AVANDARYL - rosiglitazone maleate and glimepiride tablet, film coated
Physicians Total Care, Inc.
----------
HIGHLIGHTS OF PRESCRIBING INFORMATIONThese highlights do not include all the information needed to use AVANDARYL safely and effectively. See full prescribing information for AVANDARYL.
AVANDARYL (rosiglitazone maleate and glimepiride) Tablets Initial U.S. Approval: 2005 WARNING: CONGESTIVE HEART FAILURE AND MYOCARDIAL INFARCTIONSee full prescribing information for complete boxed warning.
RECENT MAJOR CHANGES
INDICATIONS AND USAGEAVANDARYL is a combination antidiabetic product containing a thiazolidinedione and a sulfonylurea. After consultation with a healthcare professional who has considered and advised the patient of the risks and benefits of rosiglitazone, this drug is indicated as an adjunct to diet and exercise to improve glycemic control when treatment with both rosiglitazone and glimepiride is appropriate in adults with type 2 diabetes who either are: (1)
Other Important Limitations of Use: (1)
DOSAGE AND ADMINISTRATION
DOSAGE FORMS AND STRENGTHSRounded triangular tablets containing rosiglitazone/glimepiride: 4 mg/1 mg, 4 mg/2 mg, 4 mg/4 mg, 8 mg/2 mg, and 8 mg/4 mg (3) (3) CONTRAINDICATIONS
WARNINGS AND PRECAUTIONS
ADVERSE REACTIONSCommon adverse reactions (≥5%) reported in clinical trials for AVANDARYL without regard to causality were headache, hypoglycemia, and nasopharyngitis. (6.1) To report SUSPECTED ADVERSE REACTIONS, contact GlaxoSmithKline at 1-888-825-5249 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. DRUG INTERACTIONS
USE IN SPECIFIC POPULATIONS
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide. Revised: 06/2013 |
FULL PRESCRIBING INFORMATION
WARNING: CONGESTIVE HEART FAILURE AND MYOCARDIAL INFARCTION
- •
- Thiazolidinediones, including rosiglitazone, cause or exacerbate congestive heart failure in some patients [see Warnings and Precautions (5.2)]. After initiation of AVANDARYL, and after dose increases, observe patients carefully for signs and symptoms of heart failure (including excessive, rapid weight gain, dyspnea, and/or edema). If these signs and symptoms develop, the heart failure should be managed according to current standards of care. Furthermore, discontinuation or dose reduction of AVANDARYL must be considered.
- •
- AVANDARYL is not recommended in patients with symptomatic heart failure. Initiation of AVANDARYL in patients with established NYHA Class III or IV heart failure is contraindicated. [See Contraindications (4) and Warnings and Precautions (5.2).]
- •
- A meta-analysis of 52 clinical trials (mean duration 6 months; 16,995 total patients), most of which compared rosiglitazone to placebo, showed rosiglitazone to be associated with an increased risk of myocardial infarction. Three other trials (mean duration 46 months; 14,067 total patients), comparing rosiglitazone to some other approved oral antidiabetic agents or placebo, showed a statistically non-significant increased risk of myocardial infarction, and a statistically non-significant decreased risk of death. There have been no clinical trials directly comparing cardiovascular risk of rosiglitazone and ACTOS® (pioglitazone, another thiazolidinedione), but in a separate trial, pioglitazone (when compared to placebo) did not show an increased risk of myocardial infarction or death. [See Warnings and Precautions (5.3).]
- •
- Because of the potential increased risk of myocardial infarction, AVANDARYL is available only through a restricted distribution program called the AVANDIA-Rosiglitazone Medicines Access Program. Both prescribers and patients need to enroll in the program. To enroll, call 1-800-AVANDIA or visit www.AVANDIA.com. [See Warnings and Precautions (5.4).]
1 INDICATIONS AND USAGE
After consultation with a healthcare professional who has considered and advised the patient of the risks and benefits of rosiglitazone, AVANDARYL® is indicated as an adjunct to diet and exercise to improve glycemic control when treatment with both rosiglitazone and glimepiride is appropriate in adults with type 2 diabetes mellitus who either are:
- •
- already taking rosiglitazone, or
- •
- not already taking rosiglitazone and unable to achieve glycemic control on other diabetes medications and, in consultation with their healthcare provider, have decided not to take pioglitazone (ACTOS®) or pioglitazone-containing products (ACTOSPLUS MET®, ACTOPLUS MET XR®, DUETACT®) for medical reasons.
Other Important Limitations of Use:
- •
- Due to its mechanism of action, rosiglitazone is active only in the presence of endogenous insulin. Therefore, AVANDARYL should not be used in patients with type 1 diabetes or for the treatment of diabetic ketoacidosis.
- •
- Coadministration of AVANDARYL with insulin is not recommended [see Warnings and Precautions (5.2, 5.3)].
2 DOSAGE AND ADMINISTRATION
Prior to prescribing AVANDARYL, refer to Indications and Usage (1) for appropriate patient selection. Only prescribers enrolled in the AVANDIA-Rosiglitazone Medicines Access Program can prescribe AVANDARYL [see Warnings and Precautions (5.4)].
2.1 Starting Dose
The recommended starting dose is 4 mg/1 mg administered once daily with the first meal of the day. For adults already treated with a sulfonylurea or rosiglitazone, a starting dose of 4 mg/2 mg may be considered.
All patients should start the rosiglitazone component of AVANDARYL at the lowest recommended dose. Further increases in the dose of rosiglitazone should be accompanied by careful monitoring for adverse events related to fluid retention [see Boxed Warning and Warnings and Precautions (5.6)].
When switching from combination therapy of rosiglitazone plus glimepiride as separate tablets, the usual starting dose of AVANDARYL is the dose of rosiglitazone and glimepiride already being taken.
2.2 Dose Titration
Dose increases should be individualized according to the glycemic response of the patient. Patients who may be more sensitive to glimepiride [see Warnings and Precautions (5.5)], including the elderly, debilitated, or malnourished, and those with renal, hepatic, or adrenal insufficiency, should be carefully titrated to avoid hypoglycemia. If hypoglycemia occurs during up-titration of the dose or while maintained on therapy, a dosage reduction of the glimepiride component of AVANDARYL may be considered. Increases in the dose of rosiglitazone should be accompanied by careful monitoring for adverse events related to fluid retention [see Boxed Warning and Warnings and Precautions (5.6)].
To switch to AVANDARYL for adults currently treated with rosiglitazone, dose titration of the glimepiride component of AVANDARYL is recommended if patients are not adequately controlled after 1 to 2 weeks. The glimepiride component may be increased in no more than 2 mg increments. After an increase in the dosage of the glimepiride component, dose titration of AVANDARYL is recommended if patients are not adequately controlled after 1 to 2 weeks.
To switch to AVANDARYL for adults currently treated with sulfonylurea, it may take 2 weeks to see a reduction in blood glucose and 2 to 3 months to see the full effect of the rosiglitazone component. Therefore, dose titration of the rosiglitazone component of AVANDARYL is recommended if patients are not adequately controlled after 8 to 12 weeks. Patients should be observed carefully (1 to 2 weeks) for hypoglycemia when being transferred from longer half-life sulfonylureas (e.g., chlorpropamide) to AVANDARYL due to potential overlapping of drug effect. After an increase in the dosage of the rosiglitazone component, dose titration of AVANDARYL is recommended if patients are not adequately controlled after 2 to 3 months.
2.4 Specific Patient Populations
Elderly and Malnourished Patients and Those With Renal, Hepatic, or Adrenal Insufficiency: In elderly, debilitated, or malnourished patients, or in patients with renal, hepatic, or adrenal insufficiency, the starting dose, dose increments, and maintenance dosage of AVANDARYL should be conservative to avoid hypoglycemic reactions. [See Warnings and Precautions (5.5) and Clinical Pharmacology (12.3).]
Hepatic Impairment: Liver enzymes should be measured prior to initiating treatment with AVANDARYL. Therapy with AVANDARYL should not be initiated if the patient exhibits clinical evidence of active liver disease or increased serum transaminase levels (ALT >2.5X upper limit of normal at start of therapy). After initiation of AVANDARYL, liver enzymes should be monitored periodically per the clinical judgment of the healthcare professional. [See Warnings and Precautions (5.8) and Clinical Pharmacology (12.3).]
Pregnancy and Lactation: AVANDARYL should not be used during pregnancy or in nursing mothers.
Pediatric Use: Safety and effectiveness of AVANDARYL in pediatric patients have not been established. AVANDARYL and its components, rosiglitazone and glimepiride, are not recommended for use in pediatric patients.
3 DOSAGE FORMS AND STRENGTHS
Each rounded triangular tablet contains rosiglitazone maleate and glimepiride as follows:
- •
- 4 mg/1 mg – yellow, gsk debossed on one side and 4/1 on the other.
- •
- 4 mg/2 mg – orange, gsk debossed on one side and 4/2 on the other.
- •
- 4 mg/4 mg – pink, gsk debossed on one side and 4/4 on the other.
- •
- 8 mg/2 mg – pale pink, gsk debossed on one side and 8/2 on the other.
- •
- 8 mg/4 mg – red, gsk debossed on one side and 8/4 on the other.
4 CONTRAINDICATIONS
Initiation of AVANDARYL in patients with established New York Heart Association (NYHA) Class III or IV heart failure is contraindicated [see Boxed Warning].
5 WARNINGS AND PRECAUTIONS
5.1 Increased Risk of Cardiovascular Mortality for Sulfonylurea Drugs
The administration of oral hypoglycemic drugs has been reported to be associated with increased cardiovascular mortality as compared to treatment with diet alone or diet plus insulin. This warning is based on the trial conducted by the University Group Diabetes Program (UGDP), a long-term, prospective clinical trial designed to evaluate the effectiveness of glucose-lowering drugs in preventing or delaying vascular complications in patients with non-insulin-dependent diabetes. The trial involved 823 patients who were randomly assigned to one of four treatment groups (Diabetes 1970;19[Suppl. 2]:747-830). UGDP reported that patients treated for 5 to 8 years with diet plus a fixed dose of tolbutamide (1.5 grams per day) had a rate of cardiovascular mortality approximately 2½ times that of patients treated with diet alone. A significant increase in total mortality was not observed, but the use of tolbutamide was discontinued based on the increase in cardiovascular mortality, thus limiting the opportunity for the trial to show an increase in overall mortality. Despite controversy regarding the interpretation of these results, the findings of the UGDP trial provide an adequate basis for this warning. The patient should be informed of the potential risks and advantages of glimepiride-containing tablets and of alternative modes of therapy.
Although only one drug in the sulfonylurea class (tolbutamide) was included in this trial, it is prudent from a safety standpoint to consider that this warning may also apply to other oral hypoglycemic drugs in this class, in view of their close similarities in mode of action and chemical structure.
5.2 Cardiac Failure With Rosiglitazone
Rosiglitazone, like other thiazolidinediones, alone or in combination with other antidiabetic agents, can cause fluid retention, which may exacerbate or lead to heart failure. Patients should be observed for signs and symptoms of heart failure. If these signs and symptoms develop, the heart failure should be managed according to current standards of care. Furthermore, discontinuation or dose reduction of rosiglitazone must be considered [see Boxed Warning].
Patients with congestive heart failure (CHF) NYHA Class I and II treated with rosiglitazone have an increased risk of cardiovascular events. A 52-week, double-blind, placebo-controlled echocardiographic trial was conducted in 224 patients with type 2 diabetes mellitus and NYHA Class I or II CHF (ejection fraction ≤45%) on background antidiabetic and CHF therapy. An independent committee conducted a blinded evaluation of fluid-related events (including congestive heart failure) and cardiovascular hospitalizations according to predefined criteria (adjudication). Separate from the adjudication, other cardiovascular adverse events were reported by investigators. Although no treatment difference in change from baseline of ejection fractions was observed, more cardiovascular adverse events were observed with rosiglitazone treatment compared to placebo during the 52-week trial. (See Table 1.)
|
Events |
Rosiglitazone |
Placebo |
|
N = 110 n (%) |
N = 114 n (%) |
|
|
Adjudicated | ||
|
Cardiovascular deaths |
5 (5%) |
4 (4%) |
|
CHF worsening |
7 (6%) |
4 (4%) |
|
– with overnight hospitalization |
5 (5%) |
4 (4%) |
|
– without overnight hospitalization |
2 (2%) |
0 (0%) |
|
New or worsening edema |
28 (25%) |
10 (9%) |
|
New or worsening dyspnea |
29 (26%) |
19 (17%) |
|
Increases in CHF medication |
36 (33%) |
20 (18%) |
|
Cardiovascular hospitalizationa |
21 (19%) |
15 (13%) |
|
Investigator-reported, non-adjudicated | ||
|
Ischemic adverse events |
10 (9%) |
5 (4%) |
|
– Myocardial infarction |
5 (5%) |
2 (2%) |
|
– Angina |
6 (5%) |
3 (3%) |
aIncludes hospitalization for any cardiovascular reason.
