APIDRA
-
insulin glulisine injection, solution
APIDRA SOLOSTAR
-
insulin glulisine injection, solution
sanofi-aventis U.S. LLC
----------
|
|||||||||||||||||||||||||||||||||
FULL PRESCRIBING INFORMATION
1 INDICATIONS AND USAGE
APIDRA is indicated to improve glycemic control in adults and children with diabetes mellitus.
2 DOSAGE AND ADMINISTRATION
2.1 Dosage considerations
APIDRA is a recombinant insulin analog that is equipotent to human insulin (i.e. one unit of APIDRA has the same glucose-lowering effect as one unit of regular human insulin) when given intravenously. When given subcutaneously, APIDRA has a more rapid onset of action and a shorter duration of action than regular human insulin.
The dosage of APIDRA must be individualized. Blood glucose monitoring is essential in all patients receiving insulin therapy.
The total daily insulin requirement may vary and is usually between 0.5 to 1 Unit/kg/day. Insulin requirements may be altered during stress, major illness, or with changes in exercise, meal patterns, or coadministered drugs.
2.2 Subcutaneous administration
APIDRA should be given within 15 minutes before a meal or within 20 minutes after starting a meal.
APIDRA given by subcutaneous injection should generally be used in regimens with an intermediate or long-acting insulin.
APIDRA should be administered by subcutaneous injection in the abdominal wall, thigh, or upper arm. Injection sites should be rotated within the same region (abdomen, thigh or upper arm) from one injection to the next to reduce the risk of lipodystrophy [See Adverse Reactions (6.1)].
2.3 Continuous subcutaneous infusion (insulin pump)
APIDRA may be administered by continuous subcutaneous infusion in the abdominal wall. Do not use diluted or mixed insulins in external insulin pumps. Infusion sites should be rotated within the same region to reduce the risk of lipodystrophy [See Adverse Reactions (6.1)]. The initial programming of the external insulin infusion pump should be based on the total daily insulin dose of the previous regimen.
The following insulin pumps1 have been used in APIDRA clinical trials conducted by sanofi-aventis, the manufacturer of APIDRA:
- Disetronic® H-Tron® plus V100 and D-Tron® with Disetronic catheters (Rapid™, Rapid C™, Rapid D™, and Tender™)
- MiniMed® Models 506, 507, 507c and 508 with MiniMed catheters (Sof-set Ultimate QR™, and Quick-set™).
Before using a different insulin pump with APIDRA, read the pump label to make sure the pump has been evaluated with APIDRA.
Physicians and patients should carefully evaluate information on pump use in the APIDRA prescribing information, Patient Information Leaflet, and the pump manufacturer's manual. APIDRA-specific information should be followed for in-use time, frequency of changing infusion sets, or other details specific to APIDRA usage, because APIDRA-specific information may differ from general pump manual instructions.
Based on in vitro studies which have shown loss of the preservative, metacresol and insulin degradation, APIDRA in the reservoir should be changed at least every 48 hours. APIDRA in clinical use should not be exposed to temperatures greater than 98.6°F (37°C). [See Warnings and Precautions (5.7) and How Supplied/Storage and Handling (16.2)].
2.4 Intravenous administration
APIDRA can be administered intravenously under medical supervision for glycemic control with close monitoring of blood glucose and serum potassium to avoid hypoglycemia and hypokalemia. For intravenous use, APIDRA should be used at concentrations of 0.05 Units/mL to 1 Unit/mL insulin glulisine in infusion systems using polyvinyl chloride (PVC) bags. APIDRA has been shown to be stable only in normal saline solution (0.9% sodium chloride). Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit. Do not administer insulin mixtures intravenously.
3 DOSAGE FORMS AND STRENGTHS
APIDRA 100 units per mL (U-100) is available as:
- 10 mL vials
- 3 mL cartridges for use in the OptiClik® Insulin Delivery Device
- 3 mL SoloStar prefilled pen
4 CONTRAINDICATIONS
APIDRA is contraindicated:
- during episodes of hypoglycemia
- in patients who are hypersensitive to APIDRA or to any of its excipients
When used in patients with known hypersensitivity to APIDRA or its excipients, patients may develop localized or generalized hypersensitivity reactions [See Adverse Reactions (6.1)].
5 WARNINGS AND PRECAUTIONS
5.1 Dosage adjustment and monitoring
Glucose monitoring is essential for patients receiving insulin therapy. Changes to an insulin regimen should be made cautiously and only under medical supervision. Changes in insulin strength, manufacturer, type, or method of administration may result in the need for a change in insulin dose. Concomitant oral antidiabetic treatment may need to be adjusted.
As with all insulin preparations, the time course of action for APIDRA may vary in different individuals or at different times in the same individual and is dependent on many conditions, including the site of injection, local blood supply, or local temperature. Patients who change their level of physical activity or meal plan may require adjustment of insulin dosages.
5.2 Hypoglycemia
Hypoglycemia is the most common adverse reaction of insulin therapy, including APIDRA. The risk of hypoglycemia increases with tighter glycemic control. Patients must be educated to recognize and manage hypoglycemia. Severe hypoglycemia may lead to unconsciousness and/or convulsions and may result in temporary or permanent impairment of brain function or death. Severe hypoglycemia requiring the assistance of another person and/or parenteral glucose infusion or glucagon administration has been observed in clinical trials with insulin, including trials with APIDRA.
The timing of hypoglycemia usually reflects the time-action profile of the administered insulin formulations. Other factors such as changes in food intake (e.g., amount of food or timing of meals), injection site, exercise, and concomitant medications may also alter the risk of hypoglycemia [See Drug Interactions (7)].
As with all insulins, use caution in patients with hypoglycemia unawareness and in patients who may be predisposed to hypoglycemia (e.g., the pediatric population and patients who fast or have erratic food intake). The patient's ability to concentrate and react may be impaired as a result of hypoglycemia. This may present a risk in situations where these abilities are especially important, such as driving or operating other machinery.
Rapid changes in serum glucose levels may induce symptoms similar to hypoglycemia in persons with diabetes, regardless of the glucose value. Early warning symptoms of hypoglycemia may be different or less pronounced under certain conditions, such as longstanding diabetes, diabetic nerve disease, use of medications such as beta-blockers [See Drug Interactions (7)], or intensified diabetes control. These situations may result in severe hypoglycemia (and, possibly, loss of consciousness) prior to the patient's awareness of hypoglycemia.
Intravenously administered insulin has a more rapid onset of action than subcutaneously administered insulin, requiring closer monitoring for hypoglycemia.
5.3 Hypersensitivity and allergic reactions
Severe, life-threatening, generalized allergy, including anaphylaxis, can occur with insulin products, including APIDRA [See Adverse reactions (6.1)].
5.4 Hypokalemia
All insulin products, including APIDRA, cause a shift in potassium from the extracellular to intracellular space, possibly leading to hypokalemia. Untreated hypokalemia may cause respiratory paralysis, ventricular arrhythmia, and death. Use caution in patients who may be at risk for hypokalemia (e.g., patients using potassium-lowering medications, patients taking medications sensitive to serum potassium concentrations). Monitor glucose and potassium frequently when APIDRA is administered intravenously.
5.5 Renal or hepatic impairment
Frequent glucose monitoring and insulin dose reduction may be required in patients with renal or hepatic impairment [See Clinical Pharmacology (12.4)].
5.6 Mixing of insulins
APIDRA for subcutaneous injection should not be mixed with insulin preparations other than NPH insulin. If APIDRA is mixed with NPH insulin, APIDRA should be drawn into the syringe first. Injection should occur immediately after mixing.
Do not mix APIDRA with other insulins for intravenous administration or for use in a continuous subcutaneous infusion pump.
APIDRA for intravenous administration should not be diluted with solutions other than 0.9% sodium chloride (normal saline). The efficacy and safety of mixing APIDRA with diluents or other insulins for use in external subcutaneous infusion pumps have not been established.
5.7 Subcutaneous insulin infusion pumps
When used in an external insulin pump for subcutaneous infusion, APIDRA should not be diluted or mixed with any other insulin. APIDRA in the reservoir should be changed at least every 48 hours. APIDRA should not be exposed to temperatures greater than 98.6°F (37°C).
Malfunction of the insulin pump or infusion set or insulin degradation can rapidly lead to hyperglycemia and ketosis. Prompt identification and correction of the cause of hyperglycemia or ketosis is necessary. Interim subcutaneous injections with APIDRA may be required. Patients using continuous subcutaneous insulin infusion pump therapy must be trained to administer insulin by injection and have alternate insulin therapy available in case of pump failure. [See Dosage and Administration (2.3), How Supplied/Storage and Handling (16), and Patient Counseling Information (17.2)].
5.8 Intravenous administration
When APIDRA is administered intravenously, glucose and potassium levels must be closely monitored to avoid potentially fatal hypoglycemia and hypokalemia.
Do not mix APIDRA with other insulins for intravenous administration. APIDRA may be diluted only in normal saline solution.
5.9 Drug interactions
Some medications may alter insulin requirements and the risk for hypoglycemia or hyperglycemia [See Drug Interactions (7)].
6 ADVERSE REACTIONS
The following adverse reactions are discussed elsewhere:
- Hypoglycemia [See Warnings and Precautions (5.2)]
- Hypokalemia [See Warnings and Precautions (5.4)]
6.1 Clinical trial experience
Because clinical trials are conducted under widely varying designs, the adverse reaction rates reported in one clinical trial may not be easily compared to those rates reported in another clinical trial, and may not reflect the rates actually observed in clinical practice.
The frequencies of adverse drug reactions during APIDRA clinical trials in patients with type 1 diabetes mellitus and type 2 diabetes mellitus are listed in the tables below.
| APIDRA, % (n=950) | All comparators*, % (n=641) |
|
|---|---|---|
| Nasopharyngitis | 10.6 | 12.9 |
| Hypoglycemia† | 6.8 | 6.7 |
| Upper respiratory tract infection | 6.6 | 5.6 |
| Influenza | 4.0 | 5.0 |
| APIDRA, % (n=883) | Regular human insulin, % (n=883) |
|
|---|---|---|
| Upper respiratory tract infection | 10.5 | 7.7 |
| Nasopharyngitis | 7.6 | 8.2 |
| Edema peripheral | 7.5 | 7.8 |
| Influenza | 6.2 | 4.2 |
| Arthralgia | 5.9 | 6.3 |
| Hypertension | 3.9 | 5.3 |
- Pediatrics
Table 3 summarizes the adverse reactions occurring with frequency higher than 5% in a clinical study in children and adolescents with type 1 diabetes treated with APIDRA (n=277) or insulin lispro (n=295).
| APIDRA, % (n=277) | Lispro, % (n=295) |
|
|---|---|---|
| Nasopharyngitis | 9.0 | 9.5 |
| Upper respiratory tract infection | 8.3 | 10.8 |
| Headache | 6.9 | 11.2 |
| Hypoglycemic seizure | 6.1 | 4.7 |
- Severe symptomatic hypoglycemia
