosteroid side effects.
Ketoconazole (also a strong CYP3A4 inhibitor), administered in multiple 200 mg doses to steady-state, increased plasma exposure of fluticasone propionate, reduced plasma cortisol AUC, but had no effect on urinary excretion of cortisol, following administration of a single 1000 mcg dose of fluticasone propionate by oral inhalation route.
Caution should be exercised when Dymista Nasal Spray is coadministered with ketoconazole and other known strong CYP3A4 inhibitors.
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Dymista Nasal Spray: Teratogenic Effects: Pregnancy Category C:
There are no adequate and well-controlled clinical trials of Dymista Nasal Spray, azelastine hydrochloride only, or fluticasone propionate only in pregnant women. Animal reproductive studies of azelastine hydrochloride and fluticasone propionate in mice, rats, and/or rabbits revealed evidence of teratogenicity as well as other developmental toxic effects. Because animal reproduction studies are not always predictive of human response, Dymista Nasal Spray should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Azelastine hydrochloride: Teratogenic Effects: In mice, azelastine hydrochloride caused embryo-fetal death, malformations (cleft palate; short or absent tail; fused, absent or branched ribs), delayed ossification, and decreased fetal weight at an oral dose approximately 610 times the maximum recommended human daily intranasal dose (MRHDID) in adults (on a mg/m2 basis at a maternal dose of 68.6 mg/kg). This dose also caused maternal toxicity as evidenced by decreased body weight. Neither fetal nor maternal effects occurred at a dose that was approximately 26 times the MRHDID (on a mg/m2 basis at a maternal dose of 3 mg/kg).
In rats, azelastine hydrochloride caused malformations (oligo- and brachydactylia), delayed ossification and skeletal variations, in the absence of maternal toxicity, at an oral dose approximately 530 times the MRHDID in adults (on a mg/m2 basis at a maternal dose of 30 mg/kg). At a dose approximately 1200 times the MRHDID (on a mg/m2 basis at a maternal dose of 68.6 mg/kg), azelastine hydrochloride also caused embryo-fetal death and decreased fetal weight; however, this dose caused severe maternal toxicity. Neither fetal nor maternal effects occurred at a dose approximately 53 times the MRHDID (on a mg/m2 basis at a maternal dose of 3 mg/kg).
In rabbits, azelastine hydrochloride caused abortion, delayed ossification, and decreased fetal weight at oral doses approximately 1100 times the MRHDID in adults (on a mg/m2 basis at a maternal dose of 30 mg/kg); however, these doses also resulted in severe maternal toxicity. Neither fetal nor maternal effects occurred at a dose approximately 11 times the MRHDID (on a mg/m2 basis at a maternal dose of 0.3 mg/kg).
Fluticasone propionate: Teratogenic Effects: Corticosteroids have been shown to be teratogenic in laboratory animals when administered systemically at relatively low dosage levels. Subcutaneous studies in the mouse and rat at doses approximately equivalent to and 4 times, respectively, the MRHDID in adults (on a mcg/m2 basis at maternal doses of 45 and 100 mcg/kg, respectively), revealed fetal toxicity characteristic of potent corticosteroid compounds, including embryonic growth retardation, omphalocele, cleft palate, and retarded cranial ossification.
In the rabbit, fetal weight reduction and cleft palate were observed at a subcutaneous dose less than the MRHDID in adults (on a mcg/m2 basis at a maternal dose of 4 mcg/kg). However, no teratogenic effects were reported at oral doses up to approximately 25 times the MRHDID in adults (on a mcg/m2 basis at a maternal dose of 300 mcg/kg) of fluticasone propionate to the rabbit. No fluticasone propionate was detected in the plasma in this study, consistent with the established low bioavailability following oral administration [see Clinical Pharmacology (12.3)].
Experience with oral corticosteroids since their introduction in pharmacologic, as opposed to physiologic, doses suggests that rodents are more prone to teratogenic effects from corticosteroids than humans. In addition, because there is a natural increase in corticosteroid production during pregnancy, most women will require a lower exogenous corticosteroid dose and many will not need corticosteroid treatment during pregnancy.
Nonteratogenic Effects: Fluticasone propionate crossed the placenta following oral administration of approximately 4 and 25 times the MRHDID in adults (on a mcg/m2 basis at maternal doses of 100 mcg/kg and 300 mcg/kg to rats and rabbits, respectively).
8.3 Nursing Mothers
Dymista Nasal Spray: It is not known whether Dymista Nasal Spray is excreted in human breast milk. Because many drugs are excreted in human milk, caution should be exercised when Dymista Nasal Spray is administered to a nursing woman. Since there are no data from well-controlled human studies on the use of Dymista Nasal Spray by nursing mothers, based on data from the individual components, a decision should be made whether to discontinue nursing or to discontinue Dymista Nasal Spray, taking into account the importance of Dymista Nasal Spray to the mother.
Azelastine hydrochloride: It is not known if azelastine hydrochloride is excreted in human milk.
Fluticasone propionate: It is not known if fluticasone propionate is excreted in human milk. However, other corticosteroids are excreted in human milk. Subcutaneous administration to lactating rats of 10 mcg/kg of tritiated fluticasone propionate (less than the maximum recommended daily intranasal dose in adults on a mcg/m2 basis) resulted in measurable radioactivity in the milk.
8.4 Pediatric Use
Safety and effectiveness of Dymista Nasal Spray in pediatric patients below the age of 12 years have not been established.