Initiation of AVANDARYL in patients with established NYHA Class III or IV heart failure is contraindicated. AVANDARYL is not recommended in patients with symptomatic heart failure. [See Boxed Warning.]
Patients experiencing acute coronary syndromes have not been studied in controlled clinical trials. In view of the potential for development of heart failure in patients having an acute coronary event, initiation of AVANDARYL is not recommended for patients experiencing an acute coronary event, and discontinuation of AVANDARYL during this acute phase should be considered.
Patients with NYHA Class III and IV cardiac status (with or without CHF) have not been studied in controlled clinical trials. AVANDARYL is not recommended in patients with NYHA Class III and IV cardiac status.
Congestive Heart Failure During Coadministration of Rosiglitazone With Insulin: In trials in which rosiglitazone was added to insulin, rosiglitazone increased the risk of congestive heart failure. Coadministration of rosiglitazone and insulin is not recommended. [See Indications and Usage (1) and Warnings and Precautions (5.3).]
In 7 controlled, randomized, double-blind trials which had durations from 16 to 26 weeks and which were included in a meta-analysis1 [see Warnings and Precautions (5.3)], patients with type 2 diabetes mellitus were randomized to coadministration of rosiglitazone and insulin (N = 1,018) or insulin (N = 815). In these 7 trials, rosiglitazone was added to insulin. These trials included patients with long-standing diabetes (median duration of 12 years) and a high prevalence of pre-existing medical conditions, including peripheral neuropathy, retinopathy, ischemic heart disease, vascular disease, and congestive heart failure. The total number of patients with emergent congestive heart failure was 23 (2.3%) and 8 (1.0%) in the rosiglitazone plus insulin and insulin groups, respectively.
Heart Failure in Observational Studies of Elderly Diabetic Patients Comparing Rosiglitazone to Pioglitazone: Three observational studies2-4 in elderly diabetic patients (age 65 years and older) found that rosiglitazone statistically significantly increased the risk of hospitalized heart failure compared to use of pioglitazone. One other observational study5 in patients with a mean age of 54 years, which also included an analysis in a subpopulation of patients >65 years of age, found no statistically significant increase in emergency department visits or hospitalization for heart failure in patients treated with rosiglitazone compared to pioglitazone in the older subgroup.
5.3 Major Adverse Cardiovascular Events
Cardiovascular adverse events have been evaluated in a meta-analysis of 52 clinical trials, in long-term, prospective, randomized, controlled trials, and in observational studies.
Meta-Analysis of Major Adverse Cardiovascular Events in a Group of 52 Clinical Trials: A meta-analysis was conducted retrospectively to assess cardiovascular adverse events reported across 52 double-blind, randomized, controlled clinical trials (mean duration 6 months).1 These trials had been conducted to assess glucose-lowering efficacy in type 2 diabetes. Prospectively planned adjudication of cardiovascular events did not occur in most of the trials. Some trials were placebo-controlled and some used active oral antidiabetic drugs as controls. Placebo-controlled trials included monotherapy trials (monotherapy with rosiglitazone versus placebo monotherapy) and add-on trials (rosiglitazone or placebo, added to sulfonylurea, metformin, or insulin). Active control trials included monotherapy trials (monotherapy with rosiglitazone versus sulfonylurea or metformin monotherapy) and add-on trials (rosiglitazone plus sulfonylurea or rosiglitazone plus metformin, versus sulfonylurea plus metformin). A total of 16,995 patients were included (10,039 in treatment groups containing rosiglitazone, 6,956 in comparator groups), with 5,167 patient-years of exposure to rosiglitazone and 3,637 patient-years of exposure to comparator. Cardiovascular events occurred more frequently for patients who received rosiglitazone than for patients who received comparators (see Table 2).
|
Eventa |
Rosiglitazone (N=10,039) n (%) |
Comparator (N=6,956) n (%) |
|
MACE (a composite of myocardial infarction, cardiovascular death, or stroke) |
70 (0.7) |
39 (0.6) |
|
Myocardial Infarction |
45 (0.4) |
20 (0.3) |
|
Cardiovascular Death |
17 (0.2) |
9 (0.1) |
|
Stroke |
18 (0.2) |
16 (0.2) |
|
All-cause Death |
29 (0.3) |
17 (0.2) |
a Events are not exclusive: i.e., a patient with a cardiovascular death due to a myocardial infarction would be counted in 4 event categories (myocardial infarction; myocardial infarction, cardiovascular death, or stroke; cardiovascular death; all-cause death).
In this analysis, a statistically significant increased risk of myocardial infarction with rosiglitazone versus pooled comparators was observed. Analyses were performed using a composite of major adverse cardiovascular events (myocardial infarction, stroke, and cardiovascular death), referred to hereafter as MACE. Rosiglitazone had a statistically non-significant increased risk of MACE compared to the pooled comparators. A statistically significant increased risk of myocardial infarction and statistically non-significant increased risk of MACE with rosiglitazone was observed in the placebo-controlled trials. In the active-controlled trials, there was no increased risk of myocardial infarction or MACE. (See Figure 1 and Table 3.)
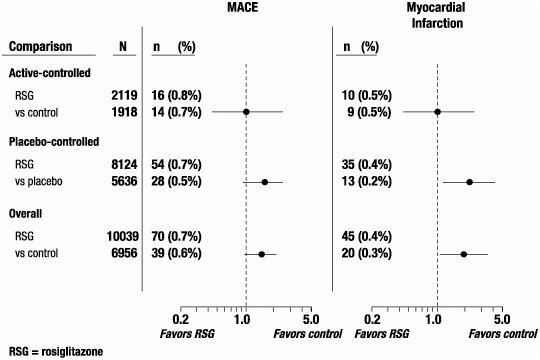
Figure 1. Forest Plot of Odds Ratios (95% Confidence Intervals) for MACE and Myocardial Infarction in the Meta-Analysis of 52 Clinical Trials
|
MACE |
Myocardial Infarction |
|||||
|
N |
n (%) |
OR (95%CI) |
n (%) |
OR (95%CI) |
||
|
Active- Controlled Trials |
RSG |
2,119 |
16 (0.8%) |
1.05 |
10 (0.5%) |
1.00 |
|
Control |
1,918 |
14 (0.7%) |
(0.48, 2.34) |
9 (0.5%) |
(0.36, 2.82) |
|
|
Placebo- Controlled Trials |
RSG |
8,124 |
54 (0.7%) |
1.53 |
35 (0.4%) |
2.23 |
|
Placebo |
5,636 |
28 (0.5%) |
(0.94, 2.54) |
13 (0.2%) |
(1.14, 4.64) |
|
|
Overall |
RSG |
10,039 |
70 (0.7%) |
1.44 |
45 (0.4%) |
1.8 |
|
Control |
6,956 |
39 (0.6%) |
(0.95, 2.20) |
20 (0.3%) |
(1.03, 3.25) |
|
RSG = rosiglitazone
Of the placebo-controlled trials in the meta-analysis, 7 trials had patients randomized to rosiglitazone plus insulin or insulin. There were more patients in the rosiglitazone plus insulin group compared to the insulin group with myocardial infarctions, MACE, cardiovascular deaths, and all-cause deaths (see Table 4). The total number of patients with stroke was 5 (0.5%) and 4 (0.5%) in the rosiglitazone plus insulin and insulin groups, respectively. The use of rosiglitazone in combination with insulin may increase the risk of myocardial infarction [See Warnings and Precautions (5.1).]
|
Eventa |
Rosiglitazone (N=1,018) (%) |
Insulin (N = 815) (%) |
OR (95% CI) |
|
MACE (a composite of myocardial infarction, cardiovascular death, or stroke) |
1.3 |
0.6 |
2.14 (0.70, 7.83) |
|
Myocardial infarction |
0.6 |
0.1 |
5.6 (0.67, 262.7) |
|
Cardiovascular death |
0.4 |
0.0 |
ND, (0.47, ∞) |
|
All-cause death |
0.6 |
0.2 |
2.19 (0.38, 22.61) |
ND = not defined
a Events are not exclusive: i.e., a patient with a cardiovascular death due to a myocardial infarction would be counted in 4 event categories (myocardial infarction; myocardial infarction, cardiovascular death, or stroke; cardiovascular death; all-cause death).
Myocardial Infarction Events in Large, Long-Term, Prospective, Randomized, Controlled Trials of Rosiglitazone: Data from 3 large, long-term, prospective, randomized, controlled clinical trials of rosiglitazone were assessed separately from the meta-analysis.6-8 These 3 trials included a total of 14,067 patients (treatment groups containing rosiglitazone N = 6,311; comparator groups N = 7,756), with patient-year exposure of 24,534 patient-years for rosiglitazone and 28,882 patient-years for comparator. Patient populations in the trials included patients with impaired glucose tolerance, patients with type 2 diabetes who were initiating oral agent monotherapy, and patients with type 2 diabetes who had failed monotherapy and were initiating dual oral agent therapy. Duration of follow-up exceeded 3 years in each trial.
In each of these trials, there was a statistically non-significant increase in the risk of myocardial infarction for rosiglitazone versus comparator medications.
In a long-term, randomized, placebo-controlled, 2x2 factorial trial intended to evaluate rosiglitazone, and separately ramipril (an angiotensin converting enzyme inhibitor [ACEI]), on progression to overt diabetes in 5,269 subjects with glucose intolerance, the incidence of myocardial infarction was higher in the subset of subjects who received rosiglitazone in combination with ramipril than among subjects who received ramipril alone but not in the subset of subjects who received rosiglitazone alone compared to placebo.6 The higher incidence of myocardial infarction among subjects who received rosiglitazone in combination with ramipril was not confirmed in the two other large (total N = 8,798) long-term, randomized, active-controlled clinical trials conducted in patients with type 2 diabetes, in which 30% and 40% of patients in the two trials reported angiotensin-converting enzyme inhibitor use at baseline.7,8
There have been no adequately designed clinical trials directly comparing rosiglitazone to pioglitazone on cardiovascular risks. However, in a long-term, randomized, placebo-controlled cardiovascular outcomes trial comparing pioglitazone to placebo in patients with type 2 diabetes mellitus and prior macrovascular disease, pioglitazone was not associated with an increased risk of myocardial infarction or total mortality.9
The increased risk of myocardial infarction observed in the meta-analysis and large, long-term controlled clinical trials, and the increased risk of MACE observed in the meta-analysis described above, have not translated into a consistent finding of excess mortality from controlled clinical trials or observational studies. Clinical trials have not shown any difference between rosiglitazone and comparator medications in overall mortality or CV-related mortality.
Mortality in Observational Studies of Rosiglitazone Compared to Pioglitazone: Three observational studies in elderly diabetic patients (age 65 years and older) found that rosiglitazone statistically significantly increased the risk of all-cause mortality compared to use of ACTOS (pioglitazone).2-4 One observational study5 in patients with a mean age of 54 years found no difference in all-cause mortality between patients treated with rosiglitazone compared to ACTOS (pioglitazone) and reported similar results in the subpopulation of patients >65 years of age. One additional small, prospective, observational study10 found no statistically significant differences for CV mortality and all-cause mortality in patients treated with rosiglitazone compared to ACTOS (pioglitazone).
5.4 Rosiglitazone REMS (Risk Evaluation and Mitigation Strategy) Program
Because of the potential increased risk of myocardial infarction, AVANDARYL is available only through a restricted distribution program called the AVANDIA-Rosiglitazone Medicines Access Program [see Indications and Usage (1)]. Both prescribers and patients must enroll in the program to be able to prescribe or receive AVANDARYL, respectively. AVANDARYL will be available only from specially certified pharmacies participating in the program. As part of the program, prescribers will be educated about the potential increased risk of myocardial infarction and the need to limit the use of AVANDARYL to eligible patients. Prescribers will need to discuss with patients the risks and benefits of taking AVANDARYL. To enroll, call 1-800-AVANDIA or visit www.AVANDIA.com.
5.5 Hypoglycemia
AVANDARYL is a combination tablet containing rosiglitazone and glimepiride, a sulfonylurea. All sulfonylurea drugs are capable of producing severe hypoglycemia. Proper patient selection, dosage, and instructions are important to avoid hypoglycemic episodes. Elderly patients are particularly susceptible to hypoglycemic action of glucose-lowering drugs. Debilitated or malnourished patients, and those with adrenal, pituitary, renal, or hepatic insufficiency are particularly susceptible to the hypoglycemic action of glucose-lowering drugs. A starting dose of 1 mg glimepiride, as contained in AVANDARYL 4 mg/1 mg, followed by appropriate dose titration is recommended in these patients. [See Clinical Pharmacology (12.3).] Hypoglycemia may be difficult to recognize in the elderly and in people who are taking beta-adrenergic blocking drugs or other sympatholytic agents. Hypoglycemia is more likely to occur when caloric intake is deficient, after severe or prolonged exercise, when alcohol is ingested, or when more than one glucose-lowering drug is used.
Patients receiving rosiglitazone in combination with a sulfonylurea may be at risk for hypoglycemia, and a reduction in the dose of the sulfonylurea may be necessary [see Dosage and Administration (2.2)].