Hypoglycemia is the most commonly observed adverse reaction in patients using insulin, including APIDRA [See Warnings and Precautions (5.2)]. The rates and incidence of severe symptomatic hypoglycemia, defined as hypoglycemia requiring intervention from a third party, were comparable for all treatment regimens (see Table 4). In the phase 3 clinical trial, children and adolescents with type 1 diabetes had a higher incidence of severe symptomatic hypoglycemia in the two treatment groups compared to adults with type 1 diabetes. (see Table 4) [See Clinical Studies (14)].
| Type 1 Diabetes Adults 12 weeks with insulin glargine | Type 1 Diabetes Adults 26 weeks with insulin glargine | Type 2 Diabetes Adults 26 weeks with NPH human insulin | Type 1 Diabetes Pediatrics 26 weeks |
||||||
|---|---|---|---|---|---|---|---|---|---|
| APIDRA Pre-meal | APIDRA Post-meal | Regular Human Insulin | APIDRA | Insulin Lispro | APIDRA | Regular Human Insulin | APIDRA | Insulin Lispro | |
|
|||||||||
| Events per month per patient | 0.05 | 0.05 | 0.13 | 0.02 | 0.02 | 0.00 | 0.00 | 0.09 | 0.08 |
| Percent of patients (n/total N) | 8.4% (24/286) | 8.4% (25/296) | 10.1% (28/278) | 4.8% (16/339) | 4.0% (13/333) | 1.4% (6/416) | 1.2% (5/420) | 16.2% (45/277) | 19.3% (57/295) |
- Insulin initiation and intensification of glucose control
Intensification or rapid improvement in glucose control has been associated with a transitory, reversible ophthalmologic refraction disorder, worsening of diabetic retinopathy, and acute painful peripheral neuropathy. However, long-term glycemic control decreases the risk of diabetic retinopathy and neuropathy.
- Lipodystrophy
Long-term use of insulin, including APIDRA, can cause lipodystrophy at the site of repeated insulin injections or infusion. Lipodystrophy includes lipohypertrophy (thickening of adipose tissue) and lipoatrophy (thinning of adipose tissue), and may affect insulin absorption. Rotate insulin injection or infusion sites within the same region to reduce the risk of lipodystrophy. [See Dosage and Administration (2.2, 2.3)].
- Weight gain
Weight gain can occur with insulin therapy, including APIDRA, and has been attributed to the anabolic effects of insulin and the decrease in glucosuria.
- Peripheral Edema
Insulin, including APIDRA, may cause sodium retention and edema, particularly if previously poor metabolic control is improved by intensified insulin therapy.
- Adverse Reactions with Continuous Subcutaneous Insulin Infusion (CSII)
In a 12-week randomized study in patients with type 1 diabetes (n=59), the rates of catheter occlusions and infusion site reactions were similar for APIDRA and insulin aspart treated patients (Table 5).
| APIDRA (n=29) | insulin aspart (n=30) |
|
|---|---|---|
| Catheter occlusions/month | 0.08 | 0.15 |
| Infusion site reactions | 10.3% (3/29) | 13.3% (4/30) |
- Allergic Reactions
Local Allergy
As with any insulin therapy, patients taking APIDRA may experience redness, swelling, or itching at the site of injection. These minor reactions usually resolve in a few days to a few weeks, but in some occasions may require discontinuation of APIDRA. In some instances, these reactions may be related to factors other than insulin, such as irritants in a skin cleansing agent or poor injection technique.
Systemic Allergy
Severe, life-threatening, generalized allergy, including anaphylaxis, may occur with any insulin, including APIDRA. Generalized allergy to insulin may cause whole body rash (including pruritus), dyspnea, wheezing, hypotension, tachycardia, or diaphoresis.
In controlled clinical trials up to 12 months duration, potential systemic allergic reactions were reported in 79 of 1833 patients (4.3%) who received APIDRA and 58 of 1524 patients (3.8%) who received the comparator short-acting insulins. During these trials treatment with APIDRA was permanently discontinued in 1 of 1833 patients due to a potential systemic allergic reaction.
Localized reactions and generalized myalgias have been reported with the use of metacresol, which is an excipient of APIDRA.
Antibody Production
In a study in patients with type 1 diabetes (n=333), the concentrations of insulin antibodies that react with both human insulin and insulin glulisine (cross-reactive insulin antibodies) remained near baseline during the first 6 months of the study in the patients treated with APIDRA. A decrease in antibody concentration was observed during the following 6 months of the study. In a study in patients with type 2 diabetes (n=411), a similar increase in cross-reactive insulin antibody concentration was observed in the patients treated with APIDRA and in the patients treated with human insulin during the first 9 months of the study. Thereafter the concentration of antibodies decreased in the APIDRA patients and remained stable in the human insulin patients. There was no correlation between cross-reactive insulin antibody concentration and changes in HbA1c, insulin doses, or incidence of hypoglycemia. The clinical significance of these antibodies is not known.
APIDRA did not elicit a significant antibody response in a study of children and adolescents with type 1 diabetes.
6.2 Postmarketing experience
The following adverse reactions have been identified during post-approval use of APIDRA.
Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to estimate reliably their frequency or establish a causal relationship to drug exposure.
Medication errors have been reported in which other insulins, particularly long-acting insulins, have been accidentally administered instead of APIDRA [See Patient Counseling Information (17)].
7 DRUG INTERACTIONS
A number of drugs affect glucose metabolism and may necessitate insulin dose adjustment and particularly close monitoring.
Drugs that may increase the blood glucose-lowering effect of insulins including APIDRA, and therefore increase the risk of hypoglycemia, include oral antidiabetic products, pramlintide, ACE inhibitors, disopyramide, fibrates, fluoxetine, monoamine oxidase inhibitors, propoxyphene, pentoxifylline, salicylates, somatostatin analogs, and sulfonamide antibiotics.
Drugs that may reduce the blood-glucose-lowering effect of APIDRA include corticosteroids, niacin, danazol, diuretics, sympathomimetic agents (e.g., epinephrine, albuterol, terbutaline), glucagon, isoniazid, phenothiazine derivatives, somatropin, thyroid hormones, estrogens, progestogens (e.g., in oral contraceptives), protease inhibitors, and atypical antipsychotics.
Beta-blockers, clonidine, lithium salts, and alcohol may either increase or decrease the blood-glucose-lowering effect of insulin.
Pentamidine may cause hypoglycemia, which may sometimes be followed by hyperglycemia.
The signs of hypoglycemia may be reduced or absent in patients taking anti-adrenergic drugs such as beta-blockers, clonidine, guanethidine, and reserpine.
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category C: Reproduction and teratology studies have been performed with insulin glulisine in rats and rabbits using regular human insulin as a comparator. Insulin glulisine was given to female rats throughout pregnancy at subcutaneous doses up to 10 Units/kg once daily (dose resulting in an exposure 2 times the average human dose, based on body surface area comparison) and did not have any remarkable toxic effects on embryo-fetal development.
Insulin glulisine was given to female rabbits throughout pregnancy at subcutaneous doses up to 1.5 Units/kg/day (dose resulting in an exposure 0.5 times the average human dose, based on body surface area comparison). Adverse effects on embryo-fetal development were only seen at maternal toxic dose levels inducing hypoglycemia. Increased incidence of post-implantation losses and skeletal defects were observed at a dose level of 1.5 Units/kg once daily (dose resulting in an exposure 0.5 times the average human dose, based on body surface area comparison) that also caused mortality in dams. A slight increased incidence of post-implantation losses was seen at the next lower dose level of 0.5 Units/kg once daily (dose resulting in an exposure 0.2 times the average human dose, based on body surface area comparison) which was also associated with severe hypoglycemia but there were no defects at that dose. No effects were observed in rabbits at a dose of 0.25 Units/kg once daily (dose resulting in an exposure 0.1 times the average human dose, based on body surface area comparison). The effects of insulin glulisine did not differ from those observed with subcutaneous regular human insulin at the same doses and were attributed to secondary effects of maternal hypoglycemia.
There are no well-controlled clinical studies of the use of APIDRA in pregnant women. Because animal reproduction studies are not always predictive of human response, this drug should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. It is essential for patients with diabetes or a history of gestational diabetes to maintain good metabolic control before conception and throughout pregnancy. Insulin requirements may decrease during the first trimester, generally increase during the second and third trimesters, and rapidly decline after delivery. Careful monitoring of glucose control is essential in these patients.
8.3 Nursing mothers
It is unknown whether insulin glulisine is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when APIDRA is administered to a nursing woman. Use of APIDRA is compatible with breastfeeding, but women with diabetes who are lactating may require adjustments of their insulin doses.
8.4 Pediatric use
The safety and effectiveness of subcutaneous injections of APIDRA have been established in pediatric patients (age 4 to 17 years) with type 1 diabetes [See Clinical Studies (14.4)]. APIDRA has not been studied in pediatric patients with type 1 diabetes younger than 4 years of age and in pediatric patients with type 2 diabetes.
As in adults, the dosage of APIDRA must be individualized in pediatric patients based on metabolic needs and frequent monitoring of blood glucose.
8.5 Geriatric use
In clinical trials (n=2408), APIDRA was administered to 147 patients ≥65 years of age and 27 patients ≥75 years of age. The majority of this small subset of elderly patients had type 2 diabetes. The change in HbA1c values and hypoglycemia frequencies did not differ by age. Nevertheless, caution should be exercised when APIDRA is administered to geriatric patients.
10 OVERDOSAGE
Excess insulin may cause hypoglycemia and, particularly when given intravenously, hypokalemia. Mild episodes of hypoglycemia usually can be treated with oral glucose. Adjustments in drug dosage, meal patterns, or exercise may be needed. More severe episodes of hypoglycemia with coma, seizure, or neurologic impairment may be treated with intramuscular/subcutaneous glucagon or concentrated intravenous glucose. Sustained carbohydrate intake and observation may be necessary because hypoglycemia may recur after apparent clinical recovery. Hypokalemia must be corrected appropriately.
11 DESCRIPTION
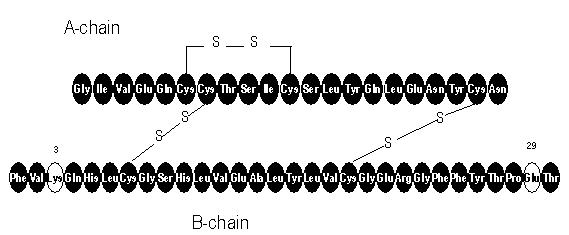
APIDRA® (insulin glulisine [rDNA origin] injection) is a rapid-acting human insulin analog used to lower blood glucose. Insulin glulisine is produced by recombinant DNA technology utilizing a non-pathogenic laboratory strain of Escherichia coli (K12). Insulin glulisine differs from human insulin in that the amino acid asparagine at position B3 is replaced by lysine and the lysine in position B29 is replaced by glutamic acid. Chemically, insulin glulisine is 3B-lysine-29B-glutamic acid-human insulin, has the empirical formula C258H384N64O78S6 and a molecular weight of 5823 and has the following structural formula:
APIDRA is a sterile, aqueous, clear, and colorless solution. Each milliliter of APIDRA contains 100 units (3.49 mg) insulin glulisine, 3.15 mg metacresol, 6 mg tromethamine, 5 mg sodium chloride, 0.01 mg polysorbate 20, and water for injection. APIDRA has a pH of approximately 7.3. The pH is adjusted by addition of aqueous solutions of hydrochloric acid and/or sodium hydroxide.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of action
Regulation of glucose metabolism is the primary activity of insulins and insulin analogs, including insulin glulisine. Insulins lower blood glucose by stimulating peripheral glucose uptake by skeletal muscle and fat, and by inhibiting hepatic glucose production. Insulins inhibit lipolysis and proteolysis, and enhance protein synthesis.
The glucose lowering activities of APIDRA and of regular human insulin are equipotent when administered by the intravenous route. After subcutaneous administration, the effect of APIDRA is more rapid in onset and of shorter duration compared to regular human insulin. [See Pharmacodynamics (12.2)].
12.2 Pharmacodynamics
Studies in healthy volunteers and patients with diabetes demonstrated that APIDRA has a more rapid onset of action and a shorter duration of activity than regular human insulin when given subcutaneously.
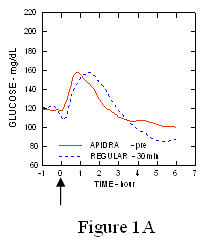
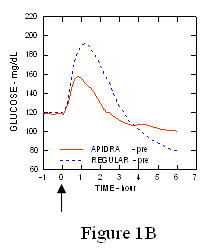
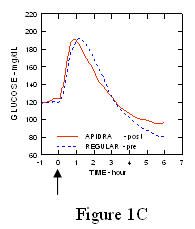
In a study in patients with type 1 diabetes (n= 20), the glucose-lowering profiles of APIDRA and regular human insulin were assessed at various times in relation to a standard meal at a dose of 0.15 Units/kg. (Figure 1.)
The maximum blood glucose excursion (ΔGLUmax; baseline subtracted glucose concentration) for APIDRA injected 2 minutes before a meal was 65 mg/dL compared to 64 mg/dL for regular human insulin injected 30 minutes before a meal (see Figure 1A), and 84 mg/dL for regular human insulin injected 2 minutes before a meal (see Figure 1B). The maximum blood glucose excursion for APIDRA injected 15 minutes after the start of a meal was 85 mg/dL compared to 84 mg/dL for regular human insulin injected 2 minutes before a meal (see Figure 1C).
Figure 1. Serial mean blood glucose collected up to 6 hours following a single dose of APIDRA and regular human insulin. APIDRA given 2 minutes (APIDRA - pre) before the start of a meal compared to regular human insulin given 30 minutes (Regular - 30 min) before start of the meal (Figure 1A) and compared to regular human insulin (Regular - pre) given 2 minutes before a meal (Figure 1B). APIDRA given 15 minutes (APIDRA - post) after start of a meal compared to regular human insulin (Regular - pre) given 2 minutes before a meal (Figure 1C). On the x-axis zero (0) is the start of a 15-minute meal.
 |  |
 |  |
In a randomized, open-label, two-way crossover study, 16 healthy male subjects received an intravenous infusion of APIDRA or regular human insulin with saline diluent at a rate of 0.8 milliUnits/kg/min for two hours. Infusion of the same dose of APIDRA or regular human insulin produced equivalent glucose disposal at steady state.
12.3 Pharmacokinetics
Absorption and bioavailability
Pharmacokinetic profiles in healthy volunteers and patients with diabetes (type 1 or type 2) demonstrated that absorption of insulin glulisine was faster than that of regular human insulin.
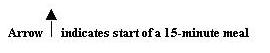
In a study in patients with type 1 diabetes (n=20) after subcutaneous administration of 0.15 Units/kg, the median time to maximum concentration (Tmax) was 60 minutes (range 40 to 120 minutes) and the peak concentration (Cmax) was 83 microUnits/mL (range 40 to 131 microUnits/mL) for insulin glulisine compared to a median Tmax of 120 minutes (range 60 to 239 minutes) and a Cmax of 50 microUnits/mL (range 35 to 71 microUnits/mL) for regular human insulin. (Figure 2)
Figure 2. Pharmacokinetic profiles of insulin glulisine and regular human insulin in patients with type 1 diabetes after a dose of 0.15 Units/kg.
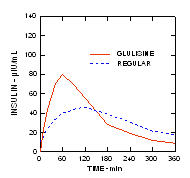
Insulin glulisine and regular human insulin were administered subcutaneously at a dose of 0.2 Units/kg in an euglycemic clamp study in patients with type 2 diabetes (n=24) and a body mass index (BMI) between 20 and 36 kg/m2. The median time to maximum concentration (Tmax) was 100 minutes (range 40 to 120 minutes) and the median peak concentration (Cmax) was 84 microUnits/mL (range 53 to 165 microUnits/mL) for insulin glulisine compared to a median Tmax of 240 minutes (range 80 to 360 minutes) and a median Cmax of 41 microUnits/mL (range 33 to 61 microUnits/mL) for regular human insulin. (Figure 3.)
Figure 3. Pharmacokinetic profiles of insulin glulisine and regular human insulin in patients with type 2 diabetes after a subcutaneous dose of 0.2 Units/kg.
When APIDRA was injected subcutaneously into different areas of the body, the time-concentration profiles were similar. The absolute bioavailability of insulin glulisine after subcutaneous administration is approximately 70%, regardless of injection area (abdomen 73%, deltoid 71%, thigh 68%).
In a clinical study in healthy volunteers (n=32) the total insulin glulisine bioavailability was similar after subcutaneous injection of insulin glulisine and NPH insulin (premixed in the syringe) and following separate simultaneous subcutaneous injections. There was 27% attenuation of the maximum concentration (Cmax) of APIDRA after premixing; however, the time to maximum concentration (Tmax) was not affected. No data are available on mixing APIDRA with insulin preparations other than NPH insulin. [See Clinical Studies (14)].
Distribution and elimination
The distribution and elimination of insulin glulisine and regular human insulin after intravenous administration are similar with volumes of distribution of 13 and 21 L and half-lives of 13 and 17 minutes, respectively. After subcutaneous administration, insulin glulisine is eliminated more rapidly than regular human insulin with an apparent half-life of 42 minutes compared to 86 minutes.
12.4 Clinical pharmacology in specific populations
Pediatric patients
The pharmacokinetic and pharmacodynamic properties of APIDRA and regular human insulin were assessed in a study conducted in children 7 to 11 years old (n=10) and adolescents 12 to 16 years old (n=10) with type 1 diabetes. The relative differences in pharmacokinetics and pharmacodynamics between APIDRA and regular human insulin in these patients with type 1 diabetes were similar to those in healthy adult subjects and adults with type 1 diabetes.
Race
A study in 24 healthy Caucasians and Japanese subjects compared the pharmacokinetics and pharmacodynamics after subcutaneous injection of insulin glulisine, insulin lispro, and regular human insulin. With subcutaneous injection of insulin glulisine, Japanese subjects had a greater initial exposure (33%) for the ratio of AUC(0–1h) to AUC(0–clamp end) than Caucasians (21%) although the total exposures were similar. There were similar findings with insulin lispro and regular human insulin.
Obesity
Insulin glulisine and regular human insulin were administered subcutaneously at a dose of 0.3 Units/kg in a euglycemic clamp study in obese, non-diabetic subjects (n=18) with a body mass index (BMI) between 30 and 40 kg/m2. The median time to maximum concentration (Tmax) was 85 minutes (range 49 to 150 minutes) and the median peak concentration (Cmax) was 192 microUnits/mL (range 98 to 380 microUnits/mL) for insulin glulisine compared to a median Tmax of 150 minutes (range 90 to 240 minutes) and a median Cmax of 86 microUnits/mL (range 43 to 175 microUnits/mL) for regular human insulin.
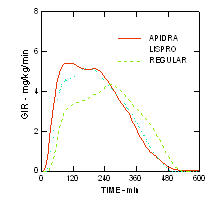
The more rapid onset of action and shorter duration of activity of APIDRA and insulin lispro compared to regular human insulin were maintained in an obese non-diabetic population (n= 18). (Figure 4.)
Figure 4. Glucose infusion rates (GIR) in a euglycemic clamp study after subcutaneous injection of 0.3 Units/kg of APIDRA, insulin lispro or regular human insulin in an obese population.
Renal impairment
Studies with human insulin have shown increased circulating levels of insulin in patients with renal failure. In a study performed in 24 non-diabetic subjects with normal renal function (ClCr >80 mL/min), moderate renal impairment (30–50 mL/min) and severe renal impairment (<30 mL/min), the subjects with moderate and severe renal impairment had increased exposure to insulin glulisine by 29% to 40% and reduced clearance of insulin glulisine by 20% to 25% compared to subjects with normal renal function. [See Warnings and Precautions (5.4)].
Hepatic impairment
The effect of hepatic impairment on the pharmacokinetics and pharmacodynamics of APIDRA has not been studied. Some studies with human insulin have shown increased circulating levels of insulin in patients with liver failure. [See Warnings and Precautions (5.4)].
Gender
The effect of gender on the pharmacokinetics and pharmacodynamics of APIDRA has not been studied.
Pregnancy
The effect of pregnancy on the pharmacokinetics and pharmacodynamics of APIDRA has not been studied.
Smoking
The effect of smoking on the pharmacokinetics and pharmacodynamics of APIDRA has not been studied.
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, mutagenesis, impairment of fertility
Standard 2-year carcinogenicity studies in animals have not been performed. In Sprague Dawley rats, a 12-month repeat dose toxicity study was conducted with insulin glulisine at subcutaneous doses of 2.5, 5, 20 or 50 Units/kg twice daily (dose resulting in an exposure 1, 2, 8, and 20 times the average human dose, based on body surface area comparison).
There was a non-dose dependent higher incidence of mammary gland tumors in female rats administered insulin glulisine compared to untreated controls. The incidence of mammary tumors for insulin glulisine and regular human insulin was similar. The relevance of these findings to humans is not known. Insulin glulisine was not mutagenic in the following tests: Ames test, in vitro mammalian chromosome aberration test in V79 Chinese hamster cells, and in vivo mammalian erythrocyte micronucleus test in rats.
In fertility studies in male and female rats at subcutaneous doses up to 10 Units/kg once daily (dose resulting in an exposure 2 times the average human dose, based on body surface area comparison), no clear adverse effects on male and female fertility, or general reproductive performance of animals were observed.
14 CLINICAL STUDIES
The safety and efficacy of APIDRA was studied in adult patients with type 1 and type 2 diabetes (n =1833) and in children and adolescent patients (4 to 17 years) with type 1 diabetes (n=572). The primary efficacy parameter in these trials was glycemic control, assessed using glycated hemoglobin (GHb reported as HbA1c equivalent).
14.1 Type 1 Diabetes-Adults
A 26-week, randomized, open-label, active-controlled, non-inferiority study was conducted in patients with type 1 diabetes to assess the safety and efficacy of APIDRA (n= 339) compared to insulin lispro (n= 333) when administered subcutaneously within 15 minutes before a meal. Insulin glargine was administered once daily in the evening as the basal insulin. There was a 4-week run-in period with insulin lispro and insulin glargine prior to randomization. Most patients were Caucasian (97%). Fifty eight percent of the patients were men. The mean age was 39 years (range 18 to 74 years). Glycemic control, the number of daily short-acting insulin injections and the total daily doses of APIDRA and insulin lispro were similar in the two treatment groups (Table 6).
| Treatment duration Treatment in combination with: | 26 weeks Insulin glargine |
|
|---|---|---|
| APIDRA | Insulin Lispro | |
|
||
| Glycated hemoglobin (GHb)* (%) | ||