Controlled clinical studies have shown that intranasal corticosteroids may cause a reduction in growth velocity in pediatric patients. This effect has been observed in the absence of laboratory evidence of HPA axis suppression, suggesting that growth velocity is a more sensitive indicator of systemic corticosteroid exposure in pediatric patients than some commonly used tests of HPA axis function. The long-term effects of this reduction in growth velocity associated with intranasal corticosteroids, including the impact on final adult height, are unknown. The potential for “catch-up” growth following discontinuation of treatment with intranasal corticosteroids has not been adequately studied. The growth of pediatric patients receiving intranasal corticosteroids, including Dymista Nasal Spray, should be monitored routinely (e.g., via stadiometry). The potential growth effects of prolonged treatment should be weighed against the clinical benefits obtained and the risks/benefits of treatment alternatives.
8.5 Geriatric Use
Clinical trials of Dymista Nasal Spray did not include sufficient numbers of patients 65 years of age and older to determine whether they respond differently from younger patients. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
10 OVERDOSAGE
Dymista Nasal Spray: Dymista Nasal Spray contains both azelastine hydrochloride and fluticasone propionate; therefore, the risks associated with overdosage for the individual components described below apply to Dymista Nasal Spray.
Azelastine hydrochloride: There have been no reported overdosages with azelastine hydrochloride. Acute azelastine hydrochloride overdosage by adults with this dosage form is unlikely to result in clinically significant adverse events, other than increased somnolence, since one (1) 23 g bottle of Dymista Nasal Spray contains approximately 23 mg of azelastine hydrochloride. Clinical trials in adults with single doses of the oral formulation of azelastine hydrochloride (up to 16 mg) have not resulted in increased incidence of serious adverse events. General supportive measures should be employed if overdosage occurs. There is no known antidote to Dymista Nasal Spray. Oral ingestion of antihistamines has the potential to cause serious adverse effects in children. Accordingly, Dymista Nasal Spray should be kept out of the reach of children.
Fluticasone propionate: Chronic fluticasone propionate overdosage may result in signs/symptoms of hypercorticism [see Warnings and Precautions (5.5)]. Intranasal administration of 2 mg (10 times the recommended dose) of fluticasone propionate twice daily for 7 days to healthy human volunteers was well tolerated. Single oral fluticasone propionate doses up to 16 mg have been studied in human volunteers with no acute toxic effects reported. Repeat oral doses up to 80 mg daily for 10 days in volunteers and repeat oral doses up to 10 mg daily for 14 days in patients were well tolerated. Adverse reactions were of mild or moderate severity, and incidences were similar in active and placebo treatment groups. Acute overdosage with this dosage form is unlikely since one (1) 23 g bottle of Dymista Nasal Spray contains approximately 8.5 mg of fluticasone propionate.
11 DESCRIPTION
Dymista (azelastine hydrochloride and fluticasone propionate) Nasal Spray is formulated as a white, uniform metered-spray suspension for intranasal administration. It is a fixed dose combination product containing an antihistamine (H1 receptor antagonist) and a corticosteroid as active ingredients.
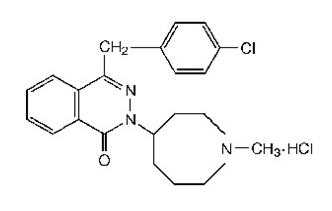
Azelastine hydrochloride active ingredient occurs as a white, odorless, crystalline powder with a bitter taste. It has a molecular weight of 418.37. It is sparingly soluble in water, methanol, and propylene glycol and slightly soluble in ethanol, octanol, and glycerin. It has a melting point of 225°C and the pH of 5.2. Its chemical name is (±)-1-(2H)-phthalazinone,4-[(4-chlorophenyl) methyl]-2-(hexahydro-1-methyl-1H-azepin-4-yl)-, monohydrochloride. Its molecular formula is C22H24ClN3O•HCl with the following chemical structure:
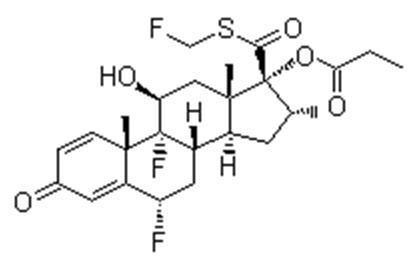
Fluticasone propionate active ingredient is a white powder with a melting point of 273°C, a molecular weight of 500.6, and the empirical formula is C25H31F3O5S. It is practically insoluble in water, freely soluble in dimethyl sulfoxide and dimethylformamide, and slightly soluble in methanol and 95% ethanol. Fluticasone propionate is a synthetic corticosteroid having the chemical name S-(fluoromethyl)-6α,9-difluoro-11β,-17-dihydroxy-16α-methyl-3-oxoandrosta-1,4-diene-17β-carbothioate, 17-propionate, and the following chemical structure:
Dymista (azelastine hydrochloride and fluticasone propionate) Nasal Spray, 137 mcg / 50 mcg contains 0.1% solution of azelastine hydrochloride and 0.037% suspension of micronized fluticasone propionate in an isotonic aqueous suspension containing glycerin, microcrystalline cellulose and carboxymethylcellulose sodium, phenylethyl alcohol (2.5 mg/g), edetate disodium, benzalkonium chloride (0.1 mg/g), polysorbate 80, and purified water. It has a pH of approximately 6.0.
After priming [see Dosage and Administration (2.2)], each metered spray delivers a 0.137 mL mean volume of suspension containing 137 mcg of azelastine hydrochloride (equivalent to 125 mcg of azelastine base) and 50 mcg of fluticasone propionate. The 23 g bottle provides 120 metered sprays, after priming.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Dymista Nasal Spray: Dymista Nasal Spray contains both azelastine hydrochloride and fluticasone propionate; therefore, the mechanisms of actions described below for the individual components apply to Dymista Nasal Spray. These drugs represent two different classes of medications (histamine H1-receptor antagonist and synthetic corticosteroid).