5.6 Edema
AVANDARYL should be used with caution in patients with edema. In a clinical trial in healthy volunteers who received 8 mg of rosiglitazone once daily for 8 weeks, there was a statistically significant increase in median plasma volume compared to placebo.
Since thiazolidinediones, including rosiglitazone, can cause fluid retention, which can exacerbate or lead to congestive heart failure, AVANDARYL should be used with caution in patients at risk for heart failure. Patients should be monitored for signs and symptoms of heart failure [see Boxed Warning, Warnings and Precautions (5.2), and Patient Counseling Information (17.1)].
In controlled clinical trials of patients with type 2 diabetes, mild to moderate edema was reported in patients treated with rosiglitazone, and may be dose-related. Patients with ongoing edema were more likely to have adverse events associated with edema if started on combination therapy with insulin and rosiglitazone [see Adverse Reactions (6.1)]. The use of AVANDARYL in combination with insulin is not recommended[see Warnings and Precautions (5.2, 5.3)].
5.7 Weight Gain
Dose-related weight gain was seen with AVANDARYL, rosiglitazone alone, and rosiglitazone together with other hypoglycemic agents (see Table 5). The mechanism of weight gain is unclear but probably involves a combination of fluid retention and fat accumulation.
|
Monotherapy |
||||
|
Duration |
Control Group |
Rosiglitazone 4 mg |
Rosiglitazone 8 mg |
|
|
26 weeks |
Placebo |
-0.9 (-2.8, 0.9) N = 210 |
1.0 (-0.9, 3.6) N = 436 |
3.1 (1.1, 5.8) N = 439 |
|
52 weeks |
Sulfonylurea |
2.0 (0, 4.0) N = 173 |
2.0 (-0.6, 4.0) N = 150 |
2.6 (0, 5.3) N = 157 |
|
Combination Therapy |
||||
|
Rosiglitazone + Control Therapy |
||||
|
Duration |
Control Group |
Rosiglitazone 4 mg |
Rosiglitazone 8 mg |
|
|
24-26 weeks |
Sulfonylurea |
0 (-1.0, 1.3) N = 1,155 |
2.2 (0.5, 4.0) N = 613 |
3.5 (1.4, 5.9) N = 841 |
|
26 weeks |
Metformin |
-1.4 (-3.2, 0.2) N = 175 |
0.8 (-1.0, 2.6) N = 100 |
2.1 (0, 4.3) N = 184 |
|
26 weeks |
Insulin |
0.9 (-0.5, 2.7) N = 162 |
4.1 (1.4, 6.3) N = 164 |
5.4 (3.4, 7.3) N = 150 |
In a 4- to 6-year, monotherapy, comparative trial (ADOPT) in patients recently diagnosed with type 2 diabetes not previously treated with antidiabetic medication, the median weight change (25th, 75th percentiles) from baseline at 4 years was 3.5 kg (0.0, 8.1) for rosiglitazone, 2.0 kg (-1.0, 4.8) for glyburide, and -2.4 kg (-5.4, 0.5) for metformin.
In postmarketing experience with rosiglitazone alone or in combination with other hypoglycemic agents, there have been rare reports of unusually rapid increases in weight and increases in excess of that generally observed in clinical trials. Patients who experience such increases should be assessed for fluid accumulation and volume-related events such as excessive edema and congestive heart failure [see Boxed Warning].
5.8 Hepatic Effects
With sulfonylureas, including glimepiride, there may be an elevation of liver enzyme levels in rare cases. In isolated instances, impairment of liver function (e.g., with cholestasis and jaundice), as well as hepatitis (which may also lead to liver failure) have been reported.
Liver enzymes should be measured prior to the initiation of therapy with AVANDARYL in all patients and periodically thereafter per the clinical judgment of the healthcare professional. Therapy with AVANDARYL should not be initiated in patients with increased baseline liver enzyme levels (ALT >2.5X upper limit of normal). Patients with mildly elevated liver enzymes (ALT levels ≤2.5X upper limit of normal) at baseline or during therapy with AVANDARYL should be evaluated to determine the cause of the liver enzyme elevation. Initiation of, or continuation of, therapy with AVANDARYL in patients with mild liver enzyme elevations should proceed with caution and include close clinical follow-up, including more frequent liver enzyme monitoring, to determine if the liver enzyme elevations resolve or worsen. If at any time ALT levels increase to >3X the upper limit of normal in patients on therapy with AVANDARYL, liver enzyme levels should be rechecked as soon as possible. If ALT levels remain >3X the upper limit of normal, therapy with AVANDARYL should be discontinued.
If any patient develops symptoms suggesting hepatic dysfunction, which may include unexplained nausea, vomiting, abdominal pain, fatigue, anorexia, and/or dark urine, liver enzymes should be checked. The decision whether to continue the patient on therapy with AVANDARYL should be guided by clinical judgment pending laboratory evaluations. If jaundice is observed, drug therapy should be discontinued.
5.9 Macular Edema
Macular edema has been reported in postmarketing experience in some diabetic patients who were taking rosiglitazone or another thiazolidinedione. Some patients presented with blurred vision or decreased visual acuity, but some patients appear to have been diagnosed on routine ophthalmologic examination. Most patients had peripheral edema at the time macular edema was diagnosed. Some patients had improvement in their macular edema after discontinuation of their thiazolidinedione. Patients with diabetes should have regular eye exams by an ophthalmologist, per the Standards of Care of the American Diabetes Association. Additionally, any diabetic who reports any kind of visual symptom should be promptly referred to an ophthalmologist, regardless of the patient’s underlying medications or other physical findings. [See Adverse Reactions (6.3).]
5.10 Fractures
In a 4- to 6-year comparative trial (ADOPT) of glycemic control with monotherapy in drug-naïve patients recently diagnosed with type 2 diabetes mellitus, an increased incidence of bone fracture was noted in female patients taking rosiglitazone. Over the 4- to 6-year period, the incidence of bone fracture in females was 9.3% (60/645) for rosiglitazone versus 3.5% (21/605) for glyburide and 5.1% (30/590) for metformin. This increased incidence was noted after the first year of treatment and persisted during the course of the trial. The majority of the fractures in the women who received rosiglitazone occurred in the upper arm, hand, and foot. These sites of fracture are different from those usually associated with postmenopausal osteoporosis (e.g., hip or spine). Other trials suggest that this risk may also apply to men, although the risk of fracture among women appears higher than that among men. The risk of fracture should be considered in the care of patients treated with rosiglitazone, and attention given to assessing and maintaining bone health according to current standards of care.
5.11 Hematologic Effects
Decreases in hemoglobin and hematocrit occurred in a dose-related fashion in adult patients treated with rosiglitazone [see Adverse Reactions (6.2)]. The observed changes may be related to the increased plasma volume observed with treatment with rosiglitazone.
5.12 Hemolytic Anemia
Treatment of patients with glucose 6-phosphate dehydrogenase (G6PD) deficiency with sulfonylurea agents can lead to hemolytic anemia. Because glimepiride, a component of AVANDARYL, belongs to the class of sulfonylurea agents, caution should be used in patients with G6PD deficiency and a non-sulfonylurea alternative should be considered. In post-marketing experience, hemolytic anemia has also been reported in patients receiving sulfonylureas who did not have known G6PD deficiency [see Adverse Reactions (6.1)].
5.13 Diabetes and Blood Glucose Control
When a patient stabilized on any antidiabetic regimen is exposed to stress such as fever, trauma, infection, or surgery, a temporary loss of glycemic control may occur. At such times, it may be necessary to withhold AVANDARYL and temporarily administer insulin. AVANDARYL may be reinstituted after the acute episode is resolved.
Periodic fasting glucose and HbA1c measurements should be performed to monitor therapeutic response.
5.14 Ovulation
Therapy with rosiglitazone, like other thiazolidinediones, may result in ovulation in some premenopausal anovulatory women. As a result, these patients may be at an increased risk for pregnancy while taking rosiglitazone [see Use in Specific Populations (8.1)]. Thus, adequate contraception in premenopausal women should be recommended. This possible effect has not been specifically investigated in clinical trials; therefore the frequency of this occurrence is not known.
Although hormonal imbalance has been seen in preclinical studies [see Nonclinical Toxicology (13.1)], the clinical significance of this finding is not known. If unexpected menstrual dysfunction occurs, the benefits of continued therapy with AVANDARYL should be reviewed.
6 ADVERSE REACTIONS
6.1 Clinical Trial Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Trials utilizing rosiglitazone in combination with a sulfonylurea provide support for the use of AVANDARYL. Adverse event data from these trials, in addition to adverse events reported with the use of rosiglitazone and glimepiride therapy, are presented below.
Rosiglitazone: The most common adverse experiences with rosiglitazone monotherapy (≥5%) were upper respiratory tract infection, injury, and headache. Overall, the types of adverse experiences reported when rosiglitazone was added to a sulfonylurea were similar to those during monotherapy with rosiglitazone. In controlled combination therapy trials with sulfonylureas, mild to moderate hypoglycemic symptoms, which appear to be dose-related, were reported. Few patients were withdrawn for hypoglycemia (<1%) and few episodes of hypoglycemia were considered to be severe (<1%).
Events of anemia and edema tended to be reported more frequently at higher doses, and were generally mild to moderate in severity and usually did not require discontinuation of treatment with rosiglitazone.
Edema was reported by 4.8% of patients receiving rosiglitazone compared to 1.3% on placebo, and 1.0% on sulfonylurea monotherapy. The reporting rate of edema was higher for rosiglitazone 8 mg added to a sulfonylurea (12.4%) compared to other combinations, with the exception of insulin. Anemia was reported by 1.9% of patients receiving rosiglitazone compared to 0.7% on placebo, 0.6% on sulfonylurea monotherapy, and 2.3% on rosiglitazone in combination with a sulfonylurea. Overall, the types of adverse experiences reported when rosiglitazone was added to a sulfonylurea were similar to those during monotherapy with rosiglitazone.
In 26-week double-blind, fixed-dose trials, edema was reported with higher frequency in the rosiglitazone plus insulin combination trials (insulin, 5.4%; and rosiglitazone in combination with insulin, 14.7%). Reports of new onset or exacerbation of congestive heart failure occurred at rates of 1% for insulin alone, and 2% (4 mg) and 3% (8 mg) for insulin in combination with rosiglitazone [see Boxed Warning and Warnings and Precautions (5.2)]. The use of rosiglitazone in combination with insulin may increase the risk of myocardial infarction [see Warnings and Precautions (5.3)].
Glimepiride: Hypoglycemia: The incidence of hypoglycemia with glimepiride, as documented by blood glucose values <60 mg/dL, ranged from 0.9% to 1.7% in 2 large, well-controlled, 1-year trials. In patients treated with glimepiride in US placebo-controlled trials (N = 746), adverse events, other than hypoglycemia, considered to be possibly or probably related to trial drug that occurred in more than 1% of patients included dizziness (1.7%), asthenia (1.6%), headache (1.5%), and nausea (1.1%).
Gastrointestinal Reactions: Vomiting, gastrointestinal pain, and diarrhea have been reported, but the incidence in placebo-controlled trials was less than 1%. In rare cases, there may be an elevation of liver enzyme levels. In isolated instances, impairment of liver function (e.g., with cholestasis and jaundice), as well as hepatitis, which may also lead to liver failure have been reported with sulfonylureas, including glimepiride.
Dermatologic Reactions: Allergic skin reactions, e.g., pruritus, erythema, urticaria, and morbilliform or maculopapular eruptions, occur in less than 1% of treated patients. These may be transient and may disappear despite continued use of glimepiride. If those hypersensitivity reactions persist or worsen, the drug should be discontinued. Porphyria cutanea tarda, photosensitivity reactions, and allergic vasculitis have been reported with sulfonylureas, including glimepiride.
Hematologic Reactions: Leukopenia, agranulocytosis, thrombocytopenia, hemolytic anemia [see Warnings and Precautions (5.12)], aplastic anemia, and pancytopenia have been reported with sulfonylureas, including glimepiride.
Metabolic Reactions: Hepatic porphyria reactions and disulfiram-like reactions have been reported with sulfonylureas, including glimepiride. Cases of hyponatremia have been reported with glimepiride and all other sulfonylureas, most often in patients who are on other medications or have medical conditions known to cause hyponatremia or increase release of antidiuretic hormone. The syndrome of inappropriate antidiuretic hormone (SIADH) secretion has been reported with certain other sulfonylureas, including glimepiride, and it has been suggested that certain sulfonylureas may augment the peripheral (antidiuretic) action of ADH and/or increase release of ADH.
Other Reactions: Changes in accommodation and/or blurred vision may occur with the use of glimepiride. This is thought to be due to changes in blood glucose, and may be more pronounced when treatment is initiated. This condition is also seen in untreated diabetic patients, and may actually be reduced by treatment. In placebo-controlled trials of glimepiride, the incidence of blurred vision was placebo, 0.7%, and glimepiride, 0.4%.