| Number of patients | 331 | 322 |
| Baseline mean | 7.6 | 7.6 |
| Adjusted mean change from baseline | -0.1 | -0.1 |
| Treatment difference: APIDRA – Insulin Lispro | 0.0 | |
| 95% CI for treatment difference | (-0.1; 0.1) | |
| Basal insulin dose (Units/day) | ||
| Baseline mean | 24 | 24 |
| Adjusted mean change from baseline | 0 | 2 |
| Short-acting insulin dose (Units/day) | ||
| Baseline mean | 30 | 31 |
| Adjusted mean change from baseline | -1 | -1 |
| Mean number of short-acting insulin injections per day | 3 | 3 |
| Body weight (kg) | ||
| Baseline mean | 73.9 | 74.1 |
| Mean change from baseline | 0.6 | 0.3 |
14.2 Type 2 Diabetes-Adults
A 26-week, randomized, open-label, active-controlled, non-inferiority study was conducted in insulin-treated patients with type 2 diabetes to assess the safety and efficacy of APIDRA (n= 435) given within 15 minutes before a meal compared to regular human insulin (n=441) administered 30 to 45 minutes prior to a meal. NPH human insulin was given twice a day as the basal insulin. All patients participated in a 4-week run-in period with regular human insulin and NPH human insulin. Eighty-five percent of patients were Caucasian and 11% were Black. The mean age was 58 years (range 26 to 84 years). The average body mass index (BMI) was 34.6 kg/m2. At randomization, 58% of the patients were taking an oral antidiabetic agent. These patients were instructed to continue use of their oral antidiabetic agent at the same dose throughout the trial. The majority of patients (79%) mixed their short-acting insulin with NPH human insulin immediately prior to injection. The reductions from baseline in GHb were similar between the 2 treatment groups (see Table 7). No differences between APIDRA and regular human insulin groups were seen in the number of daily short-acting insulin injections or basal or short-acting insulin doses. (See Table 7.)
| Treatment duration | 26 weeks | |
|---|---|---|
| Treatment in combination with: | NPH human insulin | |
| APIDRA | Regular Human Insulin | |
|
||
| Glycated hemoglobin (GHb)* (%) | ||
| Number of patients | 404 | 403 |
| Baseline mean | 7.6 | 7.5 |
| Adjusted mean change from baseline | -0.5 | -0.3 |
| Treatment difference: APIDRA – Regular Human Insulin | -0.2 | |
| 95% CI for treatment difference | (-0.3; -0.1) | |
| Basal insulin dose (Units/day) | ||
| Baseline mean | 59 | 57 |
| Adjusted mean change from baseline | 6 | 6 |
| Short-acting insulin dose (Units/day) | ||
| Baseline mean | 32 | 31 |
| Adjusted mean change from baseline | 4 | 5 |
| Mean number of short-acting insulin injections per day | 2 | 2 |
| Body weight (kg) | ||
| Baseline mean | 100.5 | 99.2 |
| Mean change from baseline | 1.8 | 2.0 |
14.3 Type 1 Diabetes-Adults: Pre- and post-meal administration
A 12-week, randomized, open-label, active-controlled, non-inferiority study was conducted in patients with type 1 diabetes to assess the safety and efficacy of APIDRA administered at different times with respect to a meal. APIDRA was administered subcutaneously either within 15 minutes before a meal (n=286) or immediately after a meal (n=296) and regular human insulin (n= 278) was administered subcutaneously 30 to 45 minutes prior to a meal. Insulin glargine was administered once daily at bedtime as the basal insulin. There was a 4-week run-in period with regular human insulin and insulin glargine followed by randomization. Most patients were Caucasian (94%). The mean age was 40 years (range 18 to 73 years). Glycemic control (see Table 8) was comparable for the 3 treatment regimens. No changes from baseline between the treatments were seen in the total daily number of short-acting insulin injections. (See Table 8.)
| Treatment duration Treatment in combination with: | 12 weeks insulin glargine | 12 weeks insulin glargine | 12 weeks insulin glargine |
|---|---|---|---|
| APIDRA pre meal | APIDRA post meal | Regular Human Insulin | |
| Glycated hemoglobin (GHb)* (%) | |||
| Number of patients | 268 | 276 | 257 |
| Baseline mean | 7.7 | 7.7 | 7.6 |
| Adjusted mean change from baseline† | -0.3 | -0.1 | -0.1 |
| Basal insulin dose (Units/day) | |||
| Baseline mean | 29 | 29 | 28 |
| Adjusted mean change from baseline | 1 | 0 | 1 |
| Short-acting insulin dose (Units/day) | |||
| Baseline mean | 29 | 29 | 27 |
| Adjusted mean change from baseline | -1 | -1 | 2 |
| Mean number of short-acting insulin injections per day | 3 | 3 | 3 |
| Body weight (kg) | |||
| Baseline mean | 79.2 | 80.3 | 78.9 |
| Mean change from baseline | 0.3 | -0.3 | 0.3 |
14.4 Type 1 Diabetes-Pediatric patients
A 26-week, randomized, open-label, active-controlled, non-inferiority study was conducted in children and adolescents older than 4 years of age with type 1 diabetes mellitus to assess the safety and efficacy of APIDRA (n= 277) compared to insulin lispro (n= 295) when administered subcutaneously within 15 minutes before a meal. Patients also received insulin glargine (administered once daily in the evening) or NPH insulin (administered once in the morning and once in the evening). There was a 4-week run-in period with insulin lispro and insulin glargine or NPH prior to randomization. Most patients were Caucasian (91%). Fifty percent of the patients were male. The mean age was 12.5 years (range 4 to 17 years). Mean BMI was 20.6 kg/m2. Glycemic control (see Table 9) was comparable for the two treatment regimens.
| APIDRA | Lispro | |
|---|---|---|
| Number of patients | 271 | 291 |
| Basal Insulin | NPH or insulin glargine | NPH or insulin glargine |
|
||
| Glycated hemoglobin (GHb)* (%) | ||
| Baseline mean | 8.2 | 8.2 |
| Adjusted mean change from baseline | 0.1 | 0.2 |
| Treatment Difference: Mean (95% confidence interval) | -0.1 (-0.2, 0.1) | |
| Basal insulin dose (Units/kg/day) | ||
| Baseline mean | 0.5 | 0.5 |
| Mean change from baseline | 0.0 | 0.0 |
| Short-acting insulin dose (Units/kg/day) | ||
| Baseline mean | 0.5 | 0.5 |
| Mean change from baseline | 0.0 | 0.0 |
| Mean number of short-acting insulin injections per day | 3 | 3 |
| Baseline mean body weight (kg) | 51.5 | 50.8 |
| Mean weight change from baseline (kg) | 2.2 | 2.2 |
14.5 Type 1 Diabetes-Adults: Continuous subcutaneous insulin infusion
A 12-week randomized, active control study (APIDRA versus insulin aspart) conducted in adults with type 1 diabetes (APIDRA n= 29, insulin aspart n=30) evaluated the use of APIDRA in an external continuous subcutaneous insulin pump. All patients were Caucasian. The mean age was 46 years (range 21 to 73 years). The mean GHb increased from baseline to endpoint in both treatment groups (from 6.8% to 7.0% for APIDRA; from 7.1% to 7.2% for insulin aspart).
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How supplied
|
|
| APIDRA 100 units per mL (U-100) is available as: | |
| 10 mL vials | NDC 0088-2500-33 |
| 3 mL cartridge system*, package of 5 | NDC 0088-2500-52 |
| 3 mL SoloStar prefilled pen, package of 5 | NDC 0088-2502-05 |
Pen needles are not included in the packs.
BD Ultra-Fine™ pen needles1 to be used in conjunction with OptiClik are sold separately and are manufactured by Becton Dickinson and Company.
Solostar is compatible with all pen needles from Becton Dickinson and Company, Ypsomed and Owen Mumford.
16.2 Storage
Do not use after the expiration date (see carton and container).
Unopened Vial/Cartridge System/SoloStar
Unopened APIDRA vials, cartridge systems and SoloStar should be stored in a refrigerator, 36°F–46°F (2°C–8°C). Protect from light. APIDRA should not be stored in the freezer and it should not be allowed to freeze. Discard if it has been frozen.
Unopened vials/cartridge systems/SoloStar not stored in a refrigerator must be used within 28 days.
Open (In-Use) Vial:
Opened vials, whether or not refrigerated, must be used within 28 days. If refrigeration is not possible, the open vial in use can be kept unrefrigerated for up to 28 days away from direct heat and light, as long as the temperature is not greater than 77°F (25°C).
Open (In-Use) Cartridge System:
The opened (in-use) cartridge system inserted in OptiClik® should NOT be refrigerated but should be kept below 77°F (25°C) away from direct heat and light. The opened (in-use) cartridge system must be discarded after 28 days. Do not store OptiClik®, with or without cartridge system, in a refrigerator at any time.
Open (In-Use) SoloStar prefilled pen:
The opened (in-use) SoloStar should NOT be refrigerated but should be kept below 77°F (25°C) away from direct heat and light. The opened (in-use) SoloStar kept at room temperature must be discarded after 28 days.
Infusion sets:
Infusion sets (reservoirs, tubing, and catheters) and the APIDRA in the reservoir should be discarded after 48 hours of use or after exposure to temperatures that exceed 98.6°F (37°C).
Intravenous use:
Infusion bags prepared as indicated under DOSAGE AND ADMINISTRATION (2.4) are stable at room temperature for 48 hours.
16.3 Preparation and handling
After dilution for intravenous use, the solution should be inspected visually for particulate matter and discoloration prior to administration. Do not use the solution if it has become cloudy or contains particles; use only if it is clear and colorless. APIDRA is not compatible with Dextrose solution and Ringers solution and, therefore, cannot be used with these solution fluids. The use of APIDRA with other solutions has not been studied and is, therefore, not recommended.
Cartridge system: If OptiClik® (the Insulin Delivery Device for APIDRA) malfunctions, APIDRA may be drawn from the cartridge system into a U-100 syringe and injected.
17 PATIENT COUNSELING INFORMATION
See FDA-approved patient labeling.
17.1 Instructions for all patients
Patients should be instructed on self-management procedures including glucose monitoring, proper injection technique, and management of hypoglycemia and hyperglycemia.
Patients must be instructed on handling of special situations such as intercurrent conditions (illness, stress, or emotional disturbances), an inadequate or skipped insulin dose, inadvertent administration of an increased insulin dose, inadequate food intake, and skipped meals.
Refer patients to the APIDRA Patient Information Leaflet for additional information.
Women with diabetes should be advised to inform their doctor if they are pregnant or are contemplating pregnancy.
Accidental mix-ups between APIDRA and other insulins, particularly long-acting insulins, have been reported. To avoid medication errors between APIDRA and other insulins, patients should be instructed to always check the insulin label before each injection.
17.2 For patients using continuous subcutaneous insulin pumps
Patients using external pump infusion therapy should be trained appropriately.
The following insulin pumps1 have been used in APIDRA clinical trials conducted by sanofi-aventis, the manufacturer of APIDRA:
- Disetronic® H-Tron® plus V100 and D-Tron® with Disetronic catheters (Rapid™, Rapid C™, Rapid D™, and Tender™)
- MiniMed® Models 506, 507, 507c and 508 with MiniMed catheters (Sof-set Ultimate QR™, and Quick-set™).
Before using a different insulin pump with APIDRA, read the pump label to make sure the pump has been evaluated with APIDRA.
To minimize insulin degradation, infusion set occlusion, and loss of the preservative (metacresol), the infusion sets (reservoir, tubing, and catheter) and the APIDRA in the reservoir should be replaced every 48 hours and a new infusion site should be selected. The temperature of the insulin may exceed ambient temperature when the pump housing, cover, tubing or sport case is exposed to sunlight or radiant heat. Insulin exposed to temperatures higher than 98.6°F (37°C) should be discarded. Infusion sites that are erythematous, pruritic, or thickened should be reported to the healthcare professional, and a new site selected because continued infusion may increase the skin reaction or alter the absorption of APIDRA.