Azelastine hydrochloride: Azelastine hydrochloride, a phthalazinone derivative, exhibits histamine H1-receptor antagonist activity in isolated tissues, animal models, and humans. Azelastine hydrochloride in Dymista Nasal Spray is administered as a racemic mixture with no difference in pharmacologic activity noted between the enantiomers in in vitro studies. The major metabolite, desmethylazelastine, also possesses H1-receptor antagonist activity.
Fluticasone propionate: Fluticasone propionate is a synthetic trifluorinated corticosteroid with anti-inflammatory activity. In vitro dose response studies on a cloned human glucocorticoid receptor system involving binding and gene expression afforded 50% responses at 1.25 and 0.17 nM concentrations, respectively. Fluticasone propionate was 3-fold to 5-fold more potent than dexamethasone in these assays. Data from the McKenzie vasoconstrictor assay in man also support its potent glucocorticoid activity. The clinical relevance of these findings is unknown.
The precise mechanism through which fluticasone propionate affects allergic rhinitis symptoms is not known. Corticosteroids have been shown to have a wide range of effects on multiple cell types (e.g., mast cells, eosinophils, neutrophils, macrophages, and lymphocytes) and mediators (e.g., histamine, eicosanoids, leukotrienes, and cytokines) involved in inflammation.
12.2 Pharmacodynamics
Cardiac Effects:
In a placebo-controlled trial (95 patients with allergic rhinitis), there was no evidence of an effect of azelastine hydrochloride nasal spray (2 sprays per nostril twice daily for 56 days) on cardiac repolarization as represented by the corrected QT interval (QTc) of the electrocardiogram. Following multiple dose oral administration of azelastine 4 mg or 8 mg twice daily, the mean change in QTc was 7.2 msec and 3.6 msec, respectively.
Interaction studies investigating the cardiac repolarization effects of concomitantly administered oral azelastine hydrochloride and erythromycin or ketoconazole were conducted. These drugs had no effect on QTc based on analysis of serial electrocardiograms.
12.3 Pharmacokinetics
Absorption: After intranasal administration of two sprays per nostril (548 mcg of azelastine hydrochloride and 200 mcg of fluticasone) of Dymista Nasal Spray, the mean (± standard deviation) peak plasma exposure (Cmax) was 194.5 ± 74.4 pg/mL for azelastine and 10.3±3.9 pg/mL for fluticasone propionate and the mean total exposure (AUC) was 4217 ± 2618 pg/mL*hr for azelastine and 97.7 ± 43.1 pg/mL*hr for fluticasone. The median time to peak exposure (tmax) from a single dose was 0.5 hours for azelastine and 1.0 hours for fluticasone.
Systemic bioavailability of azelastine from Dymista Nasal Spray following intranasal administration was comparable with monotherapy azelastine hydrochloride (Astelin®) nasal spray (i.e., approximately 40%). Systemic bioavailability of fluticasone from Dymista Nasal Spray following intranasal administration was 44-61% higher than monotherapy fluticasone propionate (bioavailability for monotherapy fluticasone nasal spray was less than 2%). Due to the low intranasal bioavailability, pharmacokinetic data for fluticasone propionate were obtained via other routes of administration. Studies using oral dosing of radiolabeled fluticasone propionate showed negligible oral bioavailability and high extraction from plasma. The majority of the circulating radioactivity was due to an inactive metabolite.
Distribution: Based on intravenous and oral administration, the steady-state volume of distribution of azelastine hydrochloride is 14.5 L/kg. In vitro studies with human plasma indicate that the plasma protein binding of azelastine hydrochloride and its metabolite, desmethylazelastine, are approximately 88% and 97%, respectively.
Following intravenous administration, the initial disposition phase for fluticasone propionate was rapid and consistent with its high lipid solubility and tissue binding. The volume of distribution averaged 4.2 L/kg.
The percentage of fluticasone propionate bound to human plasma proteins averaged 91% with no obvious concentration relationship. Fluticasone propionate is weakly and reversibly bound to erythrocytes and freely equilibrates between erythrocytes and plasma. Fluticasone propionate is not significantly bound to human transcortin.
Metabolism: Azelastine hydrochloride is oxidatively metabolized to the principal active metabolite, desmethylazelastine, by the cytochrome P450 enzyme system. The specific P450 isoforms responsible for the biotransformation of azelastine have not been identified. The total clearance of azelastine is approximately 0.50 L/kg/hr.
For fluticasone propionate, the only circulating metabolite detected in man is the 17β-carboxylic acid derivative, which is formed through the CYP3A4 pathway. This inactive metabolite had less affinity (approximately 1/2,000) than the parent drug for the glucocorticoid receptor of human lung cytosol in vitro and negligible pharmacological activity in animal studies. Other metabolites detected in vitro using cultured human hepatoma cells have not been detected in man. The average total clearance of fluticasone propionate is relatively high (approximately 66 L/hr).
Elimination: Following intranasal administration of Dymista Nasal Spray, the elimination half-life of azelastine hydrochloride is approximately 25 hours. Approximately 75% of an oral dose of radiolabeled azelastine hydrochloride was excreted in the feces with less than 10% as unchanged azelastine.
Following intravenous dosing, fluticasone propionate showed polyexponential kinetics and had a terminal elimination half-life of approximately 7.8 hours. Less than 5% of a radiolabeled oral dose was excreted in the urine as metabolites, with the remainder excreted in the feces as parent drug and metabolites.
Special Populations:
Dymista Nasal Spray was not studied in any special populations, and no gender-specific pharmacokinetic data have been obtained.
