JEVTANA- cabazitaxel
Sanofi-Aventis U.S. LLC
----------
HIGHLIGHTS OF PRESCRIBING INFORMATIONThese highlights do not include all the information needed to use JEVTANA safely and effectively. See full prescribing information for JEVTANA.
JEVTANA (cabazitaxel) Injection, 60 mg/1.5 mL, for intravenous infusion only Initial U.S. Approval: 2010 WARNING: NEUTROPENIA AND HYPERSENSITIVITYSee full prescribing information for complete boxed warning.
INDICATIONS AND USAGEJEVTANA is a microtubule inhibitor indicated in combination with prednisone for treatment of patients with hormone-refractory metastatic prostate cancer previously treated with a docetaxel-containing treatment regimen. (1) DOSAGE AND ADMINISTRATIONRecommended dose: JEVTANA 25 mg/m2 administered every three weeks as a one-hour intravenous infusion in combination with oral prednisone 10 mg administered daily throughout JEVTANA treatment. (2.1)
DOSAGE FORMS AND STRENGTHS
CONTRAINDICATIONSWARNINGS AND PRECAUTIONS
ADVERSE REACTIONSMost common all grades adverse reactions (≥10%) are neutropenia, anemia, leukopenia, thrombocytopenia, diarrhea, fatigue, nausea, vomiting, constipation, asthenia, abdominal pain, hematuria, back pain, anorexia, peripheral neuropathy, pyrexia, dyspnea, dysgeusia, cough, arthralgia, and alopecia. (6) To report SUSPECTED ADVERSE REACTIONS, contact sanofi-aventis U.S. LLC at 1-800-633-1610 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. DRUG INTERACTIONS
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling. Revised: 04/2013 |
FULL PRESCRIBING INFORMATION
WARNING : NEUTROPENIA AND HYPERSENSITIVITY
Neutropenic deaths have been reported. In order to monitor the occurrence of neutropenia, frequent blood cell counts should be performed on all patients receiving JEVTANA. JEVTANA should not be given to patients with neutrophil counts of ≤1,500 cells/mm3.
Severe hypersensitivity reactions can occur and may include generalized rash/erythema, hypotension and bronchospasm. Severe hypersensitivity reactions require immediate discontinuation of the JEVTANA infusion and administration of appropriate therapy [see Warnings and Precautions (5.2)]. Patients should receive premedication [see Dosage and Administrations (2.3)]. JEVTANA must not be given to patients who have a history of severe hypersensitivity reactions to JEVTANA or to other drugs formulated with polysorbate 80 [see Contraindications (4)].
1. INDICATIONS AND USAGE
JEVTANA® is a microtubule inhibitor indicated in combination with prednisone for the treatment of patients with hormone-refractory metastatic prostate cancer previously treated with a docetaxel-containing treatment regimen.
2. DOSAGE AND ADMINISTRATION
2.1 General Dosing Information
- The individual dosage of JEVTANA is based on calculation of the Body Surface Area (BSA) and is 25 mg/m2 administered as a one-hour intravenous infusion every three weeks in combination with oral prednisone 10 mg administered daily throughout JEVTANA treatment.
- Premedication is recommended prior to treatment [see Dosage and Administration (2.3)].
- JEVTANA should be administered under the supervision of a qualified physician experienced in the use of antineoplastic medicinal products. Appropriate management of complications is possible only when the adequate diagnostic and treatment facilities are readily available.
- JEVTANA Injection single-use vial requires two dilutions prior to administration [see Dosage and Administration (2.5)].
- Do not use PVC infusion containers and polyurethane infusions sets for preparation and administration of JEVTANA infusion solution [see Dosage and Administration (2.5)].
- Both the JEVTANA Injection and the diluent vials contain an overfill to compensate for liquid loss during preparation.
2.2 Dose Modifications
The JEVTANA dose should be reduced to 20 mg/m2 if patients experience the following adverse reactions.
| Toxicity | Dosage Modification |
|---|---|
| Prolonged grade ≥ 3 neutropenia (greater than 1 week) despite appropriate medication including G-CSF | Delay treatment until neutrophil count is > 1,500 cells/mm3, then reduce dosage of JEVTANA to 20 mg/m2. Use G-CSF for secondary prophylaxis. |
| Febrile neutropenia | Delay treatment until improvement or resolution, and until neutrophil count is > 1,500 cells/mm3, then reduce dosage of JEVTANA to 20 mg/m2. Use G-CSF for secondary prophylaxis. |
| Grade ≥ 3 diarrhea or persisting diarrhea despite appropriate medication, fluid and electrolytes replacement | Delay treatment until improvement or resolution, then reduce dosage of JEVTANA to 20 mg/m2. |
Discontinue JEVTANA treatment if a patient continues to experience any of these reactions at 20 mg/m2.
2.3 Premedication
Premedicate at least 30 minutes prior to each dose of JEVTANA with the following intravenous medications to reduce the risk and/or severity of hypersensitivity:
- antihistamine (dexchlorpheniramine 5 mg, or diphenhydramine 25 mg or equivalent antihistamine),
- corticosteroid (dexamethasone 8 mg or equivalent steroid),
- H2 antagonist (ranitidine 50 mg or equivalent H2 antagonist).
Antiemetic prophylaxis is recommended and can be given orally or intravenously as needed.
2.4 Administration Precautions
JEVTANA is a cytotoxic anticancer drug and caution should be exercised when handling and preparing JEVTANA solutions, taking into account the use of containment devices, personal protective equipment (e.g., gloves), and preparation procedures. Please refer to Handling and Disposal (16.3).
If JEVTANA Injection, first diluted solution, or second (final) dilution for intravenous infusion should come into contact with the skin, immediately and thoroughly wash with soap and water. If JEVTANA Injection, first diluted solution, or second (final) dilution for intravenous infusion should come into contact with mucosa, immediately and thoroughly wash with water.
2.5 Instructions for Preparation
Do not use PVC infusion containers or polyurethane infusions sets for preparation and administration of JEVTANA infusion solution.
Read this entire section carefully before mixing and diluting. JEVTANA requires two dilutions prior to administration. Please follow the preparation instructions provided below. Note: Both the JEVTANA Injection and the diluent vials contain an overfill to compensate for liquid loss during preparation. This overfill ensures that after dilution with the entire contents of the accompanying diluent, there is an initial diluted solution containing 10 mg/mL JEVTANA.
The following two-step dilution process must be carried out under aseptic conditions to prepare the second (final) infusion solution.
Set aside the JEVTANA Injection and supplied diluent vials. The JEVTANA Injection is a clear yellow to brownish-yellow viscous solution, if appropriately stored.
Step 1 – First Dilution
Each vial of JEVTANA (cabazitaxel) 60 mg/1.5 mL must first be mixed with the entire contents of supplied diluent. Once reconstituted, the resultant solution contains 10 mg/mL of JEVTANA.
When transferring the diluent, direct the needle onto the inside wall of JEVTANA vial and inject slowly to limit foaming. Remove the syringe and needle and gently mix the initial diluted solution by repeated inversions for at least 45 seconds to assure full mixing of the drug and diluent. Do not shake.
Let the solution stand for a few minutes to allow any foam to dissipate, and check that the solution is homogeneous and contains no visible particulate matter. It is not required that all foam dissipate prior to continuing the preparation process.
