BLEOMYCIN
-
bleomycin injection, powder, lyophilized, for solution
Hospira, Inc.
----------
Bleomycin for Injection, USP
Rx only
WARNING
It is recommended that Bleomycin for Injection be administered under the supervision of a qualified physician experienced in the use of cancer chemotherapeutic agents. Appropriate management of therapy and complications is possible only when adequate diagnostic and treatment facilities are readily available.
Pulmonary fibrosis is the most severe toxicity associated with Bleomycin for Injection. The most frequent presentation is pneumonitis occasionally progressing to pulmonary fibrosis. Its occurrence is higher in elderly patients and in those receiving greater than 400 units total dose, but pulmonary toxicity has been observed in young patients and those treated with low doses.
A severe idiosyncratic reaction consisting of hypotension, mental confusion, fever, chills, and wheezing has been reported in approximately 1% of lymphoma patients treated with Bleomycin for Injection.
DESCRIPTION
Bleomycin for Injection, USP is a mixture of cytotoxic glycopeptide antibiotics isolated from a strain of Streptomyces verticillus and is freely soluble in water.
It is available as a lyophilized powder for intramuscular, intravenous or subcutaneous injection. Each vial contains sterile bleomycin sulfate equivalent to 15 units or 30 units of bleomycin. Sulfuric acid or Sodium hydroxide used, if necessary to adjust the pH.
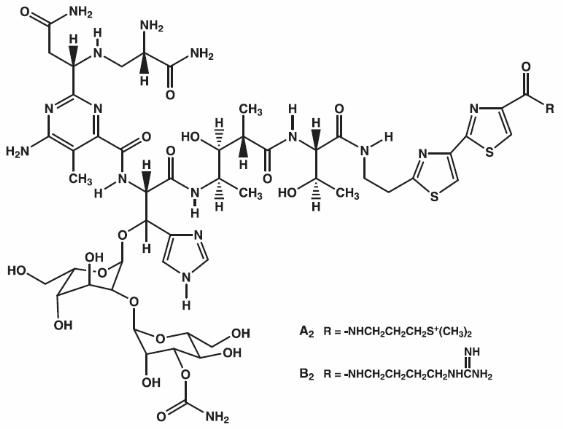
Bleomycins are a group of related basic glycopeptides which differ in the terminal amine substituent of the common structural unit, bleomycin acid. The main components of Bleomycin for Injection are bleomycins A2 and B2. Chemically, bleomycin A2 is N1-[3-(dimethylsulfonio)propyl]-bleomycinamide and bleomycin B2 is N1-[4-(aminoiminomethyl)amino]butyl]-bleomycinamide.
The molecular formula of bleomycin A2 is C55H84N17O21S3 and a calculated molecular weight of 1414. The molecular formula of bleomycin B2 is C55H84N20O21S2 and a calculated molecular weight of 1425. The structural formula of bleomycins A2 and B2 are shown below.
Note: A unit of bleomycin is equal to the formerly used milligram activity. The term milligram activity is a misnomer and was changed to units to be more precise.
CLINICAL PHARMACOLOGY
Although the exact mechanism of action of bleomycin is unknown, available evidence would seem to indicate that the main mode of action is the inhibition of DNA synthesis with some evidence of lesser inhibition of RNA and protein synthesis.
In mice, high concentration of bleomycin are found in the skin, lungs, kidneys, peritoneum, and lymphatics. Tumor cells of the skin and lungs have been found to have high concentrations of bleomycin in contrast to the low concentrations found in hematopoietic tissue. The low concentrations of bleomycin found in bone marrow may be related to high levels of bleomycin degradative enzymes found in that tissue.
In patients with normal renal function, 60% to 70% of an administered dose is recovered in the urine as active bleomycin. In patients with a creatinine clearance of > 35 mL per minute, the serum or plasma terminal elimination half-life of bleomycin is approximately 115 minutes. In patients with a creatinine clearance of < 35 mL per minute, the plasma or serum terminal elimination half-life increases exponentially as the creatinine clearance decreases. It was reported that patients with moderately severe renal failure excreted less than 20% of the dose in the urine. This result would suggest that severe renal impairment could lead to accumulation of the drug in blood.
Information on the dose proportionality of bleomycin is not available.
INDICATIONS AND USAGE
Bleomycin for Injection should be considered a palliative treatment. It has been shown to be useful in the management of the following neoplasms either as a single agent or in proven combinations with other approved chemotherapeutic agents:
Squamous Cell Carcinoma
Head and neck (including mouth, tongue, tonsil, nasopharynx, oropharynx, sinus, palate, lip, buccal mucosa, gingivae, epiglottis, skin, larynx), penis, cervix, and vulva. The response to bleomycin is poorer in patients with previously irradiated head and neck cancer.