Hepatic Impairment: Following oral administration of azelastine hydrochloride, pharmacokinetic parameters were not influenced by hepatic impairment.
Renal Impairment: Based on oral, single-dose studies of azelastine hydrochloride, renal impairment (creatinine clearance <50 mL/min) resulted in a 70-75% higher Cmax and AUC compared to healthy subjects. Time to maximum concentration was unchanged.
Age: Following oral administration of azelastine hydrochloride, pharmacokinetic parameters were not influenced by age.
Gender: Following oral administration of azelastine hydrochloride, pharmacokinetic parameters were not influenced by gender.
Race: The effect of race has not been evaluated.
Drug-Drug Interactions:
No formal drug interaction studies have been performed with Dymista Nasal Spray. The drug interactions of the combination are expected to reflect those of the individual components.
Erythromycin: Coadministration of orally administered azelastine (4 mg twice daily) with erythromycin (500 mg three times daily for 7 days) resulted in Cmax of 5.36 ± 2.6 ng/mL and AUC of 49.7 ± 24 ng•h/mL for azelastine, whereas, administration of azelastine alone resulted in Cmax of 5.57 ± 2.7 ng/mL and AUC of 48.4 ± 24 ng•h/mL for azelastine.
In another multiple-dose drug interaction study, coadministration of orally inhaled fluticasone propionate (500 mcg twice daily) and erythromycin (333 mg three times daily) did not affect fluticasone propionate pharmacokinetics.
Cimetidine and Ranitidine: In a multiple-dose, steady-state drug interaction trial in healthy subjects, cimetidine (400 mg twice daily) increased orally administered mean azelastine hydrochloride (4 mg twice daily) concentrations by approximately 65%. Coadministration of orally administered azelastine hydrochloride (4 mg twice daily) with ranitidine hydrochloride (150 mg twice daily) resulted in Cmax of 8.89 ± 3.28 ng/mL and AUC of 88.22 ± 40.43 ng•h/mL for azelastine hydrochloride, whereas, administration of azelastine hydrochloride alone resulted in Cmax of 7.83 ± 4.06 ng/mL and AUC of 80.09 ± 43.55 ng•h/mL for azelastine hydrochloride.
Theophylline: No significant pharmacokinetic interaction was observed with the coadministration of an oral 4 mg dose of azelastine hydrochloride twice daily and theophylline 300 mg or 400 mg twice daily.
Ritonavir: Coadministration of fluticasone propionate and the strong CYP3A4 inhibitor, ritonavir, is not recommended based upon a multiple-dose, crossover drug interaction study in 18 healthy subjects. Fluticasone propionate aqueous nasal spray (200 mcg once daily) was coadministered for 7 days with ritonavir (100 mg twice daily). Plasma fluticasone propionate concentrations following fluticasone propionate aqueous nasal spray alone were undetectable (<10 pg/mL) in most subjects, and when concentrations were detectable, peak levels (Cmax) averaged 11.9 pg/mL (range, 10.8 to 14.1 pg/mL) and AUC(0-τ) averaged 8.43 pg•hr/mL (range, 4.2 to 18.8 pg•hr/mL). Fluticasone propionate Cmax and AUC(0-τ) increased to 318 pg/mL (range, 110 to 648 pg/mL) and 3,102.6 pg•hr/mL (range, 1,207.1 to 5,662.0 pg•hr/mL), respectively, after coadministration of ritonavir with fluticasone propionate aqueous nasal spray. This significant increase in plasma fluticasone propionate exposure resulted in a significant decrease (86%) in plasma cortisol area under the plasma concentration versus time curve (AUC).
Caution should be exercised when other strong CYP3A4 inhibitors are coadministered with fluticasone propionate. In a drug interaction study, coadministration of orally inhaled fluticasone propionate (1,000 mcg) and ketoconazole (200 mg once daily) resulted in increased fluticasone propionate exposure and reduced plasma cortisol AUC, but had no effect on urinary excretion of cortisol. [see Drug Interactions (7.2)]
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Dymista Nasal Spray: No studies of carcinogenicity, mutagenicity, or impairment of fertility were conducted with Dymista Nasal Spray; however, studies are available for the individual active components, azelastine hydrochloride and fluticasone propionate, as described below.
Azelastine hydrochloride: In 2-year carcinogenicity studies in rats and mice, azelastine hydrochloride did not show evidence of carcinogenicity at oral doses up to 30 mg/kg and 25 mg/kg, respectively. These doses were approximately 530 and 220 times the maximum recommended human daily intranasal dose [MRHDID] on a mg/m2 basis.
Azelastine hydrochloride showed no genotoxic effects in the Ames test, DNA repair test, mouse lymphoma forward mutation assay, mouse micronucleus test, or chromosomal aberration test in rat bone marrow.
Reproduction and fertility studies in rats showed no effects on male or female fertility at oral doses up to 30 mg/kg (approximately 530 times the MRHDID in adults on a mg/m2 basis). At 68.6 mg/kg (approximately 1200 times the MRHDID on a mg/m2 basis), the duration of estrous cycles was prolonged and copulatory activity and the number of pregnancies were decreased. The numbers of corpora lutea and implantations were decreased; however, pre-implantation loss was not increased.
Fluticasone propionate: Fluticasone propionate demonstrated no tumorigenic potential in mice at oral doses up to 1,000 mcg/kg (approximately 20 times the maximum recommended daily intranasal dose in adults and approximately 10 times the maximum recommended daily intranasal dose in children on a mcg/m2 basis) for 78 weeks or in rats at inhalation doses up to 57 mcg/kg (approximately 2 times the MRHDID in adults on a mcg/m2 basis) for 104 weeks.