The resulting initial diluted JEVTANA solution (cabazitaxel 10 mg/mL) requires further dilution before administration. The second dilution should be done immediately (within 30 minutes) to obtain the final infusion as detailed in Step 2.
Step 2 – Second (Final) Dilution
Withdraw the recommended dose from the JEVTANA solution containing 10 mg/mL as prepared in Step 1 using a calibrated syringe and further dilute into a sterile 250 mL PVC-free container of either 0.9% sodium chloride solution or 5% dextrose solution for infusion. If a dose greater than 65 mg of JEVTANA is required, use a larger volume of the infusion vehicle so that a concentration of 0.26 mg/mL JEVTANA is not exceeded. The concentration of the JEVTANA final infusion solution should be between 0.10 mg/mL and 0.26 mg/mL.
JEVTANA should not be mixed with any other drugs.
Remove the syringe and thoroughly mix the final infusion solution by gently inverting the bag or bottle.
JEVTANA final infusion solution (in either 0.9% sodium chloride solution or 5% dextrose solution) should be used within 8 hours at ambient temperature (including the one-hour infusion) or within a total of 24 hours if refrigerated (including the one-hour infusion).
As the final infusion solution is supersaturated, it may crystallize over time. Do not use if this occurs and discard.
Inspect visually for particulate matter, any crystals and discoloration prior to administration. If the JEVTANA first diluted solution or second (final) infusion solution is not clear or appears to have precipitation, it should be discarded.
Discard any unused portion.
2.6 Administration
The final JEVTANA infusion solution should be administered intravenously as a one-hour infusion at room temperature.
Use an in-line filter of 0.22 micrometer nominal pore size (also referred to as 0.2 micrometer) during administration.
The final JEVTANA infusion solution should be used immediately. However, in-use storage time can be longer under specific conditions, i.e. 8 hours under ambient conditions (including the one-hour infusion) or for a total of 24 hours if refrigerated (including the one-hour infusion) [see Dosage and Administration (2.5)].
3. DOSAGE FORMS AND STRENGTHS
JEVTANA (cabazitaxel) Injection 60 mg/1.5 mL is supplied as a kit consisting of the following:
- –
- JEVTANA Injection 60 mg/1.5 mL: contains 60 mg cabazitaxel in 1.5 mL polysorbate 80,
- –
- Diluent for JEVTANA Injection 60 mg/1.5 mL: contains approximately 5.7 mL of 13% (w/w) ethanol in water for injection.
4. CONTRAINDICATIONS
JEVTANA should not be used in patients with neutrophil counts of ≤ 1,500/mm3.
JEVTANA is contraindicated in patients who have a history of severe hypersensitivity reactions to cabazitaxel or to other drugs formulated with polysorbate 80.
5. WARNINGS AND PRECAUTIONS
5.1 Neutropenia
Five patients experienced fatal infectious adverse events (sepsis or septic shock). All had grade 4 neutropenia and one had febrile neutropenia. One additional patient's death was attributed to neutropenia without a documented infection.
G-CSF may be administered to reduce the risks of neutropenia complications associated with JEVTANA use. Primary prophylaxis with G-CSF should be considered in patients with high-risk clinical features (age > 65 years, poor performance status, previous episodes of febrile neutropenia, extensive prior radiation ports, poor nutritional status, or other serious comorbidities) that predispose them to increased complications from prolonged neutropenia. Therapeutic use of G-CSF and secondary prophylaxis should be considered in all patients considered to be at increased risk for neutropenia complications.
Monitoring of complete blood counts is essential on a weekly basis during cycle 1 and before each treatment cycle thereafter so that the dose can be adjusted, if needed [see Dosage and Administration (2.2)].
JEVTANA should not be administered to patients with neutrophils ≤ 1,500/mm3 [see Contraindications (4)].
If a patient experiences febrile neutropenia or prolonged neutropenia (greater than one week) despite appropriate medication (e.g., G-CSF), the dose of JEVTANA should be reduced [see Dosage and Administration (2.2)]. Patients can restart treatment with JEVTANA only when neutrophil counts recover to a level > 1,500/mm3 [see Contraindications (4)].
5.2 Hypersensitivity Reactions
All patients should be premedicated prior to the initiation of the infusion of JEVTANA [see Dosage and Administration (2.3)]. Patients should be observed closely for hypersensitivity reactions, especially during the first and second infusions. Hypersensitivity reactions may occur within a few minutes following the initiation of the infusion of JEVTANA, thus facilities and equipment for the treatment of hypotension and bronchospasm should be available. Severe hypersensitivity reactions can occur and may include generalized rash/erythema, hypotension and bronchospasm. Severe hypersensitivity reactions require immediate discontinuation of the JEVTANA infusion and appropriate therapy. Patients with a history of severe hypersensitivity reactions should not be re-challenged with JEVTANA [see Contraindications (4)].
5.3 Gastrointestinal Symptoms
Nausea, vomiting and severe diarrhea, at times, may occur. Death related to diarrhea and electrolyte imbalance occurred in the randomized clinical trial. Intensive measures may be required for severe diarrhea and electrolyte imbalance. Patients should be treated with rehydration, anti-diarrheal or anti-emetic medications as needed. Treatment delay or dosage reduction may be necessary if patients experience Grade ≥ 3 diarrhea [see Dosage and Administration (2.2)].
5.4 Renal Failure
Renal failure, including four cases with fatal outcome, was reported in the randomized clinical trial. Most cases occurred in association with sepsis, dehydration, or obstructive uropathy [see Adverse Reactions (6.1)]. Some deaths due to renal failure did not have a clear etiology. Appropriate measures should be taken to identify causes of renal failure and treat aggressively.
5.5 Elderly Patients
In the randomized clinical trial, 3 of 131 (2%) patients < 65 years of age and 15 of 240 (6%) ≥ 65 years of age died of causes other than disease progression within 30 days of the last cabazitaxel dose. Patients ≥ 65 years of age are more likely to experience certain adverse reactions, including neutropenia and febrile neutropenia [see Adverse Reactions (6) and Use in Specific Populations (8.5)].
5.6 Hepatic Impairment
No dedicated hepatic impairment trial for JEVTANA has been conducted. Patients with impaired hepatic function (total bilirubin ≥ ULN, or AST and/or ALT ≥ 1.5 × ULN) were excluded from the randomized clinical trial.
Cabazitaxel is extensively metabolized in the liver, and hepatic impairment is likely to increase cabazitaxel concentrations.
Hepatic impairment increases the risk of severe and life-threatening complications in patients receiving other drugs belonging to the same class as JEVTANA. JEVTANA should not be given to patients with hepatic impairment (total bilirubin ≥ ULN, or AST and/or ALT ≥ 1.5 × ULN).
5.7 Pregnancy
Pregnancy category D.
JEVTANA can cause fetal harm when administered to a pregnant woman. In non-clinical studies in rats and rabbits, cabazitaxel was embryotoxic, fetotoxic, and abortifacient at exposures significantly lower than those expected at the recommended human dose level.
There are no adequate and well-controlled studies in pregnant women using JEVTANA. If this drug is used during pregnancy, or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to the fetus. Women of childbearing potential should be advised to avoid becoming pregnant during treatment with JEVTANA [see Use in Specific Populations (8.1)].
6. ADVERSE REACTIONS
The following serious adverse reactions are discussed in greater detail in another section of the label:
- Neutropenia [see Warnings and Precautions (5.1)].