Pump or infusion set malfunctions or insulin degradation can lead to rapid hyperglycemia and ketosis. This is especially pertinent for rapid-acting insulin analogs that are more rapidly absorbed through skin and have a shorter duration of action. Prompt identification and correction of the cause of hyperglycemia or ketosis is necessary. Problems include pump malfunction, infusion set occlusion, leakage, disconnection or kinking, and degraded insulin. Less commonly, hypoglycemia from pump malfunction may occur. If these problems cannot be promptly corrected, patients should resume therapy with subcutaneous insulin injection and contact their healthcare professional. [See Dosage and Administration (2.3), Warnings and Precautions (5.7), and How Supplied/Storage and Handling (16)].
- 1
- The brands listed are the registered trademarks of their respective owners and are not trademarks of sanofi-aventis U.S. LLC
sanofi-aventis U.S. LLC
Bridgewater, NJ 08807
©2009 sanofi-aventis U.S. LLC
Patient Information
APIDRA (uh PEE druh)
(insulin glulisine [recombinant DNA origin] injection)
solution for injection
Read the Patient Information that comes with APIDRA before you start taking it and each time you get a refill. There may be new information. This leaflet does not take the place of talking with your healthcare provider about your diabetes or treatment. If you have questions about APIDRA or about diabetes, talk with your healthcare provider.
What is APIDRA?
APIDRA is a man-made insulin used to control high blood sugar in adults and children with diabetes mellitus.
It is not known if APIDRA is safe or effective in:
- children under age 4 with type 1 diabetes
- children with type 2 diabetes
Who should NOT take APIDRA?
Do not take APIDRA:
- when your blood sugar is too low (hypoglycemia). See the section, "What are the possible side effects of APIDRA?"
- if you are allergic to any of the ingredients in APIDRA. See the end of this leaflet for a complete list of ingredients. Ask your healthcare provider if you are not sure.
What should I tell my healthcare provider before taking APIDRA?
Medical conditions can affect your insulin needs. Tell your healthcare provider about all of your medical conditions, including if you:
- have liver or kidney problems.
- are pregnant, plan to become pregnant, or are breast-feeding. It is not known if APIDRA will harm your unborn baby or nursing child. You and your healthcare provider should talk about the best way to manage your diabetes while you are pregnant or breast-feeding. It is especially important to keep good control of your blood sugar during pregnancy.
Tell your healthcare provider about all the medicines you take, including prescription and non-prescription medicines, vitamins, and herbal supplements.
Know the medicines you take. Keep a list of your medicines with you and show it to your healthcare provider and pharmacist when you get a new medicine.
How should I take APIDRA?
- Take APIDRA exactly as prescribed.
- Do not make any changes to your dose or type of insulin unless told to do so by your healthcare provider.
- Know your insulin. Make sure you know:
- the type and strength of insulin prescribed for you
- the amount of insulin you take
- the best time for you to take your insulin. This may change if you take a different type of insulin or if the way you give your insulin changes for example, using an insulin pump instead of giving injections under the skin (subcutaneous injections).
- APIDRA starts working faster than regular insulin, but does not work as long.
- APIDRA is usually used with a longer-acting insulin when given by injection under the skin (subcutaneous), or by itself when using an insulin pump.
- Read the instructions for use that come with your APIDRA. Talk to your healthcare provider if you have any questions. Your healthcare provider should show you how to inject APIDRA before you start taking it.
- Your healthcare provider will prescribe the best type of APIDRA for you. APIDRA is available in:
- 3 mL cartridge system for use in OptiClik® Insulin Delivery Device
- 3 mL SoloStar® prefilled pen
- 10 mL vials
- Check your blood sugar level before each use of APIDRA. Ask your healthcare provider what your blood sugars should be and when you should check your blood sugar levels.
- Check the label to make sure you have the correct insulin type. This is especially important if you also take long-acting insulin.
- APIDRA should look clear and colorless. Do not use APIDRA if it looks cloudy, colored, or has particles in it. Talk with your pharmacist or healthcare provider if you have any questions.
- If you take to much APIDRA, your blood sugar may fall low (hypoglycemia). You can treat mild low blood sugar (hypoglycemia) by drinking or eating something sugary right away.
- Do not share needles, insulin pens or syringes with others.
Your dose of APIDRA may need to be changed because of:
|
|
Check your blood sugar and stay on the diet and exercise plan as prescribed by your healthcare provider.
What should I consider while taking APIDRA?
- Alcohol may affect your blood sugar when you take APIDRA
-
Driving and operating machinery. You may have trouble paying attention or reacting if you have low blood sugar (hypoglycemia). Be careful when you drive a car or operate machinery. Ask your healthcare provider if it is alright for you to drive if you have:
- low blood sugar (hypoglycemia)
- decreased or no warning signs of low blood sugar
What are the possible side effects of APIDRA?
APIDRA can cause serious side effects, including:
-
Low blood sugar (hypoglycemia). Symptoms of low blood sugar may include:
- feeling anxious, or irritable, mood changes
- trouble concentrating or feeling confused
- tingling in your hands, feet, lips, or tongue
- feeling dizzy, light-headed, or drowsy
- nightmares or trouble sleeping
- headache
- blurred vision
- slurred speech
- a fast heart beat
- sweating
- shakiness
- walking unsteady
Very low blood sugar (hypoglycemia) can cause unconsciousness (passing out), seizures, and death. Talk to your healthcare provider about how to tell if you have low blood sugar and what to do if this happens while taking APIDRA. Know your symptoms of low blood sugar. Follow your healthcare provider’s instructions for treating your low blood sugar.
Talk to your healthcare provider if low blood sugar is a problem for you. Your dose of APIDRA may need to be changed.
-
Serious allergic reactions.
Get medical help right away if you have any of these symptoms of a severe allergic reaction:
- a rash all over your body
- shortness of breath
- trouble breathing (wheezing)
- fast pulse
- sweating
- feel faint (due to low blood pressure)
- Low potassium in your blood. Your doctor will check you for this.
Common side effects include:
- Reactions at the injection site (local allergic reaction). You may get redness, swelling and itching at the injection site. If you keep having skin reactions or they are serious talk to your healthcare provider.
- Skin thickening or pits at the injection site. Do not inject insulin into skin where this has happened. Choose an injection area (upper arm, thigh, or stomach area). Change injection sites within the area you choose with each dose. Do not inject into the exact same spot for each injection.
- Weight gain
Tell your healthcare provider about any side effect that bothers you or that does not go away. These are not all of the possible side effects of APIDRA.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-332-1088.
- See the Patient Instructions for Use that come with your APIDRA for specific storage instructions.
Unopened APIDRA:
- Do not use APIDRA after the expiration date stamped on the label.
- Keep all unopened APIDRA in the refrigerator between 36°F to 46°F (2°C to 8°C).
- Do not freeze. Do not use APIDRA if it has been frozen.
- Keep APIDRA away from direct heat and light.
- Unopened vials, cartridge systems and SoloStar that were not kept in a refrigerator must be used within 28 days after opening.
General Information about APIDRA
Medicines are sometimes prescribed for conditions that are not mentioned in patient information leaflets. Do not use APIDRA for a condition for which it was not prescribed. Do not give APIDRA to other people, even if they have the same symptoms you have. It may harm them.
This leaflet summarizes the most important information about APIDRA. If you would like more information, talk with your healthcare provider. You can ask your healthcare provider for information about APIDRA that is written for healthcare providers. For more information about APIDRA call 1-800-633-1610 or go to www.apidra.com.
What are the ingredients in APIDRA?
Active ingredient: insulin glulisine
Inactive ingredients: metacresol, tromethamine, sodium chloride, polysorbate 20, water for injection, hydrochloric acid or sodium hydroxide
ADDITIONAL INFORMATION
DIABETES FORECAST is a national magazine designed especially for patients with diabetes and their families and is available by subscription from the American Diabetes Association, (ADA), P.O. Box 363, Mt. Morris, IL 61054-0363, 1-800-DIABETES (1-800-342-2383). You may also visit the ADA website at www.diabetes.org.
Another publication, COUNTDOWN, is available from the Juvenile Diabetes Research Foundation International (JDRF), 120 Wall Street, 19th Floor, New York, New York 10005, 1-800-JDF-CURE (1-800-533-2873). You may also visit the JDRF website at www.jdf.org.
To get more information about diabetes, check with your healthcare provider or diabetes educator or visit www.DiabetesWatch.com.
For more information about APIDRA or OptiClik® call 1-800-633-1610 or visit www.apidra.com or www.opticlik.com.
Rev. February 2009
sanofi-aventis U.S. LLC
Bridgewater NJ 08807
©2009 sanofi-aventis U.S. LLC
PATIENT INSTRUCTIONS FOR USE
APIDRA 10 mL vial (100 Units/mL)
This Instructions for Use has two parts:
Part 1 Use with a syringe
Part 2 Use with an external insulin infusion pump
Be sure to read, understand and follow these instructions before taking APIDRA.
If you will give yourself subcutaneous injections of APIDRA:
- You should take APIDRA within 15 minutes before a meal or within 20 minutes after starting a meal.
- Do not inject APIDRA if you are not going to eat within 15 minutes.
- Inject APIDRA into the skin of your upper arm, thigh, or stomach area. Do not inject APIDRA into a vein or into a muscle.
- Choose an injection area (upper arm, thigh, or stomach area). Change injection sites within the area you choose with each dose. Do not inject into the exact same spot for each injection.
- Do not mix APIDRA with insulins other than NPH, for subcutaneous injections. If mixing APIDRA with NPH insulin, draw up APIDRA into the syringe first. Inject the mixture right away.
- Use the needles and syringes prescribed by your healthcare provider.
Before every injection make sure you have the following items:
- Alcohol swabs
- Needle and syringe
- Insulin vial
- Puncture resistant container. See "How do I dispose of used needles and syringes?".
Drawing the insulin into a syringe
- 1.
- Use a new syringe each time you give an injection of APIDRA.
Preparing for an injection
- 2.
- Wash your hands with soap and water. Before you start to prepare your injection, check the label to make sure that you are taking the right type of insulin.
- 3.
- Look at the APIDRA in the vial. It should look clear. Do not use this vial of APIDRA if the solution is colored, or cloudy, or if you see particles in it.
- 4.
- If you are using a new vial, remove the protective cap. Do not remove the stopper.