Fluticasone propionate did not induce gene mutation in prokaryotic or eukaryotic cells in vitro. No significant clastogenic effect was seen in cultured human peripheral lymphocytes in vitro or in the mouse micronucleus test.
No evidence of impairment of fertility was observed in reproductive studies conducted in male and female rats at subcutaneous doses up to 50 mcg/kg (approximately 2 times the MRHDID in adults on a mcg/m2 basis). Prostate weight was significantly reduced at a subcutaneous dose of 50 mcg/kg.
14 CLINICAL STUDIES
The efficacy and safety of Dymista Nasal Spray in seasonal allergic rhinitis was evaluated in 3 randomized, multicenter, double-blind, placebo-controlled clinical trials in 853 adult and adolescent patients 12 years and older with seasonal allergic rhinitis. The population of the trials was 12 to 78 years of age (64% female, 36% male; 80% white, 16% black, 2% Asian, 1% other).
Patients were randomized to one of four treatment groups: one spray per nostril twice daily of Dymista Nasal Spray, azelastine hydrochloride nasal spray, fluticasone propionate nasal spray, and vehicle placebo. The azelastine hydrochloride and fluticasone propionate comparators use the same device and vehicle as Dymista Nasal Spray and are not commercially marketed. Assessment of efficacy was based on the reflective total nasal symptom score (rTNSS), in addition to the instantaneous total nasal symptom score (iTNSS) and other supportive secondary efficacy variables. TNSS is calculated as the sum of the patients' scoring of the 4 individual nasal symptoms (rhinorrhea, nasal congestion, sneezing, and nasal itching) on a 0 to 3 categorical severity scale (0 = absent, 1 = mild, 2 = moderate, 3 = severe). Patients were required to record symptom severity daily reflecting over the previous 12 hours (morning, AM, and evening, PM). For the primary efficacy endpoint, the combined AM+PM rTNSS (maximum score of 24) was assessed as a change from baseline for each day and then averaged over a 2-week treatment period. The primary efficacy endpoint was the mean change from baseline in combined AM+PM rTNSS over 2 weeks. The iTNSS was recorded immediately prior to the next dose.
In these trials, Dymista Nasal Spray demonstrated statistically significant greater decreases in rTNSS as compared to azelastine hydrochloride and to fluticasone propionate, as well as to placebo. The differences between the monotherapies and placebo also were statistically significant. Representative results from one of the trials are shown below (Table 2).
| * Sum of AM and PM rTNSS for each day (Maximum Score =24) and averaged over the 14 day treatment period
† Not commercially marketed |
||||||
| LS Mean, 95% CI, and p-value are obtained from the repeated-measures analysis of covariance model using observed data. | ||||||
| Baseline | Change from
Baseline | Difference From Dymista Nasal Spray | ||||
| Treatment
(one spray /nostril twice daily) | N | LS Mean | LS Mean | LS Mean | 95% CI | P-value |
| Dymista Nasal Spray | 207 | 18.3 | -5.6 | -- | -- | -- |
| Azelastine HCl Nasal Spray† | 208 | 18.3 | -4.3 | -1.4 | (-2.2, -0.5) | 0.002 |
| Fluticasone Propionate Nasal Spray† | 207 | 18.2 | -4.7 | -1.0 | (-1.8, -0.2) | 0.022 |
| Placebo | 209 | 18.6 | -2.9 | -2.7 | (-3.5, -1.9) | <0.001 |
In these trials, Dymista Nasal Spray also demonstrated statistically significant, greater decreases in iTNSS as compared to placebo, as did the azelastine hydrochloride and fluticasone propionate comparators. Representative results from one of the trials are shown below (Table 3).
| * Sum of AM and PM iTNSS for each day (Maximum Score =24) and averaged over the 14 day treatment period
† Not commercially marketed |
||||||
| LS Mean, 95% CI, and p-value are obtained from the repeated-measures analysis of covariance model using observed data. | ||||||
| Baseline | Change from
Baseline | Difference From Placebo | ||||
| Treatment
(one spray /nostril twice daily) | N | LS Mean | LS Mean | LS Mean | 95% CI | P-value |
| Dymista Nasal Spray | 207 | 17.2 | -5.2 | -2.6 | (-3.4, -1.8) | <0.001 |
| Azelastine HCl Nasal Spray† | 208 | 16.8 | -3.9 | -1.3 | (-2.0, -0.6) | <0.001 |
| Fluticasone Propionate Nasal Spray† | 207 | 16.8 | -4.5 | -1.9 | (-2.6, -1.2) | <0.001 |
| Placebo | 209 | 17.3 | -2.7 | -- | -- | -- |
Onset of action, defined as the first timepoint at which Dymista Nasal Spray was statistically superior to placebo in the mean change from baseline in iTNSS and which was sustained thereafter, was assessed in each of the three trials. Onset of action was observed as early as 30 minutes following the initial dose of Dymista Nasal Spray.
The subjective impact of seasonal allergic rhinitis on patient's health-related quality of life was evaluated by the Rhinoconjunctivitis Quality of Life Questionnaire (RQLQ) (28 items in 7 domains (activities, sleep, non-nose/eye symptoms, practical problems, nasal symptoms, eye symptoms, and emotional) evaluated on a 7-point scale where 0=no impairment and 6=maximum impairment), which was administered to patients 18 years of age and older. An overall RQLQ score is calculated from the mean of all items in the instrument. A change from baseline of at least 0.5 points is considered a clinically meaningful improvement. In each of these trials, Dymista Nasal Spray demonstrated a statistically significant greater decrease from baseline in the overall RQLQ than placebo, which ranged from -0.55 (95% CI -0.72, -0.39) to -0.80 (95% CI -1.05, -0.55). In these trials, the treatment differences between Dymista Nasal Spray and the monotherapies were less than the minimum important difference of 0.5 points.
