LYSODREN
-
mitotane tablet
Bristol-Myers Squibb
----------
LYSODREN®
(mitotane tablets,
USP)
WARNINGS
LYSODREN (mitotane tablets, USP) should be administered under the supervision of a qualified physician experienced in the uses of cancer chemotherapeutic agents. LYSODREN should be temporarily discontinued immediately following shock or severe trauma since adrenal suppression is its prime action. Exogenous steroids should be administered in such circumstances, since the depressed adrenal may not immediately start to secrete steroids.
DESCRIPTION
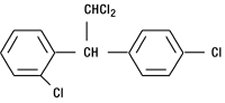
LYSODREN® (mitotane tablets, USP) is an oral chemotherapeutic agent. It is best known by its trivial name, o,p′-DDD, and is chemically, 1,1-dichloro-2-(o-chlorophenyl)-2-(p-chlorophenyl) ethane. The chemical structure is shown below:
LYSODREN is a white granular solid composed of clear colorless crystals. It is tasteless and has a slight pleasant aromatic odor. It is soluble in ethanol, isooctane, and carbon tetrachloride. It has a molecular weight of 320.05.
Inactive ingredients in LYSODREN tablets are: avicel, Polyethylene Glycol 3350, silicon dioxide, and starch.
LYSODREN is available as 500 mg scored tablets for oral administration.
CLINICAL PHARMACOLOGY
LYSODREN can best be described as an adrenal cytotoxic agent, although it can cause adrenal inhibition, apparently without cellular destruction. Its biochemical mechanism of action is unknown. Data are available to suggest that the drug modifies the peripheral metabolism of steroids as well as directly suppressing the adrenal cortex. The administration of LYSODREN alters the extra-adrenal metabolism of cortisol in man; leading to a reduction in measurable 17-hydroxy corticosteroids, even though plasma levels of corticosteroids do not fall. The drug apparently causes increased formation of 6-β-hydroxycortisol.
Data in adrenal carcinoma patients indicate that about 40% of oral LYSODREN is absorbed and approximately 10% of the administered dose is recovered in the urine as a water-soluble metabolite. A variable amount of metabolite (1%-17%) is excreted in the bile and the balance is apparently stored in the tissues.
Following discontinuation of LYSODREN, the plasma terminal half-life has ranged from 18 to 159 days. In most patients blood levels become undetectable after 6 to 9 weeks. Autopsy data have provided evidence that LYSODREN is found in most tissues of the body; however, fat tissues are the primary site of storage. LYSODREN is converted to a water-soluble metabolite.
No unchanged LYSODREN has been found in urine or bile.
INDICATIONS AND USAGE
LYSODREN is indicated in the treatment of inoperable adrenal cortical carcinoma of both functional and nonfunctional types.
CONTRAINDICATIONS
LYSODREN (mitotane tablets, USP) should not be given to individuals who have demonstrated a previous hypersensitivity to it.
WARNINGS
LYSODREN should be temporarily discontinued immediately following shock or severe trauma, since adrenal suppression is its prime action. Exogenous steroids should be administered in such circumstances, since the depressed adrenal may not immediately start to secrete steroids.
LYSODREN should be administered with care to patients with liver disease other than metastatic lesions from the adrenal cortex, since the metabolism of LYSODREN may be interfered with and the drug may accumulate.
All possible tumor tissues should be surgically removed from large metastatic masses before LYSODREN administration is instituted. This is necessary to minimize the possibility of infarction and hemorrhage in the tumor due to a rapid cytotoxic effect of the drug.
Long-term continuous administration of high doses of LYSODREN may lead to brain damage and impairment of function. Behavioral and neurological assessments should be made at regular intervals when continuous LYSODREN treatment exceeds 2 years.
A substantial percentage of the patients treated show signs of adrenal insufficiency. It therefore appears necessary to watch for and institute steroid replacement in those patients. However, some investigators have recommended that steroid replacement therapy be administered concomitantly with LYSODREN. It has been shown that the metabolism of exogenous steroids is modified and consequently somewhat higher doses than normal replacement therapy may be required.
PRECAUTIONS
General
Adrenal insufficiency may develop in patients treated with LYSODREN, and adrenal steroid replacement should be considered for these patients.
Since sedation, lethargy, vertigo, and other CNS side effects can occur, ambulatory patients should be cautioned about driving, operating machinery, and other hazardous pursuits requiring mental and physical alertness.
Drug Interactions
LYSODREN has been reported to accelerate the metabolism of warfarin by the mechanism of hepatic microsomal enzyme induction, leading to an increase in dosage requirements for warfarin. Therefore, physicians should closely monitor patients for a change in anticoagulant dosage requirements when administering LYSODREN to patients on coumarin-type anticoagulants. In addition, LYSODREN should be given with caution to patients receiving other drugs susceptible to the influence of hepatic enzyme induction.
Carcinogenesis, Mutagenesis, Impairment of Fertility
The carcinogenic and mutagenic potentials of LYSODREN (mitotane tablets, USP) are unknown. However, the mechanism of action of this compound suggests that it probably has less carcinogenic potential than other cytotoxic chemotherapeutic drugs.