- Hypersensitivity Reactions [see Warnings and Precautions (5.2)].
- Gastrointestinal Symptoms [see Warnings and Precautions (5.3)].
- Renal Failure [see Warnings and Precautions (5.4)].
6.1 Clinical Trial Experience
Because clinical trials are conducted under widely varying conditions, the adverse reaction rates observed cannot be directly compared to rates in other trials and may not reflect the rates observed in clinical practice.
The safety of JEVTANA in combination with prednisone was evaluated in 371 patients with hormone-refractory metastatic prostate cancer treated in a single randomized trial, compared to mitoxantrone plus prednisone.
Deaths due to causes other than disease progression within 30 days of last study drug dose were reported in 18 (5%) JEVTANA-treated patients and 3 (< 1%) mitoxantrone-treated patients. The most common fatal adverse reactions in JEVTANA-treated patients were infections (n=5) and renal failure (n=4). The majority (4 of 5 patients) of fatal infection-related adverse reactions occurred after a single dose of JEVTANA. Other fatal adverse reactions in JEVTANA-treated patients included ventricular fibrillation, cerebral hemorrhage, and dyspnea.
The most common (≥ 10%) grade 1–4 adverse reactions were anemia, leukopenia, neutropenia, thrombocytopenia, diarrhea, fatigue, nausea, vomiting, constipation, asthenia, abdominal pain, hematuria, back pain, anorexia, peripheral neuropathy, pyrexia, dyspnea, dysguesia, cough, arthralgia, and alopecia.
The most common (≥ 5%) grade 3–4 adverse reactions in patients who received JEVTANA were neutropenia, leukopenia, anemia, febrile neutropenia, diarrhea, fatigue, and asthenia.
Treatment discontinuations due to adverse drug reactions occurred in 18% of patients who received JEVTANA and 8% of patients who received mitoxantrone. The most common adverse reactions leading to treatment discontinuation in the JEVTANA group were neutropenia and renal failure. Dose reductions were reported in 12% of JEVTANA-treated patients and 4% of mitoxantrone-treated patients. Dose delays were reported in 28% of JEVTANA-treated patients and 15% of mitoxantrone-treated patients.
| JEVTANA 25 mg/m2 every 3 weeks with prednisone 10 mg daily n=371 | Mitoxantrone 12 mg/m2 every 3 weeks with prednisone 10 mg daily n=371 |
|||
|---|---|---|---|---|
| Grade 1–4 n (%) | Grade 3–4 n (%) | Grade 1–4 n (%) | Grade 3–4 n (%) |
|
|
||||
| Any Adverse Reaction | ||||
| Blood and Lymphatic System Disorders | ||||
| Neutropenia† | 347 (94%) | 303 (82%) | 325 (87%) | 215 (58%) |
| Febrile Neutropenia | 27 (7%) | 27 (7%) | 5 (1%) | 5 (1%) |
| Anemia† | 361 (98%) | 39 (11%) | 302 (82%) | 18 (5%) |
| Leukopenia† | 355 (96%) | 253 (69%) | 343 (93%) | 157 (42%) |
| Thrombocytopenia† | 176 (48%) | 15 (4%) | 160 (43%) | 6 (2%) |
| Cardiac Disorders | ||||
| Arrhythmia‡ | 18 (5%) | 4 (1%) | 6 (2%) | 1 (< 1%) |
| Gastrointestinal Disorders | ||||
| Diarrhea | 173 (47%) | 23 (6%) | 39 (11%) | 1 (< 1%) |
| Nausea | 127 (34%) | 7 (2%) | 85 (23%) | 1 (< 1%) |
| Vomiting | 83 (22%) | 6 (2%) | 38 (10%) | 0 |
| Constipation | 76 (20%) | 4 (1%) | 57 (15%) | 2 (< 1%) |
| Abdominal Pain§ | 64 (17%) | 7 (2%) | 23 (6%) | 0 |
| Dyspepsia¶ | 36 (10%) | 0 | 9 (2%) | 0 |
| General Disorders and Administration Site Conditions | ||||
| Fatigue | 136 (37%) | 18 (5%) | 102 (27%) | 11 (3%) |
| Asthenia | 76 (20%) | 17 (5%) | 46 (12%) | 9 (2%) |
| Pyrexia | 45 (12%) | 4 (1%) | 23 (6%) | 1 (< 1%) |
| Peripheral Edema | 34 (9%) | 2 (< 1%) | 34 (9%) | 2 (< 1%) |
| Mucosal Inflammation | 22 (6%) | 1 (< 1%) | 10 (3%) | 1 (< 1%) |
| Pain | 20 (5%) | 4 (1%) | 18 (5%) | 7 (2%) |
| Infections and Infestations | ||||
| Urinary Tract Infection# | 29 (8%) | 6 (2%) | 12 (3%) | 4 (1%) |
| Investigations | ||||
| Weight Decreased | 32 (9%) | 0 | 28 (8%) | 1 (< 1%) |
| Metabolism and Nutrition Disorders | ||||
| Anorexia | 59 (16%) | 3 (< 1%) | 39 (11%) | 3 (< 1%) |
| Dehydration | 18 (5%) | 8 (2%) | 10 (3%) | 3 (< 1%) |
| Musculoskeletal and Connective Tissue Disorders | ||||
| Back Pain | 60 (16%) | 14 (4%) | 45 (12%) | 11 (3%) |
| Arthralgia | 39 (11%) | 4 (1%) | 31 (8%) | 4 (1%) |
| Muscle Spasms | 27 (7%) | 0 | 10 (3%) | 0 |
| Nervous System Disorders | ||||
| Peripheral NeuropathyÞ | 50 (13%) | 3 (< 1%) | 12 (3.2%) | 3 (< 1%) |
| Dysgeusia | 41 (11%) | 0 | 15 (4%) | 0 |
| Dizziness | 30 (8%) | 0 | 21 (6%) | 2 (< 1%) |
| Headache | 28 (8%) | 0 | 19 (5%) | 0 |
| Renal and Urinary Tract Disorders | ||||
| Hematuria | 62 (17%) | 7 (2%) | 13 (4%) | 1 (< 1%) |
| Dysuria | 25 (7%) | 0 | 5 (1%) | 0 |
| Respiratory, Thoracic and Mediastinal Disorders | ||||
| Dyspnea | 43 (12%) | 4 (1%) | 16 (4%) | 2 (< 1%) |
| Cough | 40 (11%) | 0 | 22 (6%) | 0 |
| Skin and Subcutaneous Tissue Disorders | ||||
| Alopecia | 37 (10%) | 0 | 18 (5%) | 0 |
| Vascular Disorders | ||||
| Hypotension | 20 (5%) | 2 (<1 %) | 9 (2%) | 1 (< 1%) |
| Median Duration of Treatment | 6 cycles | 4 cycles |
||
Neutropenia and Associated Clinical Events:
Five patients experienced fatal infectious adverse events (sepsis or septic shock). All had grade 4 neutropenia and one had febrile neutropenia. One additional patient's death was attributed to neutropenia without a documented infection. Twenty-two (6%) patients discontinued JEVTANA treatment due to neutropenia, febrile neutropenia, infection, or sepsis. The most common adverse reaction leading to treatment discontinuation in the JEVTANA group was neutropenia (2%).