16 HOW SUPPLIED/STORAGE AND HANDLING
Dymista Nasal Spray (NDC 0037-0245-23) is supplied as an amber glass bottle fitted with a metered-dose spray pump unit. The spray pump unit consists of a nasal spray pump with a white nasal adapter and clear plastic dust cap. Each bottle contains a net fill weight of 23 g and will deliver 120 metered sprays after priming [see Dosage and Administration (2.1)]. Dymista Nasal Spray should be shaken gently before each use and primed with 6 sprays before the initial use or with 1 spray after a non-use period of 14 days. Each spray delivers a suspension volume of 0.137 mL as a fine mist, containing 137 mcg of azelastine hydrochloride and 50 mcg of fluticasone propionate (137 mcg/50 mcg). The correct amount of medication in each spray cannot be assured before the initial priming and after 120 sprays have been used, even though the bottle is not completely empty. The bottle should be discarded after 120 medicated sprays have been used.
Dymista Nasal Spray should not be used after the expiration date “EXP” printed on the bottle label and carton.
17 PATIENT COUNSELING INFORMATION
See FDA-approved patient labeling (Patient Information and Instructions for Use)
Patients should be instructed to use Dymista Nasal Spray only as prescribed. For the proper use of the nasal spray and to attain maximum improvement, the patient should read and follow carefully the accompanying FDA-Approved Patient Labeling.
17.1 Somnolence
Somnolence has been reported in some patients (6 of 853 patients) taking Dymista Nasal Spray. Patients should be cautioned against engaging in hazardous occupations requiring complete mental alertness and motor coordination such as driving or operating machinery after administration of Dymista Nasal Spray [see Warnings and Precautions (5.1)].
17.2 Concurrent Use of Alcohol and other Central Nervous System Depressants
Concurrent use of Dymista Nasal Spray with alcohol or other central nervous system depressants should be avoided because additional reductions in alertness and additional impairment of central nervous system performance may occur [see Warnings and Precautions (5.1)].
17.3 Local Nasal Effects
Nasal corticosteroids are associated with nasal septal perforation and impaired wound healing. Patients who have experienced recent nasal ulcers, nasal surgery, or nasal trauma should not use Dymista Nasal Spray until healing has occurred [see Warnings and Precautions (5.2)].
17.4 Glaucoma and Cataracts
Patients should be informed that glaucoma and cataracts are associated with nasal and inhaled corticosteroid use. Patients should inform his/her health care provider if a change in vision is noted while using Dymista Nasal Spray [see Warnings and Precautions (5.3)].
17.5 Immunosuppression
Patients who are on immunosuppressant doses of corticosteroids should be warned to avoid exposure to chickenpox or measles and, if exposed, to consult their physician without delay. Patients should be informed of potential worsening of existing tuberculosis, fungal, bacterial, viral or parasitic infections, or ocular herpes simplex [see Warnings and Precautions (5.4)].
17.6 Priming
Patients should be instructed to shake the bottle gently before each use and prime the pump before initial use and when Dymista Nasal Spray has not been used for 14 or more days [see Dosage and Administration (2.2)].
17.7 Keep Spray Out of Eyes
Patients should be instructed to avoid spraying Dymista Nasal Spray into their eyes.
17.8 Keep Out of Children's Reach
Patients should be instructed to keep Dymista Nasal Spray out of the reach of children. If a child accidentally ingests Dymista Nasal Spray, seek medical help or call a poison control center immediately.
17.9 Potential Drug Interactions
Patients should be advised that coadministration of Dymista Nasal Spray and ritonavir is not recommended and to be cautious if Dymista Nasal Spray is coadministered with ketoconazole [see Drug Interactions (7.2)].
U.S. Patents 8,163,723; 8,168,620
Manufactured by:
Cipla Ltd. Goa, India
Distributed by:
MEDA PHARMACEUTICALS®
Meda Pharmaceuticals Inc.
Somerset, New Jersey 08873-4120
Dymista is a trademark of Meda Pharmaceuticals Inc.
Made in India.
PATIENT INFORMATION
Dymista Nasal Spray (Dy-Mist-A)
(azelastine hydrochloride and fluticasone propionate)
Nasal Spray
Important: For use in your nose only
Read this Patient Information before you start using Dymista Nasal Spray and each time you get a refill. There may be new information. This information does not take the place of talking to your healthcare provider about your medical condition or your treatment.
What is Dymista Nasal Spray?
Dymista Nasal Spray is a prescription medicine used to treat symptoms of seasonal allergic rhinitis in people 12 years of age and older, who need treatment with both azelastine hydrochloride and fluticasone propionate. It helps reduce the symptoms of seasonal allergic rhinitis (inflammation of the lining of the nose), such as stuffy nose, itching, and sneezing.
It is not known if Dymista Nasal Spray is safe or effective in children under 12 years of age.
What should I tell my healthcare provider before using Dymista Nasal Spray?
Before using Dymista Nasal Spray tell your healthcare provider if you:
- have had recent nasal sores, nasal surgery, or nasal injury
- have eye or vision problems, such as cataracts or glaucoma (increased pressure in your eye)
- have tuberculosis or any untreated fungal, bacterial, viral infections or eye infections caused by herpes
- have been near someone who has chickenpox or measles
- are not feeling well or have any other symptoms that you do not understand
- have any other medical conditions
- are pregnant or plan to become pregnant. It is not known if Dymista Nasal Spray will harm your unborn baby. Talk to your doctor if you are pregnant or plan to become pregnant.