Pregnancy
Pregnancy Category C
Animal reproduction studies have not been conducted with LYSODREN. It is also not known whether LYSODREN can cause fetal harm when administered to a pregnant woman or can affect reproduction capacity. LYSODREN should be given to a pregnant woman only if clearly needed.
Nursing Mothers
It is not known whether this drug is excreted in human milk. Because many drugs are excreted in human milk and because of the potential for adverse reactions in nursing infants from mitotane, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
Pediatric Use
Safety and effectiveness in pediatric patients have not been established.
Geriatric Use
Clinical studies of LYSODREN did not include sufficient numbers of patients aged 65 years and older to determine whether they respond differently than younger patients. Other reported clinical experience has not identified differences in responses between elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
ADVERSE REACTIONS
A very high percentage of patients treated with LYSODREN have shown at least one type of side effect. The main types of adverse reactions consist of the following:
- Gastrointestinal disturbances, which consist of anorexia, nausea or vomiting, and in some cases diarrhea, occur in about 80% of the patients.
- Central nervous system side effects occur in 40% of the patients. These consist primarily of depression as manifested by lethargy and somnolence (25%), and dizziness or vertigo (15%).
- Skin toxicity has been observed in about 15% of the cases. These skin changes consist primarily of transient skin rashes which do not seem to be dose related. In some instances, this side effect subsided while the patients were maintained on the drug without a change of dose. Infrequently occurring side effects involve the eye (visual blurring, diplopia, lens opacity, toxic retinopathy); the genitourinary system (hematuria, hemorrhagic cystitis, and albuminuria); cardiovascular system (hypertension, orthostatic hypotension, and flushing); and some miscellaneous effects including generalized aching, hyperpyrexia, and lowered protein bound iodine (PBI).
OVERDOSAGE
No proven antidotes have been established for LYSODREN overdosage.
DOSAGE AND ADMINISTRATION
The recommended treatment schedule is to start the patient at 2 g to 6 g of LYSODREN per day in divided doses, either 3 or 4 times a day. Doses are usually increased incrementally to 9 g to 10 g per day. If severe side effects appear, the dose should be reduced until the maximum tolerated dose is achieved. If the patient can tolerate higher doses and improved clinical response appears possible, the dose should be increased until adverse reactions interfere. Experience has shown that the maximum tolerated dose (MTD) will vary from 2 g to 16 g per day, but has usually been 9 g to 10 g per day. The highest doses used in the studies to date were 18 g to 19 g per day.
Treatment should be instituted in the hospital until a stable dosage regimen is achieved.
Treatment should be continued as long as clinical benefits are observed. Maintenance of clinical status or slowing of growth of metastatic lesions can be considered clinical benefits if they can clearly be shown to have occurred.
If no clinical benefits are observed after 3 months at the maximum tolerated dose, the case would generally be considered a clinical failure. However, 10% of the patients who showed a measurable response required more than 3 months at the MTD. Early diagnosis and prompt institution of treatment improve the probability of a positive clinical response. Clinical effectiveness can be shown by reduction in tumor mass; reduction in pain, weakness or anorexia; and reduction of symptoms and signs due to excessive steroid production.
A number of patients have been treated intermittently with treatment being restarted when severe symptoms have reappeared. Patients often do not respond after the third or fourth such course. Experience accumulated to date suggests that continuous treatment with the maximum possible dosage of LYSODREN is the best approach.
Procedures for proper handling and disposal of anticancer drugs should be considered. Several guidelines on this subject have been published.1-4
To minimize the risk of dermal exposure, always wear impervious gloves when handling bottles containing LYSODREN tablets. LYSODREN tablets should not be crushed. Personnel should avoid exposure to crushed and/or broken tablets. If contact with broken tablets occurs, wash immediately and thoroughly. More information is available in the references listed below.
HOW SUPPLIED
LYSODREN® (mitotane tablets, USP)
NDC 0015-3080-60—500 mg Tablets, bottle of 100
STORAGE
Store at 25°C (77°F); excursions permitted to 15°C-30°C (59°F-86°F) [see USP Controlled Room Temperature].
REFERENCES
- NIOSH Alert: Preventing occupational exposures to antineoplastic and other hazardous drugs in healthcare settings. 2004. U.S. Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health, DHHS (NIOSH) Publication No. 2004-165.
- OSHA Technical Manual, TED 1-0.15A, Section VI: Chapter 2. Controlling Occupational Exposure to Hazardous Drugs. OSHA, 1999. http://www.osha.gov/dts/osta/otm/otm_vi/otm_vi_2.html
- American Society of Health-System Pharmacists. ASHP guidelines on handling hazardous drugs. Am J Health-Syst Pharm. 2006;63:1172-1193.
- Polovich M, White JM, Kelleher LO, eds. 2005. Chemotherapy and biotherapy guidelines and recommendations for practice (2nd ed.) Pittsburgh, PA: Oncology Nursing Society.
Bristol-Myers Squibb Company
Princeton,
New Jersey 08543 USA
Made in Italy
1050972A3
Rev
February 2009
| LYSODREN
mitotane tablet |
||||||||||||||||||||||
|
||||||||||||||||||||||
|
||||||||||||||||||||||
|
||||||||||||||||||||||
|
||||||||||||||||||||||
Revised: 03/2009Bristol-Myers Squibb