Hematuria:
Adverse events of hematuria, including those requiring medical intervention, were more common in JEVTANA-treated patients. The incidence of grade ≥ 2 hematuria was 6% in JEVTANA-treated patients and 2% in mitoxantrone-treated patients. Other factors associated with hematuria were well-balanced between arms and do not account for the increased rate of hematuria on the JEVTANA arm.
Hepatic Laboratory Abnormalities:
The incidences of grade 3–4 increased AST, increased ALT, and increased bilirubin were each ≤ 1%.
Elderly Population:
The following grade 1–4 adverse reactions were reported at rates ≥ 5% higher in patients 65 years of age or greater compared to younger patients: fatigue (40% vs. 30%), neutropenia (97% vs. 89%), asthenia (24% vs. 15%), pyrexia (15% vs. 8%), dizziness (10% vs. 5%), urinary tract infection (10% vs. 3%) and dehydration (7% vs. 2%), respectively.
The incidence of the following grade 3–4 adverse reactions were higher in patients ≥ 65 years of age compared to younger patients; neutropenia (87% vs. 74%), and febrile neutropenia (8% vs. 6%) [see Use in Specific Populations (8.5)].
7. DRUG INTERACTIONS
No formal clinical drug-drug interaction trials have been conducted with JEVTANA.
Prednisone or prednisolone administered at 10 mg daily did not affect the pharmacokinetics of cabazitaxel.
7.1 Drugs That May Increase Cabazitaxel Plasma Concentrations
CYP3A4 Inhibitors: Cabazitaxel is primarily metabolized through CYP3A [see Clinical Pharmacology (12.3)]. Though no formal drug interaction trials have been conducted for JEVTANA, concomitant administration of strong CYP3A inhibitors (e.g., ketoconazole, itraconazole, clarithromycin, atazanavir, indinavir, nefazodone, nelfinavir, ritonavir, saquinavir, telithromycin, voriconazole) is expected to increase concentrations of cabazitaxel. Therefore, co-administration with strong CYP3A inhibitors should be avoided. Caution should be exercised with concomitant use of moderate CYP3A inhibitors.
7.2 Drugs That May Decrease Cabazitaxel Plasma Concentrations
CYP3A4 Inducers: Though no formal drug interaction trials have been conducted for JEVTANA, the concomitant administration of strong CYP3A inducers (e.g., phenytoin, carbamazepine, rifampin, rifabutin, rifapentin, phenobarbital) is expected to decrease cabazitaxel concentrations. Therefore, co-administration with strong CYP3A inducers should be avoided. In addition, patients should also refrain from taking St. John's Wort.
8. USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy category D. See 'Warnings and Precautions' section.
JEVTANA can cause fetal harm when administered to a pregnant woman. There are no adequate and well-controlled studies of JEVTANA in pregnant women.
Non-clinical studies in rats and rabbits have shown that cabazitaxel is embryotoxic, fetotoxic, and abortifacient. Cabazitaxel was shown to cross the placenta barrier within 24 hours of a single intravenous administration of a 0.08 mg/kg dose (approximately 0.02 times the maximum recommended human dose-MRHD) to pregnant rats at gestational day 17.
Cabazitaxel administered once daily to female rats during organogenesis at a dose of 0.16 mg/kg/day (approximately 0.02–0.06 times the Cmax in patients with cancer at the recommended human dose) caused maternal and embryofetal toxicity consisting of increased post-implantation loss, embryolethality, and fetal deaths. Decreased mean fetal birth weight associated with delays in skeletal ossification were observed at doses ≥ 0.08 mg/kg (approximately 0.02 times the Cmax at the MRHD). In utero exposure to cabazitaxel did not result in fetal abnormalities in rats or rabbits at exposure levels significantly lower than the expected human exposures.
If this drug is used during pregnancy or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to the fetus. Women of childbearing potential should be advised to avoid becoming pregnant while taking JEVTANA.
8.3 Nursing Mothers
Cabazitaxel or cabazitaxel metabolites are excreted in maternal milk of lactating rats. It is not known whether this drug is excreted in human milk. Within 2 hours of a single intravenous administration of cabazitaxel to lactating rats at a dose of 0.08 mg/kg (approximately 0.02 times the maximum recommended human dose), radioactivity related to cabazitaxel was detected in the stomachs of nursing pups. This was detectable for up to 24 hours post-dose. Approximately 1.5% of the dose delivered to the mother was calculated to be delivered in the maternal milk. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in nursing infants from JEVTANA, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
8.4 Pediatric Use
The safety and effectiveness of JEVTANA in pediatric patients have not been established.
8.5 Geriatric Use
Based on a population pharmacokinetic analysis, no significant difference was observed in the pharmacokinetics of cabazitaxel between patients < 65 years (n=100) and older (n=70).
Of the 371 patients with prostate cancer treated with JEVTANA every three weeks plus prednisone, 240 patients (64.7%) were 65 years of age and over, while 70 patients (18.9%) were 75 years of age and over. No overall differences in effectiveness were observed between patients ≥ 65 years of age and younger patients. Elderly patients (≥ 65 years of age) may be more likely to experience certain adverse reactions. The incidence of neutropenia, fatigue, asthenia, pyrexia, dizziness, urinary tract infection and dehydration occurred at rates ≥ 5% higher in patients who were 65 years of age or greater compared to younger patients [see Adverse Reactions (6.1)].
8.6 Renal Impairment
No dedicated renal impairment trial for JEVTANA has been conducted. Based on the population pharmacokinetic analysis, no significant difference in clearance was observed in patients with mild (50 mL/min ≤ creatinine clearance (CLcr) < 80 mL/min) and moderate renal impairment (30 mL/min ≤ CLcr < 50 mL/min). No data are available for patients with severe renal impairment or end-stage renal disease [see Clinical Pharmacology (12.3)]. Caution should be used in patients with severe renal impairment (CLcr < 30 mL/min) and patients with end-stage renal diseases.
8.7 Hepatic Impairment
No dedicated hepatic impairment trial for JEVTANA has been conducted. The safety of JEVTANA has not been evaluated in patients with hepatic impairment [see Warnings and Precautions (5.6)].
As cabazitaxel is extensively metabolized in the liver, hepatic impairment is likely to increase the cabazitaxel concentrations. Patients with impaired hepatic function (total bilirubin ≥ ULN, or AST and/or ALT ≥ 1.5 × ULN) were excluded from the randomized clinical trial.
10 OVERDOSAGE
There is no known antidote for JEVTANA overdose. Anticipated complications of overdose include exacerbation of adverse reactions such as bone marrow suppression and gastrointestinal disorders.
In case of overdose, the patient should be kept in a specialized unit where vital signs, chemistry and particular functions can be closely monitored. Patients should receive therapeutic G-CSF as soon as possible after discovery of overdose. Other appropriate symptomatic measures should be taken, as needed.
11 DESCRIPTION
JEVTANA (cabazitaxel) is an antineoplastic agent belonging to the taxane class. It is prepared by semi-synthesis with a precursor extracted from yew needles.
The chemical name of cabazitaxel is (2α,5β,7β,10β,13α)-4-acetoxy-13-({(2R,3S)-3-[(tertbutoxycarbonyl) amino]-2-hydroxy-3-phenylpropanoyl}oxy)-1-hydroxy-7,10-dimethoxy-9-oxo-5,20-epoxytax-11-en-2-yl benzoate – propan-2-one(1:1).