Human Ophthalmology Data: Ophthalmic examinations were carried out in more than 500 subjects during long-term trials of glimepiride using the methodology of Taylor and West and Laties et al. No significant differences were seen between glimepiride and glyburide in the number of subjects with clinically important changes in visual acuity, intraocular tension, or in any of the 5 lens-related variables examined. Ophthalmic examinations were carried out during long-term trials using the method of Chylack et al. No significant or clinically meaningful differences were seen between glimepiride and glipizide with respect to cataract progression by subjective LOCS II grading and objective image analysis systems, visual acuity, intraocular pressure, and general ophthalmic examination [see Nonclinical Toxicology (13.2)].
Long-Term Trial of Rosiglitazone as Monotherapy: A 4- to 6-year trial (ADOPT) compared the use of rosiglitazone (n = 1,456), glyburide (n = 1,441), and metformin (n = 1,454) as monotherapy in patients recently diagnosed with type 2 diabetes who were not previously treated with antidiabetic medication. Table 6 presents adverse reactions without regard to causality; rates are expressed per 100 patient-years (PY) exposure to account for the differences in exposure to trial medication across the 3 treatment groups.
In ADOPT, fractures were reported in a greater number of women treated with rosiglitazone (9.3%, 2.7/100 patient-years) compared to glyburide (3.5%, 1.3/100 patient-years) or metformin (5.1%, 1.5/100 patient-years). The majority of the fractures in the women who received rosiglitazone were reported in the upper arm, hand, and foot. [See Warnings and Precautions (5.10).] The observed incidence of fractures for male patients was similar among the 3 treatment groups.
|
Rosiglitazone |
Glyburide |
Metformin |
|
|
N = 1,456 |
N = 1,441 |
N = 1,454 |
|
|
PY = 4,954 |
PY = 4,244 |
PY = 4,906 |
|
|
Nasopharyngitis |
6.3 |
6.9 |
6.6 |
|
Back pain |
5.1 |
4.9 |
5.3 |
|
Arthralgia |
5.0 |
4.8 |
4.2 |
|
Hypertension |
4.4 |
6.0 |
6.1 |
|
Upper respiratory tract infection |
4.3 |
5.0 |
4.7 |
|
Hypoglycemia |
2.9 |
13.0 |
3.4 |
|
Diarrhea |
2.5 |
3.2 |
6.8 |
6.2 Laboratory Abnormalities
Rosiglitazone: Hematologic: Decreases in mean hemoglobin and hematocrit occurred in a dose-related fashion in adult patients treated with rosiglitazone (mean decreases in individual trials as much as 1.0 g/dL hemoglobin and as much as 3.3% hematocrit). The changes occurred primarily during the first 3 months following initiation of therapy with rosiglitazone or following a dose increase in rosiglitazone. The time course and magnitude of decreases were similar in patients treated with a combination of rosiglitazone and other hypoglycemic agents or monotherapy with rosiglitazone. White blood cell counts also decreased slightly in adult patients treated with rosiglitazone. Decreases in hematologic parameters may be related to increased plasma volume observed with treatment with rosiglitazone.
Lipids: Changes in serum lipids have been observed following treatment with rosiglitazone in adults [see Clinical Pharmacology (12.2)].
Serum Transaminase Levels: In pre-approval clinical trials in 4,598 patients treated with rosiglitazone encompassing approximately 3,600 patient-years of exposure, there was no evidence of drug-induced hepatotoxicity.
In pre-approval controlled trials, 0.2% of patients treated with rosiglitazone had reversible elevations in ALT >3X the upper limit of normal compared to 0.2% on placebo and 0.5% on active comparators. The ALT elevations in patients treated with rosiglitazone were reversible. Hyperbilirubinemia was found in 0.3% of patients treated with rosiglitazone compared with 0.9% treated with placebo and 1% in patients treated with active comparators. In pre-approval clinical trials, there were no cases of idiosyncratic drug reactions leading to hepatic failure. [See Warnings and Precautions (5.8).]
In the 4- to 6-year ADOPT trial, patients treated with rosiglitazone (4,954 patient-years exposure), glyburide (4,244 patient-years exposure) or metformin (4,906 patient-years exposure) as monotherapy had the same rate of ALT increase to >3X upper limit of normal (0.3 per 100 patient-years exposure).
6.3 Postmarketing Experience
In addition to adverse reactions reported from clinical trials, the events described below have been identified during post-approval use of AVANDARYL or its individual components. Because these events are reported voluntarily from a population of unknown size, it is not possible to reliably estimate their frequency or to always establish a causal relationship to drug exposure.
In patients receiving thiazolidinedione therapy, serious adverse events with or without a fatal outcome, potentially related to volume expansion (e.g., congestive heart failure, pulmonary edema, and pleural effusions) have been reported [see Boxed Warning and Warnings and Precautions (5.2)].
There are postmarketing reports with rosiglitazone of hepatitis, hepatic enzyme elevations to 3 or more times the upper limit of normal, and hepatic failure with and without fatal outcome, although causality has not been established.
There are postmarketing reports with rosiglitazone of rash, pruritus, urticaria, angioedema, anaphylactic reaction, Stevens-Johnson syndrome, and new onset or worsening diabetic macular edema with decreased visual acuity [see Warnings and Precautions (5.9)].
7 DRUG INTERACTIONS
7.1 Drugs Metabolized by Cytochrome P450
An inhibitor of CYP2C8 (e.g., gemfibrozil) may increase the AUC of rosiglitazone and an inducer of CYP2C8 (e.g., rifampin) may decrease the AUC of rosiglitazone. Therefore, if an inhibitor or an inducer of CYP2C8 is started or stopped during treatment with rosiglitazone, changes in diabetes treatment may be needed based upon clinical response. [See Clinical Pharmacology (12.4).]
A potential interaction between oral miconazole and oral hypoglycemic agents leading to severe hypoglycemia has been reported. Whether this interaction also occurs with the IV, topical, or vaginal preparations of miconazole is not known. Potential interactions of glimepiride with other drugs metabolized by cytochrome P450 2C9 also include phenytoin, diclofenac, ibuprofen, naproxen, and mefenamic acid. [See Clinical Pharmacology (12.4).]
7.2 Drugs That Produce Hyperglycemia
Certain drugs tend to produce hyperglycemia and may lead to loss of control. These drugs include the thiazides and other diuretics, corticosteroids, phenothiazines, thyroid products, estrogens, oral contraceptives, phenytoin, nicotinic acid, sympathomimetics, and isoniazid. When these drugs are administered to a patient receiving glimepiride, the patient should be closely observed for loss of control. When these drugs are withdrawn from a patient receiving glimepiride, the patient should be observed closely for hypoglycemia.
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category C.
All pregnancies have a background risk of birth defects, loss, or other adverse outcome regardless of drug exposure. This background risk is increased in pregnancies complicated by hyperglycemia and may be decreased with good metabolic control. It is essential for patients with diabetes or history of gestational diabetes to maintain good metabolic control before conception and throughout pregnancy. Careful monitoring of glucose control is essential in such patients. Most experts recommend that insulin monotherapy be used during pregnancy to maintain blood glucose levels as close to normal as possible. AVANDARYL should not be used during pregnancy.
Human Data: There are no adequate and well-controlled trials with AVANDARYL or its individual components in pregnant women. Rosiglitazone has been reported to cross the human placenta and be detectable in fetal tissue. The clinical significance of these findings is unknown.
Animal Studies: No animal studies have been conducted with AVANDARYL. The following data are based on findings in studies performed with rosiglitazone or glimepiride individually.
Rosiglitazone: There was no effect on implantation or the embryo with rosiglitazone treatment during early pregnancy in rats, but treatment during mid-late gestation was associated with fetal death and growth retardation in both rats and rabbits. Teratogenicity was not observed at doses up to 3 mg/kg in rats and 100 mg/kg in rabbits (approximately 20 and 75 times human AUC at the maximum recommended human daily dose, respectively). Rosiglitazone caused placental pathology in rats (3 mg/kg/day). Treatment of rats during gestation through lactation reduced litter size, neonatal viability, and postnatal growth, with growth retardation reversible after puberty. For effects on the placenta, embryo/fetus, and offspring, the no-effect dose was 0.2 mg/kg/day in rats and 15 mg/kg/day in rabbits. These no-effect levels are approximately 4 times human AUC at the maximum recommended human daily dose. Rosiglitazone reduced the number of uterine implantations and live offspring when juvenile female rats were treated at 40 mg/kg/day from 27 days of age through to sexual maturity (approximately 68 times human AUC at the maximum recommended daily dose). The no-effect level was 2 mg/kg/day (approximately 4 times human AUC at the maximum recommended daily dose). There was no effect on pre- or post-natal survival or growth.
Glimepiride: Glimepiride did not produce teratogenic effects in rats exposed orally up to 4,000 mg/kg body weight (approximately 4,000 times the maximum recommended human dose based on surface area) or in rabbits exposed up to 32 mg/kg body weight (approximately 60 times the maximum recommended human dose based on surface area). Glimepiride has been shown to be associated with intrauterine fetal death in rats when given in doses as low as 50 times the human dose based on surface area and in rabbits when given in doses as low as 0.1 times the human dose based on surface area. This fetotoxicity, observed only at doses inducing maternal hypoglycemia, has been similarly noted with other sulfonylureas, and is believed to be directly related to the pharmacologic (hypoglycemic) action of glimepiride.
In some studies in rats, offspring of dams exposed to high levels of glimepiride during pregnancy and lactation developed skeletal deformities consisting of shortening, thickening, and bending of the humerus during the postnatal period. Significant concentrations of glimepiride were observed in the serum and breast milk of the dams as well as in the serum of the pups. These skeletal deformations were determined to be the result of nursing from mothers exposed to glimepiride. Prolonged severe hypoglycemia (4 to 10 days) has been reported in neonates born to mothers who were receiving a sulfonylurea drug at the time of delivery. This has been reported more frequently with the use of agents with prolonged half-lives.
8.2 Labor and Delivery
The effect of AVANDARYL or its components on labor and delivery in humans is unknown.
8.3 Nursing Mothers
No trials have been conducted with AVANDARYL. It is not known whether rosiglitazone or glimepiride is excreted in human milk. Because many drugs are excreted in human milk, AVANDARYL should not be administered to a nursing woman.
Rosiglitazone: Drug-related material was detected in milk from lactating rats.
Glimepiride: In rat reproduction studies, significant concentrations of glimepiride were observed in the serum and breast milk of the dams, as well as in the serum of the pups. Although it is not known whether glimepiride is excreted in human milk, other sulfonylureas are excreted in human milk.
8.4 Pediatric Use
Safety and effectiveness of AVANDARYL in pediatric patients have not been established. AVANDARYL and its components, rosiglitazone and glimepiride, are not indicated for use in pediatric patients.
8.5 Geriatric Use
Rosiglitazone: Results of the population pharmacokinetic analysis showed that age does not significantly affect the pharmacokinetics of rosiglitazone [see Clinical Pharmacology (12.3)]. Therefore, no dosage adjustments are required for the elderly. In controlled clinical trials, no overall differences in safety and effectiveness between older (≥65 years) and younger (<65 years) patients were observed.
Glimepiride: In US clinical trials of glimepiride, 608 of 1,986 patients were 65 and older. No overall differences in safety or effectiveness were observed between these subjects and younger subjects, but greater sensitivity of some older individuals cannot be ruled out.
Comparison of glimepiride pharmacokinetics in type 2 diabetes patients ≤65 years (N = 49) and those >65 years (N = 42) was performed in a trial using a dosing regimen of 6 mg daily. There were no significant differences in glimepiride pharmacokinetics between the 2 age groups [see Clinical Pharmacology (12.3)].
The drug is known to be substantially excreted by the kidney, and the risk of toxic reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and it may be useful to monitor renal function.
Elderly patients are particularly susceptible to hypoglycemic action of glucose-lowering drugs. In elderly, debilitated, or malnourished patients, or in patients with renal, hepatic or adrenal insufficiency, the starting dose, dose increments, and maintenance dosage should be conservative based upon blood glucose levels prior to and after initiation of treatment to avoid hypoglycemic reactions. Hypoglycemia may be difficult to recognize in the elderly and in people who are taking beta-adrenergic blocking drugs or other sympatholytic agents [see Dosage and Administration (2.4), Warnings and Precautions (5.5), and Clinical Pharmacology (12.3)].
10 OVERDOSAGE
Rosiglitazone: Limited data are available with regard to overdosage in humans. In clinical trials in volunteers, rosiglitazone has been administered at single oral doses of up to 20 mg and was well tolerated. In the event of an overdose, appropriate supportive treatment should be initiated as dictated by the patient’s clinical status.
Glimepiride: Overdosage of sulfonylureas, including glimepiride, can produce hypoglycemia. Mild hypoglycemic symptoms without loss of consciousness or neurologic findings should be treated aggressively with oral glucose and adjustments in drug dosage and/or meal patterns. Close monitoring should continue until the physician is assured that the patient is out of danger. Severe hypoglycemic reactions with coma, seizure, or other neurological impairment occur infrequently, but constitute medical emergencies requiring immediate hospitalization. If hypoglycemic coma is diagnosed or suspected, the patient should be given a rapid IV injection of concentrated (50%) glucose solution. This should be followed by a continuous infusion of a more dilute (10%) glucose solution at a rate that will maintain the blood glucose level above 100 mg/dL. Patients should be closely monitored for a minimum of 24 to 48 hours, because hypoglycemia may recur after apparent clinical recovery.