- 5.
- Wipe the rubber stopper with an alcohol swab. You do not have to shake the vial of APIDRA before use.

- 6.
- Use the needles and syringes prescribed by your healthcare provider. APIDRA 10 mL vials come with 100 units of insulin in 1 mL of APIDRA.
- 7.
- Use a new needle and syringe for each injection. Use disposable syringes and needles only one time.
- 8.
- Draw air into the syringe equal to the insulin dose prescribed by your healthcare provider.

- 9.
- Put the needle through the rubber stopper of the vial and push the plunger to inject the air into the vial.

- 10.
- Leave the syringe in the vial and turn both upside down. Hold the syringe and vial firmly in one hand.
- 11.
- Make sure the tip of the needle is in the insulin solution. With your free hand, pull back on the plunger to draw the correct dose of insulin into the syringe.

- 12
- Before you take the needle out of the vial, check the syringe for air bubbles. If you see bubbles in the syringe, hold the syringe straight up and tap the side of the syringe with your finger a few times to make any air bubbles float to the top. Gently push the air bubbles out with the plunger and draw insulin back into the syringe until you have the correct dose. If you are mixing APIDRA with NPH insulin, check with your healthcare provider on how to mix it the right way.

- 13.
- Remove the needle from the vial. Do not let the needle touch anything. You are now ready to inject.
Giving the injection
Do the injection exactly as shown to you by your healthcare provider. Inject APIDRA under your skin.
- 14.
- Choose an injection area (for example upper arm, thigh or stomach area). Change injection sites within the area you choose. Do not inject in the same spot.
- 15.
- Clean the area with an alcohol swab. Let the injection site dry before you inject.

- 16.
- Pinch the skin. Insert the needle into the skin. Release the skin.
- 17.
- Inject the dose by slowly pushing in the plunger of the syringe all the way, making sure you have injected all the insulin. Keep the needle in the skin for at least 10 seconds.

Pull the needle out of your skin, gently press the injection site with a finger for several seconds. Do not rub the area. - 18.
- Do not recap the needle. Recapping can lead to a needle stick injury and passing of infection. See "How do I dispose of used needles and syringes?".
If your injection is given by another person, this person must also be careful to prevent accidental needle stick injury and passing infections.
How do I dispose of used needles and syringes?
- 19.
- Check with your healthcare provider's office for instructions about the right way to dispose of used needles and syringes. There may be local or state laws about how to dispose of used needles and syringes. Do not dispose of used needles or syringes in household trash and do not recycle them.
- 20.
- Put used needles and syringes in a container specially made for throwing away syringes and needles (called a "sharps" container) or a hard plastic container with a screw-on cap or a metal container with a plastic lid labeled "Used Syringes". These containers should be sealed and dispose of the right way.
See "How should I store APIDRA?" in the Patient Information leaflet that comes With APIDRA for complete instructions on how to store APIDRA vials.
Part 2 Use with an external insulin pump:
Be sure to read, understand, and follow these instructions before using APIDRA with an external insulin infusion pump. Always read the instruction manual for your pump.
If you will be using an insulin pump:
- APIDRA should be given into the stomach area.
- Change injection sites in the stomach area.
- Do not mix APIDRA with other insulins and do not dilute APIDRA.
- Use only insulin pumps that have been specially tested with APIDRA.
Follow your healthcare provider or pharmacist instructions for which insulin pumps may be used. - Change the infusion set (reservoir, tubing, and catheter), and the APIDRA in the reservoir every 2 days (48 hours). Change all of these parts sooner if they have been exposed to temperatures higher than 98.6°F (37°C).
Important information about using APIDRA with an external insulin infusion pump
- Do not mix APIDRA with any other insulin or liquid when used in a pump.
- If your APIDRA infusion pump set is not working the right way, you may not get the right amount of insulin that can cause:
- low blood sugar (hypoglycemia)
- high blood sugar (hyperglycemia)
- high amounts of sugar and ketones in your blood or urine
- When you start using APIDRA by infusion pump, your insulin dose may need to be adjusted. Check with your healthcare provider before making any changes to your insulin dose.
How to use APIDRA with an external insulin infusion pump?
- Check with your healthcare provider or pharmacist to see if your pump and infusion set can be used with APIDRA. See the instruction manual of your specific pump on proper use of insulin in a pump. Call your healthcare provider if you have questions about using the pump.
- Change the infusion set, reservoir with insulin, and injection site:
- at least every 48 hours, change more often than every 48 hours if you have high blood sugar (hyperglycemia), or the pump alarm sounds.
- if the insulin has been in temperatures over 98.6°F (37°C). Dark colored pump cases or sport covers can increase this type of heat. The location where the pump is worn may affect the temperature.
If you get reactions at the injections infusion site you may need to change infusion sites more often.
If your APIDRA infusion pump is not working the right way, follow these steps:
- Use insulin from a new vial of APIDRA if infusion pump alarms do not respond to all of the following:
- a repeat injection or bolus of APIDRA
- a change in the infusion set and the reservoir
- a change in the infusion injection site
- If the same problems happen again, do not use your infusion pump with APIDRA. You may need to restart insulin injections with syringes and needles.
- Contact your healthcare provider right away.
- See section I of the Instructions for Use ("Use with a syringe") for the steps for giving injections of APIDRA using syringes and needles.
- Continue to check your blood sugar often.
How should I store APIDRA 10 mL vial?
- Keep in the refrigerator or below 77°F (25°C).
- Keep vials away from direct heat and light.
- Dispose of any opened vial after 28 days after the first use, even if there is insulin left in the vial.
Rev. February 2009
sanofi-aventis U.S. LLC
Bridgewater NJ 08807
©2009 sanofi-aventis U.S. LLC
PATIENT INSTRUCTIONS FOR USE
APIDRA 3 mL cartridge system (100 Units/mL)
Be sure to read, understand, and follow these instructions before using your APIDRA® 3 mL cartridge system. Also read and follow the step-by-step instructions in the "OptiClik® Instructions for Use Leaflet" that comes with OptiClik. If you do not follow the instructions, you may take too much or too little insulin. Your healthcare provider should show you how to use the APIDRA 3 mL cartridge system and OptiClik to inject APIDRA before you use it for the first time. Ask your healthcare provider if you have any questions.
Important Information
If you will give yourself subcutaneous injections of APIDRA:
- You should take APIDRA within 15 minutes before a meal or within 20 minutes after starting a meal.
- Do not inject APIDRA if you are not going to eat within 15 minutes.
- Inject APIDRA into the skin of your upper arm, stomach area, or thigh. Do not inject APIDRA into a vein or into a muscle.
- Choose an injection area (upper arm, thigh, or stomach area). Change injection sites within the area you choose with each dose. Do not inject into the exact same spot for each injection.
- Only use your APIDRA 3 mL cartridge system with OptiClik, a reusable insulin delivery device.
- Use a new needle each time you give an APIDRA injection.
- Use BD Ultra-Fine pen needles with the OptiClik. The needles do not come with the APIDRA 3 mL cartridge system or OptiClik. You will need to buy these from a pharmacy. Talk to your healthcare provider if you have questions.
- Needles, OptiClik and cartridge systems must not be shared.
Getting ready
Make sure you have the following items:
- OptiClik insulin delivery device
- Pen needles
- Alcohol swab
- APIDRA cartridge system
- Puncture resistant container. See "How do I dispose of used needles and cartridge systems?
Preparing for an injection
- Wash your hands with soap and water before you start to touch the cartridge system or the OptiClik.
- Use a new needle for each injection.
- Always perform the safety test before use (see the OptiClik Instruction Leaflet).
- Do not use APIDRA if the solution is colored, cloudy, or if you see particles in it.
- Choose an injection area (for example upper arm, thigh, or stomach area). Change injection sites within the area you choose. Do not inject into the exact same spot for each injection.
- After injecting APIDRA, leave the needle in the skin for at least 10 seconds. Then pull the needle straight out. Gently press the injection site for a few seconds. Do not rub the area.
- Handle OptiClik® with care
- Do not use OptiClik if it is damaged or if you are not sure that it is working correctly.
How do I dispose of used needles and cartridge systems?
- Check with your healthcare provider for instructions about the right way to dispose of used needles and pens. There may be local or state laws about how to dispose of used needles and pens. Do not dispose of used needles or pens in household trash and do not recycle.
- Put used needles and used empty cartridge systems in a container made specially for disposing of used syringes and needles (called a "sharps" container) or a hard plastic container (such as detergent bottles),with a screw-on cap, or metal container with a plastic lid labeled "Used Syringes". These containers should be sealed and disposed of the right way.
How should I store APIDRA cartridge system?
- Store the opened cartridge system in the OptiClik (Insulin Delivery Device) below 77°F (25°C). Do not refrigerate.
- Keep away from direct heat and light.
- Dispose of any used APIDRA cartridge system 28 days after the first use even if there is insulin left in the cartridge.
If your blood glucose reading is high or low, tell your healthcare provider so the dose can be changed.
If you have lost your OptiClik Instruction Leaflet or have a question, go to www.opticlik.com or call 1-800-633-1610.
Rev. February 2009
sanofi-aventis U.S. LLC
Bridgewater NJ 08807
©2009 sanofi-aventis U.S. LLC
OptiClik®
INSTRUCTION LEAFLET
Your healthcare professional has decided that OptiClik® is right for you. Before using OptiClik®, your healthcare provider should provide training for the use of the pen and injection technique, or direct you to the appropriate person to get training.
Read these instructions carefully before using your OptiClik. Read both sides of the leaflet. If you are not able to follow all the instructions completely on your own, use OptiClik only if you have help from a person who is able to follow the instructions.
Hold the pen as shown in this leaflet. The word "OptiClik" must be readable to the left of the digital dose display to ensure the correct reading of the dose.If you do not follow these instructions completely, you may get too much or too little insulin.
OptiClik is a reusable pen for the injection of insulin. You can set doses from 1 to 80 units in steps of 1 unit. OptiClik can only be used with 3 mL (300 units) Lantus or Apidra® cartridge (U-100) systems.
OptiClik is available in different colors. If you use two different types of insulin with OptiClik, you should use a different color pen for each insulin.
Keep this leaflet for future reference for each time you use OptiClik.
If you have any questions about OptiClik or about diabetes, ask your health care professional, go to www.opticlik.com or call sanofi-aventis at 1-800-633-1610.
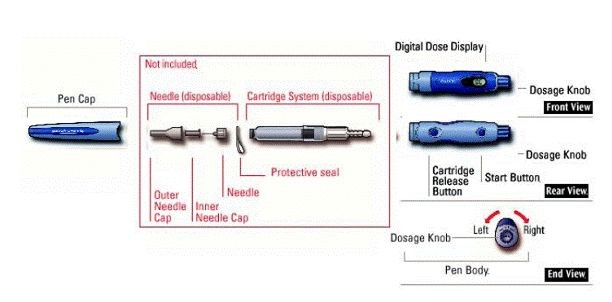
Important information for use of OptiClik:
- Always attach a new needle before each use. BD Ultra-Fine needles are available from BD Consumer Healthcare. Contact your healthcare professional for further information.
- Always perform the safety test before each injection (see Step 4).
- If you use two different types of insulin with OptiClik, you should use a different color pen for each insulin. Always check the label of your insulin before use.
- Accidental pressing of the start button or the cartridge release button may interfere with normal operation. Avoid accidentally pressing these buttons.
- This pen is only for your use. Do not share it with anyone else.
- If your injection is given by another person, special caution must be taken by this person to avoid accidental needle penetration and transmission of infection.
- OptiClik should not be used near electrical and electronic equipment.
- Never use OptiClik if it is damaged or if you are not sure that it is working properly.
- Always have a back-up method for delivering your insulin.
- Do not store your OptiClik in a refrigerator
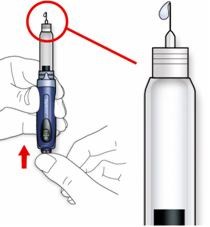
Step 1: Insert a new Cartridge System

- A.
- Make sure the dosage knob is pushed in.
- B.
- Check the label on your cartridge system to make sure you have the correct insulin. Using the wrong insulin may result in unwanted changes in blood sugar that could be harmful to your health.