Cabazitaxel has the following structural formula:
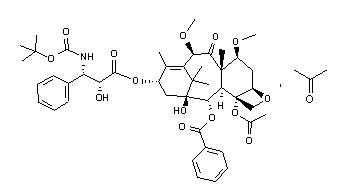
Cabazitaxel is a white to almost-white powder with a molecular formula of C45H57NO14.C3H6O and a molecular weight of 894.01 (for the acetone solvate) / 835.93 (for the solvent free). It is lipophilic, practically insoluble in water and soluble in alcohol.
JEVTANA (cabazitaxel) Injection 60 mg/1.5 mL is a sterile, non-pyrogenic, clear yellow to brownish-yellow viscous solution and is available in single-use vials containing 60 mg cabazitaxel (anhydrous and solvent free) and 1.56 g polysorbate 80.
Each mL contains 40 mg cabazitaxel (anhydrous) and 1.04 g polysorbate 80.
DILUENT for JEVTANA is a clear, colorless, sterile, and non-pyrogenic solution containing 13% (w/w) ethanol in water for injection, approximately 5.7 mL.
JEVTANA requires two dilutions prior to intravenous infusion. JEVTANA injection should be diluted only with the supplied DILUENT for JEVTANA, followed by dilution in either 0.9% sodium chloride solution or 5% dextrose solution.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Cabazitaxel is a microtubule inhibitor. Cabazitaxel binds to tubulin and promotes its assembly into microtubules while simultaneously inhibiting disassembly. This leads to the stabilization of microtubules, which results in the inhibition of mitotic and interphase cellular functions.
12.2 Pharmacodynamics
Cabazitaxel demonstrated antitumor activity against advanced human tumors xenografted in mice. Cabazitaxel is active in docetaxel-sensitive tumors. In addition, cabazitaxel demonstrated activity in tumor models insensitive to chemotherapy including docetaxel.
12.3 Pharmacokinetics
A population pharmacokinetic analysis was conducted in 170 patients with solid tumors at doses ranging from 10 to 30 mg/m2 weekly or every three weeks.
Absorption
Based on the population pharmacokinetic analysis, after an intravenous dose of cabazitaxel 25 mg/m2 every three weeks, the mean Cmax in patients with metastatic prostate cancer was 226 ng/mL (CV 107%) and was reached at the end of the one-hour infusion (Tmax). The mean AUC in patients with metastatic prostate cancer was 991 ng∙h/mL (CV 34%).
No major deviation from the dose proportionality was observed from 10 to 30 mg/m2 in patients with advanced solid tumors.
Distribution
The volume of distribution (Vss) was 4,864 L (2,643 L/m2 for a patient with a median BSA of 1.84 m2) at steady state.
In vitro, the binding of cabazitaxel to human serum proteins was 89 to 92% and was not saturable up to 50,000 ng/mL, which covers the maximum concentration observed in clinical trials. Cabazitaxel is mainly bound to human serum albumin (82%) and lipoproteins (88% for HDL, 70% for LDL, and 56% for VLDL). The in vitro blood-to-plasma concentration ratio in human blood ranged from 0.90 to 0.99, indicating that cabazitaxel was equally distributed between blood and plasma.
Metabolism
Cabazitaxel is extensively metabolized in the liver (> 95%), mainly by the CYP3A4/5 isoenzyme (80% to 90%), and to a lesser extent by CYP2C8. Cabazitaxel is the main circulating moiety in human plasma. Seven metabolites were detected in plasma (including the 3 active metabolites issued from O-demethylation), with the main one accounting for 5% of cabazitaxel exposure. Around 20 metabolites of cabazitaxel are excreted into human urine and feces.
Based on in vitro studies, the potential for cabazitaxel to inhibit drugs that are substrates of other CYP isoenzymes (1A2,-2B6,-2C9, -2C8, -2C19, -2E1, -2D6, and CYP3A4/5) is low. In addition, cabazitaxel did not induce CYP isozymes (-1A, -2C and -3A) in vitro.
A drug interaction study in 11 patients with advanced cancers has shown that cabazitaxel (25 mg/m2 administered as a single 1-hour infusion) did not modify the plasma levels of midazolam, a probe substrate of CYP3A. Therefore, cabazitaxel is not an inhibitor of CYP3A in vivo.
Elimination
After a one-hour intravenous infusion [14C]-cabazitaxel 25 mg/m2, approximately 80% of the administered dose was eliminated within 2 weeks. Cabazitaxel is mainly excreted in the feces as numerous metabolites (76% of the dose); while renal excretion of cabazitaxel and metabolites account for 3.7% of the dose (2.3% as unchanged drug in urine).
Based on the population pharmacokinetic analysis, cabazitaxel has a plasma clearance of 48.5 L/h (CV 39%; 26.4 L/h/m2 for a patient with a median BSA of 1.84 m2) in patients with metastatic prostate cancer. Following a one-hour intravenous infusion, plasma concentrations of cabazitaxel can be described by a three-compartment pharmacokinetic model with α-, β-, and γ- half-lives of 4 minutes, 2 hours, and 95 hours, respectively.
Renal Impairment
Cabazitaxel is minimally excreted via the kidney. No formal pharmacokinetic trials have been conducted with cabazitaxel in patients with renal impairment. The population pharmacokinetic analysis carried out in 170 patients including 14 patients with moderate renal impairment (30 mL/min ≤ CLcr < 50 mL/min) and 59 patients with mild renal impairment (50 mL/min ≤ CLcr < 80 mL/min) showed that mild to moderate renal impairment did not have meaningful effects on the pharmacokinetics of cabazitaxel. No data are available for patients with severe renal impairment or end-stage renal disease [see Use in Special Populations (8.6)].
Hepatic Impairment
No formal trials in patients with hepatic impairment have been conducted. As cabazitaxel is extensively metabolized in the liver, hepatic impairment is likely to increase the cabazitaxel concentrations [see Warnings and Precautions (5.6), and Use in Special Populations (8.7)].
Drug interactions
As cabazitaxel is mainly metabolized by CYP3A in vitro, strong CYP3A inducers or inhibitors are expected to affect the pharmacokinetics of cabazitaxel.
Prednisone or prednisolone administered at 10 mg daily did not affect the pharmacokinetics of cabazitaxel.
In vitro, cabazitaxel did not inhibit the multidrug-resistance protein 1 (MRP1) 2 (MRP2) or organic cation transporter (OCT1). In vitro, cabazitaxel inhibited P-gp, BRCP, and organic anion transporting polypeptides (OATP1B1, OATP1B3). However the in vivo risk of cabazitaxel inhibiting MRPs, OCT1, P-gp, BCRP, OATP1B1 or OATP1B3 is low at the dose of 25 mg/m2.
In vitro, cabazitaxel is a substrate of P-gp, but not a substrate of MRP1, MRP2, BCRP, OCT1, OATP1B1 or OATP1B3.
12.6 Cardiac Electrophysiology
The effect of cabazitaxel following a single dose of 25 mg/m2 administered by intravenous infusion on QTc interval was evaluated in 94 patients with solid tumors. No large changes in the mean QT interval (i.e., > 20 ms) from baseline based on Fridericia correction method were detected. However, a small increase in the mean QTc interval (i.e., < 10 ms) cannot be excluded due to study design limitations.