11 DESCRIPTION
AVANDARYL contains 2 oral antidiabetic drugs used in the management of type 2 diabetes: rosiglitazone maleate and glimepiride.
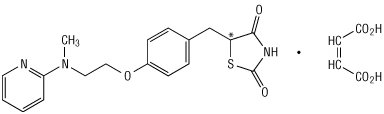
Rosiglitazone maleate is an oral antidiabetic agent which acts primarily by increasing insulin sensitivity. Rosiglitazone maleate is not chemically or functionally related to the sulfonylureas, the biguanides, or the alpha-glucosidase inhibitors. Chemically, rosiglitazone maleate is (±)-5-[[4-[2-(methyl-2-pyridinylamino)ethoxy]phenyl]methyl]-2,4-thiazolidinedione, (Z)-2-butenedioate (1:1) with a molecular weight of 473.52 (357.44 free base). The molecule has a single chiral center and is present as a racemate. Due to rapid interconversion, the enantiomers are functionally indistinguishable. The molecular formula is C18H19N3O3S•C4H4O4. Rosiglitazone maleate is a white to off-white solid with a melting point range of 122° to 123°C. The pKa values of rosiglitazone maleate are 6.8 and 6.1. It is readily soluble in ethanol and a buffered aqueous solution with pH of 2.3; solubility decreases with increasing pH in the physiological range. The structural formula of rosiglitazone maleate is:
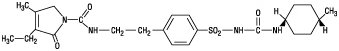
Glimepiride is an oral antidiabetic drug of the sulfonylurea class. Glimepiride is a white to yellowish-white, crystalline, odorless to practically odorless powder. Chemically, glimepiride is 1-[[p-[2-(3-ethyl-4-methyl-2-oxo-3-pyrroline-1-carboxamido)ethyl]phenyl]sulfonyl]-3-(trans-4-methylcyclohexyl)urea with a molecular weight of 490.62. The molecular formula for glimepiride is C24H34N4O5S. Glimepiride is practically insoluble in water. The structural formula of glimepiride is:
AVANDARYL is available for oral administration as tablets containing rosiglitazone maleate and glimepiride, respectively, in the following strengths (expressed as rosiglitazone maleate/glimepiride): 4 mg/1 mg, 4 mg/2 mg, 4 mg/4 mg, 8 mg/2 mg, and 8 mg/4 mg. Each tablet contains the following inactive ingredients: Hypromellose 2910, lactose monohydrate, macrogol (polyethylene glycol), magnesium stearate, microcrystalline cellulose, sodium starch glycolate, titanium dioxide, and 1 or more of the following: Yellow, red, or black iron oxides.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
AVANDARYL combines 2 antidiabetic agents with different mechanisms of action to improve glycemic control in patients with type 2 diabetes: Rosiglitazone maleate, a member of the thiazolidinedione class, and glimepiride, a member of the sulfonylurea class. Thiazolidinediones are insulin-sensitizing agents that act primarily by enhancing peripheral glucose utilization, whereas sulfonylureas act primarily by stimulating release of insulin from functioning pancreatic beta cells.
Rosiglitazone: Rosiglitazone improves glycemic control by improving insulin sensitivity. Rosiglitazone is a highly selective and potent agonist for the peroxisome proliferator-activated receptor-gamma (PPARγ). In humans, PPAR receptors are found in key target tissues for insulin action such as adipose tissue, skeletal muscle, and liver. Activation of PPARγ nuclear receptors regulates the transcription of insulin-responsive genes involved in the control of glucose production, transport, and utilization. In addition, PPARγ-responsive genes also participate in the regulation of fatty acid metabolism.
Insulin resistance is a common feature characterizing the pathogenesis of type 2 diabetes. The antidiabetic activity of rosiglitazone has been demonstrated in animal models of type 2 diabetes in which hyperglycemia and/or impaired glucose tolerance is a consequence of insulin resistance in target tissues. Rosiglitazone reduces blood glucose concentrations and reduces hyperinsulinemia in the ob/ob obese mouse, db/db diabetic mouse, and fa/fa fatty Zucker rat.
In animal models, the antidiabetic activity of rosiglitazone was shown to be mediated by increased sensitivity to insulin’s action in the liver, muscle, and adipose tissues. Pharmacologic studies in animal models indicate that rosiglitazone improves sensitivity to insulin in muscle and adipose tissue and inhibits hepatic gluconeogenesis. The expression of the insulin-regulated glucose transporter GLUT-4 was increased in adipose tissue. Rosiglitazone did not induce hypoglycemia in animal models of type 2 diabetes and/or impaired glucose tolerance.
Glimepiride: The primary mechanism of action of glimepiride in lowering blood glucose appears to be dependent on stimulating the release of insulin from functioning pancreatic beta cells. In addition, extrapancreatic effects may also play a role in the activity of sulfonylureas such as glimepiride. This is supported by both preclinical and clinical trials demonstrating that glimepiride administration can lead to increased sensitivity of peripheral tissues to insulin. These findings are consistent with the results of a long-term, randomized, placebo-controlled trial in which glimepiride therapy improved postprandial insulin/C-peptide responses and overall glycemic control without producing clinically meaningful increases in fasting insulin/C-peptide levels. However, as with other sulfonylureas, the mechanism by which glimepiride lowers blood glucose during long-term administration has not been clearly established.
12.2 Pharmacodynamics
The lipid profiles of rosiglitazone and glimepiride in a clinical trial of patients with inadequate glycemic control on diet and exercise were consistent with the known profile of each monotherapy. AVANDARYL was associated with increases in HDL and LDL (3% to 4% for each) and decreases in triglycerides (-4%), that were not considered to be clinically meaningful.
The pattern of LDL and HDL changes following therapy with rosiglitazone in patients previously treated with a sulfonylurea was generally similar to those seen with rosiglitazone in monotherapy. Rosiglitazone as monotherapy was associated with increases in total cholesterol, LDL, and HDL and decreases in free fatty acids. The changes in triglycerides during therapy with rosiglitazone were variable and were generally not statistically different from placebo or glyburide controls.
12.3 Pharmacokinetics
In a bioequivalence trial of AVANDARYL 4 mg/4 mg, the area under the curve (AUC) and maximum concentration (Cmax) of rosiglitazone following a single dose of the combination tablet were bioequivalent to rosiglitazone 4 mg concomitantly administered with glimepiride 4 mg under fasted conditions. The AUC of glimepiride following a single fasted 4 mg/4 mg dose was equivalent to glimepiride concomitantly administered with rosiglitazone, while the Cmax was 13% lower when administered as the combination tablet (see Table 7).
|
Rosiglitazone |
Glimepiride |
|||
|
Parameter (Units) |
Regimen A |
Regimen B |
Regimen A |
Regimen B |
|
AUC0-inf (ng.hr/mL) |
1,259 (833-2,060) |
1,253 (756-2,758) |
1,052 (643-2,117) |
1,101 (648-2,555) |
|
AUC0-t (ng.hr/mL) |
1,231 (810-2,019) |
1,224 (744-2,654) |
944 (511-1,898) |
1,038 (606-2,337) |
|
Cmax (ng/mL) |
257 (157-352) |
251 (77.3-434) |
151 (63.2-345) |
173 (70.5-329) |
|
T½ (hr) |
3.53 (2.60-4.57) |
3.54 (2.10-5.03) |
7.63 (4.42-12.4) |
5.08 (1.80-11.31) |
|
Tmax (hr) |
1.00 (0.48-3.02) |
0.98 (0.48-5.97) |
3.02 (1.50-8.00) |
2.53 (1.00-8.03) |
AUC = area under the curve; Cmax = maximum concentration; T½ = terminal half-life; Tmax = time of maximum concentration.
Regimen A = AVANDARYL 4 mg/4 mg tablet; Regimen B = Concomitant dosing of a rosiglitazone 4 mg tablet AND a glimepiride 4 mg tablet.
Data presented as geometric mean (range), except T½ which is presented as arithmetic mean (range) and Tmax, which is presented as median (range).
The rate and extent of absorption of both the rosiglitazone component and glimepiride component of AVANDARYL when taken with food were equivalent to the rate and extent of absorption of rosiglitazone and glimepiride when administered concomitantly as separate tablets with food.
Absorption: The AUC and Cmax of glimepiride increased in a dose-proportional manner following administration of AVANDARYL 4 mg/1 mg, 4 mg/2 mg, and 4 mg/4 mg. Administration of AVANDARYL in the fed state resulted in no change in the overall exposure of rosiglitazone; however, the Cmax of rosiglitazone decreased by 32% compared to the fasted state. There was an increase in both AUC (19%) and Cmax (55%) of glimepiride in the fed state compared to the fasted state.
Rosiglitazone: The absolute bioavailability of rosiglitazone is 99%. Peak plasma concentrations are observed about 1 hour after dosing. The Cmax and AUC of rosiglitazone increase in a dose-proportional manner over the therapeutic dose range.
Glimepiride: After oral administration, glimepiride is completely (100%) absorbed from the gastrointestinal tract. Trials with single oral doses in normal subjects and with multiple oral doses in patients with type 2 diabetes have shown significant absorption of glimepiride within 1 hour after administration and Cmax at 2 to 3 hours.
Distribution: Rosiglitazone: The mean (CV%) oral volume of distribution (Vss/F) of rosiglitazone is approximately 17.6 (30%) liters, based on a population pharmacokinetic analysis. Rosiglitazone is approximately 99.8% bound to plasma proteins, primarily albumin.
Glimepiride: After intravenous (IV) dosing in normal subjects, the volume of distribution (Vd) was 8.8 L (113 mL/kg), and the total body clearance (CL) was 47.8 mL/min. Protein binding was greater than 99.5%.
Metabolism and Excretion: Rosiglitazone: Rosiglitazone is extensively metabolized with no unchanged drug excreted in the urine. The major routes of metabolism were N-demethylation and hydroxylation, followed by conjugation with sulfate and glucuronic acid. All the circulating metabolites are considerably less potent than parent and, therefore, are not expected to contribute to the insulin-sensitizing activity of rosiglitazone. In vitro data demonstrate that rosiglitazone is predominantly metabolized by cytochrome P450 (CYP) isoenzyme 2C8, with CYP2C9 contributing as a minor pathway. Following oral or IV administration of [14C]rosiglitazone maleate, approximately 64% and 23% of the dose was eliminated in the urine and in the feces, respectively. The plasma half-life of [14C]related material ranged from 103 to 158 hours. The elimination half-life is 3 to 4 hours and is independent of dose.
Glimepiride: Glimepiride is completely metabolized by oxidative biotransformation after either an IV or oral dose. The major metabolites are the cyclohexyl hydroxy methyl derivative (M1) and the carboxyl derivative (M2). Cytochrome P450 2C9 has been shown to be involved in the biotransformation of glimepiride to M1. M1 is further metabolized to M2 by one or several cytosolic enzymes. M1, but not M2, possesses about ⅓ of the pharmacological activity as compared to its parent in an animal model; however, whether the glucose-lowering effect of M1 is clinically meaningful is not clear.
When [14C]glimepiride was given orally, approximately 60% of the total radioactivity was recovered in the urine in 7 days and M1 (predominant) and M2 accounted for 80 to 90% of that recovered in the urine. Approximately 40% of the total radioactivity was recovered in feces and M1 and M2 (predominant) accounted for about 70% of that recovered in feces. No parent drug was recovered from urine or feces. After IV dosing in patients, no significant biliary excretion of glimepiride or its M1 metabolite has been observed.
Special Populations: No pharmacokinetic data are available for AVANDARYL in the following special populations. Information is provided for the individual components of AVANDARYL.
Gender: Rosiglitazone: Results of the population pharmacokinetics analysis showed that the mean oral clearance of rosiglitazone in female patients (N = 405) was approximately 6% lower compared to male patients of the same body weight (N = 642). Combination therapy with rosiglitazone and sulfonylureas improved glycemic control in both males and females with a greater therapeutic response observed in females. For a given body mass index (BMI), females tend to have a greater fat mass than males. Since the molecular target of rosiglitazone, PPARγ, is expressed in adipose tissues, this differentiating characteristic may account, at least in part, for the greater response to rosiglitazone in combination with sulfonylureas in females. Since therapy should be individualized, no dose adjustments are necessary based on gender alone.
Glimepiride: There were no differences between males and females in the pharmacokinetics of glimepiride when adjustment was made for differences in body weight.
Geriatric: Rosiglitazone: Results of the population pharmacokinetics analysis (N = 716 <65 years; N = 331 ≥65 years) showed that age does not significantly affect the pharmacokinetics of rosiglitazone.