- are breastfeeding or plan to breastfeed. It is not known if Dymista Nasal Spray passes into your breast milk. Talk to your doctor about the best way to feed your baby while using Dymista Nasal Spray.
Tell your healthcare provider about all the medicines you take, including prescription and non-prescription medicines, vitamins, and herbal supplements.
Dymista Nasal Spray may affect the way other medicines work, and other medicines may affect how Dymista Nasal Spray works.
Especially tell your healthcare provider if you take:
- ritanovir (Norvir) or medicines that contain ritanovir (commonly used to treat HIV infection or AIDS)
- ketoconazole, fluconazole, or itraconazole (for fungal infections)
Ask your healthcare provider or pharmacist for a list of these medications, if you are not sure.
Know the medicines you take. Keep a list of your medicines and show it to your healthcare provider and pharmacist when you get a new medicine.
How should I use Dymista Nasal Spray?
- See the Patient Instructions for Use at the end of this leaflet for information about the right way to use Dymista Nasal Spray.
- Dymista Nasal Spray is for use in your nose only. Do not spray it into your eyes or mouth. If you spray Dymista Nasal Spray into your eyes, flush your eye(s) with large amounts of water for 10 minutes and then call your doctor.
- Use Dymista Nasal Spray exactly as your healthcare provider tells you to use it. Your healthcare provider will tell you how much Dymista Nasal Spray to use and when to use it.
- If a child accidentally swallows Dymista Nasal Spray or you use too much Dymista Nasal Spray, call your doctor or go to the nearest hospital emergency room right away.
What should I avoid while using Dymista Nasal Spray?
- Dymista Nasal Spray can cause sleepiness or drowsiness. Do not drive, operate machinery, or do anything that needs you to be alert until you know how Dymista Nasal Spray affects you.
- Do not drink alcohol or take any other medicines that may cause you to feel sleepy while using Dymista Nasal Spray. It can increase your chances of having serious side effects.
What are the possible side effects of Dymista Nasal Spray?
Dymista Nasal Spray may cause serious side effects including:
- Sleepiness or drowsiness.
-
Nasal Problems. Symptoms of nasal problems may include:
- crusting in the nose
- nosebleeds
- runny nose
- hole in the cartilage between your nose (nasal septal perforation). A whistling sound when you breathe may be a symptom of nasal septal perforation.
- Slow wound healing. You should not use Dymista Nasal Spray until your nose has healed if you have a sore in your nose, if you have had surgery on your nose, or if your nose has been injured.
- Thrush (candida), a fungal infection in your nose and throat. Tell your doctor if you have any redness or white colored patches in your nose or mouth.
- Eye problems, such as glaucoma or cataracts. Some people may have eye problems, including glaucoma and cataracts. You should have regular eye exams when using Dymista Nasal Spray.
-
Immune system problems that may increase your risk of infections. Dymista Nasal Spray may cause problems with the way your immune system protects your body against infection and increase your risk of infection. Avoid contact with people who have contagious diseases such as chickenpox or measles while you use Dymista Nasal Spray. Symptoms of infection may include:
- fever
- aches or pains
- chills
- feeling tired
-
Adrenal Insufficiency. Adrenal insufficiency is a condition in which the adrenal glands do not make enough steroid hormones. Symptoms of adrenal insufficiency may include:
- tiredness
- weakness
- nausea
- vomiting
- low blood pressure
- Slowed or delayed growth in children. A child's growth should be checked regularly while using Dymista Nasal Spray.
Call your healthcare provider or get medical help right away if you have symptoms of any of the serious side effects listed above.
The most common side effects of Dymista Nasal Spray include:
- changes in taste
- nosebleeds
- headache
Tell your healthcare provider if you have any side effect that bothers you or that does not go away. These are not all of the possible side effects of Dymista Nasal Spray. For more information, ask your healthcare provider or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store Dymista Nasal Spray?
- Store Dymista Nasal Spray upright at controlled room temperature 68° to 77°F (20° to 25°C).
- Do not freeze or refrigerate Dymista Nasal Spray.
- Protect Dymista Nasal Spray from light.
- Safely throw away medicine that is out of date or no longer needed.
- Throw away your Dymista Nasal Spray bottle after using 120 sprays after initial priming. Even though the bottle may not be completely empty, you may not get the correct dose of medicine if you continue to use it.
Keep Dymista Nasal Spray and all medicines out of reach of children.
General information about Dymista Nasal Spray
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet. Do not use Dymista Nasal Spray for a condition for which it was not prescribed. Do not give Dymista Nasal Spray to other people, even if they have the same symptoms that you have. It may harm them.
This Patient Information leaflet summarizes the most important information about Dymista Nasal Spray. If you would like more information, talk with your healthcare provider. You can ask your pharmacist or healthcare provider for information about Dymista Nasal Spray that is written for health professionals.
For more information, go to www.DYMISTA.com or call Meda Pharmaceuticals Inc. at 1-888-939-6478.
What are the ingredients in Dymista Nasal Spray?
Active ingredients: azelastine hydrochloride and fluticasone propionate
Inactive ingredients: glycerin, microcrystalline cellulose and carboxymethylcellulose sodium, phenylethyl alcohol, edetate disodium, benzalkonium chloride, polysorbate 80, and purified water.
Instructions for Use
For use in your nose only. Do not spray in your eyes.
Read the Instructions for Use before you start to use Dymista Nasal Spray and each time you get a refill. There may be new information. This leaflet does not take the place of talking with your healthcare provider about your medical condition or treatment. Before you use Dymista Nasal Spray, make sure your healthcare provider shows you the right way to use it.
Shake the bottle gently before each use.