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Long-term animal studies have not been performed to evaluate the carcinogenic potential of cabazitaxel.
Cabazitaxel was positive for clastogenesis in the in vivo micronucleus test, inducing an increase of micronuclei in rats at doses ≥ 0.5 mg/kg. Cabazitaxel increased numerical aberrations with or without metabolic activation in an in vitro test in human lymphocytes though no induction of structural aberrations was observed. Cabazitaxel did not induce mutations in the bacterial reverse mutation (Ames) test. The positive in vivo genotoxicity findings are consistent with the pharmacological activity of the compound (inhibition of tubulin depolymerization).
Cabazitaxel may impair fertility in humans. In a fertility study performed in female rats at cabazitaxel doses of 0.05, 0.1, or 0.2 mg/kg/day there was no effect of administration of the drug on mating behavior or the ability to become pregnant. There was an increase in pre-implantation loss at the 0.2 mg/kg/day dose and an increase in early resorptions at doses ≥ 0.1 mg/kg/day (approximately 0.02–0.06 times the human clinical exposure based on Cmax). In multi-cycle studies following the clinically recommended dosing schedule, atrophy of the uterus was observed at the 5 mg/kg dose level (approximately the AUC in patients with cancer at the recommended human dose) along with necrosis of the corpora lutea at doses ≥ 1 mg/kg (approximately 0.2 times the AUC at the clinically recommended human dose).
Cabazitaxel did not affect mating performances or fertility of treated male rats at doses of 0.05, 0.1, or 0.2 mg/kg/day. In multiple-cycle studies following the clinically recommended dosing schedule, however, degeneration of seminal vesicle and seminiferous tubule atrophy in the testis were observed in rats treated intravenously with cabazitaxel at a dose of 1 mg/kg (approximately 0.2–0.35 times the AUC in patients with cancer at the recommended human dose), and minimal testicular degeneration (minimal epithelial single cell necrosis in epididymis) was observed in dogs treated with a dose of 0.5 mg/kg (approximately one-tenth of the AUC in patients with cancer at the recommended human dose).
14. CLINICAL STUDIES
The efficacy and safety of JEVTANA in combination with prednisone were evaluated in a randomized, open-label, international, multi-center study in patients with hormone-refractory metastatic prostate cancer previously treated with a docetaxel-containing treatment regimen.
A total of 755 patients were randomized to receive either JEVTANA 25 mg/m2 intravenously every 3 weeks for a maximum of 10 cycles with prednisone 10 mg orally daily (n=378), or to receive mitoxantrone 12 mg/m2 intravenously every 3 weeks for 10 cycles with prednisone 10 mg orally daily (n=377) for a maximum of 10 cycles.
This study included patients over 18 years of age with hormone-refractory metastatic prostate cancer either measurable by RECIST criteria or non-measurable disease with rising PSA levels or appearance of new lesions, and ECOG (Eastern Cooperative Oncology Group) performance status 0–2. Patients had to have neutrophils >1,500 cells/mm3, platelets > 100,000 cells/mm3, hemoglobin > 10 g/dL, creatinine < 1.5 × upper limit of normal (ULN), total bilirubin < 1×ULN, AST < 1.5 × ULN, and ALT < 1.5 × ULN. Patients with a history of congestive heart failure, or myocardial infarction within the last 6 months, or patients with uncontrolled cardiac arrhythmias, angina pectoris, and/or hypertension were not included in the study.
Demographics, including age, race, and ECOG performance status (0–2) were balanced between the treatment arms. The median age was 68 years (range 46–92) and the racial distribution for all groups was 83.9% Caucasian, 6.9% Asian, 5.3% Black, and 4% Others in the JEVTANA group.
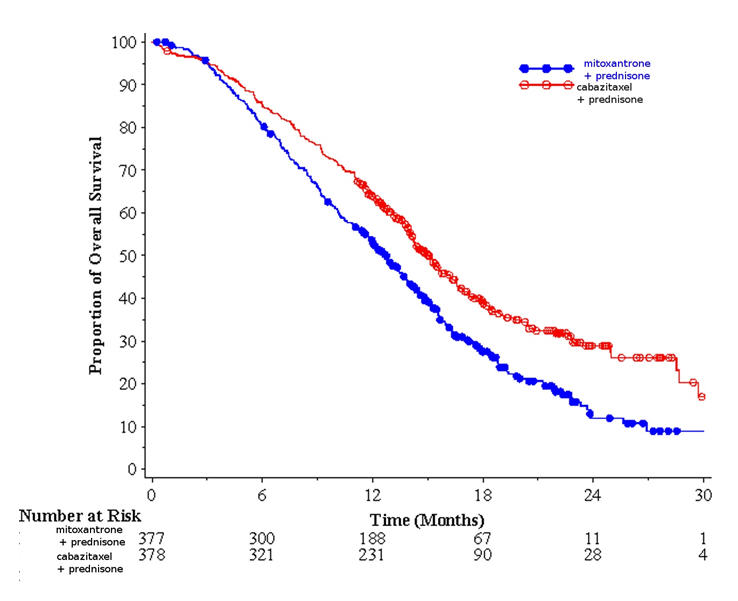
Efficacy results for the JEVTANA arm versus the control arm are summarized in Table 3 and Figure 1.
| JEVTANA + Prednisone n=378 | Mitoxantrone + Prednisone n=377 |
|
|---|---|---|
|
||
| Overall Survival | ||
| Number of deaths (%) | 234 (61.9 %) | 279 (74%) |
| Median survival (month) (95% CI) | 15.1 (14.1–16.3) | 12.7 (11.6–13.7) |
| Hazard Ratio* (95% CI) | 0.70 (0.59–0.83) | |
| p-value | <0.0001 | |
| Figure 1 - Kaplan-Meier Overall Survival Curves |
 |
Investigator-assessed tumor response of 14.4% (95%CI: 9.6–19.3) was higher for patients in the JEVTANA arm compared to 4.4% (95%CI: 1.6–7.2) for patients in the mitoxantrone arm, p=0.0005.
15. REFERENCES
- NIOSH Alert: Preventing occupational exposures to antineoplastic and other hazardous drugs in healthcare settings. 2004. U.S. Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health, DHHS (NIOSH) Publication No. 2004-165.
- OSHA Technical Manual, TED 1-0.15A, Section VI: Chapter 2. Controlling Occupational Exposure to Hazardous Drugs. OSHA, 1999. http://www.osha.gov/dts/osta/otm/otm_vi/otm_vi_2.html
- American Society of Health-System Pharmacists. (2006) ASHP Guidelines on Handling Hazardous Drugs. Am J Health-Syst Pharm 2006; 63:1172–1193.
- Polovich, M., White, J. M., & Kelleher, L.O. (eds.) 2005. Chemotherapy and biotherapy guidelines and recommendations for practice (2nd. ed.) Pittsburgh, PA: Oncology Nursing Society.
16. HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
JEVTANA is supplied as a kit containing one single-use vial of JEVTANA (cabazitaxel) Injection (clear glass vial with a grey rubber closure, aluminum cap and light green plastic flip-off cap) and one vial of Diluent for JEVTANA (13% (w/w) ethanol in water for injection) in a clear glass vial with a grey rubber closure, gold-color aluminum cap and colorless plastic flip-off cap. Both items are in a blister pack in one carton.