- C.
- Insert the cartridge system straight into the pen body. Make sure that it clicks in.
- If you meet resistance, wiggle the cartridge system while inserting it.
If the cartridge system does not click into the pen body properly, do not use force:
- Check that the dosage knob is pressed in before you start
- Take the cartridge system out and try again, aligning it carefully.
- Try pressing the release button as you insert the cartridge.
- D.
- Try pulling out the cartridge system. The cartridge system should not come out. Make sure you do not press the cartridge release button during or after this check.
OptiClik is now ready for attaching the needle (Step 3), or it can be stored with the attached pen cap.
- A.
- Take off the pen cap.
- B.
- Check the label on your cartridge system to make sure you have the correct insulin.
- C.
- Check the appearance of your insulin. OptiClik cartridge systems, Lantus or Apidra, only contain clear insulin. Do not use this cartridge system if the insulin is cloudy, colored or has particles.
Always use a new sterile needle for each injection. This helps prevent contamination, and potential needle blocks.
- A.
- Wipe the rubber seal on the end of the cartridge system with alcohol.

- B
- Remove the protective seal from a new needle.

- C.
- Line up the needle with the pen, and keep it straight as you attach it (screw or push on, depending on the needle type.).

-
- If the needle is not kept straight while you attach it, it can damage the rubber seal and cause leakage, or the needle can be bend.
Always perform the safety test before each injection. This ensures that you get an accurate dose by:
- ensuring that pen and needle work properly
- removing air bubbles
Do not press the cartridge release button during these steps.

- A.
- Press the start button. The dosage knob comes out.

- B.
- "00"appears in the digital dose display.

- C.
- Select a dose of 1 unit by turning the dosage knob forward (clockwise) until it clicks.

- D.
- Take off the outer needle cap and keep it to remove the used needle after injection. Take off the inner needle cap and discard it.
- E.
- Hold the pen with the needle pointing up.
- F.
- Tap the insulin reservoir so that any air bubbles rise up towards the needle.
- G.
- Press the dosage knob fully until it stays in. Check that insulin comes out of the needle tip. If it does not you must repeat the test until it does.
With a new cartridge system, or if there are air bubbles in the cartridge system, you may have to perform the safety test several times before insulin is seen.
If no insulin comes out, first check:
- that '01' was visible on the dose display
- that the cartridge system is properly inserted (see Step 1) and then repeat the safety test.
If still no insulin comes out, then:
- Check for air bubbles and repeat the safety test two more times using a dose of 2 units instead of 1 unit.
- If still no insulin comes out, the needle may be blocked. Change the needle and try again.
- If no insulin comes out after changing the needle, your cartridge system may be damaged.
Do not use this cartridge system. Insert a new one.
You can set the dose in steps of 1 unit, from a minimum of 1 unit to a maximum of 80 units. If you need a dose greater than 80 units, you should give it as two or more injections.

- A.
- Press the start button.
- B.
- Select your required dose by turning the dosage knob forward to the right. Make sure that the dosage knob is not in between two dose steps. You must feel and hear a click.
- If you have selected a dose that is too high, simply turn the dosage knob backwards to the left.
- Do not dial past 80. If you do dial past 80, follow the instructions in B. "Questions and answers" section I, to reset the pen.
- You cannot turn the dosage knob past the number of units left in the cartridge system. Do not force the dosage knob to turn. In this case, either you can inject what is remaining in this cartridge system and complete your dose with a new cartridge system, or use a new cartridge system for your full dose.

- A.
- Clean the area of skin to be injected with rubbing alcohol.
- B.
- Use the injection method as instructed by your healthcare professional
- C.
- Insert the needle into the skin.

- D.
- Deliver the dose by pressing the dosage knob all the way in. Do not press the cartridge release button or the start button while injecting.
- If the dosage knob cannot be pressed down, you may have turned the dosage knob so that it is between two dose steps. The pen prevents you from pressing down the dosage knob if you are between two dose steps. Turn the dosage knob to the left or right to the correct dose.
- E.
- Keep the dosage knob pressed all the way in. Slowly count to 10, then make sure that the dosage knob stays in before you withdraw the needle from the skin. This ensures that the full dosage is delivered.
After injecting your dose, the digital dose display will not go back to "0" but will show the delivered dose for 2 minutes. Do not re-inject your dose as this may result in an overdose.
Step 7: Remove and discard the needle
Always remove the needle after each injection and store OptiClik without a needle attached. This prevents entry of air into the insulin reservoir and leakage of insulin, which can cause inaccurate dosing.
- A.
- Put the outer needle cap back on the needle, and use it to unscrew the needle from the pen. To reduce the risk of accidental needle penetration, never replace the inner needle cap.
- If your injection is given by another person, special caution must be taken by this person when removing and disposing the needle. Follow recommended safety measures for removal and disposal of needles (e.g. a one handed capping technique) in order to reduce the risk of accidental needle penetration and transmission of infectious diseases.

- B.
- Dispose of the needle safely, as instructed by your healthcare professional. For safe disposal of needles see (A.) GENERAL NOTES, Needles for OptiClik.
- C.
- Always put the pen cap back on the pen body, then store the pen until your next injection.
Step 8: Replacing an empty cartridge system