Lymphomas
Hodgkin’s Disease, non-Hodgkin’s lymphoma.
Testicular Carcinoma
Embryonal cell, choriocarcinoma, and teratocarcinoma.
CONTRAINDICATIONS
Bleomycin for Injection is contraindicated in patients who have demonstrated a hypersensitive or an idiosyncratic reaction to it.
WARNINGS
Patients receiving bleomycin must be observed carefully and frequently during and after therapy. It should be used with extreme caution in patients with significant impairment of renal function or compromised pulmonary function.
Pulmonary toxicities occur in 10% of treated patients. In approximately 1%, the nonspecific pneumonitis induced by bleomycin progresses to pulmonary fibrosis, and death. Although this is age and dose related, the toxicity is unpredictable. Frequent roentgenograms are recommended (see ADVERSE REACTIONS: Pulmonary).
A severe idiosyncratic reaction (similar to anaphylaxis) consisting of hypotension, mental confusion, fever, chills, and wheezing has been reported in approximately 1% of lymphoma patients treated with bleomycin. Since these reactions usually occur after the first or second dose, careful monitoring is essential after these doses (see ADVERSE REACTIONS: Idiosyncratic Reactions).
Renal or hepatic toxicity, beginning as a deterioration in renal or liver function tests, have been reported, infrequently. These toxicities may occur, however, at any time after initiation of therapy.
Usage in Pregnancy
Pregnancy Category D:
Bleomycin can cause fetal harm when administered to a pregnant woman. It has been shown to be teratogenic in rats. Administration of intraperitoneal doses of 1.5 mg/kg/day to rats (about 1.6 times the recommended human dose on a unit/m2 basis) on days 6-15 of gestation caused skeletal malformations, shortened innominate artery and hydroureter. Bleomycin is abortifacient but not teratogenic in rabbits, at I.V. doses of 1.2 mg/kg/day (about 2.4 times the recommended human dose on a unit/m2 basis) given on gestation days 6-18.
There have been no studies in pregnant women. If Bleomycin for Injection is used during pregnancy, or if the patient becomes pregnant while receiving this drug, the patient should be apprised of the potential hazard to the fetus. Women of child bearing potential should be advised to avoid becoming pregnant during therapy with Bleomycin for Injection.
PRECAUTIONS
General
Bleomycin clearance may be reduced in patients with impaired renal function. No guidelines have been established for dose adjustments, but bleomycin should be used with extreme caution in patients with significant renal impairment.
Carcinogenesis, Mutagenesis, and Impairment of Fertility
The carcinogenic potential of bleomycin in humans is unknown. A study in F344-type male rats demonstrated an increased incidence of nodular hyperplasia after induced lung carcinogenesis by nitrosamines, followed by treatment with bleomycin. In another study where the drug was administered to rats by subcutaneous injection at 0.35 mg/kg weekly (3.82 units/m2 weekly or about 30% at the recommended human dose), necropsy findings included dose related injection site fibrosarcomas as well as various renal tumors. Bleomycin has been shown to be mutagenic both in vitro and in vivo. The effects of bleomycin on fertility have not been studied.
Pregnancy
Pregnancy Category D (see WARNINGS section).
Nursing Mothers
It is not known whether the drug is excreted in human milk. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in nursing infants, it is recommended that nursing be discontinued by women receiving bleomycin therapy.
Pediatric Use
Safety and effectiveness of Bleomycin for Injection in pediatric patients have not been established.
Geriatric Use
In clinical trials, pulmonary toxicity was more common in patients older than 70 years than in younger patients (see BOX WARNING, WARNINGS, and ADVERSE REACTIONS: Pulmonary). Other reported clinical experience has not identified other differences in responses between elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
Bleomycin is known to be substantially excreted by the kidney, and the risk of toxic reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and it may be useful to monitor renal function.
ADVERSE REACTIONS
Pulmonary
This is potentially the most serious side effect, occurring in approximately 10% of treated patients. The most frequent presentation is pneumonitis occasionally progressing to pulmonary fibrosis. Approximately 1% of patients treated have died of pulmonary fibrosis. Pulmonary toxicity is both dose and age related, being more common in patients over 70 years of age and in those receiving over 400 units total dose. This toxicity, however, is unpredictable and has been seen occasionally in young patients receiving low doses.
Some published reports have suggested that the risk of pulmonary toxicity may be increased when bleomycin is used in combination with G-CSF (filgrastim) or other cytokines. However, randomized clinical studies completed to date have not demonstrated an increased risk of pulmonary complications in patients treated with bleomycin and G-CSF.