NDC 0024-5824-11
16.2 Storage
JEVTANA Injection and Diluent for JEVTANA:
Store at 25°C (77°F); excursions permitted between 15°–30°C (59°–86°F).
Do not refrigerate.
Stability of the First Diluted Solution in the Vial:
First diluted solution of JEVTANA should be used immediately (within 30 minutes). Discard any unused portion [see Dosage and Administration (2.5)].
Stability of the Second (Final) Dilution Solution in the Infusion Bag:
Fully prepared JEVTANA infusion solution (in either 0.9% sodium chloride solution or 5% dextrose solution) should be used within 8 hours at ambient temperature (including the one-hour infusion), or for a total of 24 hours (including the one-hour infusion) under the refrigerated conditions.
In addition, chemical and physical stability of the infusion solution has been demonstrated for 24 hours under refrigerated conditions. As both the first diluted solution and the second (final) infusion solution are supersaturated, the solutions may crystallize over time. If crystals and/or particulates appear, the solutions must not be used and should be discarded [see Dosage and Administration (2.5)].
16.3 Handling and Disposal
Procedures for proper handling and disposal of antineoplastic drugs should be followed. Several guidelines on this subject have been published [see References (15)]. Any unused product or waste material should be disposed of in accordance with local requirements.
17. PATIENT COUNSELING INFORMATION
See FDA-Approved Patient Labeling
- Educate patients about the risk of potential hypersensitivity associated with JEVTANA. Confirm patients do not have a history of severe hypersensitivity reactions to cabazitaxel or to other drugs formulated with polysorbate 80. Instruct patients to immediately report signs of a hypersensitivity reaction.
- Explain the importance of routine blood cell counts. Instruct patients to monitor their temperature frequently and immediately report any occurrence of fever to the treating oncologist.
- Explain that it is important to take the oral prednisone as prescribed. Instruct patients to report if they were not compliant with oral corticosteroid regimen.
- Explain to patients that severe and fatal infections, dehydration, and renal failure have been associated with cabazitaxel exposure. Patients should immediately report fever, significant vomiting or diarrhea, decreased urinary output, and hematuria to the treating oncologist.
- Inform patients about the risk of drug interactions and the importance of providing a list of prescription and non-prescription drugs to the treating oncologist [see Drug Interactions (7)].
- Inform elderly patients that certain side effects may be more frequent or severe.
Patient Information
JEVTANA® (JEV-TA-NA)
(cabazitaxel)
Injection
Read this Patient Information before you start receiving JEVTANA and each time before you receive your infusion. There may be new information. This information does not take the place of talking to your doctor about your medical condition or your treatment.
What is the most important information I should know about JEVTANA?
JEVTANA may cause serious side effects including:
-
Low white blood cells. Low white blood cells can cause you to get serious infections, and may lead to death. People who are 65 years or older may be more likely to have these problems. Your doctor:
- will do blood tests regularly to check your white blood cell counts during your treatment with JEVTANA.
- may lower your dose of JEVTANA, change how often you receive it, or stop JEVTANA until your doctor decides that you have enough white blood cells.
- may prescribe a medicine for you called G-CSF, to help prevent complications if your white blood cell count is too low.
Tell your doctor right away if you have any of these symptoms of infection while receiving JEVTANA:
- fever. Take your temperature often during treatment with JEVTANA.
- cough
- burning on urination
- muscle aches
Also, tell your doctor if you have any diarrhea during the time that your white blood cell count is low. Your doctor may prescribe treatment for you as needed.
-
Severe allergic reactions. Severe allergic reactions can happen within a few minutes after your infusion of JEVTANA starts, especially during the first and second infusions. Your doctor should prescribe medicines before each infusion to help prevent severe allergic reactions.
Tell your doctor or nurse right away if you have any of these symptoms of a severe allergic reaction during or soon after an infusion of JEVTANA:
- rash or itching
- skin redness
- feeling dizzy or faint
- breathing problems
- chest or throat tightness
- swelling of face
- Gastrointestinal symptoms. Vomiting and diarrhea can happen when you take JEVTANA. Severe vomiting and diarrhea with JEVTANA can lead to loss of too much body fluid (dehydration), or too much of your body salts (electrolytes). Death has happened from having severe diarrhea and losing too much body fluid or body salts with JEVTANA. Tell your doctor if you have vomiting or diarrhea. Your doctor will prescribe medicines to prevent or treat vomiting and diarrhea, as needed with JEVTANA. Tell your doctor if your symptoms get worse or do not get better. You may need to go to the hospital for treatment.
-
Kidney failure. Kidney failure may happen with JEVTANA, because of severe infection, loss of too much body fluid (dehydration), and other reasons, which may lead to death. Your doctor will check you for this problem and treat you if needed. Tell your doctor if you develop:
- swelling of your face or body
- decrease in the amount of urine that your body makes each day.
What is JEVTANA?
JEVTANA is a prescription anti-cancer medicine used with the steroid medicine prednisone. JEVTANA is used to treat people with prostate cancer that has worsened (progressed) after treatment with other anti-cancer medicines, including docetaxel.
It is not known if JEVTANA is safe and works in children.
Who should not receive JEVTANA?
Do not receive JEVTANA if:
- your white blood cell (neutrophil count) is too low
- you have had a severe allergic reaction to cabazitaxel or other medicines that contain polysorbate 80. Ask your doctor if you are not sure.
What should I tell my doctor before receiving JEVTANA?
Before receiving JEVTANA, tell your doctor if you:
- had allergic reactions in the past
- have kidney or liver problems
- are over the age of 65
- have any other medical conditions
- if you are a female and:
- are pregnant or plan to become pregnant. JEVTANA can harm your unborn baby. Talk to your doctor about the best way for you to prevent pregnancy while you are receiving JEVTANA.
- are breastfeeding or plan to breastfeed. It is not known if JEVTANA passes into your breast milk. You and your doctor should decide if you will take JEVTANA or breastfeed. You should not do both.
Tell your doctor about all the medicines you take, including prescription and non-prescription medicines, vitamins, and herbal supplements. JEVTANA can interact with many other medicines. Do not take any new medicines without asking your doctor first. Your doctor will tell you if it is safe to take the new medicine with JEVTANA.
How will I receive JEVTANA?
- JEVTANA will be given to you by an intravenous (IV) infusion into your vein.
- Your treatment will take about 1 hour.
- JEVTANA is usually given every 3 weeks. Your doctor will decide how often you will receive JEVTANA .
- Your doctor will also prescribe another medicine called prednisone, for you to take by mouth every day during treatment with JEVTANA. Your doctor will tell you how and when to take your prednisone.
It is important that you take prednisone exactly as prescribed by your doctor. If you forget to take your prednisone, or do not take it on schedule, make sure to tell your doctor or nurse. Before each infusion of JEVTANA, you may receive other medicines to prevent or treat side effects.
What are the possible side effects of JEVTANA?
JEVTANA may cause serious side effects including:
Common side effects of JEVTANA include:
- Low red blood cell count (anemia). Your doctor will regularly check your red blood cell count. Symptoms of anemia include shortness of breath and tiredness.
- Low blood platelet count. Tell your doctor if you have any unusual bruising or bleeding.
|
|
Tell your doctor if you have any side effect that bothers you or that does not go away.
These are not all the possible side effects of JEVTANA. For more information, ask your doctor or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
General information about JEVTANA
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet.