- A.
- Make sure the dosage knob is pushed in.
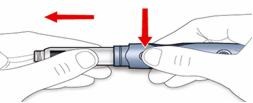
- B.
- Press the cartridge release button, and remove the entire cartridge system. Dispose of the cartridge system.
Start again at Step 1.
Cartridge system
The cartridge system is available separately. Each cartridge system contains 300 units of insulin.
Be sure to read and follow the instructions in the patient information leaflet for the insulin.
Do not remove the cartridge system from packaging until ready to use. This will prevent dust or dirt from getting into the mechanical parts of the cartridge system.
When you need a new cartridge system, take it out of the refrigerator 1–2 hours before you inject to allow it to warm up to room temperature. Cold insulin is more painful to inject.
Do not open or manipulate the cartridge system in any way.
Needles for OptiClik
BD Ultra-Fine needles are available from BD Consumer Healthcare.
Needles may vary from country to country and may not be interchangeable. If you intend to travel abroad, make sure that you have sufficient needles and insulin with you.
Needle disposal
Used needles should be placed in sharps containers (such as red biohazard containers), hard plastic containers (such as detergent bottles), or metal containers (such as an empty coffee can). Such containers should be sealed and disposed of properly.
B. QUESTIONS AND ANSWERS
I. Dose-setting
You hear no clicking sound during dose-setting:
The cartridge system may have been inserted incorrectly. Check by trying to pull the cartridge system gently out. If the cartridge system comes out, reinsert it completely following the instructions in Step 1. Perform a safety test before dialing your dose.
If you still hear no clicking sound, try a new cartridge system and listen for clicking sound. In case there is still no clicking sound, obtain a new OptiClik.
If insulin drips from the needle tip during dose-setting
Or, if you have dialed to 80 and then continued to dial:
The maximum dose of OptiClik is 80 units. If you continue to dial after reaching 80 units, insulin will drip from the needle and the display will continue to show "80".
- DO NOT dial back to your required dose, instead dial back to "00".
- Then press the dosage knob to eject excess insulin and to reset OptiClik. OptiClik is now again ready for dose setting.
If you need a dose greater than 80 units, you should give it as two or more injections.
If you cannot turn the dosage knob to set your dose:
Do not force the dosage knob to turn any further.
- a)
- You are turning to the left and trying to dial down below zero. Turn the dosage knob forward to the right to dial your dose.
- b)
- The cartridge system is almost empty and no longer contains a sufficient amount of insulin for the dose you need.
- 1)
- EITHER, inject the partial dose that is in this cartridge system, then change the cartridge system and complete your dose from the new cartridge system.
- 2)
- OR, change the cartridge system and give your complete dose from the new cartridge system. Dial back (to the left) to "00" before releasing the old cartridge system.
- c)
- You have dialed past the maximum dose of 80 units and either have no needle attached or the needle is blocked.
- Dial completely backward to "00"
- Attach a new needle and then perform a safety test before dialing your dose.
The dosage knob does not stop at "00":
When turned back completely, the dosage knob should stop with the dose display at "00", however, sometimes it may stop at "02" or "01". Make sure that a needle is attached, then press the dosage knob down (insulin will appear at the tip of the needle). OptiClik is now ready for use.
The dosage knob no longer turns after a new cartridge system has been inserted:
Check that the cartridge system is firmly clicked in. Reseat the cartridge system and try again. If it still does not work, try again with a new cartridge system. Otherwise, get a new OptiClik.
The dosage knob does not come out after you pressed the start button:
Do not pull out the dosage knob. Check that the cartridge system is firmly clicked in (see Step 1C and D).
II. Insulin injection
The dosage knob cannot be pressed down for the insulin injection:
- a)
- You have dialed between two dose steps (see Step 5B)
- b)
- The needle may be blocked or defective. Use a new needle.
The dosage knob does not stay down at the end of injection:
Make sure you are not accidentally pressing the start button at the same time.
After withdrawing the needle from your skin, more than one drop of insulin drips from the needle:
It is possible that you may not have injected your full insulin dose. DO NOT try to make up for the shortfall in your insulin dose by giving a second injection (otherwise you will be at risk for low blood sugar).
Please check your blood sugar and consult with your healthcare professional.
You can avoid the problem next time by taking the following steps:
- a)
- Remove any air bubbles that may be present in the cartridge system (see step 4).
- b)
- After delivering the insulin dose, slowly count to 10 before withdrawing the needle from your skin.
III. Digital dose display functions
Reading the dose display
To read the dose correctly, hold OptiClik as shown in Step 5B, Select the dose. The printed "OptiClik" must be readable left of the dose display. Do not hold the pen upside down when reading the dose display; otherwise you may misread the dose on the digital dose display.
Dose display energy save function
The dose display switches off after two minutes of no activity, to conserve battery power.
The dose display goes blank during dose setting
The device has been inactive for 2 minutes (e.g. if you were interrupted in the middle of your injection preparations) and the display has turned off to conserve battery power. Turn the dosage knob one click forward. OptiClik should now be ready to use again; check the digital dose display and adjust for the right dose if needed.
No numbers appear on the Digital Dose Display when the start button is pressed or when the dosage knob is released:
Press the dosage knob. Start with a Safety Test (Step 4).
If there are still no numbers on the digital dose display, you should obtain a new OptiClik.
 is displayed:
is displayed:
The dosage knob has been forced into the negative range with excessive force. The cartridge system might be damaged and needs to be replaced. Remove this cartridge system (step 8) and start again at Step 1 with a new cartridge system.
 and
and flash alternately:
flash alternately:
- a)
- The dosage knob has been forced into the negative range and was pushed in. The cartridge system might be damaged and needs to be replaced. Remove this cartridge system (step 8) and start again at Step 1 with a new cartridge system.
- b)
- The dosage knob has been turned too quickly.
- EITHER, dispose of the unknown pre-set dose by pressing the dosage knob. Set your dose (Step 5) and inject your dose (Step 6).
OR, turn the dosage knob slowly backward until it stops, and then push the dosage knob in. Restart OptiClik and dial your dose.
IV. Lifetime of OptiClik and the battery information.
Lifetime of OptiClik:
OptiClik has a lifetime of 3 years after first use.
 flashes when the Start Button is pressed:
flashes when the Start Button is pressed:
OptiClik is reaching the end of its lifetime (3 years). The digital dose display will continue to operate for about 4 more weeks. Please obtain a new OptiClik.
 stays when the Start Button is pressed:
stays when the Start Button is pressed:
OptiClik has reached the end of its lifetime. When you continue to turn the dosage knob, the display still shows  . Please obtain a new OptiClik.
. Please obtain a new OptiClik.
Battery information:
 flashes when the Start Button is pressed:
flashes when the Start Button is pressed:
Your battery is running out. Please obtain a new OptiClik as soon as possible.
 is displayed when the Start Button is pressed:
is displayed when the Start Button is pressed:
Your battery has run out. Please obtain a new OptiClik.
C. STORAGE INSTRUCTIONS
Never store OptiClik in a refrigerator. Protect OptiClik from moisture and direct heat.
Always store OptiClik without the needle attached.
When OptiClik is stored, push the dosage knob in. This conserves the battery and ensures that the pen functions throughout its scheduled lifetime.
To avoid dust or dirt from getting into the pen body, always replace the pen cap.
Once the cartridge system is in use, it can be used for up to 28 days under normal carrying conditions (for Lantus, below 86°F [30°C]; for Apidra, below 77°F [25°C]). For specific insulin storage information, see "Patient Information" for Lantus or Apidra 3 mL Cartridge System for cartridge system storage information.
D. CARING FOR YOUR OPTICLIK
Care, cleaning, and maintenance instructions
Handle OptiClik carefully. Regularly clean your OptiClik, by using a clean damp cloth. Dirt can impede the operation. DO NOT use cleaning agents. Use an alcohol swab only for cleaning the cartridge system's rubber seal.
Damage to OptiClik
OptiClik may become damaged by rough handling, dropping, or turning of the dosage knob by force. Make sure that no dirt comes in contact with the mechanical parts. You should always make sure that:
- 1)
- The cartridge system is not damaged.
- 2)
- The start Button, dosage knob, and digital dose display still operate properly.
Do not use tools on OptiClik. If you are not sure whether or not your OptiClik is damaged, contact your health care professional or call 1-800-633-1610. If damaged, it is no longer safe to use it. In an emergency, you can draw up the insulin from the cartridge system using a U-100 insulin syringe.
APIDRA® SoloStar®
(insulin glulisine [rDNA origin] injection)
3 mL prefilled pen
Patient Instructions for Use
Be sure that you read, understand and follow these instructions before you use your APIDRA SoloStar®. Talk with your healthcare provider about the right way to use your APIDRA SoloStar before you use it for the first time. Keep this leaflet in case you need to look at it again later.
APIDRA SoloStar should not be used by people who are blind or have severe vision problems, without the help of a person who has good eyesight and who is trained to use the APIDRA SoloStar the right way.
APIDRA SoloStar is a disposable prefilled pen used to inject APIDRA. Each APIDRA SoloStar has 300 units of insulin which can be used for many doses. You can select a dose from 1 to 80 units. The pen plunger moves with each dose. The plunger will only move to the end of the cartridge when 300 units of insulin have been given.
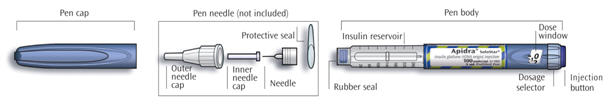
If you will give yourself subcutaneous injections of APIDRA:
- You should take APIDRA within 15 minutes before a meal or within 20 minutes after starting a meal.
- Do not inject APIDRA if you are not going to eat within 15 minutes.
- Inject APIDRA into the skin of your upper arm, thigh, or stomach area. Do not inject APIDRA into a vein or into a muscle.
- Choose an injection area (upper arm, thigh, or stomach area). Change injection sites within the area you choose with each dose. Do not inject into the exact same spot for each injection.
Important information for use of APIDRA SoloStar:
- Use a new needle for each injection.
APIDRA Solostar may be used with pen needles from Becton Dickinson and Company, Ypsomed and Owen Mumford. Contact your healthcare provider for further information. - Do a safety test before each injection. (See step 3.)
- Do not share your APIDRA SoloStar with others even if they have diabetes.
- If your injection is given by another person, this person must be careful to avoid accidental needle stick injury and prevent passing (transmission of) infection.
- Do not use APIDRA SoloStar if it is damaged or if you are not sure that it is working correctly.
- Always carry an extra APIDRA SoloStar prefilled pen in case your APIDRA SoloStar is lost or damaged.
Step 1. Preparing for an injection
Make sure you have the following items:
- Apidra SoloStar
- Pen needles
- Alcohol swab
- Puncture resistant container. See "How do I dispose of used needles and APIDRA SoloStar?".
- A.
- Check the label on your APIDRA SoloStar to make sure you have the right insulin. The APIDRA Solostar is blue. It has a dark blue injection button with a raised ring on the top.
- B.
- Check the expiration date, located on the carton or the label of your APIDRA SoloStar to make sure the date has not passed. Do not use an APIDRA SoloStar if the date has passed.
- C.
- Take off the pen cap.
- D.
- Look at the insulin in your APIDRA SoloStar. Check to make sure that the insulin looks clear. Do not use this APIDRA SoloStar if the insulin is cloudy, colored, or has particles in it.
Step 2. Attaching the needle
Always use a new sterile needle for each injection to help prevent contamination, and potential needle blocks.
Read the pen needle "Instructions for Use" before you use them.
Please note: Pen needles may look different. The pen needles shown are for illustrative purposes only.
- A.
- Wipe the Rubber Seal with alcohol.
- B.
- Remove the protective seal from the new pen needle.
- C.
- Line up the needle with the pen, and keep it straight as you attach it (screw or push on, depending on the needle type).

- If you do not keep the needle straight while you attach it this can damage the rubber seal, and cause leakage of insulin, or break the needle.

Do a safety test before each injection to make sure that you get the correct dose of APIDRA. The safety test:
- makes sure that the pen and needle work properly
- removes air bubbles
- A.
- Select a dose of 2 units by turning the dosage selector.

- B.
- Take off the outer needle cap and keep it to remove the used needle after injection. Take off the inner needle cap and dispose of it.
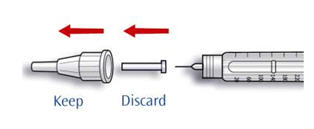
- C.
- Hold the pen with the needle pointing upwards.
- D.
- Tap the insulin reservoir so that any air bubbles rise up towards the needle.
- E.
- Press the injection button all the way in. Check if insulin comes out of the needle tip.
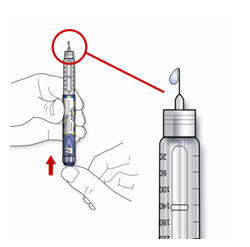
You may have to do the safety test more than once before you see the insulin.
- If no insulin comes out, check for air bubbles and repeat the safety test two more times to remove them.
- If still no insulin comes out, the needle may be blocked. Change the needle and try again.
- If no insulin comes out after changing the needle, your APIDRA SoloStar may be damaged. Do not use this APIDRA SoloStar.
Step 4. Selecting your dose
Select the APIDRA dose prescribed by your healthcare provider. You can select the insulin dose in steps of 1 unit, from a minimum of 1 unit to a maximum of 80 units. If you need a dose larger than 80 units, you should give it as two or more injections.
- A.
- Check that the dose window shows "0" after the safety test.
- B.
- Select your needed dose (in the example below, the selected dose is 30 units). If you turn past your dose, you can turn back down.
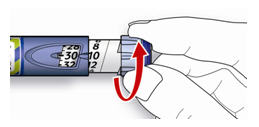
- Do not push the injection button while turning, insulin will come out.
- You cannot turn the dosage selector passed the number of units left in the pen. Do not force the dosage selector to turn. In this case, either you can inject the amount of insulin that is still in the pen and finish your dose with a new APIDRA SoloStar or you can use a new APIDRA SoloStar for your full dose.
Step 5. Giving the injection
- A.
- Give the injection exactly as shown to you by your healthcare provider.
- B.
- Insert the needle into your skin.

- C.
- Inject the dose by pressing the injection button in all the way. Only push the injection button when you are ready to inject. The number in the dose window will return to "0" as you inject.

- D.
- Keep the injection button pressed all the way in. Slowly count to 10 before you take the needle out of your skin. This will make sure that the full dose has been given.
Step 6. Removing and disposing of the pen needle
Always remove the pen needle after each injection and store your APIDRA SoloStar without a needle attached. This helps prevent:
- Contamination and infection
- Air from getting into the insulin reservoir and leakage of insulin. This will help to make sure you inject the right dose of insulin.
- A.
- Follow the instructions from your healthcare provider when removing and disposing of the needle. For example "scoop" the outer needle cap back on the needle and use it to unscrew the used needle from the pen. To lessen the risk of accidental needle stick injury and passing infection:
- do not recap needles with your fingers
- never replace the inner needle cap.
- B.
- Dispose of the needle the right way into your special puncture resistant container (See "How Do I Dispose of used needles and APIDRA SoloStar?")
- C.
- Always put the pen cap back on the pen, then store the APIDRA SoloStar until your next injection.
How do I dispose of used needles and APIDRA SoloStar?
- Check with your healthcare provider for instructions about the right way to dispose of used needles and APIDRA SoloStar s. There may be local or state laws about how to throw away used needles and APIDRA SoloStar. Do not dispose of used needles or APIDRA SoloStar in household trash and do not recycle them.
- Put used needles and used empty APIDRA SoloStar in a container made specially for disposing of used syringes and needles (called a "sharps" container) or a hard plastic container (such as empty detergent bottles),with a screw-on cap, or metal container with a plastic lid labeled "Used Syringes". These containers should be sealed and disposed of the right way.
How should I Store APIDRA SoloStar?
- Do not refrigerate APIDRA SoloStar after first use.
- Keep at room temperature below 77ºF (25ºC).
- Dispose of any opened APIDRA SoloStar 28 days after first use.
Maintenance
- Protect your APIDRA SoloStar from dust and dirt.
- You can clean the outside of your APIDRA SoloStar by wiping it with a damp cloth.
- Do not soak, wash or lubricate the pen as this may damage it.
- Handle your APIDRA SoloStar with care. Avoid situations where your APIDRA SoloStar might be damaged. If you are concerned that your APIDRA SoloStar may be damaged, use a new one.
If you have any questions about APIDRA SoloStar or about diabetes, ask your healthcare provider, go to www.apidra.com or call sanofi-aventis U.S. at 1-800-633-1610.
sanofi-aventis U.S. LLC
Bridgewater, NJ 08807
Date of revision:
February 2009
©2009 sanofi-aventis U.S. LLC
| APIDRA
insulin glulisine injection, solution |
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
| APIDRA SOLOSTAR
insulin glulisine injection, solution |
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
Revised: 03/2009sanofi-aventis U.S. LLC