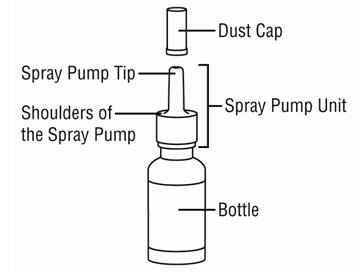
Your Dymista Nasal Spray pump. (See Figure A)
Figure A
Instructions for Using Your Dymista Nasal Spray Pump.
Before you use Dymista Nasal Spray for the first time, you will need to prime the bottle.
Before you prime the bottle, shake it gently.
Step 1. Remove the clear plastic dust cap from the spray pump tip of the bottle. (See Figure B)
Figure B

Step 2.
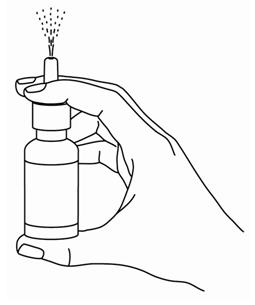
Hold the bottle upright with two fingers on the shoulders of the spray pump unit and put your thumb on the bottom of the bottle. Press upward with your thumb and release for the pumping action.
- Repeat the pumping action until you see a fine mist. You should see a fine mist of the medicine after 6 pumps or less. (See Figure C)
- To get a fine mist of medicine, you must repeat the pumping action fast and use firm pressure against the bottom of the bottle.
- If you see a stream of liquid, the spray will not work right and may cause nasal discomfort.
- If you do not use Dymista Nasal Spray for 14 or more days, you will need to prime the pump with 1 spray or until you see a fine mist. If you do not see a fine mist, clean the tip of the spray nozzle. See the cleaning section below.
- Once you see the fine mist of medicine, your Dymista Nasal Spray pump is ready for use.
Figure C
To Use Dymista Nasal Spray:
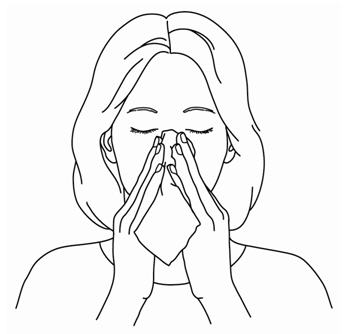
Step 3.
Gently blow your nose to clear nostrils. (See Figure D)
Figure D
Step 4.
Shake the bottle gently. Close 1 nostril with a finger. Tilt your head forward slightly. Keep the bottle upright and carefully place the spray pump tip ¼ to ½ inch into your other nostril. (See Figure E)
Figure E

Step 5.
For each spray firmly press the pump 1 time. Keep your head tilted down and at the same time, gently breathe in through your nostril. (See Figure F) Do not spray directly onto the nasal septum (the wall between your 2 nostrils).
- Repeat Step 5 in your other nostril.
- Do not tilt your head back. This will help to keep the medicine from going into your throat.
- If the medicine goes into your throat you may get a bitter taste in your mouth. This is normal.
Figure F

Step 6.
When you finish using Dymista Nasal Spray, wipe the spray tip with a clean tissue or cloth. Put the dust cap back on the spray pump tip of the bottle. (See Figure G)
Figure G

Each bottle of Dymista Nasal Spray contains enough medicine for you to spray medicine from the bottle 120 times. After initial priming, do not use your bottle of Dymista Nasal Spray after 120 sprays. You may not receive the right amount of medicine. Keep track of the number of sprays you use from your bottle of Dymista Nasal Spray and throw away the bottle even if it has medicine left in it. Do not count any sprays used for initially priming the bottle.
To Clean the Spray Pump Tip:
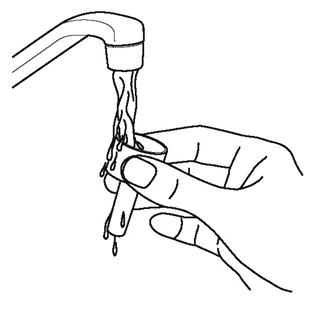
Your Dymista Nasal Spray should be cleaned at least 1 time each week. To do this:
Step 7.
Remove the dust cap and then gently pull upward on the spray pump unit to remove it from the bottle. (See Figure H)
Figure H

Step 8.
Wash the spray pump unit and dust cap in warm tap water. (See Figure I)
Figure I
Step 9.
Allow to dry completely. When dry, place the spray pump unit and dust cap back on the bottle. (See Figure J)
Figure J

Step 10.
If the spray pump unit becomes blocked, it can be removed as instructed above in Step 7 and placed in warm water to soak.
Do not try to unblock the spray pump unit by inserting a pin or other sharp object. This will damage the spray pump unit and cause you not to get the right dose of medicine.
Step 11.
After the spray pump unit is unblocked, rinse the applicator and cap with cold water, and allow them to dry as in Step 10 above. When dry, place the spray pump unit back on the bottle and put the dust cap on the spray pump tip.
Step 12.
Reprime the bottle as in Steps 1 and 2 above. Replace the dust cap and your Dymista Nasal Spray is ready for use.
This Patient Package Insert and Instructions for Use has been approved by the U.S. Food and Drug Administration.
Distributed by:
MEDA PHARMACEUTICALS®
Meda Pharmaceuticals Inc.
Somerset, New Jersey 08873-4120
©2012 Meda Pharmaceuticals Inc.
Dymista is a trademark of Meda Pharmaceuticals Inc.
U.S. Patents 8,163,723; 8,168,620
IN-023A6-03 Rev. 9/2012
| DYMISTA
azelastine hydrochloride and fluticasone propionate spray, metered |
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
| Labeler - Meda Pharmaceuticals Inc. (051229602) |