Glimepiride: Comparison of glimepiride pharmacokinetics in type 2 diabetes patients 65 years and younger with those older than 65 years was performed in a trial using a dosing regimen of 6 mg daily. There were no significant differences in glimepiride pharmacokinetics between the 2 age groups. The mean AUC at steady state for the older patients was about 13% lower than that for the younger patients; the mean weight-adjusted clearance for the older patients was about 11% higher than that for the younger patients. [See Use in Specific Populations (8.5).]
Hepatic Impairment: Therapy with AVANDARYL should not be initiated if the patient exhibits clinical evidence of active liver disease or increased serum transaminase levels (ALT >2.5X upper limit of normal) at baseline [see Warnings and Precautions (5.8)].
Rosiglitazone: Unbound oral clearance of rosiglitazone was significantly lower in patients with moderate to severe liver disease (Child-Pugh Class B/C) compared to healthy subjects. As a result, unbound Cmax and AUC0-inf were increased 2- and 3-fold, respectively. Elimination half-life for rosiglitazone was about 2 hours longer in patients with liver disease, compared to healthy subjects.
Glimepiride: No trials of glimepiride have been conducted in patients with hepatic insufficiency.
Race: Rosiglitazone: Results of a population pharmacokinetic analysis including subjects of white, black, and other ethnic origins indicate that race has no influence on the pharmacokinetics of rosiglitazone.
Glimepiride: No pharmacokinetic trials to assess the effects of race have been performed, but in placebo-controlled trials of glimepiride in patients with type 2 diabetes, the antihyperglycemic effect was comparable in whites (N = 536), blacks (N = 63), and Hispanics (N = 63).
Renal Impairment: Rosiglitazone: There are no clinically relevant differences in the pharmacokinetics of rosiglitazone in patients with mild to severe renal impairment or in hemodialysis-dependent patients compared to subjects with normal renal function.
Glimepiride: A single-dose glimepiride, open-label trial was conducted in 15 patients with renal impairment. Glimepiride (3 mg) was administered to 3 groups of patients with different levels of mean creatinine clearance (CLcr); (Group I, CLcr = 77.7 mL/min, N = 5), (Group II, CLcr = 27.7 mL/min, N = 3), and (Group III, CLcr = 9.4 mL/min, N = 7). Glimepiride was found to be well tolerated in all 3 groups. The results showed that glimepiride serum levels decreased as renal function decreased. However, M1 and M2 serum levels (mean AUC values) increased 2.3 and 8.6 times from Group I to Group III. The apparent terminal half-life (T½) for glimepiride did not change, while the half-lives for M1 and M2 increased as renal function decreased. Mean urinary excretion of M1 plus M2 as percent of dose, however, decreased (44.4%, 21.9%, and 9.3% for Groups I to III). A multiple-dose titration trial was also conducted in 16 type 2 diabetes patients with renal impairment using doses ranging from 1 to 8 mg daily for 3 months. The results were consistent with those observed after single doses. All patients with a CLcr less than 22 mL/min had adequate control of their glucose levels with a dosage regimen of only 1 mg daily. The results from this trial suggest that a starting dose of 1 mg glimepiride, as contained in AVANDARYL 4 mg/1 mg, may be given to type 2 diabetes patients with kidney disease, and the dose may be titrated based on fasting glucose levels.
Pediatric: No pharmacokinetic data from trials in pediatric subjects are available for AVANDARYL.
Rosiglitazone: Pharmacokinetic parameters of rosiglitazone in pediatric patients were established using a population pharmacokinetic analysis with sparse data from 96 pediatric patients in a single pediatric clinical trial including 33 males and 63 females with ages ranging from 10 to 17 years (weights ranging from 35 to 178.3 kg). Population mean CL/F and V/F of rosiglitazone were 3.15 L/hr and 13.5 L, respectively. These estimates of CL/F and V/F were consistent with the typical parameter estimates from a prior adult population analysis.
Glimepiride: The pharmacokinetics of glimepiride (1 mg) were evaluated in a single-dose trial conducted in 30 type 2 diabetic patients (male = 7; female = 23) between ages 10 and 17 years. The mean AUC0-last (338.8 ± 203.1 ng.hr/mL), Cmax (102.4 ± 47.7 ng/mL), and T½ (3.1 ± 1.7 hours) were comparable to those previously reported in adults (AUC0-last 315.2 ± 95.9 ng.hr/mL, Cmax 103.2 ± 34.3 ng/mL, and T½ 5.3 ± 4.1 hours).
12.4 Drug-Drug Interactions
Single oral doses of glimepiride in 14 healthy adult subjects had no clinically significant effect on the steady-state pharmacokinetics of rosiglitazone. No clinically significant reductions in glimepiride AUC and Cmax were observed after repeat doses of rosiglitazone (8 mg once daily) for 8 days in healthy adult subjects.
Rosiglitazone: Drugs That Inhibit, Induce or are Metabolized by Cytochrome P450: In vitro drug metabolism studies suggest that rosiglitazone does not inhibit any of the major P450 enzymes at clinically relevant concentrations. In vitro data demonstrate that rosiglitazone is predominantly metabolized by CYP2C8, and to a lesser extent, 2C9. [See Drug Interactions (7.1).]
Rosiglitazone (4 mg twice daily) was shown to have no clinically relevant effect on the pharmacokinetics of nifedipine and oral contraceptives (ethinyl estradiol and norethindrone), which are predominantly metabolized by CYP3A4.
Gemfibrozil: Concomitant administration of gemfibrozil (600 mg twice daily), an inhibitor of CYP2C8, and rosiglitazone (4 mg once daily) for 7 days increased rosiglitazone AUC by 127%, compared to the administration of rosiglitazone (4 mg once daily) alone. Given the potential for dose-related adverse events with rosiglitazone, a decrease in the dose of rosiglitazone may be needed when gemfibrozil is introduced [see Drug Interactions (7.1)].
Rifampin: Rifampin administration (600 mg once a day), an inducer of CYP2C8, for 6 days is reported to decrease rosiglitazone AUC by 66%, compared to the administration of rosiglitazone (8 mg) alone [see Drug Interactions (7.1)].11
Glyburide: Rosiglitazone (2 mg twice daily) taken concomitantly with glyburide (3.75 to 10 mg/day) for 7 days did not alter the mean steady-state 24-hour plasma glucose concentrations in diabetic patients stabilized on glyburide therapy. Repeat doses of rosiglitazone (8 mg once daily) for 8 days in healthy adult Caucasian subjects caused a decrease in glyburide AUC and Cmax of approximately 30%. In Japanese subjects, glyburide AUC and Cmax slightly increased following coadministration of rosiglitazone.
Digoxin: Repeat oral dosing of rosiglitazone (8 mg once daily) for 14 days did not alter the steady-state pharmacokinetics of digoxin (0.375 mg once daily) in healthy volunteers.
Warfarin: Repeat dosing with rosiglitazone had no clinically relevant effect on the steady-state pharmacokinetics of warfarin enantiomers.
Additional pharmacokinetic trials demonstrated no clinically relevant effect of acarbose, ranitidine, or metformin on the pharmacokinetics of rosiglitazone.
Glimepiride: The hypoglycemic action of sulfonylureas may be potentiated by certain drugs, including nonsteroidal anti-inflammatory drugs (NSAIDs) and other drugs that are highly protein bound, such as salicylates, sulfonamides, chloramphenicol, coumarins, probenecid, monoamine oxidase inhibitors, and beta-adrenergic blocking agents. When these drugs are administered to a patient receiving glimepiride, the patient should be observed closely for hypoglycemia. When these drugs are withdrawn from a patient receiving glimepiride, the patient should be observed closely for loss of glycemic control.
Certain drugs tend to produce hyperglycemia and may lead to loss of control. These drugs include the thiazides and other diuretics, corticosteroids, phenothiazines, thyroid products, estrogens, oral contraceptives, phenytoin, nicotinic acid, sympathomimetics, and isoniazid. When these drugs are administered to a patient receiving glimepiride, the patient should be closely observed for loss of control. When these drugs are withdrawn from a patient receiving glimepiride, the patient should be observed closely for hypoglycemia.
Drugs Metabolized by Cytochrome P450: A potential interaction between oral miconazole and oral hypoglycemic agents leading to severe hypoglycemia has been reported. Whether this interaction also occurs with the IV, topical, or vaginal preparations of miconazole is not known. There is a potential interaction of glimepiride with inhibitors (e.g., fluconazole) and inducers (e.g., rifampicin) of cytochrome P450 2C9.
Aspirin: Coadministration of aspirin (1 g three times daily) and glimepiride led to a 34% decrease in the mean glimepiride AUC and, therefore, a 34% increase in the mean CL/F. The mean Cmax had a decrease of 4%. Blood glucose and serum C-peptide concentrations were unaffected and no hypoglycemic symptoms were reported.
H2-Receptor Antagonists: Coadministration of either cimetidine (800 mg once daily) or ranitidine (150 mg twice daily) with a single 4-mg oral dose of glimepiride did not significantly alter the absorption and disposition of glimepiride, and no differences were seen in hypoglycemic symptomatology.
Beta-Blockers: Concomitant administration of propranolol (40 mg three times daily) and glimepiride significantly increased Cmax, AUC, and T½ of glimepiride by 23%, 22%, and 15%, respectively, and it decreased CL/F by 18%. The recovery of M1 and M2 from urine, however, did not change. The pharmacodynamic responses to glimepiride were nearly identical in normal subjects receiving propranolol and placebo. Pooled data from clinical trials in patients with type 2 diabetes showed no evidence of clinically significant adverse interactions with uncontrolled concurrent administration of beta-blockers. However, if beta-blockers are used, caution should be exercised and patients should be warned about the potential for hypoglycemia.
Warfarin: Concomitant administration of glimepiride tablets (4 mg once daily) did not alter the pharmacokinetic characteristics of R- and S-warfarin enantiomers following administration of a single dose (25 mg) of racemic warfarin to healthy subjects. No changes were observed in warfarin plasma protein binding. Glimepiride treatment did result in a slight, but statistically significant, decrease in the pharmacodynamic response to warfarin. The reductions in mean area under the prothrombin time (PT) curve and maximum PT values during glimepiride treatment were very small (3.3% and 9.9%, respectively) and are unlikely to be clinically important.
ACE Inhibitors: The responses of serum glucose, insulin, C-peptide, and plasma glucagon to 2 mg glimepiride were unaffected by coadministration of ramipril (an ACE inhibitor) 5 mg once daily in normal subjects. No hypoglycemic symptoms were reported.
Other: Although no specific interaction trials were performed, pooled data from clinical trials showed no evidence of clinically significant adverse interactions with uncontrolled concurrent administration of aspirin and other salicylates, H2-receptor antagonists, ACE inhibitors, calcium-channel blockers, estrogens, fibrates, NSAIDs, HMG CoA reductase inhibitors, sulfonamides, or thyroid hormone.
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
No animal studies have been conducted with AVANDARYL. The following data are based on findings in studies performed with rosiglitazone or glimepiride alone.
Rosiglitazone: Carcinogenesis: A 2-year carcinogenicity study was conducted in Charles River CD-1 mice at doses of 0.4, 1.5, and 6 mg/kg/day in the diet (highest dose equivalent to approximately 12 times human AUC at the maximum recommended human daily dose). Sprague-Dawley rats were dosed for 2 years by oral gavage at doses of 0.05 mg/kg/day, 0.3 mg/kg/day, and 2 mg/kg/day (highest dose equivalent to approximately 10 and 20 times human AUC at the maximum recommended human daily dose for male and female rats, respectively).
Rosiglitazone was not carcinogenic in the mouse. There was an increase in incidence of adipose hyperplasia in the mouse at doses ≥1.5 mg/kg/day (approximately 2 times human AUC at the maximum recommended human daily dose). In rats, there was a significant increase in the incidence of benign adipose tissue tumors (lipomas) at doses ≥0.3 mg/kg/day (approximately 2 times human AUC at the maximum recommended human daily dose). These proliferative changes in both species are considered due to the persistent pharmacological overstimulation of adipose tissue.
Mutagenesis: Rosiglitazone was not mutagenic or clastogenic in the in vitro bacterial assays for gene mutation, the in vitro chromosome aberration test in human lymphocytes, the in vivo mouse micronucleus test, and the in vivo/in vitro rat UDS assay. There was a small (about 2-fold) increase in mutation in the in vitro mouse lymphoma assay in the presence of metabolic activation.
Impairment of Fertility: Rosiglitazone had no effects on mating or fertility of male rats given up to 40 mg/kg/day (approximately 116 times human AUC at the maximum recommended human daily dose). Rosiglitazone altered estrous cyclicity (2 mg/kg/day) and reduced fertility (40 mg/kg/day) of female rats in association with lower plasma levels of progesterone and estradiol (approximately 20 and 200 times human AUC at the maximum recommended human daily dose, respectively). No such effects were noted at 0.2 mg/kg/day (approximately 3 times human AUC at the maximum recommended human daily dose). In juvenile rats dosed from 27 days of age through to sexual maturity (at up to 40 mg/kg/day), there was no effect on male reproductive performance, or on estrous cyclicity, mating performance or pregnancy incidence in females (approximately 68 times human AUC at the maximum recommended daily dose). In monkeys, rosiglitazone (0.6 and 4.6 mg/kg/day; approximately 3 and 15 times human AUC at the maximum recommended human daily dose, respectively) diminished the follicular phase rise in serum estradiol with consequential reduction in the luteinizing hormone surge, lower luteal phase progesterone levels, and amenorrhea. The mechanism for these effects appears to be direct inhibition of ovarian steroidogenesis.