Because of lack of specificity of the clinical syndrome, the identification of patients with pulmonary toxicity due to bleomycin sulfate has been extremely difficult. The earliest symptom associated with bleomycin sulfate pulmonary toxicity is dyspnea. The earliest sign is fine rales.
Radiographically, bleomycin-induced pneumonitis produces nonspecific patchy opacities, usually of the lower lung fields. The most common changes in pulmonary function tests are a decrease in total lung volume and a decrease in vital capacity. However, these changes are not predictive of the development of pulmonary fibrosis.
The microscopic tissue changes due to bleomycin toxicity include bronchiolar squamous metaplasia, reactive macrophages, atypical alveolar epithelial cells, fibrinous edema, and interstitial fibrosis. The acute stage may involve capillary changes and subsequent fibrinous exudation into alveoli producing a change similar to hyaline membrane formation and progressing to a diffuse interstitial fibrosis resembling the Hamman-Rich syndrome. These microscopic findings are nonspecific; e.g. similar changes are seen in radiation pneumonitis and pneumocystic pneumonitis.
To monitor the onset of pulmonary toxicity, roentgenograms of the chest should be taken every 1 to 2 weeks (see WARNINGS). If pulmonary changes are noted, treatment should be discontinued until it can be determined if they are drug related. Recent studies have suggested that sequential measurement of the pulmonary diffusion capacity for carbon monoxide (DLCO) during treatment with Bleomycin for Injection, USP may be an indicator of subclinical pulmonary toxicity. It is recommended that the DLCO be monitored monthly if it is to be employed to detect pulmonary toxicities, and thus the drug should be discontinued when the DLCO falls below 30% to 35% of the pretreatment value.
Because of bleomycin’s sensitization of lung tissue, patients who have received bleomycin are at greater risk of developing pulmonary toxicity when oxygen is administered in surgery. While long exposure to very high oxygen concentrations is a known cause of lung damage, after bleomycin administration, lung damage can occur at lower concentrations that are usually considered safe.
Suggested preventive measures are:
- Maintain FI 02 at concentrations approximating that of room air (25%) during surgery and the post operative period.
- Monitor carefully fluid replacement, focusing more on colloid administration rather than crystalloid.
Sudden onset of an acute chest pain syndrome suggestive of pleuropericarditis has been rarely reported during Bleomycin for Injection infusions. Although each patient must be individually evaluated, further courses of Bleomycin for Injection do not appear to be contraindicated.
Idiosyncratic Reactions
In approximately 1% of the lymphoma patients treated with Bleomycin for Injection, an idiosyncratic reaction, similar to anaphylaxis clinically, has been reported. The reaction may be immediate or delayed for several hours, and usually occurs after the first or second dose (see WARNINGS). It consists of hypotension, mental confusion, fever, chills and wheezing. Treatment is symptomatic including volume expansion, pressor agents, antihistamines, and corticosteroids.
Integument and Mucous Membranes
These are the most frequent side effects, being reported in approximately 50% of treated patients. These consist of erythema, rash, striae, vesiculation, hyperpigmentation, and tenderness of the skin. Hyperkeratosis, nail changes, alopecia, pruritus, and stomatitis have also been reported. It was necessary to discontinue bleomycin therapy in 2% of treated patients because of these toxicities.
Scleroderma-like skin changes have also been reported as part of postmarketing surveillance.
Skin toxicity is a relatively late manifestation usually developing in the 2nd and 3rd week of treatment after 150 to 200 units of bleomycin have been administered and appears to be related to the cumulative dose.
Other
Vascular toxicities coincident with the use of bleomycin in combination with other antineoplastic agents have been reported rarely. The events are clinically heterogenous and may include myocardial infarction, cerebrovascular accident, thrombotic microangiopathy (HUS) or cerebral arteritis. Various mechanisms have been proposed for these vascular complications. There are also reports of Raynaud’s phenomenon occurring in patients treated with bleomycin in combination with vinblastine with or without cisplatin, or, in a few cases, with bleomycin as a single agent. It is currently unknown if the cause of Raynaud’s phenomenon in these cases is the disease, underlying vascular compromise, bleomycin, vinblastine, hypomagnesemia, or a combination of any of these factors.
Fever, chills and vomiting were frequently reported side effects. Anorexia and weight loss are common and may persist long after termination of this medication. Pain at tumor site, phlebitis, and other local reactions were reported infrequently.
Malaise was also reported as part of postmarketing surveillance.
DOSAGE AND ADMINISTRATION
Because of the possibility of an anaphylactoid reaction, lymphoma patients should be treated with 2 units or less for the first two doses. If no acute reaction occurs, then the regular dosage schedule may be followed.