This leaflet summarizes the most important information about JEVTANA. If you would like more information, talk with your doctor. You can ask your pharmacist or doctor for information about JEVTANA that is written for health professionals.
For more information, go to www.sanofi-aventis.us or call 1-800-633-1610.
What are the ingredients in JEVTANA?
Active ingredient: cabazitaxel
Inactive ingredient: polysorbate 80
sanofi-aventis U.S. LLC
Bridgewater, NJ 08807
Issued 2013
JEVTANA® is a registered trademark of sanofi-aventis
©2013 sanofi-aventis U.S. LLC
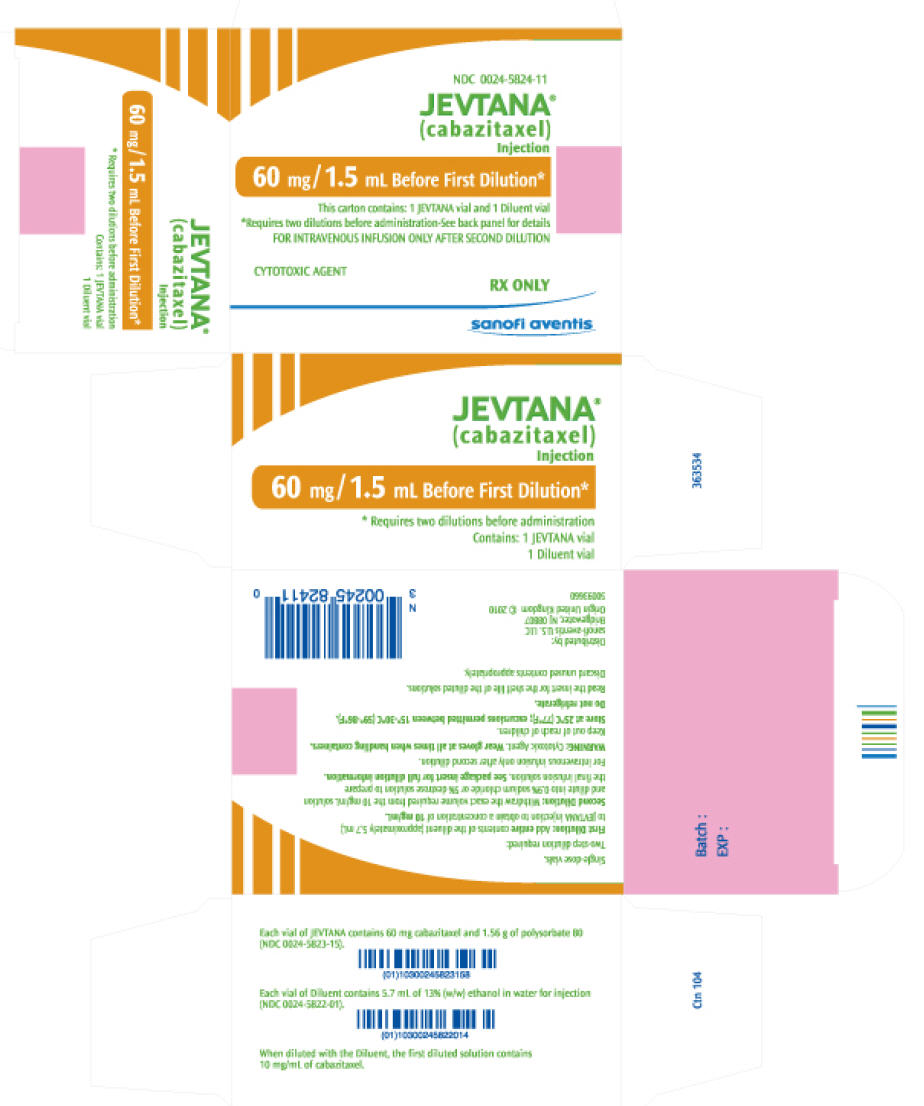
PRINCIPAL DISPLAY PANEL - Kit Carton
NDC 0024-5824-11
JEVTANA®
(cabazitaxel)
Injection
60 mg/1.5 mL Before First Dilution*
This carton contains: 1 JEVTANA vial and 1 Diluent vial
*Requires two dilutions before administration-See back panel for details
FOR INTRAVENOUS INFUSION ONLY AFTER SECOND DILUTION
CYTOTOXIC AGENT
RX ONLY
sanofi aventis
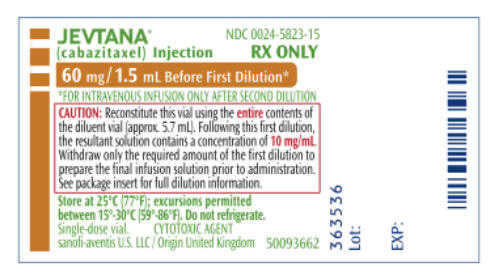
PRINCIPAL DISPLAY PANEL - 5.7 mL Label
JEVTANA®
(cabazitaxel) Injection
NDC 0024-5823-15
60 mg/1.5 mL Before First Dilution*
* FOR INTRAVENOUS INFUSION ONLY AFTER SECOND DILUTION
CAUTION: Reconstitute this vial using the entire contents of
the diluent vial (approx 5.7 mL). Following this first dilution,
the resultant solution contains a concentration of 10mg/mL.
Withdraw only the required amount of the first dilution to
prepare the final infusion solution prior to administration.
See package insert for full dilution information.
Store at 25°C (77°F); excursions permitted between 15°-30°C (59°-86°F).
Do not refrigerate.
Single-dose vial. CYTOTOXIC AGENT
sanofi-aventis U.S. LLC/ Origin: United Kingdom 50093662
RX ONLY
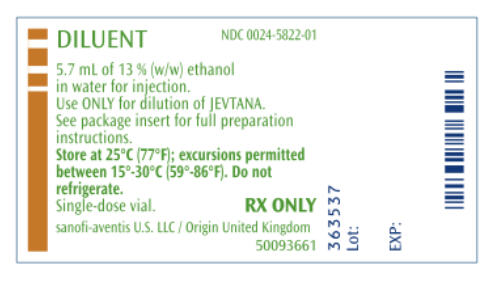
PRINCIPAL DISPLAY PANEL - 5.7 mL Label
DILUENT
NDC 0024-5822-01
5.7 mL of 13 % (w/w) ethanol
in water for injection.
Use ONLY for dilution of JEVTANA.
See package insert for full preparation
instructions.
Store at 25°C (77°F); excursions permitted
between 15°-30°C (59°-86°F). Do not
refrigerate.
Single-dose vial.
RX ONLY
sanofi-aventis U.S. LLC/Origin United Kingdom
50093661
| JEVTANA
cabazitaxel kit |
||||||||||||||
|
||||||||||||||
|
||||||||||||||
|
||||||||||||||
|
||||||||||||||
|
||||||||||||||
|
||||||||||||||
|
||||||||||||||
|
||||||||||||||
|
||||||||||||||
|
||||||||||||||
|
||||||||||||||
|
||||||||||||||
|
||||||||||||||
|
||||||||||||||
|
||||||||||||||
| Labeler - Sanofi-Aventis U.S. LLC (824676584) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
| Aventis Pharma Ltd. | 231317665 | MANUFACTURE(0024-5824), ANALYSIS(0024-5824), LABEL(0024-5824), PACK(0024-5824) | |