Glimepiride: Carcinogenesis: Studies in rats at doses of up to 5,000 parts per million (ppm) in complete feed (approximately 340 times the maximum recommended human dose, based on surface area) for 30 months showed no evidence of carcinogenesis. In mice, administration of glimepiride for 24 months resulted in an increase in benign pancreatic adenoma formation which was dose-related and is thought to be the result of chronic pancreatic stimulation. The no-effect dose for adenoma formation in mice in this study was 320 ppm in complete feed, or 46 to 54 mg/kg body weight/day. This is about 35 times the maximum human recommended dose based on surface area.
Mutagenesis: Glimepiride was non-mutagenic in a battery of in vitro and in vivo mutagenicity studies (Ames test, somatic cell mutation, chromosomal aberration, unscheduled DNA synthesis, mouse micronucleus test).
Impairment of Fertility: There was no effect of glimepiride on male mouse fertility in animals exposed up to 2,500 mg/kg body weight (>1,700 times the maximum recommended human dose based on surface area). Glimepiride had no effect on the fertility of male and female rats administered up to 4,000 mg/kg body weight (approximately 4,000 times the maximum recommended human dose based on surface area).
13.2 Animal Toxicology and/or Pharmacology
Rosiglitazone: Heart weights were increased in mice (3 mg/kg/day), rats (5 mg/kg/day), and dogs (2 mg/kg/day) with rosiglitazone treatments (approximately 5, 22, and 2 times human AUC at the maximum recommended human daily dose, respectively). Effects in juvenile rats were consistent with those seen in adults. Morphometric measurement indicated that there was hypertrophy in cardiac ventricular tissues, which may be due to increased heart work as a result of plasma volume expansion.
Glimepiride: Reduced serum glucose values and degranulation of the pancreatic beta cells were observed in beagle dogs exposed to glimepiride 320 mg/kg/day for 12 months (approximately 1,000 times the recommended human dose based on surface area). No evidence of tumor formation was observed in any organ. One female and one male dog developed bilateral subcapsular cataracts. Non-GLP studies indicated that glimepiride was unlikely to exacerbate cataract formation. Evaluation of the co-cataractogenic potential of glimepiride in several diabetic and cataract rat models was negative and there was no adverse effect of glimepiride on bovine ocular lens metabolism in organ culture [see Adverse Reactions (6.1)].
14 CLINICAL STUDIES
The safety and efficacy of rosiglitazone added to a sulfonylurea have been studied in clinical trials in patients with type 2 diabetes inadequately controlled on sulfonylureas alone. No clinical trials have been conducted with the fixed-dose combination of AVANDARYL in patients inadequately controlled on a sulfonylurea or who have initially responded to rosiglitazone alone and require additional glycemic control.
A total of 3,457 patients with type 2 diabetes participated in ten 24- to 26-week randomized, double-blind, placebo/active-controlled trials and one 2-year double-blind, active-controlled trial in elderly patients designed to assess the efficacy and safety of rosiglitazone in combination with a sulfonylurea. Rosiglitazone 2 mg, 4 mg, or 8 mg daily, was administered either once daily (3 trials) or in divided doses twice daily (7 trials), to patients inadequately controlled on a submaximal or maximal dose of sulfonylurea.
In these trials, the combination of rosiglitazone 4 mg or 8 mg daily (administered as single or twice daily divided doses) and a sulfonylurea significantly reduced FPG and HbA1c compared to placebo plus sulfonylurea or further up-titration of the sulfonylurea. Table 8 shows pooled data for 8 trials in which rosiglitazone added to sulfonylurea was compared to placebo plus sulfonylurea.
|
Twice Daily Divided Dosing (5 Trials) |
Sulfonylurea |
Rosiglitazone 2 mg twice daily + sulfonylurea |
Sulfonylurea |
Rosiglitazone 4 mg twice daily + sulfonylurea |
|
N |
397 |
497 |
248 |
346 |
|
FPG (mg/dL) | ||||
|
Baseline (mean) |
204 |
198 |
188 |
187 |
|
Change from baseline (mean) |
11 |
-29 |
8 |
-43 |
|
Difference from sulfonylurea alone (adjusted mean) |
— |
-42a |
— |
-53a |
|
% of patients with ≥30 mg/dL decrease from baseline |
17% |
49% |
15% |
61% |
|
HbA1c (%) | ||||
|
Baseline (mean) |
9.4 |
9.5 |
9.3 |
9.6 |
|
Change from baseline (mean) |
0.2 |
-1.0 |
0.0 |
-1.6 |
|
Difference from sulfonylurea alone (adjusted mean) |
— |
-1.1a |
— |
-1.4a |
|
% of patients with ≥0.7% decrease from baseline |
21% |
60% |
23% |
75% |
|
Once Daily Dosing (3 Trials) |
Sulfonylurea |
Rosiglitazone 4 mg once daily + sulfonylurea |
Sulfonylurea |
Rosiglitazone 8 mg once daily + sulfonylurea |
|
N |
172 |
172 |
173 |
176 |
|
FPG (mg/dL) | ||||
|
Baseline (mean) |
198 |
206 |
188 |
192 |
|
Change from baseline (mean) |
17 |
-25 |
17 |
-43 |
|
Difference from sulfonylurea alone (adjusted mean) |
— |
-47a |
— |
-66a |
|
% of patients with ≥30 mg/dL decrease from baseline |
17% |
48% |
19% |
55% |
|
HbA1c (%) | ||||
|
Baseline (mean) |
8.6 |
8.8 |
8.9 |
8.9 |
|
Change from baseline (mean) |
0.4 |
-0.5 |
0.1 |
-1.2 |
|
Difference from sulfonylurea alone (adjusted mean) |
- |
-0.9a |
- |
-1.4a |
|
% of patients with ≥0.7% decrease from baseline |
11% |
36% |
20% |
68% |
a P <0.0001 compared to sulfonylurea alone.
One of the 24- to 26-week trials included patients who were inadequately controlled on maximal doses of glyburide and switched to 4 mg of rosiglitazone daily as monotherapy; in this group, loss of glycemic control was demonstrated, as evidenced by increases in FPG and HbA1c.
In a 2-year double-blind trial, elderly patients (aged 59 to 89 years) on half-maximal sulfonylurea (glipizide 10 mg twice daily) were randomized to the addition of rosiglitazone (N = 115, 4 mg once daily to 8 mg as needed) or to continued up-titration of glipizide (N = 110), to a maximum of 20 mg twice daily. Mean baseline FPG and HbA1c were 157 mg/dL and 7.72%, respectively, for the rosiglitazone plus glipizide arm and 159 mg/dL and 7.65%, respectively, for the glipizide up-titration arm. Loss of glycemic control (FPG ≥180 mg/dL) occurred in a significantly lower proportion of patients (2%) on rosiglitazone plus glipizide compared to patients in the glipizide up-titration arm (28.7%). About 78% of the patients on combination therapy completed the 2 years of therapy while only 51% completed on glipizide monotherapy. The effect of combination therapy on FPG and HbA1c was durable over the 2-year trial period, with patients achieving a mean of 132 mg/dL for FPG and a mean of 6.98% for HbA1c compared to no change on the glipizide arm.
15 REFERENCES
- 1.
- Food and Drug Administration Briefing Document. Joint meeting of the Endocrinologic and Metabolic Drugs and Drug Safety and Risk Management Advisory Committees. July 13-14, 2010.
- 2.
- Winkelmayer WC, et al. Comparison of cardiovascular outcomes in elderly patients with diabetes who initiated rosiglitazone vs pioglitazone therapy. Arch Intern Med 2008;168(21):2368-2375.
- 3.
- Juurlink DN, et al. Adverse cardiovascular events during treatment with pioglitazone and rosiglitazone: population based cohort study. BMJ 2009; 339.
- 4.
- Graham DJ, et al. Risk of acute myocardial infarction, stroke, heart failure, and death in elderly medicare patients treated with rosiglitazone or pioglitazone. JAMA 2010;304:411-418.
- 5.
- Wertz DA, et al. Risk of cardiovascular events and all-cause mortality in patients with Thiazolidinediones in a managed-care population. Circ CardiovascQual Outcomes 2010;3: 538-545.
- 6.
- DREAM Trial Investigators. Effect of rosiglitazone on the frequency of diabetes in patients with impaired glucose tolerance or impaired fasting glucose: a randomised controlled trial. Lancet 2006;368:1096-1105.
- 7.
- Kahn S, et al. Glycemic durability of rosiglitazone, metformin or glyburide monotherapy. New England Journal of Medicine 2006, 355:2427-2443.
- 8.
- Home P, et al. Rosiglitazone evaluated for cardiovascular outcomes in oral agent combination therapy for type 2 diabetes (RECORD): a multicenter, randomized, open-label trial. Lancet 2009, 373:2125-35.
- 9.
- Dormandy J et al. Secondary prevention of macrovascular events in patients with type 2 diabetes in the PROactive study (Prospective Pioglitazone Clinical Trial in Macrovascular Events): a randomized controlled trial. Lancet 2005, 366:1279-89.
- 10.
- Bilik D, et al. Thiazolidinediones, cardiovascular disease and cardiovascular mortality: translating research into action for diabetes (TRIAD). Pharmocoepidemiol Drug Saf 2010; 19: 715–721.
- 11.
- Park JY, Kim KA, Kang MH, et al. Effect of rifampin on the pharmacokinetics of rosiglitazone in healthy subjects. ClinPharmacolTher 2004;75:157-162.
16 HOW SUPPLIED/STORAGE AND HANDLING
Each rounded triangular tablet contains rosiglitazone as the maleate and glimepiride as follows:
4 mg/1 mg – yellow, gsk debossed on one side and 4/1 on the other.
4 mg/2 mg – orange, gsk debossed on one side and 4/2 on the other.
4 mg/4 mg – pink, gsk debossed on one side and 4/4 on the other.
8 mg/2 mg – pale pink, gsk debossed on one side and 8/2 on the other.
8 mg/4 mg – red, gsk debossed on one side and 8/4 on the other.
4 mg/4 mg bottles of 60: NDC 54868-5739-0
Store at 25°C (77°F); excursions permitted to 15° to 30°C (59° to 86°F). Dispense in a tight, light-resistant container.
17 PATIENT COUNSELING INFORMATION
See Medication Guide.
17.1 Patient Advice
There are multiple medications available to treat type 2 diabetes. The benefits and risks of each available diabetes medication should be taken into account when choosing a particular diabetes medication for a given patient.
Patient should fully understand the risks and benefits of AVANDARYL. AVANDARYL should only be taken by adults with type 2 diabetes who are already taking rosiglitazone, or who are not already taking rosiglitazone and are unable to achieve adequate glycemic control on other diabetes medications, and, in consultation with their healthcare provider, have decided not to take pioglitazone (ACTOS) or pioglitazone-containing medications (ACTOPLUS MET, ACTOPLUS MET XR, DUETACT) for medical reasons. Inform patients that they must be enrolled in the AVANDIA-Rosiglitazone Medicines Access Program in order to receive AVANDARYL.
Patients should be informed of the following:
- •
- AVANDARYL is not recommended in patients with symptomatic heart failure.
- •
- Results of a set of clinical trials suggest that treatment with AVANDARYL is associated with an increased risk for myocardial infarction (heart attack), especially in patients taking insulin. Clinical trials have not shown any difference between rosiglitazone and comparator medications in overall mortality or CV-related mortality.
- •
- AVANDARYL is not recommended for patients who are taking insulin.
- •
- Management of type 2 diabetes should include diet control. Caloric restriction, weight loss, and exercise are essential for the proper treatment of the diabetic patient because they help improve insulin sensitivity. This is important not only in the primary treatment of type 2 diabetes, but also in maintaining the efficacy of drug therapy.
- •
- It is important to adhere to dietary instructions and to regularly have blood glucose and glycosylated hemoglobin (HbA1c) tested. It can take 2 weeks to see a reduction in blood glucose and 2 to 3 months to see the full effect of AVANDARYL.
- •
- The risks of hypoglycemia, its symptoms and treatment, and conditions that predispose to its development should be explained to patients and their family members.
- •
- Blood will be drawn to check their liver function prior to the start of therapy and periodically thereafter per the clinical judgment of the healthcare professional. Patients with unexplained symptoms of nausea, vomiting, abdominal pain, fatigue, anorexia, or dark urine should immediately report these symptoms to their physician.
- •
- Patients who experience an unusually rapid increase in weight or edema or who develop shortness of breath or other symptoms of heart failure while on AVANDARYL should immediately report these symptoms to their physician.
- •
- AVANDARYL should be taken with the first meal of the day.