The following dose schedule is recommended:
Squamous cell carcinoma, non-Hodgkin’s lymphoma, testicular carcinoma - 0.25 to 0.50 units/kg (10 to 20 units/m2) given intravenously, intramuscularly, or subcutaneously weekly or twice weekly.
Hodgkin’s Disease - 0.25 to 0.50 units/kg (10 to 20 units/m2) given intravenously, intramuscularly or subcutaneously weekly or twice weekly. After a 50% response, a maintenance dose of 1 unit daily, or 5 units weekly intravenously or intramuscularly should be given.
Pulmonary toxicity of bleomycin appears to be dose related with a striking increase when the total dose is over 400 units. Total doses over 400 units should be given with great caution.
Note: When Bleomycin for Injection is used in combination with other antineoplastic agents, pulmonary toxicities may occur at lower doses.
Improvement of Hodgkin’s Disease and testicular tumors is prompt and noted within 2 weeks. If no improvement is seen by this time, improvement is unlikely. Squamous cell cancers respond more slowly, sometimes requiring as long as 3 weeks before any improvement is noted.
Administration
Bleomycin for Injection may be given by the intramuscular, intravenous or subcutaneous routes.
Intramuscular or Subcutaneous
The Bleomycin for Injection, USP 15 units vial should be reconstituted and dissolved with 1 to 5 mL of Sterile Water for Injection, Sodium Chloride for Injection, 0.9%, USP, or Bacteriostatic Water for Injection, USP. The Bleomycin for Injection, USP 30 units vial should be reconstituted with 2 to 10 mL of the above diluents.
Intravenous
The contents of the 15 units or 30 units vial should be dissolved in 5 mL or more or 10 mL or more, respectively of Sodium Chloride for Injection, 0.9%, USP and administered slowly over a period of 10 minutes.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
Stability
The sterile powder is stable under refrigeration 2°C (36°F) to 8°C (46°F) and should not be used after the expiration date is reached.
Bleomycin for Injection should not be reconstituted or diluted with 5% Dextrose Injection or other dextrose containing diluents. When reconstituted in 5% Dextrose Injection and analyzed by HPLC, Bleomycin for Injection demonstrates a loss of A2 and B2 potency that does not occur when Bleomycin for Injection is reconstituted in 0.9% sodium chloride.
Bleomycin for Injection, USP is stable for 24 hours at room temperature in Sodium Chloride Injection.
Procedures for proper handling and disposal of anticancer drugs should be considered. Several guidelines on this subject have been published.1-8 There is no general agreement that all of the procedures recommended in the guidelines are necessary or appropriate.
HOW SUPPLIED
Bleomycin for Injection, USP contains sterile bleomycin sulfate equivalent to 15 units or 30 units of bleomycin.
NDC 61703-332-18, 15 units per vial, packaged individually.
NDC 61703-323-22, 30 units per vial, packaged individually.
REFERENCES
- ONS Clinical Practice Committee. Cancer Chemotherapy Guidelines and Recommendations for Practice. Pittsburgh, PS: Oncology Nursing Society; 1999: 32-41.
- Recommendations for the Safe Handling of Parenteral Antineoplastic Drugs. NIH Publication No. 83-2621. For sale by the Superintendent of Documents, US Government Printing Office, Washington, DC 20402.
- AMA Council Report. Guidelines for Handling Parenteral Antineoplastics. JAMA, 1985; 253(11):1590-1592.
- National Study Commission on Cytotoxic Exposure-Recommendations for Handling Cytotoxic Agents. Available from Louis P. Jeffrey, ScD, Chairman, National Study Commission on Cytotoxic Exposure, Massachusetts College of Pharmacy and Allied Health Sciences, 179 Longwood Avenue, Boston, Massachusetts 02115.
- Clinical Oncological Society of Australia: Guidelines and Recommendations for Safe Handling of Antineoplastic Agents. Med J Australia 1983: 1:426-428.
- Jones RB, et al: Safe handling of chemotherapeutic agents: A report from the Mount Sinai Medical Center. CA-A Cancer Journal for Clinicians 1983; (Sept/Oct) 258-263.
- American Society of Hospital Pharmacists Technical Assistance Bulletin on Handling Cytotoxic and Hazardous Drugs. Am J Hosp Pharm 1990; 47: 1033-1049.
- Controlling Occupational Exposure to Hazardous Drugs. (OSHA Work-Practice Guidelines), Am J Health-Syst Pharm, 1996;53: 1669-1685.
Hospira, Inc., Lake Forest, IL 60045 USA
Product of Australia
Revision July 2007
483053
| BLEOMYCIN
bleomycin injection, powder, lyophilized, for solution |
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
| BLEOMYCIN
bleomycin injection, powder, lyophilized, for solution |
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
Revised: 05/2009Hospira, Inc.