- •
- Therapy with rosiglitazone, like other thiazolidinediones, may result in ovulation in some premenopausal anovulatory women. As a result, these patients may be at an increased risk for pregnancy while taking AVANDARYL. Thus, adequate contraception in premenopausal women should be recommended. This possible effect has not been specifically investigated in clinical trials so the frequency of this occurrence is not known.
AVANDARYL and AVANDIA are registered trademarks of GlaxoSmithKline. ACTOS, ACTOPLUS MET, ACTOPLUS MET XR, and DUETACT are registered trademarks of Takeda Pharmaceutical Company Limited.
GlaxoSmithKline
Research Triangle Park, NC 27709
©2011, GlaxoSmithKline. All rights reserved.
May 2011
AVR:12PI
MEDICATION GUIDE
AVANDARYL® (ah-VAN-duh-ril)
(rosiglitazone maleate and glimepiride) Tablets
Read this Medication Guide carefully before you start taking AVANDARYL and each time you get a refill. There may be new information. This information does not take the place of talking with your doctor about your medical condition or your treatment. If you have any questions about AVANDARYL, ask your doctor or pharmacist.
What is the most important information I should know about AVANDARYL?
AVANDARYL is available only through the AVANDIA-Rosiglitazone Medicines Access Program. Both you and your doctor must be enrolled in the program so that you can get AVANDARYL. To enroll, you must:
- •
- talk to your doctor,
- •
- understand the risks and benefits of AVANDARYL, and
- •
- agree to enroll in the program.
AVANDARYL may cause serious side effects, including:
New or worse heart failure
- •
- Rosiglitazone, one of the two drugs that make up AVANDARYL, can cause your body to keep extra fluid (fluid retention), which leads to swelling (edema) and weight gain. Extra body fluid can make some heart problems worse or lead to heart failure. Heart failure means your heart does not pump blood well enough.
- •
- If you have severe heart failure, you cannot start AVANDARYL.
- •
- If you have heart failure with symptoms (such as shortness of breath or swelling), even if these symptoms are not severe, AVANDARYL may not be right for you.
Call your doctor right away if you have any of the following:
- •
- swelling or fluid retention, especially in the ankles or legs
- •
- shortness of breath or trouble breathing, especially when you lie down
- •
- an unusually fast increase in weight
- •
- unusual tiredness
Myocardial Infarction (“Heart Attack”)
Rosiglitazone, one of the medicines in AVANDARYL, may raise the risk of heart attack. The risk of having a heart attack may be higher in people who take AVANDARYL with insulin. Most people who take insulin should not also take AVANDARYL.
Symptoms of a heart attack can include the following:
- •
- chest discomfort in the center of your chest that lasts for more than a few minutes, or that goes away or comes back
- •
- chest discomfort that feels like uncomfortable pressure, squeezing, fullness or pain
- •
- pain or discomfort in your arms, back, neck, jaw or stomach
- •
- shortness of breath with or without chest discomfort
- •
- breaking out in a cold sweat
- •
- nausea or vomiting
- •
- feeling lightheaded
Call your doctor or go to the nearest hospital emergency room right away if you think you are having a heart attack.
People with diabetes have a greater risk for heart problems. It is important to work with your doctor to manage other conditions, such as high blood pressure or high cholesterol.
AVANDARYL can have other serious side effects. Be sure to read the section “What are possible side effects of AVANDARYL?”.
What is AVANDARYL?
AVANDARYL contains 2 prescription medicines to treat diabetes, rosiglitazone maleate (AVANDIA) and glimepiride (AMARYL). AVANDARYL is used with diet and exercise to treat certain adults with type 2 (“adult-onset” or “non-insulin dependent”) diabetes mellitus (“high blood sugar”) who are:
- •
- already taking rosiglitazone or rosiglitazone-containing products
- •
- unable to control their blood sugar on other diabetes medicines, and after talking with their doctor have decided not to take pioglitazone (ACTOS) or pioglitazone-containing products (ACTOPLUS MET, ACTOPLUS MET XR, DUETACT)
Glimepiride can help your body release more of its own insulin. Rosiglitazone can help your body respond better to the insulin made in your body and does not cause your body to make more insulin. These medicines can work together to help control your blood sugar.
AVANDARYL is not for people with type 1 diabetes mellitus or to treat a condition called diabetic ketoacidosis.
It is not known if AVANDARYL is safe and effective in children under 18 years old.
Who should not take AVANDARYL?
Many people with heart failure should not start taking AVANDARYL (see “What should I tell my doctor before taking AVANDARYL?”).
What should I tell my doctor before taking AVANDARYL?
Before starting AVANDARYL, ask your doctor about what the choices are for diabetes medicines and what the expected benefits and possible risks are for you in particular.
Before taking AVANDARYL, tell your doctor about all your medical conditions, including if you:
- •
- have heart problems or heart failure.
- •
- have type 1 (“juvenile”) diabetes or had diabetic ketoacidosis. These conditions should be treated with insulin and should not be treated with AVANDARYL.
- •
- have a type of diabetic eye disease called macular edema (swelling of the back of the eye).
- •
- have liver problems. Your doctor should do blood tests to check your liver before you start taking AVANDARYL and during treatment as needed.
- •
- had liver problems while taking REZULIN® (troglitazone), another medicine for diabetes.
- •
- have kidney problems. If people with kidney problems use AVANDARYL, they may need a lower dose of the medication.
- •
- have glucose 6-phosphate dehydrogenase (G6PD) deficiency. This condition runs in families. People with G6PD deficiency who take glimepiride (one of the medicines in AVANDARYL) may develop hemolytic anemia (fast breakdown of red blood cells).
- •
- are pregnant or plan to become pregnant. AVANDARYL should not be used during pregnancy. It is not known if AVANDARYL can harm your unborn baby. You and your doctor should talk about the best way to control your diabetes during pregnancy. If you are a premenopausal woman (before the “change of life”) who does not have regular monthly periods, AVANDARYL may increase your chances of becoming pregnant. Talk to your doctor about birth control choices while taking AVANDARYL. Tell your doctor right away if you become pregnant while taking AVANDARYL.
- •
- are breast-feeding or planning to breast-feed. It is not known if AVANDARYL passes into breast milk. You should not use AVANDARYL while breast-feeding.
Tell your doctor about all the medicines you take including prescription and non-prescription medicines, vitamins or herbal supplements. AVANDARYL and certain other medicines can affect each other and may lead to serious side effects including high or low blood sugar, or heart problems. Especially tell your doctor if you take:
- •
- insulin.
- •
- any medicines for high blood pressure, high cholesterol or heart failure, or for prevention of heart disease or stroke.
Know the medicines you take. Keep a list of all your medicines and show it to your doctor and pharmacist before you start a new medicine. They will tell you if it is alright to take AVANDARYL with other medicines.
How should I take AVANDARYL?
- •
- Take AVANDARYL exactly as prescribed. Your doctor may need to change your dose until your blood sugar is better controlled.
- •
- Take AVANDARYL by mouth one time each day with your first main meal.
- •
- It usually takes a few days for AVANDARYL to start lowering your blood sugar. It may take 2 to 3 months to see the full effect on your blood sugar level.
- •
- If you miss a dose of AVANDARYL, take it as soon as you remember unless it is time to take your next dose. Take your next dose at the usual time. Do not take double doses to make up for a missed dose.
- •
- If you take too much AVANDARYL, call your doctor or poison control center right away.
- •
- Test your blood sugar regularly as your doctor tells you.
- •
- Your doctor should do blood tests to check your liver before you start AVANDARYL and during treatment as needed. Your doctor should also do regular blood sugar tests (for example, “A1c”) to monitor your response to AVANDARYL.
- •
- Call your doctor if you get sick, get injured, get an infection, or have surgery. AVANDARYL may not control your blood sugar levels during these times. Your doctor may need to stop AVANDARYL for a short time and give you insulin to control your blood sugar level.
- •
- Diet and exercise can help your body use its blood sugar better. It is important to stay on your recommended diet, lose extra weight, and get regular exercise while taking AVANDARYL.
What are possible side effects of AVANDARYL?
AVANDARYL may cause serious side effects, including:
- •
- New or worse heart failure. See “What is the most important information I should know about AVANDARYL?”.
- •
- Heart attack. See “What is the most important information I should know about AVANDARYL?”.
- •
- Swelling (edema). AVANDARYL can cause swelling due to fluid retention. See “What is the most important information I should know about AVANDARYL?”.
- •
- Low blood sugar (hypoglycemia). Lightheadedness, dizziness, shakiness or hunger may mean that your blood sugar is too low. This can happen if you skip meals, drink alcohol, use another medicine that lowers blood sugar, exercise (particularly hard or long), or if you have certain medical problems. Call your doctor if low blood sugar levels are a problem for you.
- •
- Weight gain.Rosiglitazone, one of the medicines in AVANDARYL, can cause weight gain that may be due to fluid retention or extra body fat. Weight gain can be a serious problem for people with certain conditions including heart problems. See “What is the most important information I should know about AVANDARYL?”.
- •
-
Liver problems. It is important for your liver to be working normally when you take AVANDARYL. Your doctor should do blood tests to check your liver before you start taking AVANDARYL and during treatment as needed. Call your doctor right away if you have unexplained symptoms such as:
- ∘
- nausea or vomiting
- ∘
- stomach pain
- ∘
- unusual or unexplained tiredness
- ∘
- loss of appetite
- ∘
- dark urine
- ∘
- yellowing of your skin or the whites of your eyes.
- •
- Macular edema (a diabetic eye disease with swelling in the back of the eye). Tell your doctor right away if you have any changes in your vision. Your doctor should check your eyes regularly. Very rarely, some people have had vision changes due to swelling in the back of the eye while taking rosiglitazone, one of the medicines in AVANDARYL.
- •
- Fractures (broken bones), usually in the hand, upper arm or foot. Talk to your doctor for advice on how to keep your bones healthy.
- •
- Low red blood cell count (anemia).
- •
- Ovulation (release of egg from an ovary in women) leading to pregnancy. Ovulation may happen in premenopausal women who do not have regular monthly periods. This can increase the chance of pregnancy. See “What should I tell my doctor before taking AVANDARYL?”.
The most common side effects with AVANDARYL include cold-like symptoms and headache.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store AVANDARYL?
- •
- Store AVANDARYL at room temperature, 59° to 86° F (15° to 30° C). Keep AVANDARYL in the container it comes in. Keep the container closed tightly.
- •
- Safely, throw away AVANDARYL that is out of date or no longer needed.
Keep AVANDARYL and all medicines out of the reach of children.
General information about AVANDARYL
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use AVANDARYL for a condition for which it was not prescribed. Do not give AVANDARYL to other people, even if they have the same symptoms you have. It may harm them.
This Medication Guide summarizes important information about AVANDARYL. If you would like more information, talk with your doctor. You can ask your doctor or pharmacist for information about AVANDARYL that is written for healthcare professionals. You can also find out more about AVANDARYL by calling 1-888-825-5249.
What are the ingredients in AVANDARYL?
Active Ingredients: Rosiglitazone maleate and glimepiride.
Inactive Ingredients: Hypromellose 2910, lactose monohydrate, macrogol (polyethylene glycol), magnesium stearate, microcrystalline cellulose, sodium starch glycolate, titanium dioxide, triacetin, and 1 or more of the following: Yellow, red, or black iron oxides.
Always check to make sure that the medicine you are taking is the correct one. AVANDARYL tablets are triangles with rounded corners and look like this:
4 mg/1 mg – yellow with “gsk” on one side and “4/1” on the other.
4 mg/2 mg – orange with “gsk” on one side and “4/2” on the other.
4 mg/4 mg – pink with “gsk” on one side and “4/4” on the other.
8 mg/2 mg – pale pink with “gsk” on one side and “8/2” on the other.
8 mg/4 mg – red with “gsk” on one side and “8/4” on the other.
AVANDARYL and AVANDIA are registered trademarks of GlaxoSmithKline.
The other brands listed are trademarks of their respective owners and are not trademarks of GlaxoSmithKline. The makers of these brands are not affiliated with and do not endorse GlaxoSmithKline or its products.
This Medication Guide has been approved by the U.S. Food and Drug Administration.
GlaxoSmithKline
Research Triangle Park, NC 27709
©2011, GlaxoSmithKline. All rights reserved.
May 2011
AVR:4MG
Principal Display Panel
Avandaryl®
rosiglitazone maleate 4 mg*
andglimepiride 4 mg
Tablets
once daily
Rx only
Federal Law requires dispensing of AVANDARYL® with the Medication Guide provided with this bottle.
Store at 25oC (77oF); [see USP].
*Each tablet contains rosiglitazone maleate equivalent to 4 mg of rosiglitazone and 4 mg of glimepiride.
Dispense in tight, light-resistant container.
Dosage: See accompanying prescribing information.
| AVANDARYL
rosiglitazone maleate and glimepiride tablet, film coated |
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
| Labeler - Physicians Total Care, Inc. (194123980) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
| Physicians Total Care, Inc. | 194123980 | relabel(54868-5739), repack(54868-5739) | |